Abstract
PURPOSE
All-ceramic restorations required extensive tooth preparation. The purpose of this in vitro study was to investigate a minimally invasive preparation and thickness of monolithic zirconia crowns, which would provide sufficient mechanical endurance and strength.
MATERIALS AND METHODS
Crowns with thickness of 0.2 mm (group 0.2, n=32) or of 0.5 mm (group 0.5, n=32) were milled from zirconia and fixed with resin-based adhesives (groups 0.2A, 0.5A) or zinc phosphate cements (groups 0.2C, 0.5C). Half of the samples in each subgroup (n=8) underwent thermal cycling and mechanical loading (TCML)(TC: 5℃ and 55℃, 2×3,000 cycles, 2 min/cycle; ML: 50 N, 1.2×106 cycles), while the other samples were stored in water (37℃/24 h). Survival rates were compared (Kaplan-Maier). The specimens surviving TCML were loaded to fracture and the maximal fracture force was determined (ANOVA; Bonferroni; α=.05). The fracture mode was analyzed.
RESULTS
In both 0.5 groups, all crowns survived TCML, and the comparison of fracture strength among crowns with and without TCML showed no significant difference (P=.628). Four crowns in group 0.2A and all of the crowns in group 0.2C failed during TCML. The fracture strength after 24 hours of the cemented 0.2 mm-thick crowns was significantly lower than that of adhesive bonded crowns. All cemented crowns provided fracture in the crown, while about 80% of the adhesively bonded crowns fractured through crown and die.
CONCLUSION
0.5 mm thick monolithic crowns possessed sufficient strength to endure physiologic performance, regardless of the type of cementation. Fracture strength of the 0.2 mm cemented crowns was too low for clinical application.
Keywords: Zirconia, Minimal invasive, Monolithic crown, Cementation, Ceramic
INTRODUCTION
With the increasing consideration in esthetics and biocompatibility, all-ceramic restorations have gained a high popularity in dentistry.1,2,3 3-molar yttria-stabilized tetragonal zirconia polycrystal (3Y-TZP) has been used for its high strength and good reliability,4 which allows longer-span ceramic restorations even in high stress-bearing posterior areas.5 Chipping of the veneering ceramic is the most frequently reported complication of veneered zirconia restorations6,7,8,9,10 and may be attributed to the design of framework, a low strength of the veneer ceramic, or an insufficient cooling during the veneering process.11,12,13 In monolithic restorations, these disadvantages of the bilayer system can be circumvented.14,15 Monolithic crowns made of alternative ceramics like monolithic lithium disilicate showed lower fracture strength than those made of zirconia.16 Monolithic zirconia crowns also provide a higher reliability and better capability to sustain loading.13,14,15 Zirconia restorations should provide a better long-term stability and lower sensitivity for aging and fatigue effects, which may be advantageous under clinical conditions. Simulation tests with thermal cycling and mechanical loading may allow for estimating these effects. The strength of a material is of clinical interest because the material properties affect the preparation design. General ceramic preparation guidelines require an axial and occlusal tooth reduction of about 1.5 – 2.0 mm15 to ensure the stability of a glass-ceramic crown. However, the (excessive) removal of tooth structure may cause a potential damage to dental pulp15 or reduce the stability of the remaining tooth substance. The prepared teeth may be preserved using minimal invasive techniques together with a minimal thickness of the restoration. Crown thickness is supposed to have a significant effect on the stability of the restoration.17 Monolithic zirconia crowns with a chamfer width and occlusal thickness of only 0.5 mm showed sufficient strength for an application in posterior areas.18,19,20 But, the stability of the restoration is further influenced by the type of cementation.17,18,21 Adhesive bonding improved the fracture resistance of monolithic all-ceramic crowns compared with conventional cementation.22
Up to date, only limited scientific information and even less clinical data are available that show the influence of minimally invasive tooth preparation and the effect of cementation on the performance (survival) and fracture resistance of monolithic zirconia restorations. Here, in vitro tests may help evaluate the indications by combining standardized laboratory conditions with basic clinical requirements (e.g. thermal aging and mechanical loading). In contrast to simplified crash-the-crown tests,23 which show only limited clinical relevance, the in vitro tests might simulate fatigue failures and decementation, allowing a prediction of the expected performance of the investigated restoration. Even in cases without any catastrophic failures, aging and deterioration effects might be indicated by a reduced fracture resistance of the restoration.
The purpose of this in vitro study was to investigate the thickness of the restoration and the type of cementation, which are required to guarantee sufficient fatigue resistance and fracture strength of monolithic CAD/CAM-fabricated zirconia crowns. The hypothesis of the study was that in vitro performance and fracture strength of monolithic zirconia crowns depend on material thickness and type of cementation.
MATERIALS AND METHODS
A molar tooth (36; ANA-4 V CE, Frasaco, Tettnang, Germany) has been digitalized (desktop scanner Matchpoint, Biodentis, Leipzig, Germany). After determination of the margin line, the occlusal and circumferential reduction of tooth was set to be 0.2 mm or 0.5 mm for the preparation of the artificial tooth, which resulted in a circular shoulder with rounded inner angles at an isogingival height of the tooth cervix. The convergence angle between two axial walls was designed to be 8°. Edges between the occlusal surface, cone, and chamfer were rounded with a radius of 0.6 mm to reduce stress concentration. The cement gap between crown and tooth was set to be 80 µm (software Geomagic Studio 11, 333 Three D Systems Circles, Rock Hill, SC, USA).
2 × 32 zirconia crowns were designed and sintered (thickness of 0.2 mm or 0.5 mm; Zirkon BioStar HT LOT 50544966, Siladent Dr. Böhme & Schöps, Goslar, D, 2 hours 1450℃) and 2 × 32 respective composite teeth (Ambarino High-Class LOT140214, creamed, Marburg, Germany) were milled by a 5-axis milling machine (ULTRASONIC 10; Sauer, Stipshausen, Germany) with the diamond-coated spherical cutter (2 mm, 1 mm, 0.6 mm in diameter; EMUGE-Werk Richard Glimpel, Lauf, Germany) (Fig. 1). The composite tooth material provided a modulus of elasticity of 13.8 MPa, a Vickers hardness of 815 MPa, and a flexural strength of 191 MPa.
Fig. 1. Specimen example (zirconia crowns and artificial tooth).
The teeth were positioned in resin blocks (Palapress Vario, Heraeus-Kulzer, Hanau, Germany) and the resilience of the human periodontium was simulated by coating the roots of the teeth with a 1 mm polyether layer (Impregum, 3M Oral Care, Seefeld, Germany). For achieving a constant layer, the roots were dipped in wax bath, which was replaced by polyether in a second fabrication process, as described in previous studies.24,25
For the cementation of the crowns, two cements were used: a resin-based adhesive system (Panavia F 2.0 LOT4F 0099/4E0020, Kuraray Noritake Dental, Tokyo J, Elipar Trilight, 3M Oral Care, 4 × 20 s: groups “A”) and zinc phosphate cement (Harvard Cement LOT2141505/ 2101507, Harvard Dental, Dahlwitz, D: groups: “C”). According to the type of cement, the groups were divided into the following subgroups (n = 16 per subgroup):
Group 0.2A (thickness 0.2 mm, A: adhesive bonding)
Group 0.2C (thickness 0.2 mm, C: cementation)
Group 0.5A (thickness 0.5 mm, A: adhesive bonding)
Group 0.5C (thickness 0.5 mm, C: cementation).
After cementation, half of the specimens in each subgroup (n = 8) were mounted on a chewing simulator (EGO, Regensburg, Germany) and underwent thermal cycling (2 × 3,000 between 5℃ and 55℃, 2 minutes for each cycle) and simultaneous mechanical loading (1.2 × 106 cycles, 50 N, f = 1.6 Hz). 12-mm steatite balls served as antagonists and were positioned in three point occlusal contact situation. Online failure-control was performed. Failures were documented and failed samples were excluded from the further process. The applied parameters were supposed to simulate five years of intraoral function.26,27 The other half of the specimens in each subgroup (n = 8), which did not undergo TCML, served as reference and were investigated after 24 hours storage in water (37℃).
All specimens surviving TCML were mounted on a universal testing machine (Zwick 1446, Zwick, Ulm, Germany) and a load was occlusally applied with a 12 mm steel sphere (1 mm/min). A tin foil (0.25 mm, Dentaurum, Ispringen, Germany) was inserted between crown and sphere to prevent force peaks. The maximal fracture load was measured until the crown failed. Failure detection was set to 10% loss of maximal loading or acoustic signal. All teeth were optically examined under a microscope after fracture testing and the failure mode was analyzed.
Power calculation (G*Power 3.1.3) provided an estimated power of > 90% with eight specimens per subgroup. Distribution of the data was controlled with Shapiro-Wilk-test. Means and standard deviations were calculated and analyzed by one-way analysis of variance (ANOVA) and the Bonferroni-test for post-hoc analysis (SPSS 22, IBM, Armonk, NY, USA). Survival rates were compared by Kaplan-Maier-test. The level of significance was set to be α = .05.
RESULTS
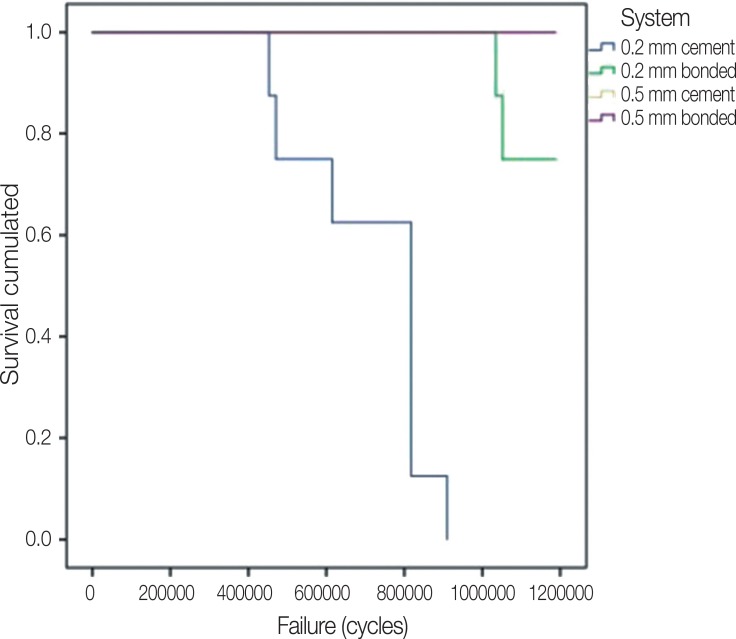
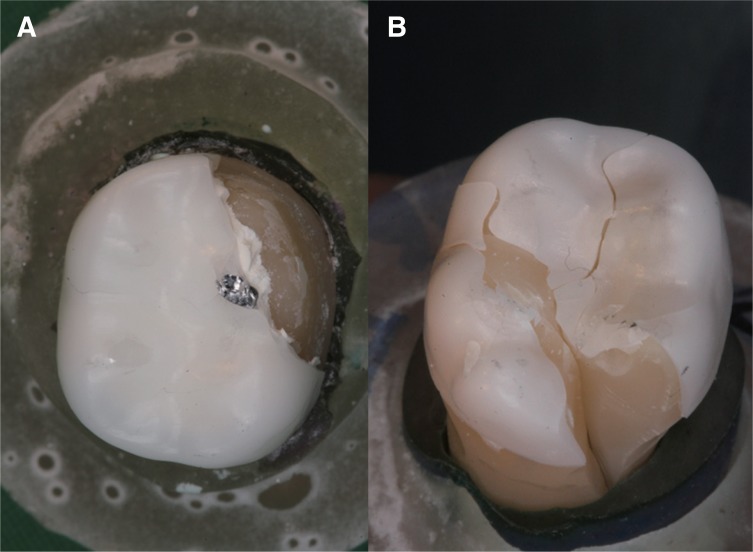
In-vitro simulation: Four crowns in group 0.2A and all crowns in group 0.2C failed during TCML. The 0.2 mm thick cemented crowns failed between 435,000 to 910,000 cycles, and 0.2 mm adhesive-bonded crowns between 1,034,500 and 1,200,000 cycles. No decementation or debonding without fracture could be detected. Figure 2 shows the cumulative survival of the crowns during TCML. All crowns of both of the 0.5 groups and four crowns of group 0.2A survived TCML. Kaplan-Maier showed significant (P = .000) survival rates. All 0.2 mm thick crowns, which failed during TCML, showed fracture of the crown (Fig. 3A) independent on type of cementation.
Fig. 2. Cumulated survival during TCML; 0.5 bonded and cemented crowns showed no failures.
Fig. 3. Fracture pattern. (A) fracture of the crown, (B) fracture through crown and tooth.
Fracture load, 24 h results: 0.2 mm thick crowns showed lower fracture results for both adhesive bonding (1164 ± 334 N) and cementation (772 ± 148 N) in comparison to 0.5 mm crown with adhesive (1628 ± 174 N) and cementation (1357 ± 340 N). One-way Anova group comparison revealed significant (P < .001) differences among the groups. 0.2C crowns had significantly (P < .037) lower fracture results than 0.2A crowns and both of the 0.5 crowns. 0.2A and 0.5A crowns showed no significant (P = .933) differences, as well as both of the 0.5 groups (P = .301).
TCML: fracture results after TCML varied between 0 N (0.2C) and 1628 ± 174 N (0.5A). Significant (P < .001) differences among the groups were found (One-way Anova). Individual Bonferroni comparison showed that 0.2C had no significantly (P = .104) different fracture strength in comparison to 0.2A. Both of the 0.5 groups showed no significantly (P > .064) different fracture results from 0.2A and between each other (P = 1.000). TCML reduced the fracture force in comparison to 24 hours data for groups 0.2C (P < .001) and 0.5A (P = .040) only. Fracture strength and statistical information are listed in Table 1. Data were normally distributed (P > .364) for the individual groups. For the crowns that underwent fracture tests, both fracture modes (fracture crown/fracture crown and die Fig. 3) could be observed. All cemented crowns showed partial crown fracture and about 80% of the bonded crowns fractured together with the tooth.
Table 1. Fracture strength [in N] after 24 h (37℃) water storage or thermal cycling and mechanical loading (TCML) (mean, standard deviation, minimum, maximum) with adhesive bonding or cementation (identical numbers and letters indicate no significant differences P < .05).
| Crown thickness 0.2 mm (group 0.2) | Crown thickness 0.5 mm (group 0.5) | |||||||
|---|---|---|---|---|---|---|---|---|
| Adhesive bonding | Cementation | Adhesive bonding | Cementation | |||||
| 24 hA | TCML12 | 24 h | TCML1 | 24 hB | TCML23 | 24 hAB | TCML23 | |
| Mean | 1164 | 725 | 772 | 0 | 1628 | 1430 | 1357 | 1510 |
| Std. Deviation | 334 | 809 | 148 | 0 | 174 | 175 | 340 | 792 |
| Minimum | 640 | 0 | 496 | 0 | 1370 | 1234 | 899 | 811 |
| Maximum | 1726 | 1982 | 932 | 0 | 1982 | 1662 | 1993 | 2947 |
DISCUSSION
Based on the results, the hypothesis that the thickness of the crown and the type of cementation influenced the in-vitro survival and fracture resistance of zirconia crowns could be approved. TCML illustrated a significantly different performance depending on the thickness of the crowns. All crowns in both of the 0.5-groups survived TCML, whereas all of the cemented 0.2 mm crowns and four adhesively bonded 0.2 mm crowns failed. The influence of cementation was obvious because the failed adhesively bonded 0.2 mm crowns provided about two times longer survival time than the analogously cemented systems (Fig. 2). Further on, all cemented crowns provided lowest minimum fracture results.
TCML parameters were chosen comparable to other in vitro studies,28,29 simulating five years of intraoral use.26,27 Clinical parameters are very individual (tooth structure, periodontal mobility, occlusal loads, chewing behavior, oral environment, preparation design), and therefore standardized conditions may help simplify conditions and simulate clinically observed failures. Although composite teeth with a comparable modulus of elasticity to human teeth were used in this study, they may differ from human teeth in terms of bonding capacity to the cement.30 Pretests were performed to guarantee adhesive bonding and limited bonding with conventional cementation, both situations comparable to human teeth. The resilient support of the abutment teeth was simulated by a polyether layer, which naturally does not stay abreast of the complex human periodontal ligament but might help avoid an overestimation of the strength of ceramic restorations.24 With high-strength zirconia, aging and deterioration often occur without any visible or catastrophic failures. In these cases, the fracture test may help locate weak points or allow a differentiation between different types of cementation. Although fracture data cannot be directly related to clinical survival, they may provide information on the stability and suitability of the restoration.
We found that TCML had a significant effect on the stability of the crowns and reduced the fracture force in comparison to 24 hours data for cemented 0.2 mm and adhesively bonded 0.5 mm crowns. These data partly confirm other investigations, showing that the fracture resistance of a monolithic crown is related with aging effects and its material and thickness.13,16,31,32 For zirconia crowns that were not aged, Nordahl et al.16 found a mean fracture strength between 787 N to 916 N with a thickness of 0.5 mm, and lower fracture force of about 450 N with a thickness of 0.3 mm. With 1.5 mm zirconia crowns, they determined fracture values higher than 3000 N. It was found that 0.7 mm thick zirconia crowns provided higher fracture strength than 1.0 mm thick crowns made of glazed lithium disilicate. Under compressive loading (chewing), occlusal thickness seemed to be of higher importance than the axial thickness, and therefore a small increase in occlusal thickness resulted in an improved fracture resistance.18 However, fracture testing may only provide limited insight into clinically relevant mechanisms of damage and underlying reasons for failure because clinically relevant complications may also be attributed to biological complications (secondary caries, pulp lesion).33,34 These investigations were confirmed by our results, where 0.5 mm thick monolithic crowns survived the aging procedure and showed a high resistance to the fracture load, which also displayed the potential to endure physiologic occlusal force. However, most of the crowns with 0.2 mm thickness failed during the aging procedures and the fracture strength was lower than that with 0.5 mm thickness.
Baseline fracture data after 24 hours confirm the influence of the cement on the stability of the tooth-crown complex. All bonded crowns showed higher fracture forces than the cemented crowns. Adhesive cementation contributes to the stability with a high mechanical strength, high bonding, and low solubility. Resin based systems showed the lowest stress and were regarded as desirable luting agent for monolithic zirconia crowns when comparing the stress distribution of zinc phosphate, polycarboxylate, glass ionomer, and resin cementation by finite element analysis.35 It has been reported that the adhesive luting technique improved the fracture resistance of glass ceramic crowns with lower strength values (e.g. feldspathic and leucite-reinforced glass ceramics13,36), while fracture loads of high-strength ceramics like zirconia were not significantly influenced by the mode of cementation.37,38 A stabilization of the crown with adhesive bonding is not necessary when zirconia crowns provide sufficient thickness.39 The actual data confirm these results for a thickness of 0.5 mm and clearly show the limitations for a 0.2 mm thick crown. The high failure numbers during TCML for 0.2 mm crowns support this conclusion. However, the reduced number of surviving crowns (and fracture data) for the 0.2 mm crowns is a limiting aspect. The failure pattern during TCML and fracture tests underline the results; whereas cemented crowns were completely de-cemented and fractured, fragments of the bonded crowns were still bonded to the dies. Partial bonding was high enough that individual teeth fractured. However, fracture patterns might be attributed to a cement dependent stress distribution in the crown-tooth system.19,40 Bindl et al.41 found multiple cracks in a zinc phosphate layer already at the beginning fracture, but no cracks in an comparable adhesive layer. For the adhesive bonding, the crack directly passed the crown and progressed into the teeth, indicating a good bonding between tooth and crown.41 This type of fracture guarantees a high stability of the tooth crown complex, but implies the risk of tooth fracture.
All fracture values of the 0.5 mm crowns and the 0.2 mm adhesively bonded control crowns exceeded maximum chewing forces, which are reported to be up to 900 N.42 Therefore these crowns have the potential to withstand occlusal forces applied in the posterior region.
CONCLUSION
0.5 mm thick monolithic zirconia crowns provided sufficient strength and in-vitro performance, regardless of the type of cementation. Fracture strength of 0.2 mm thick cemented zirconia crowns was too low for clinical application, although adhesive bonding improved the performance and stability.
References
- 1.Kelly JR, Nishimura I, Campbell SD. Ceramics in dentistry: historical roots and current perspectives. J Prosthet Dent. 1996;75:18–32. doi: 10.1016/s0022-3913(96)90413-8. [DOI] [PubMed] [Google Scholar]
- 2.Rimmer S. Modern dental ceramics: An overview. Int Dent SA. 2006;8:32–39. [Google Scholar]
- 3.Griggs JA. Recent advances in materials for all-ceramic restorations. Dent Clin North Am. 2007;51:713–727. doi: 10.1016/j.cden.2007.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999;20:1–25. doi: 10.1016/s0142-9612(98)00010-6. [DOI] [PubMed] [Google Scholar]
- 5.Sorrentino R, De Simone G, Tetè S, Russo S, Zarone F. Five-year prospective clinical study of posterior three-unit zirconia-based fixed dental prostheses. Clin Oral Investig. 2012;16:977–985. doi: 10.1007/s00784-011-0575-2. [DOI] [PubMed] [Google Scholar]
- 6.Schmitter M, Mueller D, Rues S. Chipping behaviour of all-ceramic crowns with zirconia framework and CAD/CAM manufactured veneer. J Dent. 2012;40:154–162. doi: 10.1016/j.jdent.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Kirmali O, Akin H, Ozdemir AK. Shear bond strength of veneering ceramic to zirconia core after different surface treatments. Photomed Laser Surg. 2013;31:261–268. doi: 10.1089/pho.2013.3487. [DOI] [PubMed] [Google Scholar]
- 8.Choi YS, Kim SH, Lee JB, Han JS, Yeo IS. In vitro evaluation of fracture strength of zirconia restoration veneered with various ceramic materials. J Adv Prosthodont. 2012;4:162–169. doi: 10.4047/jap.2012.4.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sundh A, Molin M, Sjögren G. Fracture resistance of yttrium oxide partially-stabilized zirconia all-ceramic bridges after veneering and mechanical fatigue testing. Dent Mater. 2005;21:476–482. doi: 10.1016/j.dental.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 10.Wimmer T, Hostettler J, Beuer F, Stawarczyk B. Load-bearing capacity of soldered and subsequently veneered 4-unit zirconia FDPs. J Mech Behav Biomed Mater. 2013;23:1–7. doi: 10.1016/j.jmbbm.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 11.Guess PC, Bonfante EA, Silva NR, Coelho PG, Thompson VP. Effect of core design and veneering technique on damage and reliability of Y-TZP-supported crowns. Dent Mater. 2013;29:307–316. doi: 10.1016/j.dental.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 12.Preis V, Letsch C, Handel G, Behr M, Schneider-Feyrer S, Rosentritt M. Influence of substructure design, veneer application technique, and firing regime on the in vitro performance of molar zirconia crowns. Dent Mater. 2013;29:e113–e121. doi: 10.1016/j.dental.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Y, Mai Z, Barani A, Bush M, Lawn B. Fracture-resistant monolithic dental crowns. Dent Mater. 2016;32:442–449. doi: 10.1016/j.dental.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y, Lee JJ, Srikanth R, Lawn BR. Edge chipping and flexural resistance of monolithic ceramics. Dent Mater. 2013;29:1201–1208. doi: 10.1016/j.dental.2013.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lameira DP, Buarque e, Andrade e Silva F, De Souza GM. Fracture strength of aged monolithic and bilayer zirconia-based crowns. Biomed Res Int. 2015;2015:418641. doi: 10.1155/2015/418641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nordahl N, Vult von Steyern P, Larsson C. Fracture strength of ceramic monolithic crown systems of different thickness. J Oral Sci. 2015;57:255–261. doi: 10.2334/josnusd.57.255. [DOI] [PubMed] [Google Scholar]
- 17.Thompson VP, Rekow DE. Dental ceramics and the molar crown testing ground. J Appl Oral Sci. 2004;12:26–36. doi: 10.1590/s1678-77572004000500004. [DOI] [PubMed] [Google Scholar]
- 18.Nakamura K, Harada A, Inagaki R, Kanno T, Niwano Y, Milleding P, Örtengren U. Fracture resistance of monolithic zirconia molar crowns with reduced thickness. Acta Odontol Scand. 2015;73:602–608. doi: 10.3109/00016357.2015.1007479. [DOI] [PubMed] [Google Scholar]
- 19.Nakamura K, Mouhat M, Nergård JM, Lægreid SJ, Kanno T, Milleding P, Örtengren U. Effect of cements on fracture resistance of monolithic zirconia crowns. Acta Biomater Odontol Scand. 2016;2:12–19. doi: 10.3109/23337931.2015.1129908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sorrentino R, Triulzio C, Tricarico MG, Bonadeo G, Gherlone EF, Ferrari M. In vitro analysis of the fracture resistance of CAD-CAM monolithic zirconia molar crowns with different occlusal thickness. J Mech Behav Biomed Mater. 2016;61:328–333. doi: 10.1016/j.jmbbm.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 21.Sun T, Zhou S, Lai R, Liu R, Ma S, Zhou Z, Longquan S. Load-bearing capacity and the recommended thickness of dental monolithic zirconia single crowns. J Mech Behav Biomed Mater. 2014;35:93–101. doi: 10.1016/j.jmbbm.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 22.Papia E, Larsson C, du Toit M, Vult von. Bonding between oxide ceramics and adhesive cement systems: a systematic review. J Biomed Mater Res B Appl Biomater. 2014;102:395–413. doi: 10.1002/jbm.b.33013. [DOI] [PubMed] [Google Scholar]
- 23.Kelly JR. Clinically relevant approach to failure testing of all-ceramic restorations. J Prosthet Dent. 1999;81:652–661. doi: 10.1016/s0022-3913(99)70103-4. [DOI] [PubMed] [Google Scholar]
- 24.Rosentritt M, Behr M, Scharnagl P, Handel G, Kolbeck C. Influence of resilient support of abutment teeth on fracture resistance of all-ceramic fixed partial dentures: an in vitro study. Int J Prosthodont. 2011;24:465–468. [PubMed] [Google Scholar]
- 25.Rosentritt M, Behr M, Gebhard R, Handel G. Influence of stress simulation parameters on the fracture strength of all-ceramic fixed-partial dentures. Dent Mater. 2006;22:176–182. doi: 10.1016/j.dental.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 26.Rosentritt M, Behr M, van der Zel JM, Feilzer AJ. Approach for valuating the influence of laboratory simulation. Dent Mater. 2009;25:348–352. doi: 10.1016/j.dental.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Rosentritt M, Siavikis G, Behr M, Kolbeck C, Handel G. Approach for valuating the significance of laboratory simulation. J Dent. 2008;36:1048–1053. doi: 10.1016/j.jdent.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Rosentritt M, Steiger D, Behr M, Handel G, Kolbeck C. Influence of substructure design and spacer settings on the in vitro performance of molar zirconia crowns. J Dent. 2009;37:978–983. doi: 10.1016/j.jdent.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Rosentritt M, Behr M, Thaller C, Rudolph H, Feilzer A. Fracture performance of computer-aided manufactured zirconia and alloy crowns. Quintessence Int. 2009;40:655–662. [PubMed] [Google Scholar]
- 30.Rosentritt M, Plein T, Kolbeck C, Behr M, Handel G. In vitro fracture force and marginal adaptation of ceramic crowns fixed on natural and artificial teeth. Int J Prosthodont. 2000;13:387–391. [PubMed] [Google Scholar]
- 31.Beuer F, Stimmelmayr M, Gueth JF, Edelhoff D, Naumann M. In vitro performance of full-contour zirconia single crowns. Dent Mater. 2012;28:449–456. doi: 10.1016/j.dental.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 32.Rekow ED, Harsono M, Janal M, Thompson VP, Zhang G. Factorial analysis of variables influencing stress in all-ceramic crowns. Dent Mater. 2006;22:125–132. doi: 10.1016/j.dental.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 33.Gehrt M, Wolfart S, Rafai N, Reich S, Edelhoff D. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clin Oral Investig. 2013;17:275–284. doi: 10.1007/s00784-012-0700-x. [DOI] [PubMed] [Google Scholar]
- 34.Rauch A, Reich S, Schierz O. Chair-side generated posterior monolithic lithium disilicate crowns: clinical survival after 6 years. Clin Oral Investig. 2017;21:2083–2089. doi: 10.1007/s00784-016-1998-6. [DOI] [PubMed] [Google Scholar]
- 35.Ha SR. Biomechanical three-dimensional finite element analysis of monolithic zirconia crown with different cement type. J Adv Prosthodont. 2015;7:475–483. doi: 10.4047/jap.2015.7.6.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ma L, Guess PC, Zhang Y. Load-bearing properties of minimal-invasive monolithic lithium disilicate and zirconia occlusal onlays: finite element and theoretical analyses. Dent Mater. 2013;29:742–751. doi: 10.1016/j.dental.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stawarczyk B, Beuer F, Ender A, Roos M, Edelhoff D, Wimmer T. Influence of cementation and cement type on the fracture load testing methodology of anterior crowns made of different materials. Dent Mater J. 2013;32:888–895. doi: 10.4012/dmj.2013-147. [DOI] [PubMed] [Google Scholar]
- 38.Al-Wahadni AM, Hussey DL, Grey N, Hatamleh MM. Fracture resistance of aluminium oxide and lithium disilicate-based crowns using different luting cements: an in vitro study. J Contemp Dent Pract. 2009;10:51–58. [PubMed] [Google Scholar]
- 39.Vult von Steyern P, Ebbesson S, Holmgren J, Haag P, Nilner K. Fracture strength of two oxide ceramic crown systems after cyclic pre-loading and thermocycling. J Oral Rehabil. 2006;33:682–689. doi: 10.1111/j.1365-2842.2005.01604.x. [DOI] [PubMed] [Google Scholar]
- 40.Raadsheer MC, van Eijden TM, van Ginkel FC, Prahl-Andersen B. Contribution of jaw muscle size and craniofacial morphology to human bite force magnitude. J Dent Res. 1999;78:31–42. doi: 10.1177/00220345990780010301. [DOI] [PubMed] [Google Scholar]
- 41.Bindl A, Lüthy H, Mörmann WH. Strength and fracture pattern of monolithic CAD/CAM-generated posterior crowns. Dent Mater. 2006;22:29–36. doi: 10.1016/j.dental.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 42.Varga S, Spalj S, Lapter Varga M, Anic Milosevic S, Mestrovic S, Slaj M. Maximum voluntary molar bite force in subjects with normal occlusion. Eur J Orthod. 2011;33:427–433. doi: 10.1093/ejo/cjq097. [DOI] [PubMed] [Google Scholar]