Abstract
Italy, along with Poland and Hungary, has the highest cesarean section rate (35.7%) in Europe. Among Italian regions, Campania has the highest rate of cesarean section (58.4%).
We developed a standardized antenatal class to evaluate whether women who attend this class during pregnancy have a lower cesarean section rate. This antenatal class was developed according to the indication of the Italian Ministry of Health and the World Health Organization. We selected a cohort of women who participated in this antenatal class and a cohort of women who did not participate. We collected information on the mode of delivery, and other characteristics, of these women from certificate of birth assistance form available in 2 hospitals where the women gave birth.
Among women who participated in the antenatal class, there were more Italians, the women were more educated, more women were employed and there were more primiparas compared with those who did not participate. Non-participants of antenatal class showed a higher rate of cesarean section than those who participated (56.2% vs 23.1%; relative risk [RR] = 2.43; 95% confidence interval [CI] 1.95–3.03; P < .0001), as well as after adjustment for other variables. This difference was stronger in 1 hospital (RR = 2.88; 95% CI 2.13–3.89; P < .0001) than in the other hospital (RR = 1.86; 95% CI 1.36–2.55; P < .0001).
Our standardized antenatal class, which was performed in an area with a high rate of cesarean section, significantly reduced this rate, and this was still significant after adjustment for potential confounders.
Keywords: antenatal class, cesarean section, childbirth, epidemiology, retrospective cohort study
1. Introduction
According the Organization for Economic Co-operation and Development Data (OECD),[1] among European countries Italy, Poland, and Hungary have the highest cesarean section (CS) rate (35.7%), whereas Scandinavian nations have the lowest (Finland 15.8%; Norway 16.6%; and Sweden 17.0%). Among Italian regions, Campania has the highest rate of CS (58.4%). Moreover, in private hospital, with the number of deliveries <500 for per year, this rate has even reached 84.4%.[2] Although antenatal classes not always have demonstrated a clear effect on the mode of birth, they can be considerate an important tool for reducing the cesarean rate.[3–8]
In a previous retrospective cohort study in the Campania region,[9] we evaluated whether participation in antenatal classes during pregnancy reduced the use of CS. We found a moderate efficacy of antenatal classes with an approximately 10% reduction in the rate of CS. However, this rate remained much higher than that recommended by the World Health Organization (WHO).[10] Our result was attributed to the heterogeneity of the classes provided, in terms of content and duration.
Therefore, we developed a unique, standardized antenatal class to evaluate whether women who attend this class during pregnancy have a reduced rate of CS, as close as possible to that of WHO.
2. Materials and methods
2.1. Setting
The study was conducted in the area of the Local Health Authority (Azienda Sanitaria Locale) in the city of Caserta (ASLCE, Campania region, Italy) which has approximately 900,000 inhabitants.[11] In this Local Health Authority we performed our standardized antenatal class. Most of the women who participated in this antenatal class gave birth in the 2 public hospitals of ASLCE: Azienda Ospedaliera S. Anna e S. Sebastiano (AO) and Presidio Ospedaliero Marcianise (PO).
2.2. Antenatal class
The antenatal class of the ASLCE was developed from 2010 to 2012, according to the indication of the Italian Ministry of Health[12–16] and of the WHO.[17,18] This class was then carried out in 2 Health Districts (Distretti Sanitari nos. 12 and 16) of ASLCE, under the scientific supervision of the Department of Psychology of the University of Campania.
The antenatal class involved 12 meetings, 11 in pregnancy and 1 in postpartum. Each meeting was propaedeutic to the next, lasted for 3 hours and provided a theoretical part and a practical part. In the theoretical part, a single member of the multidisciplinary team conducted each meeting. Information was provided on anatomy and physiology of pregnancy and maternity, food education, psychological aspects of pregnancy, labor-intensive care procedures, breastfeeding, childhood education, pediatric prevention, puerperium contraception, mother–child relationship, and depressive phenomena in the postpartum period. The practical/experiential part of the class, conducted by an obstetrician, involved pregnancy and labor exercises based on the “Metodologia Funzionale” (Functional Methodology).[19]
In meetings with a nutritionist and psychologist (III and IV), a questionnaire for food screening and 2 questionnaires on depression (Edinburgh Postnatal Depression Scale[20] and Beck Depression Inventory-Second Edition)[21] were provided for early detection of risk in pregnancy and at postpartum. During the ninth meeting conducted by the psychologist the results of the tests were returned anonymously to the pregnant women. This was performed as a starting point for teamwork to discuss the psychological aspects of postpartum and to facilitate requests for individual/or couple counseling.
The pregnant women also visited the labor, birth, and nursing rooms, to allow contact with the hospital structure and provide information on the type of care offered there.
In addition to psychological counseling, and at the request of pregnant women, midwifery, gynecological, pediatric, and nutritional counseling was offered. Finally, the women could receive a home visit for assisting in puerperium and breastfeeding. Each meeting was open to the participation of the fathers.
2.3. Certificates of birth assistance
In Italy all women who give birth are interviewed by a structured questionnaire named Certificato di Assistenza Parto (CEDAP—certificate of birth assistance). This form includes information on sociodemographic characteristics of parents, pregnancy, childbirth, newborn, causes of newborn death, and presence of malformations. However, this form does not provide information about participation of women in antenatal classes.
2.4. Study design, data collection, and participants
The study was a retrospective cohort study. The first cohort (participant in the antenatal class) was collected in the archive of the antenatal class; to get the defined sample size, this cohort included women who participated in this class from October 2013 (starting date of the antenatal class) to December 2016, and who gave birth during February 2014 to May 2017 in the 2 selected hospitals.
From October 2016 to May 2017, 3 healthcare workers of the ASLCE visited the archive of each hospital to collect data about first and second cohort from the CEDAP forms that were ordered according to the date of delivery. The healthcare workers filled in a form and transferred on another form only the information that was useful for the study, such as sociodemographic data, and information on pregnancy and childbirth. For every woman who was included as a participant in the antenatal class (first cohort), the first 3 women who matched the inclusion criteria were selected as the second cohort of women (non-participant in the antenatal class).
Research ethics committee approval for the study was obtained from the Ethics Committee of the Second University of Naples (n.927/2016).
2.5. Inclusion criteria
For the first cohort we have included, in agreement with the responsible of the antenatal class, women attending at least 9 out of 12 meetings. For the second cohort we included women with similar range of age (approximately 5 years).
2.6. Sample size
The target sample size of approximately 1000 subjects was obtained by assuming 50% of CS in non-participating to antenatal class, a relative risk of 1.25 between participation in antenatal classes and prevented CS, a ratio unexposed/exposed of 3:1, a 95% confidence level and a power of 80%.
2.7. Data analysis
Descriptive analysis was performed for all the variables. Crude relative risks (RRs) with 95% confidence intervals (CIs) were calculated between participation in antenatal class (independent variable) and the mode of delivery (dependent variable and main outcome).
Crude RRs were also calculated between the main outcome and other independent variables, including educational level (up to high school = 0; college degree = 1), marital status (unmarried = 0; other = 1), nationality (not Italian = 0; Italian = 1), number of previous pregnancies (1 = 0; >1 = 1), employment status (unemployed = 0; employed = 1), and place of childbirth (AO = 0; PO = 1). Only variables associated with the outcome with P ≤ .25 were subsequently included in the multivariate regression model and the adjusted odds ratio (OR) has been calculated. Analyses were carried out using Stata 10.[22]
3. Results
After recruitment, 1155 women were included in the study (286 participants in antenatal class and 869 non-participants).
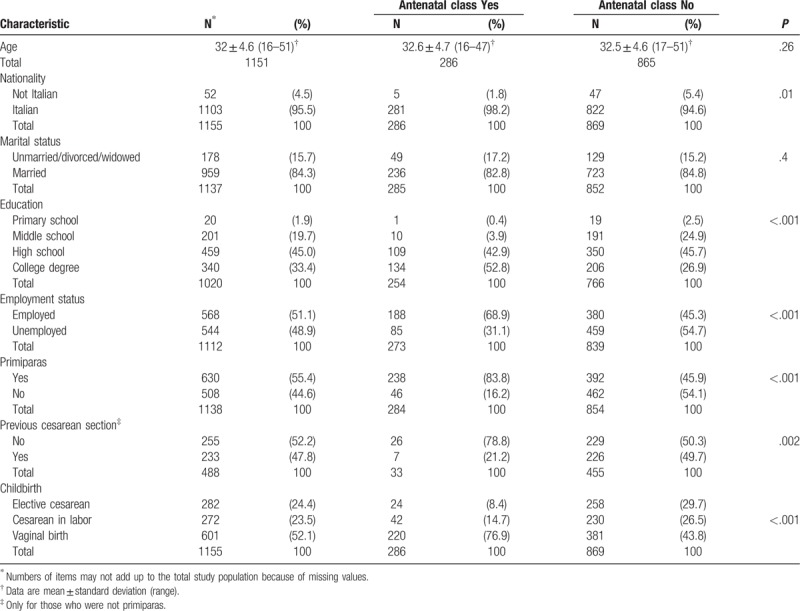
Table 1 shows the sociodemographic characteristics of the 2 cohorts. The ages of the 2 groups were similar because of the prior matching for age. In the cohort of women who participated in the antenatal class, there were more Italians (98.2% vs 94.6%), a higher rate of education (college degree: 52.8% vs 26.9%), a higher rate of employed (68.9% vs 45.3%), more primiparas (83.8% vs 45.9%), and less previous CS (21.2% vs 49.7%) than the other cohort.
Table 1.
Socio-demographic characteristics of the study population.
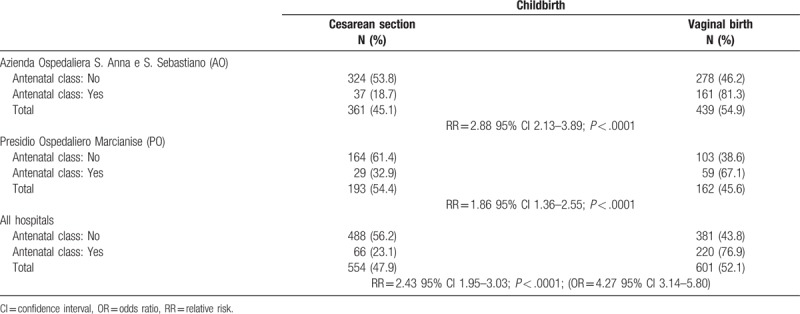
With regard to the relation between the antenatal class and the mode of delivery, non-participants of the antenatal class showed a higher rate of CS than did participants (56.2% vs 23.1%; RR = 2.43; 95% CI 1.95–3.03; P < .0001). This difference in CS rate was stronger in AO (53.8% vs 18.7%; RR = 2.88; 95% CI 2.13–3.89; P < .0001) than in PO (61.4% vs 32.9%; RR = 1.86; 95% CI 1.36–2.55; P < .0001) (Table 2). In the CEDAP form, CS was categorized into 2 types: elective and in labor. When we observed only elective CS, the difference between the 2 groups was still higher (8.4% for women who participated in the antenatal class vs 30.0% for non-participants) (Table 1).
Table 2.
Relationship between antenatal class and childbirth, divided by hospital.
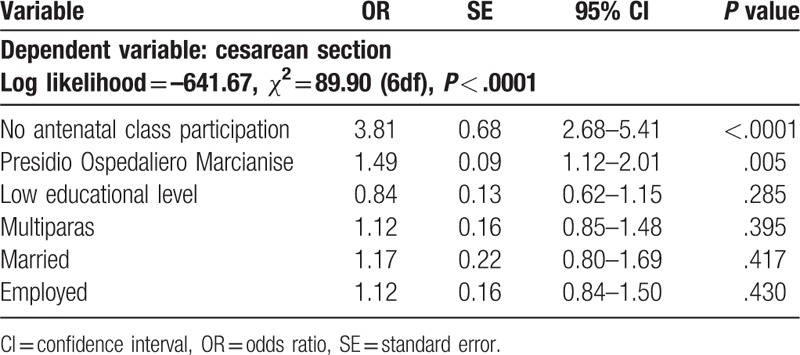
Because the 2 cohorts differed in many socio-demographic characteristics, these characteristics could confound the association between antenatal class and mode of delivery. In bivariate analysis, less educated, employed, and multiparous women were significantly associated with a higher rate of CS (Table 3). In multivariate analysis, the only variable that remained associated with a reduction in the rate of CS was participation in the antenatal class, which showed only a slight reduction in OR (from a crude OR = 4.27 to adjusted OR = 3.69) (Table 4). These results showed that participation in the antenatal class was the only variable that reduced the rate of CS.
Table 3.
Results of univariate analysis.
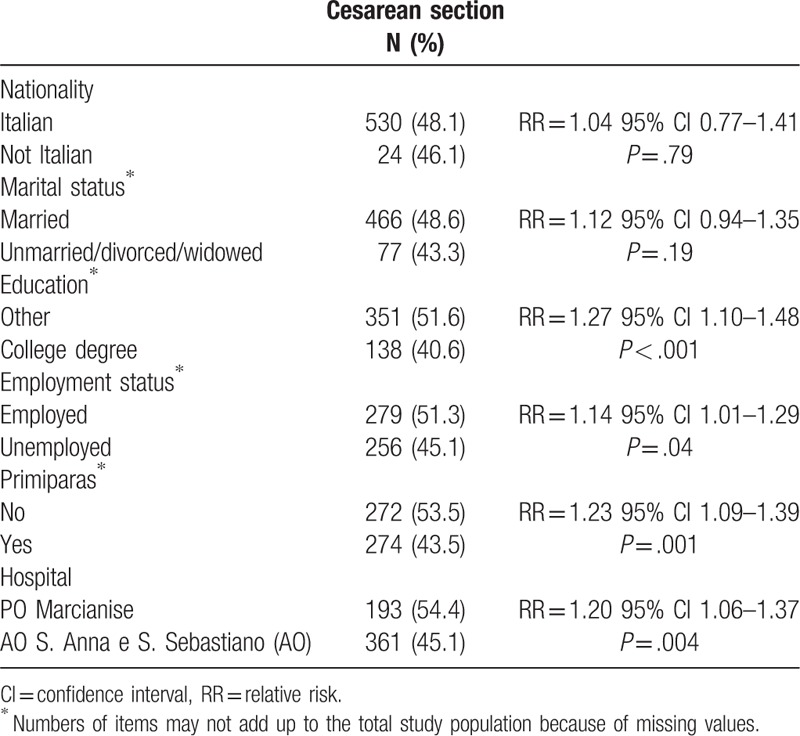
Table 4.
Multivariate logistic regression analysis.
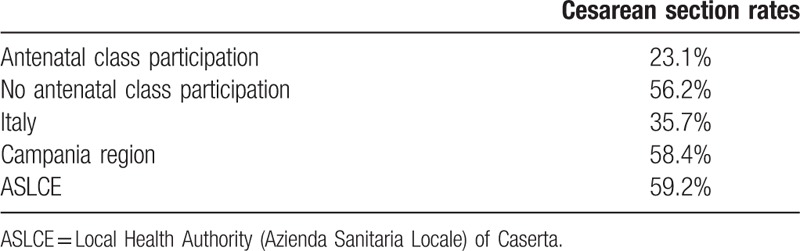
Finally, we compared the CS rate in our study with the most recent data available of the CS rate in Italy, Campania region, and ASLCE (Table 5).
Table 5.
Comparison of cesarean section rates.
4. Discussion
National and international health institutions recommend that pregnant women participate in antenatal classes to increase their capacity for autonomous management of their own health. Several studies have shown that women who attend antenatal classes appear to have less anxiety, have a higher level of knowledge and competence, and require less pharmacological analgesia because they prefer to use other strategies for controlling pain compared with those who do not attend antenatal classes. Moreover, after delivery, women who attend antenatal class appear to breastfeed for a longer period of time, have fewer emotional difficulties, and be more informed about contraceptive methods.[12–15,23–29]
By contrast, the relation between antenatal education and a reduction in CS is more controversial probably because different methods were used and the factors that were identified as affecting the effectiveness of antenatal classes in reducing the rate of CS differed in each study.[3–8] Indeed, the effectiveness of these classes depends on several factors, such as the validity of the course content, an approach supported by scientific evidence, the availability of interactive meetings, and the possibility of involving the whole population and not only women who request it, and the stage of pregnancy in which the classes are attended (at least from the second trimester). Other factors include the possibility of having at least 1 meeting after birth, and effective interaction between family counseling services and the hospital.[15]
Similarly to other studies,[14–15,23] in our study, women who participated in antenatal classes were more frequently primiparas, more educated, and had a higher rate of employment than those who did not participate. However, these characteristics did not affect the main relation between antenatal class and CS. Multivariate analysis showed that only participation in the antenatal class remained significantly associated with reduction in rate of CS. However, this consideration should be cautiously interpreted due to the limitation indicated below.
The main limitations of the study are as follows. First, women attending antenatal classes might be more oriented toward vaginal delivery, regardless of their participation in these classes. Indeed, it is conceivable that a greater attention and awareness on childbirth predisposes women both to a participation in the antenatal class, and to a tendency towards vaginal birth. Therefore, many women could participate in the antenatal classes being already oriented towards vaginal birth. If this situation is true, this could have resulted in overestimation of the effectiveness of antenatal classes. Second, we do not know the accuracy of compilation of the CEDAP form, because the forms were filled in by different healthcare workers in different locations and conditions. Third, the healthcare workers could not be blinded during data collection. However, we believe that the main outcome of interest (cesarean section/vaginal birth) is a dichotomic variable not liable to misclassification. However, another potential misclassification was the participation to antenatal class in the control group. But, in our region such participation is estimated about 10%. Secondly, this misclassification could underestimated the OR rather than overestimated it.
5. Conclusions
The high rate of cesarean sections in Italy, and even more in the Campania region, has been explained by multifactorial factors as the ignorance of the operators, the problems related to the medical–legal issues, the economic interest and the women behavior who base their decisions about childbirth on a poor, and also erroneous, information.
We found that a standardized antenatal class, which was created with strict criteria, and performed in an area with this high rate of CS, significantly seems to reduce this rate, even after adjustment for potential confounders. Indeed, in our previous study in the same area, we achieved a much weaker reduction in CS rate, probably because the independent variables, antenatal classes, were not standardized and having different characteristics.[9] Considering these results, it would be useful to extend this standardized antenatal class to other health service in Campania region.
Author contributions
Conceptualization: Daniela Cantone, Annamaria Lombardi, Francesco Attena.
Data curation: Debora Antonia Assunto, Michela Piccolo, Natascia Rizzo, Concetta Paola Pelullo.
Formal analysis: Concetta Paola Pelullo, Francesco Attena.
Investigation: Debora Antonia Assunto, Michela Piccolo, Natascia Rizzo, Concetta Paola Pelullo, Francesco Attena.
Methodology: Daniela Cantone, Annamaria Lombardi, Francesco Attena.
Software: Concetta Paola Pelullo.
Supervision: Annamaria Lombardi.
Validation: Daniela Cantone, Concetta Paola Pelullo.
Writing – original draft: Daniela Cantone, Francesco Attena.
Footnotes
Abbreviations: AO = Azienda Ospedaliera S. Anna e S. Sebastiano, ASLCE = Local Health Authority (Azienda Sanitaria Locale) of Caserta, CEDAP = certificate of birth assistance (Certificato di Assistenza Parto), CI = confidence interval, CS = cesarean section, OR = odds ratio, PO = Presidio Ospedaliero Marcianise, RR = relative risk.
Source of Funding: The authors of this work have nothing to disclose.
The authors have no conflicts of interest to disclose.
References
- [1].OECD. Caesarean sections (indicator); 2017. doi: 10.1787/adc3c39f-en (accessed on June 8, 2017). [Google Scholar]
- [2].Triassi M, Pugliese A, Castronuovo E, et al (a cura di), Report on the Natality in Campania 2014, Napoli (IT); 2016. Italian. [Google Scholar]
- [3].Campero L, Hernandez B, Osborne J, et al. Support from a prenatal instructor during childbirth is associated with reduced rates of cesarean section in a Mexican study. Midwifery 2004;20:312–23. [DOI] [PubMed] [Google Scholar]
- [4].Mehdizadeh A, Roosta F, Chaichian S, et al. Evaluation of the impact of birth preparation courses on the health of the mother and the newborn. Am J Perinatol 2005;22:7–9. [DOI] [PubMed] [Google Scholar]
- [5].Ecker JL, Frigoletto FD. Cesarean delivery and the risk-benefit calculus. N Engl J Med 2007;356:885–8. [DOI] [PubMed] [Google Scholar]
- [6].Phipps H, Charlton S, Dietz HP. Can antenatal education influence how women push in labour? Aust N Z J Obstet Gynaecol 2009;49:274–8. [DOI] [PubMed] [Google Scholar]
- [7].Bergstrom M, Kieler H, Waldenstrom U. Psychoprophylaxis during labor: associations with labor-related outcomes and experience of childbirth. Acta Obstet Gynecol Scand 2010;89:794–800. [DOI] [PubMed] [Google Scholar]
- [8].Pertile R, Pedron M, Berlanda M, et al. Antenatal course attendance among primiparous mothers, with physiological pregnancy and birth at term in Trentino (Northern Italy): characteristics of non-attender women and benefits among attender women in pregnancy behaviours, type of birth delivery and neonatal outcomes. Epidemiol Prev 2015;39:88–97. [PubMed] [Google Scholar]
- [9].Cantone D, Pelullo CP, Cancellieri M, et al. Can antenatal classes reduce the rate of cesarean section in southern Italy? Women Birth 2017;30:e83–8. [DOI] [PubMed] [Google Scholar]
- [10].World Health Organization. Appropriate technology for birth. Lancet 1985;2:436–7. [PubMed] [Google Scholar]
- [11].Resident population on 1 January 2017. Demographic statistic province of Caserta. Available at: http://dati.istat.it/Index.aspx?DataSetCode=DCIS_POPRES1. Accessed 15 May 2017. [Google Scholar]
- [12].Grandolfo ME, Donati S, Giusti A. Cognitive survey on the birth path 2002. Methodological aspects and national results. Roma: Istituto Superiore di Sanità; 2002. Available at: http://www.epicentro.iss.it/problemi/percorso-nascita/ind-pdf/nascita-1.pdf. Accessed 15 May 2017. [Google Scholar]
- [13].Spinelli A, Baglio G, Donati S, et al. Do antenatal classes benefit the mother and her baby? J Matern Fetal Neonatal Med 2003;13:94–101. [DOI] [PubMed] [Google Scholar]
- [14].Grandolfo ME, Donati S, Giusti A. Giambanco V, et al. Birth: a challenge for social-health systems and for obstetric professions. Epidemiologia e Sanità. Cento (Fe): Editeam; 2004. 27–37. [Google Scholar]
- [15].Lauria L, Lamberti A, Buoncristiano M, Bonciani M, Andreozzi S (Eds.). Birth path: promotion and evaluation of the quality of the operating models. The surveys of 2008–2009 and 2010–2011. Roma: Istituto Superiore di sanità; 2012. (Rapporti ISTISAN 12/39). [Google Scholar]
- [16].National System for Guidelines. Physiological pregnancy -2011 update. Guideline 20. Roma: SNLG-ISS; 2011. Available at: http://www.snlg-iss.it/csm/files/FG_Gravidanza.pdf. Accessed 15 May 2017. [Google Scholar]
- [17].World Health Organization, Department of Making Pregnancy Safer. Standards for Maternal and Neonatal Care. Geneva: World Health Organization; 2006. [Google Scholar]
- [18].WHO Department of Making Pregnancy Safer. Working with individuals, families and communities to improve maternal and newborn health. Geneva: World Health Organization; 2010. Available at: http://www.who.int/maternal_child_adolescent/documents/who_fch_rhr_0311/en/index.html. Accessed 15 May 2017. [Google Scholar]
- [19].Rispoli L. The Basic Experiences and the Development of the Self – Development from the Point of View of Functional Psychotherapy. Bern: Peter Lang Publishing Group; 2008. [Google Scholar]
- [20].Cox J, Holden J. Maternity and psychopathology, guide to the use of the Edinburgh Postnatal Depression Scale, a cura di Grussu P. e Quatraro R.M., Centro Studi Erikson; 2008. [Google Scholar]
- [21].Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation, 1996. Italian version: Ghisi M, Flebus GB, Montano A, Sanavio E, Sica C. O.S. Firenze; 2006. [Google Scholar]
- [22].Stata Corporation. Stata Reference Manual. Release 10.1. TX, USA: College Station; 2007. [Google Scholar]
- [23].Donati S, Andreozzi S, Grandolfo ME. Evaluation of support and information for pregnant women: national survey. Istituto Superiore di sanità; 2001. (Rapporti ISTISAN 01/5: 20). [Google Scholar]
- [24].Gagnon AJ, Sandall J. Individual or group antenatal education for childbirth or parenthood, or both. Cochrane Database Syst Rev 2007. CD002869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Schrader McMillian A, Barlow J, Redshaw M. Birth and Beyond: A Review of the Evidence About Antenatal Education. London: Department of Health; 2009. [Google Scholar]
- [26].Maimburg RD, Vaeth M, Durr J, et al. Randomised trial of structured antenatal training sessions to improve the birth process. BJOG 2010;117:921–8. [DOI] [PubMed] [Google Scholar]
- [27].Ferguson S, Davis D, Browne J. Does antenatal education affect labour and birth? A structured review of the literature. Women Birth 2013;26:e5–8. [DOI] [PubMed] [Google Scholar]
- [28].Doyle O, McGlanaghy E, Palamaro-Munsell E, et al. Home based educational intervention to improve perinatal outcomes for a disadvantaged community: a randomised control trial. Eur J Obstet Gynecol Reprod Biol 2014;180:162–7. [DOI] [PubMed] [Google Scholar]
- [29].Miller YD, Prosser SJ, Thompson R. Back to normal: a retrospective, cross- sectional study of the multi-factorial determinants of normal birth in Queens- land, Australia. Midwifery 2015;31:818–27. [DOI] [PubMed] [Google Scholar]


