Abstract
Rationale:
Transforaminal lumbar interbody fusion (TLIF) is an effective treatment for patients with degenerative lumbar disc disorder. Contralateral radiculopathy, as a complication of TLIF, has been recognized in this institution, but is rarely reported in the literature.
Patient concerns:
In this article, we report 2 cases of contralateral radiculopathy after TLIF in our institution and its associated complications.
Diagnoses:
In the 2 cases, the postoperative computed tomography (CT) and magnetic resonance image (MRI) showed obvious upward movement of the superior articular process, leading to contralateral foraminal stenosis.
Interventions:
Revision surgery was done at once to partially resect the opposite superior facet and to relieve nerve root compression.
Outcomes:
After revision surgery, the contralateral radiculopathy disappeared.
Lessons:
Contralateral radiculopathy is an avoidable potential complication. It is very important to create careful preoperative plans and to conscientiously plan the use of intraoperative techniques. In case of postoperative contralateral leg pain, the patients should be examined by CT and MRI. If CT and MRI show that the superior articular process significantly migrated upwards, which leads to contralateral foraminal stenosis, revision surgery should be done at once to partially resect the contralateral superior facet so as to relieve nerve root compression and avoid possible long-term impairment.
Keywords: complication, contralateral, radiculopathy, transforaminal lumbar interbody fusion
1. Introduction
Lumber spinal fusion with instrumentation is an effective surgical procedure for patients with degenerative spondylolisthesis and degenerative disc disease.[1] The treatment is composed of posterior lumbar interbody fusion (PLIF), anterior lumbar interbody fusion (ALIF), and transforaminal lumbar interbody fusion (TLIF) techniques.[2,3] TLIF was pioneered by Harms and Jeszenszky in 1998.[4] It has been used for a variety of degenerative lumbar disc disorders. The advantages of the TLIF technique over the ALIF and PLIF include the avoidance of the anterior approach, decreased need for nerve root retraction, and cauda equina as the facets on 1 side are totally resected.[5] Moreover, a high fusion rate was reported using this technique.[6]
In classic TLIF, we usually approach from the side of the symptomatic radiculopathy. In the past, it was commonly assumed that the TLIF spacer increases the disc space height and the foraminal height on the contralateral foramen of the TLIF approach. Although there are few reports on contralateral radiculopathy after TLIF, the authors believe that this complication occurs and has been observed in our institution.
During the past 2 years, this complication has been confirmed 4 times in our institution. Two cases were selected to illustrate this finding.
2. Methods
In this article, we reported 2 cases of contralateral radiculopathy after TLIF in our institution and the complications associated with treatment.
In these 2 cases, CT and MRI showed the significant upward movement of the superior articular process, which led to contralateral foraminal stenosis. Revision surgery was done at once to partially resect the contralateral superior facet to relieve nerve root compression. After that, contralateral radiculopathy disappeared.
3. Ethical review and patient consent
All patients provided written informed consent for permission to publish the case reports and all related images. The study also obtained approval from the ethics committee of The Third Hospital of Shijiazhuang.
4. Results
4.1. Case 1
A 58-year-old man complained of right leg pain of 4 months’ duration. He had tenderness on the lumbar vertebra of L4 and L5 and radiating pain in the right leg. There was numbness and hypesthesia distributed on the skin over L4, L5, and S1. The extensor hallucis muscle grade was IV. MRI of the lumbar spine confirmed protrusion of the intervertebral disc at L4/L5 and L5/S1 levels (Fig. 1).
Figure 1.
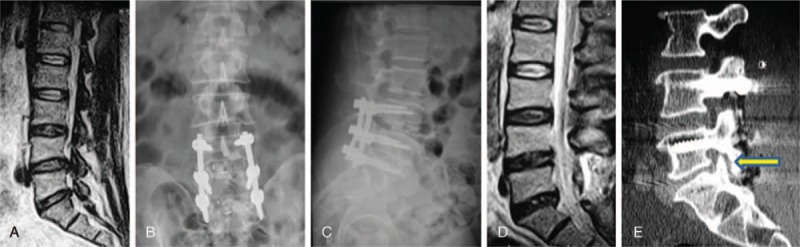
(A) Preoperative magnetic resonance imaging (MRI) demonstrated right L4–5 and L5-S1foraminal stenosis. (B, C) The postoperative x-ray demonstrated no malpositioning of the pedicle screw or disc material compressing the nerve. (d) The postoperative MRI revealed no obvious disc material compressing the nerve. (e) Postoperative computed tomography scan revealed that left S1 superior articular process shifted up and foraminal stenosis on the left side.
After failed conservative treatment, the patient underwent a right-sided TLIF on L4–S1 with decompression. The dura and nerve root were protected when the disc space was prepared for the insertion of one cage from the right side. Postoperatively, the patient reported no right leg pain. However, he complained of left leg pain with an L5 distribution.
Postoperative x-rays and MRI showed no obvious malposition of the pedicle screw or disc components that may compress the nerve. However, CT demonstrated superior displacement of left S1 superior articular process and foraminal stenosis on the left side.
The patient underwent epidural steroid injection for the second time but it was ineffective. Finally, the patient underwent spinal canal exploratory surgery. During operation, we found that the left L5 nerve root was extruded by the tip of the S1 superior articular process. We resected the tip of the S1 superior articular process and found that the left L5 nerve root canal was enlarged. There was no significant compression on the left L5 nerve root. Postoperatively, the patient's left leg pain was relieved.
4.2. Case 2
A healthy 54-year-old man complained of low back pain and radiating right leg pain with associated numbness in the L5 nerve root distribution. On physical examination, he had tenderness on L4, L5, and the right paraspinal muscle. Neurologic examination revealed L4/L5 motor strength weakness in his right extensor hallucis muscle and decreased sensation to light touch and pin prick in the dorsum and lateral aspect of his right foot. He had a markedly positive straight-leg raise test on the right side. x-rays demonstrated a degenerative L4-L5 instability. MRI of the lumbar spine confirmed a right-sided L4/L5 disc protrusion causing severe neural foraminal narrowing with impingement of the right L5 nerve root (Fig. 2).
Figure 2.
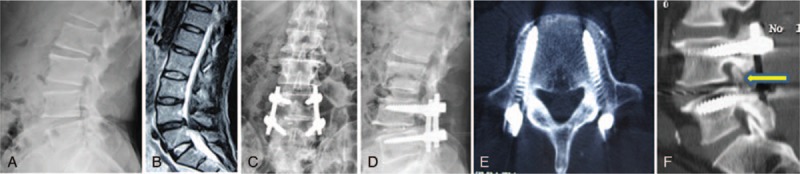
(A) Preoperative x-rays demonstrated degenerative instability in a 54-year-old with right leg pain. (B) Preoperative magnetic resonance imaging demonstrated right L4–5 foraminal stenosis. (C, D) Transforaminal lumbar interbody fusion started from the right side. The patient developed new onset left leg pain in L4 distribution. (E) The postoperative computed tomography (CT) scan revealed that the left pedicle screw was clearly outside the spinal canal and not responsible for the postoperative leg pain. (F) The postoperative CT scan revealed that left L5 superior articular process shifted up and foraminal stenosis on the left side.
The patient underwent a TLIF of L4-L5 with right-sided decompression. After the operation, the right leg pain was relieved, however, the patient complained of left leg pain in L4 distribution. Postoperative x-rays and CT showed no obvious malposition of the instrumentation or disc material compressing the nerve, but demonstrated left-sided foraminal stenosis.
After failed conservative treatment, the patient underwent L4 nerve root neurolysis. During the operation, we found that the L5 superior articular process moved upwards and extruded the left L4 nerve root. The L5 superior articular process was resected by Kerrison rongeur. After the operation, symptoms of left leg pain were relieved.
5. Discussion
TLIF is widely used in lumbar spinal fusion because it can provide circumferential fusion through the posterior approach while avoiding the morbidity of an anterior approach. TLIF techniques include pedicle screw placement; unilateral facet removal; nerve root protection; contralateral distraction; discectomy; anterior bone graft; interbody cage placement; distraction release and cage compression; and pedicle screw plate fixation.[7] Fusion is enhanced because of the increased bone graft area in the disc space with the graft under compression. Disc height is partially restored, and moderate slip reduction occurs, enhancing nerve root decompression. The successful clinical outcomes of TLIF have been recognized by most spine surgeons.[2,8,9] At the same time, the complications of TLIF have been demonstrated in many studies. It includes ipsilateral nerve injury, cerebrospinal fluid leak, wound infection, non-union, failure of fixation, and so on.[10,11] To the best of our knowledge, contralateral radiculopathy is a complication which has not been widely recognized in the literature. Contralateral radiculopathy after TLIF was reported and some reasons for the development of the complication were mentioned in the case report. However, these reasons have not been demonstrated.
We presented 2 cases of patients who complained of contralateral leg pain after TLIF and posited possible reasons for contralateral radiculopathy. The author believes that the upward movement of the superior facet plays an important role in the development of complications, which has been demonstrated during operations.
During TLIF, the compression on the pedicle screw after inserting the cage leads to the upward movement of the superior facet and induced opposite foraminal stenosis, which compressed the exiting nerve root.
The rods usually are precurved to achieve desirable lordosis. Lordosis is restored by compressing the pedicle screws along the rods and tightening the implants. However, this procedure can cause the superior articular processes to move upwards along the rods and disturb the exiting nerve root.
If the intervertebral disc cannot be completely cleared away, contralateral disc herniation after TLIF may compress the nondecompressed side of the nerve root.
Hackenberg et al[5] reported one case wherein the symptomatic compression of the contralateral nerve root resulted from herniated disc material that had been pushed to the contralateral side during cage insertion.
If the cage is not in the neutral position, the undistracted contralateral foramen will probably be compressed.
In the 2 cases, we found that the superior articular process moved upwards; consequently, the exiting nerve root was disturbed. Generally, the superior articular process should not exceed the inferior border of the vertebrae (Body-Joint Line).[12] To avoid contralateral radiculopathy, it is necessary to make a series of careful observations and to analyze the images before the operation. If imaging demonstrated that the contralateral intervertebral foramen has stenosis, for example, the tip of the superior articular process has reached the level of the lower endplate of the upper vertebral body and the risk of symptoms on the contralateral side will increase after the operation. Thus, more attention should be paid to TILF. During TLIF, the disc should be almost completely eliminated and then 1 or 2 cages should be inserted in the anterior center of intervertebral space. The cage with the appropriate size should be placed in the middle of the intervertebral disc.
It is unwise for hypolordotic degenerative spine intraoperative restoring excessively lordosis. The contralateral nerve root can be compressed by iatrogenic foraminal stenosis, which is caused by excessively correcting the flat back deformity. The rods should be moderately curved and the screws should not be compressed inordinately after cage insertion. The rods should be mounted under slight compression. For patients who have obvious foramina and lateral recess stenosis on the contralateral side, preventive decompression should be done, even though they may appear asymptomatic before the operation.
6. Conclusions
Contralateral radiculopathy is an avoidable complication. Careful preoperative planning and conscientious intraoperative manipulation is needed to avoid it. In case of the postoperative contralateral leg pain, the patients should be examined by CT and MRI in time. If CT and MRI show significant upward movement of the superior articular process, contralateral foraminal stenosis may occur. Repair operation should be done immediately to partially resect the contralateral superior facet to relieve the nerve root and avoid possible long-term impairment.
Author contributions
Conceptualization: Xianze Sun.
Data curation: Zhen-Fang Gu.
Methodology: Jinhe Yu.
Writing – original draft: Hongtao Hu, Feng-Yu Liu.
Writing – review & editing: Liang Ren, Feng-Yu Liu.
Footnotes
Abbreviations: ALIF = anterior lumbar interbody fusion, CT = computer tomography, MRI = magnetic resonance imaging, PLIF = posterolumbar interbody fusion, TLIF = transforaminal lumbar interbody fusion.
The manuscript does not involve any information on medical device(s)/drug(s).
The authors report no conflicts of interest.
References
- [1].Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis: updated cochrane review. Spine (Phila Pa 1976) 2005;30:2312–20. [DOI] [PubMed] [Google Scholar]
- [2].Whitecloud TS, Roesch WW, Ricciardi JE. Transforaminal interbody fusion versus anterior–posterior interbody fusion of the lumbar spine: a financial analysis. J Spinal Disord 2001;14:100–2. [DOI] [PubMed] [Google Scholar]
- [3].Fritzell P, Hagg O, Wessberg P, et al. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine (Phila Pa 1976) 2002;27:1131–41. [DOI] [PubMed] [Google Scholar]
- [4].Harms JG, Jeszenszky D. Die posteriore, lumbale, interkorporelle Fusion in unilateraler transforaminaler Technik. Oper Orthop Traumatol 1998;10:90–102. [DOI] [PubMed] [Google Scholar]
- [5].Hackenberg L, Halm H, Bullmann V. Liljenqvist U Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 2005;14:551–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Humphreys SC, Hodges SD, Patwardhan AG. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976) 2001;26:567–71. [DOI] [PubMed] [Google Scholar]
- [7].Singh K, Vaccaro AR. Treatment of lumbar instability: transforaminal lumbar interbody fusion. Semin Spine Surg 2005;17:259–66. [Google Scholar]
- [8].Mandan S, Boeree NR. Outcome of posterior interbody fusion versus posterolateral fusion for spondylolythic spondylolisthesis. Spine (Phila Pa 1976) 2002;27:1536–42. [DOI] [PubMed] [Google Scholar]
- [9].Schofferman J, Slosar P, Reynolds J. A prospective randomized comparison of 270 degrees fusion to 360 degrees fusion (circumferential fusions). Spine (Phila Pa 1976) 2001;26:E207–12. [DOI] [PubMed] [Google Scholar]
- [10].Hunt T, Francis H, Shen, et al. Contralateral radiculopathy after transforaminal lumbar interbody fusion. Eur Spine J 2007;16(suppl 3):311–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Potter BK, Freedman BA, Verwiebe EG. Transforaminal lumbar interbody fusion clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord 2005;18:337–46. [DOI] [PubMed] [Google Scholar]
- [12].Emery H. Spine: State of the art reviews [M]. VS: Hanley Belfus 1987;369–83. [Google Scholar]


