Abstract
PURPOSE
This study evaluated the dimensional stability of a complete-arch prosthesis processed by conventional method in water bath or microwave energy and polymerized by two different curing cycles.
MATERIALS AND METHODS
Forty maxillary complete-arch prostheses were randomly divided into four groups (n = 10): MW1 - acrylic resin cured by one microwave cycle; MW2 - acrylic resin cured by two microwave cycles: WB1 - conventional acrylic resin polymerized using one curing cycle in a water bath; WB2 - conventional acrylic resin polymerized using two curing cycles in a water bath. For evaluation of dimensional stability, occlusal vertical dimension (OVD) and area of contact points were measured in two different measurement times: before and after the polymerization method. A digital caliper was used for OVD measurement. Occlusal contact registration strips were used between maxillary and mandibular dentures to measure the contact points. The images were measured using the software IpWin32, and the differences before and after the polymerization methods were calculated. The data were statistically analyzed using the one-way ANOVA and Tukey test (α = .05).
RESULTS
he results demonstrated significant statistical differences for OVD between different measurement times for all groups. MW1 presented the highest OVD values, while WB2 had the lowest OVD values (P<.05). No statistical differences were found for area of contact points among the groups (P=.7150).
CONCLUSION
The conventional acrylic resin polymerized using two curing cycles in a water bath led to less difference in OVD of complete-arch prosthesis.
Keywords: Denture, Complete, Dental occlusion, Acrylic resins, Polymerization
INTRODUCTION
A complete-arch prothesis is used to restore teeth and oral tissues function as support and retention during the masticatory force distribution on the alveolar ridge. Thus, complete-arch prostheses are responsible for the health maintenance of the oral tissues and for promoting adaptation, comfort, aesthetics, and masticatory efficiency for the patient.1
The acrylic resin is the main material used in the manufacturing of complete-arch prostheses. For a long time, this material was polymerized only by a water bath using metallic flasks (conventional polymerization). The polymerization of the methacrylate monomer occurs chemically with reaction between benzoyl peroxide and amine (rubbery phase). The polymerization will complete with heating cycles through an exothermic reaction. It is necessary for a radical initiator (benzoyle peroxide) to create the free radicals needed to promote the chain reactions. Thus, the acrylic resin will reach the dense phase. This procedure can be realized using two cycles: short cycle (90 minutes at 65℃ + 90 minutes at 100℃) or long cycle (12 hours at 73℃). Special attention must be given to the long cycle because the high temperature (over 100℃) can create air bubbles and/or porosities in the acrylic resin.2
The polymerization method using a microwave was created to reduce the polymerization time of complete-arch prostheses. This method completes the acrylic resin polymerization in 25 minutes with similar or even higher mechanical properties than conventional polymerization.3 In this polymerization method, the monomer molecules vibrate when the acrylic resin is exposed to a high-frequency electromagnetic field. This procedure promotes intermolecular collisions that generate the heat for the activation process. However, this method has some limitations since the heat irradiation is not homogeneous.4
Besides the polymerization method, different processing techniques can be used. The processing techniques using different polymerization cycles of acrylic resin may affect retention, adaptation, and stability of a complete-arch prosthesis in the buccal cavity. A double polymerization cycle may facilitate the registration and recording of maxillomandibular relations, decrease the movement of the acrylic resin bases on oral tissue (fibromucosa), increase the accuracy of the facial arch transfer on semi-adjustable articulator (SAA), and establish a correct occlusal vertical dimension (OVD).5 Besides the increased retention of the complete-arch prosthesis base on the alveolar ridge, increased patient comfort as well as stability, this technique offers the dentist some advantages, such as stable managament of a denture base during the complete-arch prosthesis manufacturing.5,6
A good acrylic polymerization method is capable of achieving the best physicochemical and biological properties of the acrylic resin, such as hardness, porosity, and monomer release. High levels of residual monomer is cytotoxic and can create porosities, affecting negatively the acrylic resin mechanical properties.2,6 Based on scientific knowledge, it can be assumed that any change in dimensional stability can occur in a complete-arch prosthesis during or after the polymerization process, thus affecting its adaptation and the treatment's clinical success. Yet there is a lack of information as to whether the polymerization method and processing techniques with different cycles could affect the OVD. Thus, the aim of this study is to evaluate the influence of two polymerization methods (water bath or microwave) and two processing techniques (one and two polymerization) of complete-arch prostheses on OVD and occlusal contacts. The null hypothesis is that the polymerization methods and processing techniques do not influence the OVD or occlusal contacts.
MATERIALS AND METHODS
For the evaluation of the OVD alteration, 40 complete-arch maxillary dental prostheses were fabricated. An edentulous maxillary stone cast was used for fabrication of the first complete-arch maxillary prosthesis. The acrylic resin teeth (Vipi-Dent Plus, Dental Vipi Ltda., Pirassununga, SP, Brazil) were mounted on a wax basis of maxillary cast using the Curve of Spee to compensate for anteroposterior and vestibulolingual curves. These initial prostheses were cured and mounted on SAA (BioArt, São Carlos, SP, Brazil), using 30° condylar and 15° Bennet guide angles, for fabrication of a mandibular complete-arch prosthesis. The fabrication process was, as mentioned above, made with teeth mounted in accordance with teeth of maxillary prostheses. The mandibular prosthesis was also mounted on SAA after curing. The inferior assembly (stone cast + prosthesis) was maintained on SAA. On the other hand, the superior assembly was removed and duplicated in silicone (Plastitécnica Ltda., São Paulo, SP, Brazil), and the other 40 edentulous maxillary stone casts were fabricated (type III dental stone, Herodent, Vigodent, Rio de Janeiro, RJ, Brazil). The maxillary prosthesis was also duplicated in silicone as orientation for teeth arrangement in fabrication of the specimens.
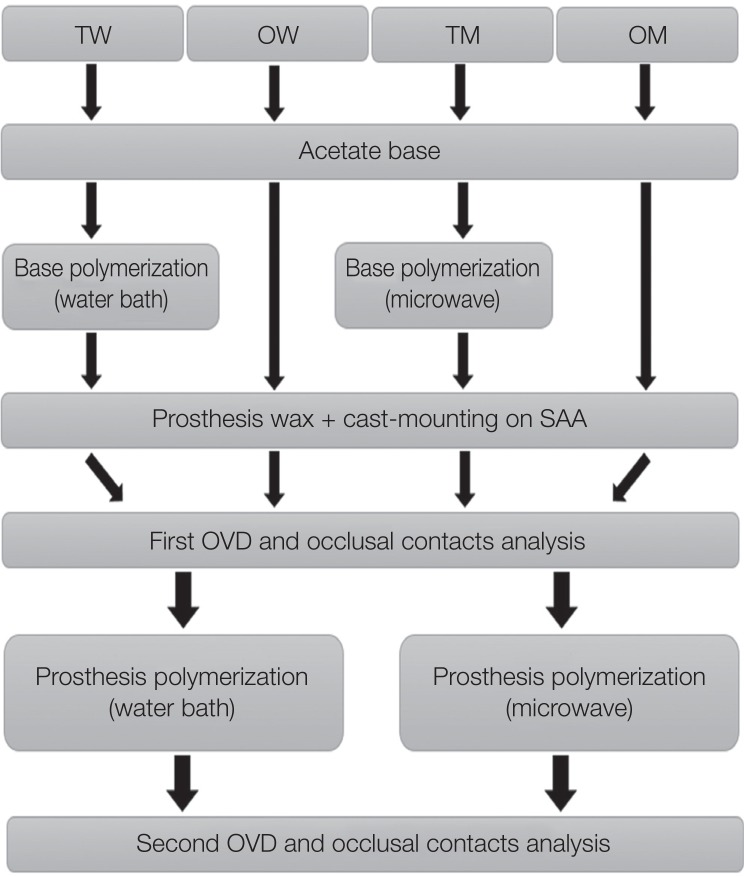
These maxillary stone casts and orientation molds were divided into four groups (n=10) according to polymerization methods and processing techniques (Fig. 1): one curing cycle in a microwave (MW1), one curing cycle in a water bath (WB1), two curing cycles in a microwave (MW2), and two curing cycles in a water bath (WB2). For each group, a specific acrylic resin was used: VIPI conventional (Dental VIPI Ltda., São Paulo, SP, Brazil) for WB1 and WB2 groups and VIPI Wave (Dental VIPI Ltda., São Paulo, SP, Brazil) for MW1 and MW2 groups. The denture fabricated by polymerization into water with one polymerization cycle was considered the control.
Fig. 1. Procedures of the polymerization process used in each group.
The basis of the complete-arch prosthesis was made with 1.5-mm-thick acetate plaques (Bio-Art, São Carlos, SP, Brazil). In MW2 and WB2 groups, acrylic resin teeth (Vipi-Dent Plus, Dental Vipi Ltda., Pirassununga, SP, Brazil) were mounted on the acetate plaques with wax, based on the orientation mold, and the stone casts with acetate plaques were positioned together with the orientation mold and teeth. Assemblies were included into plastic (microwave) or metallic (water bath) flasks, wax was removed and acrylic resin was pressed between teeth and stone cast. In WB2 and MW2 groups, first, an acrylic resin base made with the 1.5-mm-thick acetate plaque on the stone cast was subjected to polymerization. After that, acrylic resin teeth were mounted on the polymerized denture base with wax, based on the orientation mold, and the assemblies were included into plastic or metallic flasks, wax was removed and acrylic resin was pressed between teeth and polymerized denture base. Polymerization cycles used were: water bath (WB2; 3 hours at 60℃ + 9 hours at 70℃ + cooling with 25℃ at 12 hours - according to the manufacturer's instructions) or a microwave (MW2; 360 W for 3 minutes + 0 W for 4 minutes + 810 W for 3 minutes - shortest cycle found in literature7) and finishing and polishing procedures. The stone casts with acrylic resin bases were positioned on the orientation model. Metallic (Urabyp-n°6, Mac Dental, São Paulo, SP, Brazil) or microwave flasks (VIPI STG, Dental Vipi Ltda., Pirassununga, SP, Brazil) were used for the water bath and microwave groups, respectively. In both polymerization methods, flasks were submitted to a hydraulic press under a 1250 Kgf load for 30 min. Then the flask was opened and the prosthesis was removed from the mold.
The first measurement of the OVD (Fig. 2) was performed using a digital caliper (Starret, São Paulo, SP, Brazil) to measure the distance between the maxillary and mandibular elements for each pair of complete-arch prostheses (the same mandibular complete-arch prosthesis was used in all groups). The distance was measured three times and the mean was recorded. The occlusal contacts in maximum intercuspation (MI) were also performed using SAA and an articulation paper (Accufilm, Parkell, Inc. Edgewood, NY, USA) between maxillary and mandibular arches. For standardization of the contact point images, the model was placed on a stone base fixed with double adhesive tape (3M, St. Paul, MN, USA) to guarantee the same position for all device models/prostheses (Fig. 3). After marking the occlusal contact points, the superior prosthesis was placed on a stone cast to record the images with a Digital DSLR camera (D90, Nikon, Tokyo, Japan) coupled to a 18 – 55 mm focal length lens (AF-S DX Zoom-Nikkor 18 – 55 mm f/3.5 – 5.6 G, Nikon). The captured images were analyzed in the IpWin 32 software (Fig. 4). The marks of the occlusal contact points on artificial teeth were removed with cotton soaked in ethyl alcohol.
Fig. 2. Method used for measurement of alterations in occlusal vertical dimension: a digital caliper was used to measure the distance between the upper and lower frame of SAA before and after polymerization.
Fig. 3. Standardization of the contact points.
Fig. 4. Image already inserted into the software with occlusal contacts marked to have the area measured.
The maxillary prostheses (acrylic resin teeth + roll of wax on acetate base - MW1 and WB1; acrylic resin teeth + roll of wax on acrylic resin base - MW2 and WB2) were placed again in a flask using heat-activated acrylic resin (Vipi Cril, VIPI, Pirassununga, SP, Brazil), following the manufacturer's instructions. The polymerization process occurred using the same parameters previously described. Fig. 1 summarizes all the performed procedures. The complete-arch prostheses and stone casts were carefully removed from the flasks after their cooling to room temperature. Any fractured model was discarded. All specimen surfaces were finished with a tungsten carbide bur (Maxicut 1251, Edenta, São Paulo, SP, Brazil) using a dental handpiece at 10,000 rpm. Each pair of complete-arch prostheses was properly remounted on the SAA, and a second OVD and occlusal contact measurements were performed using the same procedure as the first measurement. The differences between first and second measurements were calculated (Δ) for each group. OVD and occlusal contact data were tested for normal distribution (Kolmogorov-Smirnov) and subjected to a one-way ANOVA, and the means were compared by Tukey test (α = .05).
RESULTS
The results (Δ) showed a significant difference among the groups evaluated for OVD results. MW1 presented the highest OVD values, while WB2 had the lowest OVD values (P < .05). The MW2 group showed statistically similar results with MW1 (P = .1606) and WB1 with WB2 (P = .5004). However, the polymerization methods and processing techniques do not show statistical influence regarding occlusal contacts (P = .7150) (Table 1).
Table 1. Δ means (± SD) of OVD and occlusal contacts values for each group (mm).
| Measurement | OVD | Occlusal contacts |
|---|---|---|
| MW2 | −0.75 (0.32)AB | 3.99 (3.71)A |
| MW1 | −0.87 (0.26)A | 2.72 (1.64)A |
| WB2 | −0.31 (0.12)C | 4.19 (1.69)A |
| WB1 | −0.53 (0.18)BC | 1.85 (1.48)A |
Data with different letters in column are statistically different (P < .05).
DISCUSSION
This study evaluated the effect of the polymerization process (water bath or microwave) and number of cycles performed on the stability of OVD and number of occlusal contacts. The null hypothesis was rejected for OVD measurements but was accepted for occlusal contacts. Dimensional changes that occur during the polymerization of complete-arch prostheses are not uniform and vary according to the thickness of the acrylic resin.8,9,10 In this study, to minimize possible distortions in the results, the bases of the prostheses were standardized using an acetate base with 1.5 mm thickness. The permanent-base denture technique used in complete-arch prosthesis manufacturing allows better adaptation and retention in the alveolar ridge and provides good patient comfort.11 This technique, in both water bath and microwave polymerization, and dimensional changes of the permanent-base denture after the second polymerization are considered clinically irrelevant to a prosthesis fitting in the mouth.5,9 Moreover, the choice to evaluate a maxillary wax prosthesis was based on the fact that dimensional changes can occur during the laboratory processing that modify the occlusal scheme obtained intraorally with wax. These dimensional changes are asymmetrical, and sometimes it is necessary to reassemble the prostheses in SAA for occlusal adjustment.9
With respect to OVD, all groups presented dimensional changes, independent of the processing technique and polymerization method used.12 All groups showed decreases in OVD values in the second measurements (shrinkage). The highest Δ values were evidenced in MW1 and the lowest for WB2 groups. This result can be explained by the fact that the gypsum is dehydrated during the polymerization process, causing shrinkage and/or contraction stress on the acrylic resin.12 The acrylic resin cured by microwave cycle cannot withstand high temperatures because its glass transition temperature can be quickly exceeded.6 During the high heating in the second cycle of polymerization, when the acrylic resin returns to room temperature, it induces a greater number of stresses that promote great dimensional changes.2 It does not occur in conventional acrylic resins once they have a higher glass transition temperature. Thus, the second cycle of polymerization decreases the stress, resulting in better dimensional stability.12
The OVD changes are due to teeth movement since the small separation of the incisal pin occurred in all groups. Independent of the cycle or method of polymerization, movement of the artificial teeth occurs.13 So, it is necessary for the dental wear to maintain the occlusal balance and to ensure that it does not cause injury in the buccal mucosa by pressure. The deviation of the incisal pin may have other explanations, such as thickness of the acrylic resin base,5,9 thermal expansion of the acrylic resin during polymerization14 or dental stone,15 and internal shrinkage after closing of the flask and its opening for removal of the separation plastic.12
A significant difference was observed between MW2 and WB2 groups in OVD values. These values can be justified by the fact that both groups were submitted to the first polymerization process, thus promoting greater dimensional change in the permanent-base denture polymerized in a water bath. The microwave polymerization is faster than a water bath. The intense energy promoted by a microwave is capable of polymerizing the acrylic resin through a uniform absorption of heat by the acrylic resin. It determines a good adaptation of the permanent-base denture.13 These results were expected, but they were only performed for OVD analysis to standardize the ASA assembly. The MW1 and WB1 groups also showed a significant difference. The microwave energy may have an important influence on OVD because the quick heating may impair the clinical outcome. In this study, the polymerization by microwave energy produced some contrasting results, but this procedure offers some advantages compared to the conventional water bath, such as quick handling and efficient polymerization in cleaner processing equipment,16 with all mechanical properties according to ADA guidelines.17
A recent literature review concluded that there is no indication that permanent alteration in the OVD will produce long-lasting TMD symptoms.18 Some studies showed that alterations of 3.4 to 4.5 mm caused initial speech difficulties and muscle discomfort that subsided after 1 – 2 weeks.19 But since there is no consensus, alteration in the clinically defined parameters should be avoided, even more when the alteration is not controlled but resultant from the handling methods.
Regarding the occlusal contacts (Table 1), the statistical analysis did not show significant difference, and it was performed to standardize the occlusal contact areas. The good fit of a permanent-base denture is promoted by homogeneous heating of the acrylic resin, and it is best carried out in a microwave, thus decreasing the tooth movement and occlusal contact.20 The microwave energy emitted during the polymerization generates a small temperature gradient between the acrylic resin and model, and uniform heating results in quick polymerization and stress reduction, maintaining the teeth in position.13
The alterations in occlusal contact area are directly related to the alteration of biting force.21,22 The variation observed was between 1 and 4 mm. Thus, all polymerization procedures caused alterations in occlusal contact area.
CONCLUSION
The polymerization method using two curing cycles in a water bath for conventional acrylic resin polymerization resulted in the best OVD results for complete-arch prosthesis.
References
- 1.Mahadevan V, Krishnan M, Krishnan CS, Azhagarasan NS, Sampathkumar J, Ramasubramanian H. Influence of surface modifications of acrylic resin teeth on shear bond strength with denture base resin-an invitro study. J Clin Diagn Res. 2015;9:ZC16–ZC21. doi: 10.7860/JCDR/2015/13877.6445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh S, Palaskar JN, Mittal S. Comparative evaluation of surface porosities in conventional heat polymerized acrylic resin cured by water bath and microwave energy with microwavable acrylic resin cured by microwave energy. Contemp Clin Dent. 2013;4:147–151. doi: 10.4103/0976-237X.114844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nishii M. Studies on the curing of denture base resins with microwave irradiation: with particular reference to heat-curing resins. J Osaka Dent Univ. 1968;2:23–40. [PubMed] [Google Scholar]
- 4.Sesma N, Gil C, Kolikauskas WA, Silva RA, Pannuti CM. Temperature of denture base resin under different protocols of microwave irradiation. Braz Dent J. 2011;22:388–391. doi: 10.1590/s0103-64402011000500007. [DOI] [PubMed] [Google Scholar]
- 5.Fenlon MR, Juszczyk AS, Rodriguez JM, Curtis RV. Dimensional stability of complete denture permanent acrylic resin denture bases; A comparison of dimensions before and after a second curing cycle. Eur J Prosthodont Restor Dent. 2010;18:33–38. [PubMed] [Google Scholar]
- 6.Wagner AG, Sanders SR. Permanent, heat-cured, acrylic-resin bases for complete dentures. Gen Dent. 1990;38:138–140. [PubMed] [Google Scholar]
- 7.Barbosa DB, Compagnoni MA, Leles CR. Changes in occlusal vertical dimension in microwave processing of complete dentures. Braz Dent J. 2002;13:197–200. doi: 10.1590/s0103-64402002000300011. [DOI] [PubMed] [Google Scholar]
- 8.Wolfaardt J, Cleaton-Jones P, Fatti P. The influence of processing variables on dimensional changes of heat-cured poly(methyl methacrylate) J Prosthet Dent. 1986;55:518–525. doi: 10.1016/0022-3913(86)90191-5. [DOI] [PubMed] [Google Scholar]
- 9.Mazaro JV, Gennari Filho H, Vedovatto E, Amoroso AP, Pellizzer EP, Zavanelli AC. Influence of different base thicknesses on maxillary complete denture processing: linear and angular graphic analysis on the movement of artificial teeth. J Craniofac Surg. 2011;22:1661–1665. doi: 10.1097/SCS.0b013e31822e5d8c. [DOI] [PubMed] [Google Scholar]
- 10.Gharechahi J, Asadzadeh N, Shahabian F, Gharechahi M. Flexural strength of acrylic resin denture bases processed by two different methods. J Dent Res Dent Clin Dent Prospects. 2014;8:148–152. doi: 10.5681/joddd.2014.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ribeiro JA, de Resende CM, Lopes AL, Farias-Neto A, Carreiro Ada F. The influence of mandibular ridge anatomy on treatment outcome with conventional complete dentures. Acta Odontol Latinoam. 2014;27:53–57. doi: 10.1590/S1852-48342014000200001. [DOI] [PubMed] [Google Scholar]
- 12.Silva-Concilio LR, Meloto CB, Neves ACC, Cunha LG, Rizzatti-Barbosa CM. Influence of different flasking and polymerizing methods on the occlusal vertical dimension of complete dentures. Acta Odontol Latinoam. 2012;25:312–317. [PubMed] [Google Scholar]
- 13.Negreiros WA, Consani RLX, Mesquita MF. Dimensional stability of distances between teeth in complete dentures comparing microwave polymerization and conventional cycles. Braz J Oral Sci. 2010;9:384–387. [Google Scholar]
- 14.Nogueira SS, Ogle RE, Davis EL. Comparison of accuracy between compression- and injection-molded complete dentures. J Prosthet Dent. 1999;82:291–300. doi: 10.1016/s0022-3913(99)70083-1. [DOI] [PubMed] [Google Scholar]
- 15.Salloum AM. Influence of high expansion dental stone used as investing medium on the changes in occlusal vertical dimension of complete dentures. Saudi Dent J. 2013;25:135–140. doi: 10.1016/j.sdentj.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pero AC, Barbosa DB, Marra J, Ruvolo-Filho AC, Compagnoni MA. Influence of microwave polymerization method and thickness on porosity of acrylic resin. J Prosthodont. 2008;17:125–129. doi: 10.1111/j.1532-849X.2007.00264.x. [DOI] [PubMed] [Google Scholar]
- 17.Consani RL, Mesquita MF, Sobrinho LC, Sinhoreti MA. Dimensional accuracy of upper complete denture bases: the effect of metallic flask closure methods. Gerodontology. 2009;26:58–64. doi: 10.1111/j.1741-2358.2008.00234.x. [DOI] [PubMed] [Google Scholar]
- 18.Moreno-Hay I, Okeson JP. Does altering the occlusal vertical dimension produce temporomandibular disorders? A literature review. J Oral Rehabil. 2015;42:875–882. doi: 10.1111/joor.12326. [DOI] [PubMed] [Google Scholar]
- 19.Gross MD, Ormianer Z. A preliminary study on the effect of occlusal vertical dimension increase on mandibular postural rest position. Int J Prosthodont. 1994;7:216–226. [PubMed] [Google Scholar]
- 20.Kimura H, Teraoka F, Ohnishi H, Saito T, Yato M. Application of microwave for dental technique (part 2). Adaptability of cured acrylic resins. J Osaka Univ Dent Sch. 1984;24:21–29. [PubMed] [Google Scholar]
- 21.Aras K, Hasanreisoğlu U, Shinogaya T. Masticatory performance, maximum occlusal force, and occlusal contact area in patients with bilaterally missing molars and distal extension removable partial dentures. Int J Prosthodont. 2009;22:204–209. [PubMed] [Google Scholar]
- 22.Baca E, Yengin E, Gökçen-Röhlig B, Sato S. In vivo evaluation of occlusal contact area and maximum bite force in patients with various types of implant-supported prostheses. Acta Odontol Scand. 2013;71:1181–1187. doi: 10.3109/00016357.2012.757360. [DOI] [PubMed] [Google Scholar]