Abstract
Older adolescents with attention-deficit/hyperactivity disorder (ADHD) have a significantly increased likelihood of developing comorbid depression. It is important to evaluate factors during the early adolescent period that may contribute to this risk. A predominant theory is that impairment and failure experiences lead to the development of low-self efficacy and depression, and that parent and family factors also play a role. In a sample of 326 young adolescents with ADHD (Mage = 12), the present study evaluated whether parent-adolescent conflict mediated the association between social and academic impairment and the development of depression. This study builds upon prior work by evaluating these associations longitudinally and by using a multi-rater approach, including the parent, adolescent, and teacher perspectives. Social and academic impairment directly predicted depression controlling for baseline levels of depression and change in ADHD symptoms. The association between social impairment and depression was partially mediated by parent-adolescent conflict. Mediation through conflict was not found for academic impairment, and the association between academic impairment and depression was no longer significant when accounting for conflict. These findings highlight the importance of social impairment in the development of depression in adolescents with ADHD. Caregivers may play an important role in determining whether adolescents with ADHD internalize social impairment and failure experiences and develop depressive symptoms. Implications of these findings in terms of the importance of interventions focused on parent-adolescent conflict are discussed.
Keywords: ADHD, Depression, Adolescence, Impairment, Parent-Child Conflict
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a chronic mental health condition that persists into adolescence in the majority of cases (Copeland et al., 2013). Adolescents with ADHD are at greater risk for the development of depressive disorders in comparison to their non-ADHD peers (Eberhart & Hammen, 2006; Sheeber, Hops, Alpert, Davis, & Andrews, 1997). Overall, depression occurs 5.5 times more frequently among individuals with ADHD, with prevalence rates for comorbid depression with ADHD ranging from 12% – 50% (Angold, Costello, & Erkanli, 1999; Birmaher et al., 1996). Adolescents with ADHD and depression display significantly higher rates of social and academic impairment compared to youth with ADHD alone (Blackman, Ostrander, & Herman, 2005; Karustis, Power, Rescorla, Eiraldi, & Gallagher, 2000). Further, adolescent females with ADHD and depression exhibit a greater risk for suicidality compared to their non-ADHD depressed peers and are more likely to require psychiatric hospitalization (Biederman et al., 2008). Accordingly, it is important to understand the factors that lead to the development of depression in adolescents with ADHD.
Several theoretical models outline potential causal pathways for the association between ADHD and depression (e.g., Roy et al., 2014). The Dual Failure (D.F.) and Cognitive-Behavioral (C.B.) models both posit that the ADHD-depression association is indirect, mediated through functional impairment (Patterson & Stoolmiller, 1991; Safren, Sprich, Chulvick & Otto, 2004). Youth with ADHD experience significant impairment in a variety of domains, including academic and interpersonal functioning (DuPaul & Langberg, 2015; Hoza et al., 2005). Academically, youth with ADHD receive poorer grades and are more likely to drop out of school in comparison to their peers (Kent et al., 2011). Interpersonally, youth with ADHD exhibit poorer social skills and have fewer friends (Hoza et al., 2005). The D.F. and C.B. models suggest that over time, these impairments are perceived as repeated failure experiences, and lead to the development of negative thought patterns, low self-concept, and symptoms of depression. Eddy et al. (2015) recently found empirical support for these models in a sample of college students with ADHD (N =59; 54.2% male), with academic impairment leading to a negative self-concept and the development of depressive symptoms. The fact that depressive disorders typically develop several years after the onset of ADHD (Daviss, 2008), also supports the assertion that impairment experiences may accumulate over time and lead to depressive symptoms.
To date, findings have been mixed regarding which aspects of functional impairment are most salient in the development of comorbid depression. Some studies suggest that both academic and interpersonal impairment are important mediators (e.g., Herman et al., 2007), while others find that only interpersonal impairment leads to depression (Biederman et al., 2008; Humphreys et al., 2013). In an elementary-school-aged sample (N = 426; 49.3% male), Herman et al. (2007) found that academic competence mediated the relationship between teacher-reported inattention and the development of depressive symptoms two years later. Conversely, Humphreys et al. (2013) found that interpersonal functioning and parent-child conflict, but not academic functioning, mediated the association between ADHD and depressive symptoms in a general education elementary aged sample. The Humphreys et al. study included two separate samples; a cross-sectional sample including participants with (n = 120) and without (n = 110) ADHD (overall sample = 71% male), and a sample of youth at risk for depression followed from age 5 through 20 (N = 472; 44% male). Interestingly, in both studies, parent-child problems mediated the association between ADHD and depression above and beyond impairment in peer relationships and academic functioning.
Family relationship impairment is associated with depression in adolescents (O’Shea, Spence, & Donovan, 2014). Findings from studies with typically developing youth demonstrate that conflict in the parent-child relationship longitudinally predicts depression (Sheeber, Hups, Alpert, Davis, & Andrews, 1997; Brière, Archambault, & Janosz, 2013). Moreover, some research suggests that this relationship may be reciprocal, with conflict predicting depression, in turn leading to additional conflict (Brière et al., 2013). While minimal research has evaluated the association between conflict and depression in ADHD samples, it is clear that families with a child with ADHD experience high levels of conflict (e.g., Johnston & Mash, 2001). This conflict may stem from the fact that youth with ADHD are forgetful, require multiple reminders to carry out parental instructions, frequently procrastinate, and fail to comply with requests and commands (Evans et al., 2009; Raggi & Chronis, 2006). Conflict may also stem from disagreements surrounding academic and social functioning. For example, adolescents with ADHD may experience conflict with their caregivers over low or failing test grades, missed homework, or failure to complete academic tasks (Power et al., 2006). Similarly, non-compliance and acting out in the classroom or with peers can lead to negative teacher behavioral reports, which result in parental frustration and parent-adolescent conflict.
Interestingly, conflict has been shown to peak during adolescence (Allison & Schultz, 2004), around the same time that symptoms of comorbid depression often emerge. As noted by Humphreys et al. (2013), frequent parent-adolescent conflict may lead youth to feel unsupported by their caregivers. Lack of social support, particularly within the parent-adolescent relationship, is an important risk factor for depression (Cornwell, 2003). Conversely, parent engagement, a construct defined by the parent’s willingness and ability to support and be involved in their child’s educational and socioemotional progress and development (El Nokali, Bachman, & Votruba-Drzal, 2010), is related to multiple positive youth outcomes. For instance, parent engagement and involvement is associated with higher levels of academic achievement (Jeynes, 2005; Wilder, 2014), academic motivation (Fan & Williams, 2010; Gonzalez-DeHass, Willems, & Holbein, 2005), and more positive social-emotional outcomes (Shumow & Lomax, 2002). Given these findings, it is clear that the parent-adolescent relationship is important during adolescence.
Multiple methodological limitations assciated with prior research have prevented firm conclusions from being drawn about whether impairment in academic or interpersonal functioning directly leads to the development of depression, or if this association is indirect, through parent-adolescent conflict. First, the only study to date that evaluated multiple aspects of impairment within an ADHD sample (Humphreys et al., 2013), evaluated associations cross-sectionally, and as such, it is equally plausible that depression was leading to impairment and conflict. Second, the majority of studies evaluating pathways to depression in youth with ADHD have been single source (e.g., all parent ratings), and have relied on parent-report of youth internalizing symptoms, despite the fact that self-report is considered best practice in adolescence (Moretti, Fine, Haley, & Marriage, 1985). Third, prior studies have largely focused on younger populations, (e.g., elementary-school-aged children; Blackman et al., 2005, Humphreys et al., 2013), or adult populations (Biederman et al., 2008; Eddy et al., 2015). As the transition into adolescence is a critical period for the emergence of depression (e.g., Rutter, Graham, Chadwick, & Yule, 1976), it is important to study factors leading to depressive symptoms in adolescents with ADHD. Finally, as noted in Humphreys et al. (2013), prior studies use of standardized test performance to capture academic impairment may not be ecologically valid, as the academic impairment of youth with ADHD often centers around failure to complete work, lack of preparation for tests, classroom disruptions, and failure to bring materials to class.
The present study sought to address these limitations in a longitudinal sample of young adolescents comprehensively diagnosed with ADHD. In particular, the present study incorporates parent, adolescent, and teacher ratings to protect against within-source bias, and includes a well-validated self-report measure of depressive symptoms. Further, composite variables with multiple raters were used to more fully capture the social and academic domains of functioning. The main aims of the study were to evaluate whether academic and social impairment longitudinally predict the development of depression and whether these associations are mediated by parent-adolescent conflict. In addition, the role of gender as a moderator of the association between conflict and depression was also evaluated. It was predicted that both social and academic functioning would predict the development of depressive symptoms above and beyond baselines levels of depressive symtpoms and change in ADHD symtpoms. Second, given the importance of parent-child problems as demonstrated in Humphreys et al. (2013), it was predicted that parent-adolescent conflict would mediate associations between academic and social functioning and depression. Finally, given the established associations between gender and depression (e.g., Nolen-Hoeksema & Girgus, 1994; Rutter, 1986), it was predicted that gender would moderate the relationship between conflict and depression.
Method
Participants
Participants included 326 middle-school students ages ten to fourteen at baseline (Mage = 12.26, SD = .92 years) diagnosed with ADHD. Participants were recruited over three consecutive academic years as part of a school-based randomized controlled intervention study. Seventy percent of participants were male and 77.8% identified themselves as Caucasian, 11.6% African American, 8.4% Biracial, 1.8% another race, and 1 participant chose not to respond. Forty-five percent of the sample was taking medication for ADHD. Mean family income was $55,532 (SD = 46,925).
Procedure
The study was conducted at two sites and procedures were approved by both university Institutional Review Boards (IRBs); parents provided signed consent and adolescents provided signed assent. A two-step assessment strategy was used to determine eligibility. Participants were recruited by way of study announcement letters, flyers, and direct referrals from school staff. Interested parents who contacted study personnel were provided with a comprehensive description of the study. Parents were also asked to complete an eligibility screen regarding their children; those who endorsed the presence of at least four of nine DSM-IV-TR symptoms of inattention and/or a prior diagnosis of ADHD were scheduled for an evaluation to assess eligibility. Children were eligible to participate in the study if they (a) attended a participating school; (b) met full DSM-IV-TR diagnostic criteria for ADHD-Predominantly Inattentive Type or ADHD-Combined Type on Children’s Interview for Psychiatric Syndromes – Parent Version (P-ChIPS; Weller, Weller, Fristad, Rooney, & Schecter, 2000) or combined with teacher-reported symptoms on the Disruptive Behavior Disorders Rating Scale (DBD; Van Eck, Finney, & Evans, 2010); (c) had clinically significant impairment due to ADHD symptoms on the parent or teacher versions of the Impairment Rating Scale (IRS; scores ≥ 3 demonstrate impairment; Fabiano et al., 2006); and (d) had an estimated IQ of at least 80 as assessed using the Wechsler Intelligence Scale for Children – Fourth Edition (WISC-IV; Wechsler, 2003). Children were ineligible if they had a pervasive developmental disorder or met diagnostic criteria for bipolar disorder, psychosis, or obsessive-compulsive disorder on the P-ChIPS. Two doctoral-level psychologists reviewed assessment data to determine eligibility status and diagnoses. The P-ChIPS (Weller et al., 2000) is a structured parent interview assessing the presence of symptoms of 20 disorders in children and adolescents based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR; American Psychological Association, 2000). The P-ChIPS demonstrates adequate psychometric properties (Weller et al., 2000). At baseline, 51% percent of the sample met DSM-IV criteria for ADHD – Inattentive Type and 49% for Combined Type. In addition, 53.4% of the participants met criteria for ODD and 12.2% for CD, 27% met criteria for an anxiety disorder, and 13% met criteria for a depressive disorder.
Eligible participants were randomly assigned to one of three treatment conditions and received the intervention over the course of one academic year. The first treatment condition (Challenging Horizons Program, After School; CHP-AS) was a school-based intervention that was delivered as an afterschool program. CHP-AS targeted organization, planning, study skills, and personal social goals, through a mix of group and individual meetings. The second treatment condition (Challenging Horizons Program, Mentoring; CHP-M) involved the delivery of the subset of CHP interventions via weekly individual meetings at the participants’ school with a teacher or other staff member (i.e., a mentor) that was supervised by study staff. The third condition (community control; CC) received no intervention, but was provided with an evaluation report and a list of resources in the community. For additional information about the study design and treatment conditions see Evans et al. (2016). Participants completed the measures described below at the baseline visit (Time 1; T1), 9 months following baseline (Time 2; T2) and again 18-months post-baseline (Time 3; T3).
Measures
ADHD symptoms
The Disruptive Behavior Disorders Rating Scale (DBD; Van Eck, et al., 2010), is a 45-item parent-rated rating scale used to assess symptoms of ADHD, oppositional defiant disorder (ODD), and conduct disorder (CD) using a 4-point Likert scale. The DBD items adhere closely to the diagnostic criteria for ADHD included in the Diagnostic and Statistical Manual of Mental Health Disorders – Fourth Edition (DSM-IV). Higher scores on the DBD indicate greater symptomatology. The scale has been validated for use with young adolescents (Van Eck et al., 2010) and has demonstrated evidence for internal consistency in this population (α = .96; α = .95, and α = .75 for ADHD, ODD, and CD scales, respectively). The DBD demonstrated evidence for adequate internal consistency in the present sample (α = .88, α = .89 for inattentive and hyperactive/impulsive symptom scales, respectively). For the present study, an ADHD total score was calculated by summing the responses from the 9 inattentive items and the 9 hyperactive/impulsive items. This total score was included in the models to account for the influence of ADHD symptoms over time on depressive symptoms.
Depressive symptoms
The Reynolds Adolescent Depression Scale, 2nd Edition (RADS-2; Reynolds, 2002) is a 30-item self-report measure which assesses the cognitive, behavioral, and somatic symptoms associated with depression. The RADS-2 yields a total score as well as four subscale scores: Dysphoric Mood, Anhedonia/Negative Affect, Negative Self-Evaluation, and Somatic Complaints. Adolescents are prompted to rate how often a given depressive symptom occurs from 1 (almost never) to 4 (most of the time). Higher scores indicate higher levels of depressive symptoms. The RADS-2 has been normed on a large sample of adolescents and has demonstrated adequate reliability and validity (Reynolds, 1987). For the present study, the RADS-2 Total Score was used from T3. Internal consistency in the present sample at T3 was adequate (α =.87).
Parent-Adolescent conflict
The Conflict Behavior Questionnaire (CBQ; Prinz, Foster, Kent, & O’Leary, 1979) is a measure of conflict in the parent-adolescent relationship, which incorporates responses from both parents and adolescents. The present study used the short form (Robin & Foster, 1989), which consists of 20 dichotomous items describing potential characteristics of the parent-adolescent relationship (e.g., “the talks we have are frustrating”). Parents and adolescents complete separate forms and indicate whether items are “true” or “false” with regard to their relationship. An overall conflict score is calculated by summing both parent and adolescent responses (true = 1; false = 0). Higher scores indicate more severe levels of conflict. The CBQ is a widely used measure of conflict and has been found to have adequate psychometric properties (e.g., Kane & Garber, 2009). For example, distressed families score significantly higher on the CBQ relative to non-distressed families (Robin & Foster, 1989). In the present study, T2 CBQ scores were used as a measure of parent-adolescent conflict in the analyses. Internal consistency for the parent and adolescent versions of the CBQ at T2 was adequate (α = .89 and α = .92, respectively) in this sample.
Social impairment
A social impairment composite score was created by combining parent and adolescent subscale scores from the Social Skills Improvement System (SSIS; Gresham & Elliott, 2008). The SSIS is a 75-item self- and parent-report measure that assesses social skills and problem behaviors. This measure has strong psychometric properties with internal consistencies of .95 and .96 for self-report and parent-report versions, respectively. (Gresham, Elliott, Vance, & Cook, 2011). The present study used the Social Skills subscale, which is comprised of 46 items that cover seven domains of social skills: communication, cooperation, assertion, responsibility, empathy, engagement, and self-control (Gresham & Elliott, 2008). Each item on the SSIS consists of two parts. On the self-report, respondents first decide how true the statement is for them on a four-point scale from not true to very true and then how important the statement is on a three-point scale from not important to critical. On the parent-rated SSIS, parents first rate how often their child has displayed a behavior in the past two months on a four-point scale from never to almost always and then rate how important the same behavior is to their child’s development on a three-point scale from not important to critical. Lower scores indiciate more severe levels of impairment in the social functioning domain. In the current study, a composite Social Skills subscale score was created by combining parent and adolescent ratings. For the current study, SSIS scores at T1 were included in the analyses. The composite score displayed evidence for strong internal consistency (α = .94 and α = .95 for parent- and self-report, respectively).
Academic impairment
A measure of academic impairment was created by combining teacher report and parent report of school-related impairment. One teacher-rated item from the Impairment Rating Scale (IRS; Fabiano et al., 2006) was used in combination with the school impairment domain of the Weiss Functional Impairment Rating Scale – Parent Report (WFIRS-P; Weiss, Wasdell, & Bomben, 2004). Higher scores indicate higher levels of impairment.
Teacher report
The Impairment Rating Scale (IRS; Fabiano et al., 2006) is a measure of functional impairment specifically developed for youth with ADHD. Informants are asked to rate items on a scale by marking an “X” on a line signifying a continuum of impairment ranging from 0 (no problem) to 6 (extreme problem). The current study included the academic impairment item (“How this child’s problems affect his or her academic progress” Fabiano, et al., 2006) from the teacher version of the IRS completed at T1. This item has demonstrated discriminant and convergent validity when compared to academic achievement testing and other measures of academic functioning in the school setting and has been found to effectively distinguish between youth with and without ADHD (Fabiano, et al., 2006).
Parent report
The Weiss Functional Impairment Rating Scale – Parent Report (WFIRS-P; Weiss, Wasdell, & Bomben, 2004) is a broad measure of parent-rated impairment consisting of six domains. Parents are asked to rate on a 4-point scale (0 = never, 3 = very often) the extent to which their child’s emotional/behavioral problems have affected each area of functioning. The present study used the 10-item School Impairment subscale, which evaluated impairment related to two domains, learning and behavior, and was completed at T1. Internal consistency for the T1 WFIRS school impairment score was adequate (α = .84). The WFIRS has adequate psychometric properties when used in other adolescent ADHD samples, with an internal consistency of .83 and test-re-test reliabilities ranging from .84 to .86 for the school domain. (Gajria et al., 2015).
Data Analyses
Composite scores were created to include both the parent and adolescent perspective for conflict and social impairment and the parent and teacher perspective for academic impairment. Specifically, consistent with past research in this area (Ostrander & Herman, 2006), scores for each measure were standardized and then summed to create the composite variables which ensures that the outcome variable (depression) is not differentially influenced by source variance. Furthermore, composite variables are a clinically meaningful way to capture multifaceted concepts such as academic and social impairment which may be perceived differently by parents, teachers, and the adolescent themselves (Grace & Bollen, 2008) and statistically efficient and appropriate given normality of data and associations between the variables being combined (Song, Lin, Ward, & Fine, 2013). The composite score for the conflict variable had an α of .92 and item to total correlations ranged from .31 to .60 (M = .47, SD = .10). The composite academic impairment variable had an α of .84 and item to total correlations ranged from .37 to .70 (M = .59, SD = .09). Lastly, the composite social impairment variable had an α of .94 and item to total correlations ranged from .10 to .62 (M = .42, SD = .10). Finally, in order to control for the change in ADHD symptoms over time, a change score was calculated by subtracting the ADHD total score at T3 from the ADHD total score at T1.
Bivariate correlation analyses were conducted using the composite variables to evaluate associations between academic impairment, social impairment, parent-adolescent conflict, and depressive symptoms. Next, separate hierarchical regressions were conducted between each independent variable (i.e., social and academic impairment) and the dependent variable (i.e., adolescent depression), controlling for baseline levels of depressive symptoms and the change in ADHD symptoms across time. Finally, separate mediation analyses were conducted using composite variables to evaluate the extent to which the parent-adolescent conflict composite variable mediated the relationship between social and academic impairment and depression. Last, gender was examined as a moderator of the relationship between conflict and depression.in both the social and academic models. All analyses were conducted using Model 4 for mediation and Model 14 for moderated mediation with 10,000 bootstraps in the PROCESS macro version 2.15 (Hayes, 2016) in SPSS 23.0 (SPSS, IBM, version 23.0). All model variables were also assessed for normality and all fell within a normal range. Means, standard deviations, and skew of variables are presented in Table 1. Finally, missing data was analyzed using Little’s MCAR to test whether data was missing at random based on key demographic variables (race and ethnicity, SES, and gender) and model variables. Results indicated the data was indeed missing at random (χ2 = 16.025, df = 23; p = .854). To account for missing data due to study attrition (approximately 10% missing at T2 and T3) last observation carried forward (LOCF) was used. LOCF is appropriate when longitudinal values are available before the missing value (Engels & Diehr, 2003). Analyses were run with and without the LOCF and the results did not differ. LOCF could not be used for six cases where data for a variable was missing at baseline. Accordingly, those six cases were removed from analyses and the N for all analyses reported below is 320.
Table 1.
Means, Standard Deviations, and Skewness and Kurtosis of model variables
| Measure | N | M | SD | Skewness | Kurtosis | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Statistic | S.E | Statistic | S.E | ||||
| Depression T1 | 320 | 44.51 | 9.23 | 0.87 | 0.14 | 0.27 | 0.27 |
| Depression T3 | 320 | 45.14 | 10.33 | 0.95 | 0.14 | 0.45 | 0.27 |
| ADHD T1 | 320 | 30.53 | 10.62 | −0.15 | 0.14 | −0.52 | 0.27 |
| ADHD T3 | 320 | 22.08 | 11.59 | 0.33 | 0.14 | −0.36 | 0.27 |
| Conflict T1 | 320 | 50.02 | 8.13 | 0.97 | 0.14 | 1.01 | 0.27 |
| Conflict T2 | 320 | 50.12 | 8.38 | 0.96 | 0.14 | 0.69 | 0.27 |
| Social Impairment T1 | 320 | 50.01 | 8.07 | −0.23 | 0.14 | −0.22 | 0.27 |
| Academic Impairment T1 | 320 | 50.14 | 8.55 | 0.08 | 0.14 | −0.08 | 0.27 |
Results
Prior to running analyses, we assessed whether intervention condition was significantly related to any variables of interest. No significant differences on parent or adolescent interpersonal and family variables were found in similar analyses using the same dataset by Bunford et al. (2015). However, to confirm the lack of intervention condition effects for the present study, a multivariate analysis of variance (MANOVA) was conducted at each time point (i.e., T1, T2, and T3) to evaluate whether the three groups (CHP-AS, CHP-M, and CC) differed on the variables of interest. Analyses indicated no significant differences at T1 (F(8, 630) = .940, p = .483) for any of the predictor variables (i.e., symptoms of depression, academic impairment, and social impairment), at T2 (F(2, 268) = 0.902, p = .407) for the mediator variable (i.e., parent-adolescent conflict), or at T3 (F(4, 456) = 1.433, p = .222) for the outcome variable of interest (i.e., symptoms of depression). To safeguard against any potential treatment effects, condition was still included as a covariate in the models.
Bivariate correlations between model variables are presented in Table 2. The mediator variable, parent-adolescent conflict at T2, was significantly positively correlated with both ADHD at T1 and depression at T3. Social impairment (lower scores = more impairment), was negatively correlated with ADHD symptoms at T1 and T3, parent-adolescent conflict at T2, as well as the outcome variable, depression, at T3. Academic impairment (higher scores = more impairment), was positively correlated with ADHD symptoms at T1 and T3, parent-adolescent conflict at T2, and depression at T3.
Table 2.
Correlations Between Model Variables
| Variable | ADHD T3 | Social Impairment T1 | Academic Impairment T1 | Parent- Adolescent Conflict T1 | Parent- Adolescent Conflict T2 | Depression T1 | Depression T3 |
|---|---|---|---|---|---|---|---|
| ADHD T1 | .521** | −.150** | .335** | .253** | .260** | −0.017 | 0.007 |
| ADHD T3 | -- | −.173** | .208** | .213** | .296** | −0.027 | 0.139* |
| Social Impairment T1 | -- | −.288** | −.455** | −.402** | −.309** | −.333** | |
| Academic Impairment T1 | -- | .128* | .132* | 0.051 | .117* | ||
| Parent-Adolescent Conflict T1 | -- | .773** | .389** | .311** | |||
| Parent-Adolescent Conflict T2 | -- | .193** | .326** | ||||
| Depression T1 | -- | .511** |
Notes.
Correlation is significant at the 0.01 level.
Correlation is significant at the 0.05 level.
All tests are two-tailed.
Next, hierarchical regressions revealed that social impairment at T1 significantly predicted adolescent-reported depression at T3 above and beyond baseline depressive symptoms, treatment condition, and the change in ADHD symptoms from T1 to T3, F(4, 315) = 36.07, p < .001. The addition of social impairment at T1 significantly improved prediction of depression at T3, ΔR2=.03, ΔF = 14.41, p < .001. Similarly, academic impairment at T1 predicted depression at T3 beyond baseline levels of depressive symptoms, treatment condition, and the change in ADHD symptoms, F(4, 315) = 32.80, p = < .001. The addition of academic impairment at T1 significant improved prediction of depression at T3, ΔR2=.01, ΔF = 5.05, p = .03.
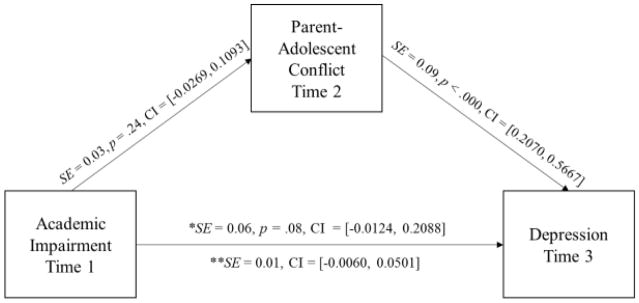
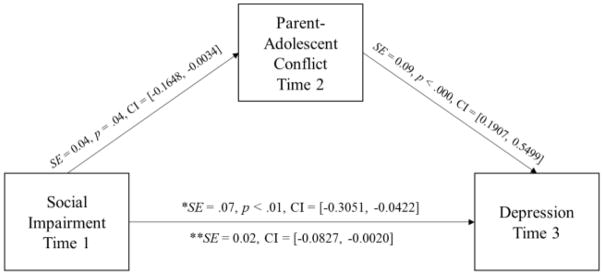
Two separate analyses were run with the T1 RADS-2 total score, ADHD change score, conflict and depression symptoms at T1, and intervention status included as covariates. First, the direct and indirect effects of academic impairment at T1 on depression at T3 via parent-adolescent conflict at T2 were examined (see Figure 1). The overall model was significant (c = 0.11, SE = 0.06, 95% CI [0.0009, 0.2274]). Although significant in the regressions, the direct effect of academic impairment on depression was not significant (c′ = 0.10, SE = 0.06, 95% CI [−0.0124, 0.2088]) in the full model with parent-adolesent conflict, nor was the indirect effect through conflict (ab = 0.02, SE = 0.01, 95% CI [−0.0060, 0.0501]). Next, the direct and indirect effects of social impairment at T1 on depression at T3 via parent-adolescent conflict at T2 were tested (see Figure 2). The overall model was significant (c = −0.20, SE = 0.07, 95% CI [−0.3385, −0.0711]). The direct effect of social impairment on depression was significant (c′ = −0.17, SE = 0.07, 95% CI [−0.3051, −0.0422]), and the indirect effect was also significant (ab = −0.03, SE = 0.02, 95% CI [−0.0827, −0.0020]), indicating that the relationship between social impairment and the later development of depression can be partially explained by the indirect effect through parent-adolescent conflict, over and above levels of depression symptoms at T1, conflict at T1, change in ADHD symptoms, and treatment condition. In this model, the indirect effect of parent-adolescent conflict accounted for 15% of the total effect of social impairment on depression.
Figure 1.
Parent-Adolescent Conflict does not mediate the relationship between Academic Impairment and Depression, All confidence intervals 95%. *lndicates direct effect **Indicates indirect effect via Parent-Adolescent Conflict. Model includes Depression atTl, Parent-Adolescent Conflict at Time 1, change in ADHD from Time I to Time 3. and intervention status as covariates.
Figure 2.
Parent-Adolescent Conflict partially mediates the relationship between Social Impairment and Depression. All confidence intervals 95%, *Indicates direct effect **Indicates indirect effect via Parent-Adolescent Conflict. Model includes Depression at T1, Parent-Adolescent Conflict at Time 1, change in ADHD from Time 1 to Time 3, and intervention status as covariatcs.
Last, a moderated mediation was conducted to assess whether gender moderated the indirect effects of impairment to depression through parent-adolescent conflict. Gender did not moderate the relationship between parent-adolescent conflict and depression in either the academic impairment mediation model (point estimate = −0.0066, SE = 0.009, 95% CI [−0.0356, 0.0031]) or the social impairment mediation model (point estimate = 0.0099, SE = 0.0142, 95% CI [−0.0069, 0.0524]).
Discussion
This study longitudinally evaluated predictors of depression and mediators of the association between impairment and depression in a large sample of young adolescents with ADHD. Similar to prior research with elementary-aged children with ADHD (Herman et al., 2007; Humphreys et al., 2013), impairment in social and academic functioning predicted depression. Interestingly, the link between social impairment, but not academic impairment, and later depression was partially mediated by parent-adolescent conflict. These findings held true while controlling for baseline levels of depression and conflict, treatment condition, and change in ADHD symptoms over time. Finally, the moderated mediation analyses were not significant, suggesting that the associations did not differ for boys and girls. Importantly, these findings build upon prior work because the data were longitudinal and included multiple sources (e.g., parents, adolescents, and teachers) in rating academic and social functioning and parent-adolescent conflict. The present study highlights the important role parents play in helping young adolescents with ADHD cope with social impairment, potentially reducing the likelihood of developing depressive symptoms.
Overall, these findings are consistent with interpersonal models of depression which suggest that interpersonal impairment, such as lack of social support and conflict with parents, plays a unique role in the development of depression (Rueger, et al, 2016; Haggerty & Williams, 1999). Consistent with previous findings (e.g., Eddy et al., 2015) the longitudinal association between academic impairment and depression was signifciant in the regression model. However, this association was no longer significant in the mediation model with parent-adolescent conflict included (see Figure 1), supporting the assertion that interpersonal factors play the most prominent role in the development of depression. Another possibility is that the adolescents’ self-perception of their functioning matters most in terms of predicting depression. In this study, parent and adolescent ratings were utilizied for social functioning but the parent and teacher perspective was emphasized for assessment of academic impairment. Future research could examine whether adolescent’s self-perception of academic impairment leads to parent-adolescent conflict and depressive symptoms. Overall, given the role of parent-child conflict found in the Humphreys et al. (2013) study in elementary age youth with ADHD and in the present sample of adolescents with ADHD, there are a number of important clinical implications.
Interventions focused on improving the functioning of adolescents with ADHD do not always target parent-adolescent communication and conflict (see Sibley, et al., 2016 for an exception). This is because many of these interventions are school-based and: (1) schools often do not have the time, resources, or expertise to actively engage parents in intervention (Eccles & Harold, 1993), (2) even when resources are in place, families can be difficult to engage (Vanderbleek, 2004). For similar reasons, most interpersonal skills interventions for youth with ADHD focus on teaching social skills and on improving the child’s peer relationships, and do not emphasize the parent-child relationship or conflict (Antshel & Remer, 2003; Mikami, Jia, & Na, 2014; Sheridan, et al., 1996). However, in non-ADHD samples, adolescents’ social functioning is positively associated with parent engagement in school and extracurricular activities (Shumow & Lomax, 2002). In contrast, parent-school contact regarding teacher-reported behavior problems is negatively associated with student engagement and intrinsic motivation (Fan & Williams, 2010). This relationship is likely explained by increased parent-child conflict following these home-school communications. As such, it may be that interpersonal skills interventions for adolescents with ADHD should focus not only on teaching social skills, but also on improving the parent-adolescent relationship and how the parent can provide the adolescent with interpersonal support. Perhaps if parents can learn strategies to help adolescents with ADHD cope with social impairments, they can serve as a buffer against the development of depression.
This study builds on previous research in several important ways. First, this study used a longitudinal design to evaluate mediation and moderated mediation, whereas prior research in ADHD samples used cross-sectional designs. In addition, previous research evaluated symptoms of depression from the parent perspective, and the current study evaluated symptoms of depression using a well-validated measure completed by the adolescents, which is consistent with best-practice recommendations that self-report is ideal for internalizing symptoms (Silverman & Ollendick, 2005). Lastly, the present study created composite variables including multiple reporters to assess levels of academic and social impairment as well as parent-adolescent conflict. This approach significantly reduces the possibility that our findings are attributed to within-source shared-variance. However, there are also some important limitations that should be noted.
The rating used for social impairment was skills based (SSIS) and thus incorporated some aspects of social impairment, this may not capture qualitative information that reflects impairment in the peer domain (i.e., depth and quality of friendships). For example, using peer informants (i.e., sociometric ratings) or arguably more “objective” ratings of social impairment, such as number of friends or time spent with peers, would add a richer understanding of the impact both ADHD and depressive symptoms have on social functioning. The use of composite variables, while having advantages, can present challenges for interpretation. Research has shown that combining raters may, in some cases, diminish any one raters’ point of view, however it can make models more parsimonious (Song, et al., 2013). As part of the composite variables, this study chose to incorporate teacher ratings which has its own set of challenges in the middle school setting given that teachers may not have the same operational definitions of behaviors being rated and may be subject to biases (e.g., Kofler, et al., 2010; Youngstrom, Loeber, & Stouthamer-Loeber, 2000). Further, teacher-rated academic impairment was based upon a single item, which may not sufficiently capture the multidimensional nature of academic impairment. The present study was also not able to consider differences between ADHD-Combined presentation and ADHD-Inattentive presentation, although important distinctions in terms of impairments and outcomes have been found between the two (Gaub & Carlson, 1997). Another consideration may be the change in depressive symptoms between T1 and T2 which was not modeled; this change may have influenced conflict at T2. It would also be important to extend these findings into older and more diverse adolescent samples. Parent-adolescent conflict may appear different in other cultures and classes (Dixon, Graber, & Brooks-Gunn, 2008). Lastly, the amount of missing data in this sample may also be considered a limitation. Choosing to handle missing data through LOCF may have attenuated the findings from this study as it can raise the potential rate of type I error (Cook, Zeng, & Yi, 2004). This method may have decreased variance at T2 and T3 as it is not sensitive to the natural trajectory of participants (Streiner, 2008).
Future Directions
Future research may want to consider a wider or different definition of conflict. In this study, conflict was defined as within the parent-adolescent relationship. However, given the extent to which symptoms of ADHD may be impairing in multiple settings (e.g., home, school, peers), and the fact that the interpersonal theory of depression suggests that relationships with peers affects the development of depression, future research could explore how conflict with peers and teachers may also be associated with the development of depression. This would have important implications for intervention, especially in those cases where engaging parents is not feasible. It may be that like parents, teachers can serve as a buffer between academic and social impairment and depression by helping students feel supported even when they struggle. Similarly, it could be important to measure the parent-adolescent relationship more broadly, and to assess social support and parent-adolescent communication in addition to conflict. Further, during the adolescent period, conflict occurs to some extent in many homes. Measuring changes in conflict on a day-to-day basis may provide clinically useful information to inform treatment.
Overall, findings from the current study suggest that interpersonal impairment is an important factor in explaining the development of comorbid depression in adolescents with ADHD. Our findings support the need for interventions focused on adolescents with ADHD to address parent-adolescent communication patterns and to provide parents with strategies to communicate more effectively surrounding academic and interpersonal concerns. Ideally, a prevention approach would be taken, so that caregivers of children with ADHD are adequately prepared to help them cope with failure experiences prior to the adolescent period, when impairments often increase in frequency and severity. Additional research is needed to evaluate the efficacy of bolstering existing school-based interventions with relationship skills training (i.e., parent-adolescent communication) in an effort to thwart the development of depression in adolescents with ADHD.
Acknowledgments
This research was supported by a grant to the second and last authors from the National Institute of Mental Health (NIMH; R01MH082865).
Footnotes
None of the authors have any actual or potential conflicts of interest to disclose.
Author Contributions
HME: developed the hypotheses, analyzed data, and directed the writing of the manuscript. EB: assisted with data analyses and writing of paper. JL: co-designed and directed the study and supervised analyses, writing, and editing of the manuscript. LE: assisted in writing and editing the manuscript. LO: assisted with writing and editing. SM: assisted with data analyses. SWE: co-designed and directed the study and assisted with manuscript edits.
Compliance with Ethical Standards
This study was funded by a grant to the third and last authors from National Institute of Mental Health (NIMH; R01MH082865). All study procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Contributor Information
Hana-May Eadeh, Virginia Commonwealth University.
Elizaveta Bourchtein, Virginia Commonwealth University.
Joshua M. Langberg, Virginia Commonwealth University
Laura D. Eddy, Virginia Commonwealth University
Lauren Oddo, Virginia Commonwealth University.
Stephen J. Molitor, Virginia Commonwealth University
Steven W. Evans, Ohio University
References
- Allison BN, Schultz JB. Parent-adolescent conflict in early adolescence. Adolescence. 2004;39:101–119. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington DC: Author; 2000. text rev. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Antshel KM, Remer R. Social skills training in children with attention deficit hyperactivity disorder: a randomized-controlled clinical trial. Journal of Clinical Child and Adolescent Psychology. 2003;32:153–165. doi: 10.1207/S15374424JCCP3201_14. [DOI] [PubMed] [Google Scholar]
- Biederman J, Ball SW, Monuteaux MC, Mick E, Spencer TJ, McCreary M, … Faraone SV. New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:426–434. doi: 10.1097/CHI.0b013e31816429d3. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, … Nelson B. Childhood and adolescent depression: a review of the past 10 years. Part I. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Blackman GL, Ostrander R, Herman KC. Children with ADHD and depression: a multisource, multimethod assessment of clinical, social, and academic functioning. Journal of Attention Disorders. 2005;8:195–207. doi: 10.1177/1087054705278777. [DOI] [PubMed] [Google Scholar]
- Brière FN, Archambault K, Janosz M. Reciprocal prospective associations between depressive symptoms and perceived relationship with parents in early adolescence. The Canadian Journal of Psychiatry/La Revue Canadienne De Psychiatrie. 2013;58:169–176. doi: 10.1177/070674371305800307. [DOI] [PubMed] [Google Scholar]
- Bunford N, Evans SW, Becker SP, Langberg JM. Attention-deficit/hyperactivity disorder and social skills in youth: A moderated mediation model of emotion dysregulation and depression. Journal of Abnormal Child Psychology. 2015;43:283–296. doi: 10.1007/s10802-014-9909-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook RJ, Zeng L, Yi GY. Marginal analysis of incomplete longitudinal binary data: a cautionary note on LOCF imputation. Biometrics. 2004;60:820–828. doi: 10.1111/j.0006-341X.2004.00234.x. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Adair CE, Smetanin P, Stiff D, Briante C, Colman I, … Angold A. Diagnostic transitions from childhood to adolescence to early adulthood. Journal of Child Psychology and Psychiatry. 2013;54:791–799. doi: 10.1111/jcpp.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B. The dynamic properties of social support: Decay, growth, and staticity, and their effects on adolescent depression. Social Forces. 2003;81:953–978. [Google Scholar]
- Daviss WB. A review of co-morbid depression in pediatric ADHD: etiologies, phenomenology, and treatment. Journal of Child and Adolescent Psychopharmacology. 2008;18:565–571. doi: 10.1089/cap.2008.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon SV, Graber JA, Brooks-Gunn J. The roles of respect for parental authority and parenting practices in parent-child conflict among African American, Latino, and European American families. Journal of Family Psychology. 2008;22:1–17. doi: 10.1037/0893-3200.22.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuPaul GJ, Langberg JM. Educational impairments in children with ADHD. In: Barkley RA, editor. Attention-deficit/hyperactivity disorder: A handbook for diagnosis and treatment. 4. New York: Guilford; 2015. pp. 169–190. [Google Scholar]
- Eberhart NK, Hammen CL. Interpersonal predictors of onset of depression during the transition to adulthood. Personal Relationships. 2006;13(2):195. [Google Scholar]
- Eccles JS, Harold RD. Parent-school involvement during the early adolescent years. Teachers College Record. 1993;94:568–587. [Google Scholar]
- Eddy LD, Dvorsky MR, Molitor SJ, Bourchtein E, Smith Z, Oddo LE, … Langberg JM. Longitudinal evaluation of the cognitive-behavioral model of ADHD in a sample of college students with ADHD. Journal of Attention Disorders. 2015 doi: 10.1177/1087054715616184. [DOI] [PubMed] [Google Scholar]
- El Nokali NE, Bachman HJ, Votruba-Drzal E. Parent involvement and children’s academic and social development in elementary school. Child Development. 2010;81(3):988–1005. doi: 10.1111/j.1467-8624.2010.01447.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engels JM, Diehr P. Imputation of missing longitudinal data: A comparison of methods. Journal of Clinical Epidemiology. 2003;56:968–976. doi: 10.1016/s0895-4356(03)00170-7. [DOI] [PubMed] [Google Scholar]
- Evans SW, Schultz BK, White LC, Brady C, Sibley MH, Van Eck K. A school-based organization intervention for young adolescents with attention-deficit/hyperactivity disorder. School Mental Health. 2009;1:78–88. doi: 10.1007/s12310-009-9009-6. [DOI] [Google Scholar]
- Evans SW, Langberg JM, Schultz BK, Vaughn A, Altaye M, Marshall SA, Zoromski AK. Evaluation of a school-based treatment program for young adolescents with ADHD. Journal of Consulting and Clinical Psychology. 2016;84:15–30. doi: 10.1037/ccp0000057. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Pelham WE, Jr, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, … Burrows-MacLean L. A practical measure of impairment: psychometric properties of the impairment rating scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology. 2006;35:369–385. doi: 10.1207/s15374424jccp3503_3. [DOI] [PubMed] [Google Scholar]
- Fan W, Williams CM. The effects of parental involvement on students’ academic self-efficacy, engagement and intrinsic motivation. Educational Psychology. 2010;30:53–74. doi: 10.1080/01443410903353302. [DOI] [Google Scholar]
- Gajria K, Kosinski M, Sikirica V, Huss M, Livote E, Reilly K, … Erder MH. Psychometric validation of the Weiss Functional Impairment Rating Scale-Parent Report Form in children and adolescents with attention-deficit/hyperactivity disorder. Health and Quality of Life Outcomes. 2015;13:184–195. doi: 10.1186/s12955-015-0379-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaub M, Carlson CL. Behavioral characteristics of DSM-IV ADHD subtypes in a school-based population. Journal of Abnormal Child Psychology. 1997;25:103–111. doi: 10.1023/a:1025775311259. [DOI] [PubMed] [Google Scholar]
- Gonzalez-DeHass AR, Willems PP, Holbein MFD. Examining the relationship between parental involvement and student motivation. Educational Psychology Review. 2005;17:99–123. [Google Scholar]
- Grace JB, Bollen KA. Representing general theoretical concepts in structural equation models: the role of composite variables. Environmental and Ecological Statistics. 2008;15:191–213. [Google Scholar]
- Gresham FM, Elliott SN. Ssis: Social Skills Improvement System: Rating Scales Manual. PsychCorp; 2008. [Google Scholar]
- Gresham FM, Elliott SN, Vance MJ, Cook CR. Comparability of the Social Skills Rating System to the Social Skills Improvement System: Content and psychometric comparisons across elementary and secondary age levels. School Psychology Quarterly. 2011;26:27–44. [Google Scholar]
- Herman KC, Lambert SF, Ialongo NS, Ostrander R. Academic pathways between attention problems and depressive symptoms among urban African American children. Journal of Abnormal Child Psychology. 2007;35:265–274. doi: 10.1007/s10802-006-9083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, … Arnold LE. What aspects of peer relationships are impaired in children with attention-deficit/hyperactivity disorder? Journal of Consulting and Clinical Psychology. 2005;73:411–423. doi: 10.1037/0022-006X.73.3.411. [DOI] [PubMed] [Google Scholar]
- Humphreys KL, Katz SJ, Lee SS, Hammen C, Brennan PA, Najman JM. The association of ADHD and depression: Mediation by peer problems and parent–child difficulties in two complementary samples. Journal of Abnormal Psychology. 2013;122:854–867. doi: 10.1037/a0033895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeynes WH. A meta-analysis of the relation of parental involvement to urban elementary school student academic achievement. Urban Education. 2005;40:237–269. doi: 10.1177/0042085905274540. [DOI] [Google Scholar]
- Johnston C, Mash EJ. Families of children with attention-deficit hyperactivity disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4:183–207. doi: 10.1023/a:1017592030434. [DOI] [PubMed] [Google Scholar]
- Kane P, Garber J. Parental depresseion and child externalizing and internalizing symptoms: Unique effects of fathers’ symptoms and perceived conflict as a mediator. Journal of Child and Family Studies. 2009;18:465–472. [Google Scholar]
- Karustis JL, Power TJ, Rescorla LA, Eiraldi RB, Gallagher PR. Anxiety and depression in children with ADHD: Unique associations with academic and social functioning. Journal of Attention Disorders. 2000;4:133–149. [Google Scholar]
- Kent KM, Pelham WE, Jr, Molina BS, Sibley MH, Waschbusch DA, Yu J, … Karch KM. The academic experience of male high school students with ADHD. Journal of Abnormal Child Psychology. 2011;39:451–462. doi: 10.1007/s10802-010-9472-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kofler MJ, Rapport MD, Bolden J, Sarver DE, Raiker JS. ADHD and working memory: the impact of central executive deficits and exceeding storage/rehearsal capacity on observed inattentive behavior. Journal of Abnormal Child Psychology. 2010;38:149–161. doi: 10.1007/s10802-009-9357-6. [DOI] [PubMed] [Google Scholar]
- Langberg JM, Evans SW, Schultz BK, Becker SP, Altaye M, Girio-Herrera E. Trajectories and Predictors of Response to the Challenging Horizons Program for Adolescents With ADHD. Behavior Therapy. 2016;47:339–354. doi: 10.1016/j.beth.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikami AY, Jia M, Na JJ. Social skills training. Child and adolescent psychiatric clinics of North America. 2014;23(4):775–788. doi: 10.1016/j.chc.2014.05.007. [DOI] [PubMed] [Google Scholar]
- Moretti MM, Fine S, Haley G, Marriage MB. Childhood and adolescent depression: Child-report versus parent-report information. Journal of the American Academy of Child Psychiatry. 1985;24:298–302. doi: 10.1016/s0002-7138(09)61090-6. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergency of gender differences in depression during adolescents. Psychological Bulletin. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- O’Shea G, Spence SH, Donovan CL. Interpersonal factors associated with depression in adolescents: Are these consistent with theories underpinning interpersonal psychotherapy? Clinical Psychology & Psychotherapy. 2014;21:548–558. doi: 10.1002/cpp.1849. [DOI] [PubMed] [Google Scholar]
- Ostrander R, Herman KC. Potential cognitive, parenting, and developmental mediators of the relationship between ADHD and depression. Journal of Consulting and Clinical Psychology. 2006;74:89–98. doi: 10.1037/0022-006X.74.1.89. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Stoolmiller M. Replications of a dual failure model for boys’ depressed mood. Journal of Consulting and Clinical Psychology. 1991;59:491–498. doi: 10.1037//0022-006x.59.4.491. [DOI] [PubMed] [Google Scholar]
- Power TJ, Werba BE, Watkins MW, Angelucci JG, Eiraldi RB. Patterns of parent-reported homework problems among ADHD-referred and non-referred children. School Psychology Quarterly. 2006;21:13–33. [Google Scholar]
- Prinz RJ, Foster S, Kent RN, O’Leary KD. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of Applied Behavior Analysis. 1979;12:691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raggi VL, Chronis AM. Interventions to address the academic impairment of children and adolescents with ADHD. Clinical Child and Family Psychology Review. 2006;9:85–111. doi: 10.1007/s10567-006-0006-0. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Professional Manual for the Reynolds Adolescent Depression Scale. Odessa, FL: Psychological assessment resources; 1987. [Google Scholar]
- Reynolds WM. PAR, Psychological Assessment Resources. 2002. RADS-2: Reynolds Adolescent Depression Scale: Professional Manual. [Google Scholar]
- Robin AL, Foster S. Negotiating parent-adolescent conflict. New York: Guilford Press; 1989. [Google Scholar]
- Roy A, Oldehinkel AJ, Verhulst FC, Ormel J, Hartman CA. Anxiety and disruptive behavior mediate pathways from attention-deficit/hyperactivity disorder to depression. The Journal of Clinical Psychiatry. 2014;75:108–113. doi: 10.4088/JCP.13m08648. [DOI] [PubMed] [Google Scholar]
- Rueger SY, Malecki CK, Pyun Y, Aycock C, Coyle S. A meta-analytic review of the association between perceived social support and depression in childhood and adolescence. Psychological Bulletin. 2016;142:1017–1067. doi: 10.1037/bul0000058. [DOI] [PubMed] [Google Scholar]
- Rutter M. The developmental psychopathology of depression: Issues and perspectives. In: Rutter M, Izard CE, Read PB, editors. Depression in young people. New York: Guilford Press; 1986. [Google Scholar]
- Rutter M, Graham P, Chadwick OF, Yule W. Adolescent turmoil: fact or fiction? Journal of Child Psychology and Psychiatry. 1976;17:35–56. doi: 10.1111/j.1469-7610.1976.tb00372.x. [DOI] [PubMed] [Google Scholar]
- Safren SA, Sprich S, Chulvick S, Otto MW. Psychosocial treatments for adults with attention-deficit/hyperactivity disorder. Psychiatric Clinics of North America. 2004;27:349–360. doi: 10.1016/S0193-953X(03)00089-3. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Alpert A, Davis B, Andrews J. Family support and conflict: Prospective relations to adolescent depression. Journal of Abnormal Child Psychology. 1997;25(4):333–344. doi: 10.1023/A:1025768504415. [DOI] [PubMed] [Google Scholar]
- Sheridan SM, Dee CC, Morgan JC, McCormick ME, Walker D. A multimethod intervention for social skills deficits in children with ADHD and their parents. School Psychology Review. 1996;25:57–76. [Google Scholar]
- Shumow L, Lomax R. Parental efficacy: Predictor of parenting behavior and adolescent outcomes. Parenting: Science and Practice. 2002;2:127–150. [Google Scholar]
- Sibley MH, Graziano PA, Kuriyan AB, Coxe S, Pelham WE, Rodriguez L, … Ward A. Parent–teen behavior therapy + motivational interviewing for adolescents with ADHD. Journal of Consulting and Clinical Psychology. 2016;84:699–712. doi: 10.1037/ccp0000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:380–411. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- Song MK, Lin FC, Ward SE, Fine JP. Composite variables: when and how. Nursing Research. 2013;62:45–49. doi: 10.1097/NNR.0b013e3182741948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streiner DL. Missing data and the trouble with LOCF. Evidence-Based Mental Health. 2008;11:3–4. doi: 10.1136/ebmh.11.1.3-a. [DOI] [PubMed] [Google Scholar]
- Van Eck K, Finney SJ, Evans SW. Parent report of ADHD symptoms of early adolescents: A confirmatory factor analysis of the disruptive behavior disorders scale. Educational and Psychological Measurement. 2010;70:1042–1059. doi: 10.11177/0013164410378093. [DOI] [Google Scholar]
- Vanderbleek LM. Engaging families in school-based mental health treatment. Journal of Mental Health Counseling. 2004;26:211. [Google Scholar]
- Wechsler D. Wechsler intelligence scale for children–Fourth Edition (WISC-IV) San Antonio, TX: The Psychological Corporation; 2003. [Google Scholar]
- Weiss MD, Wasdell MB, Bomben MM. Weiss Functional Impairment Rating Scale-Parent Report (WFIRS-P). Poster presented at American Psychiatric Association 158th Annual Meeting; Atlanta, GA. 2004. [Google Scholar]
- Weller EB, Weller RA, Fristad MA, Rooney MT, Schecter J. Children’s interview for psychiatric syndromes (ChIPS) Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:76–84. doi: 10.1097/00004583-200001000-00019. [DOI] [PubMed] [Google Scholar]
- Wilder S. Effects of parental involvement on academic achievement: A meta-synthesis. Educational Review. 2014;66:377–397. doi: 10.1080/00131911.2013.780009. [DOI] [Google Scholar]
- Youngstrom E, Loeber R, Stouthamer-Loeber M. Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. Journal of Consulting and Clinical Psychology. 2000;68:1038–1050. doi: 10.1037//0022-006x.68.6.1038. [DOI] [PubMed] [Google Scholar]