INTRODUCTION
Clear cell carcinoma is a rare low-grade salivary gland malignant neoplasm which represents approximately 1% of all salivary gland tumors. These tumors occur exclusively in minor salivary gland and are characterized by an indolent growth and less aggressive biological behavior. The clarity of cytoplasm of the clear cells has been attributed to accumulation of glycogen, loss of organelles, or as fixation artifact.[1,2,3] As a result, the differential diagnosis of intraoral clear cell neoplasms of includes a diverse group of tumors including primary salivary gland clear cell tumors, clear cell odontogenic tumors as well as few metastatic tumors. Therefore, the diagnosis of clear cell carcinoma is of exclusion.[1,2]
CASE REPORT
A 40-year-old female patient presented with a slow growing, painless swelling of 6–7 years’ duration on the right side of the face intraorally and extraorally. Habit history revealed smoking of 10 cigarettes per day for 7 years. Intraoral examination revealed a diffuse hard swelling measuring about 5 cm × 6 cm on the maxillary right posterior region, extending from the midline of the palate, from mesial aspect of 14 to the distal aspect of 18. Orthopantamograph and occlusal radiograph showed extensive bone loss and missing 16. The computed tomography at the level of the maxilla revealed a radiodense mass extending from the 14 region up to the maxillary tuberosity and also extension of the tumor mass into the maxillary antrum. A volume-rendered computed tomography showed erosion of the palatine bone on the right side of the maxilla [Figure 1]. Grossly, the tumor mass was yellowish cream in color with a reddish tinge, firm in consistency with an irregular surface texture. The cut surface was yellowish white with a few hemorrhagic foci at the periphery.
Figure 1.
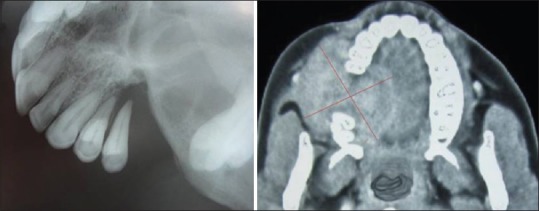
Occlusal radiograph (left) superficial erosion of the palatine bone, computed tomography (right) revealed the extent of the tumor mass
HISTOPATHOLOGIC FEATURES
Overlying orthokeratinized stratified squamous epithelium showed pseudoepitheliomatous hyperplasia, increased mitotic figures and individual cell keratinization [Figure 2]
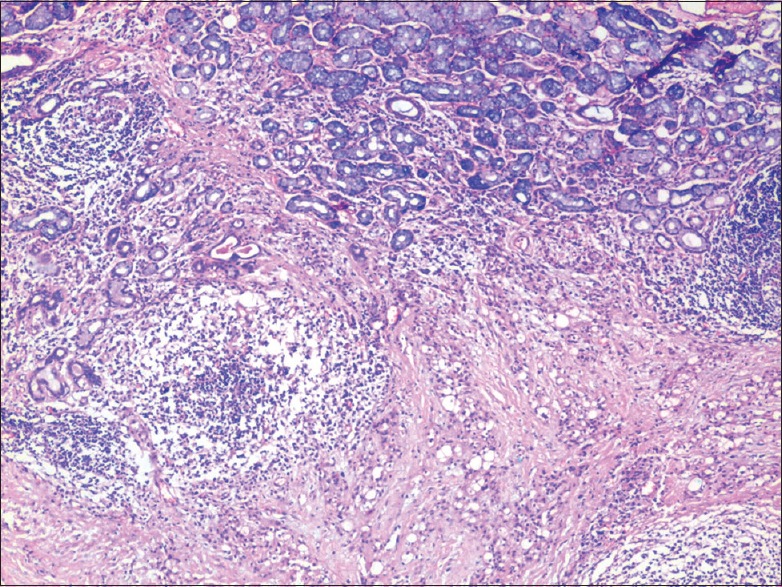
Connective tissue stroma showed sheets and strands of clear cells and small cells with eosinophilic cytoplasm with oval to round nucleus interspersed with dense, fibrocellular radiating collagen fibers [Figure 3]
Some of the cells are arranged in nests and cords along with duct-like structures filled with mucoid material [Figure 4]
Clear cells appear to be pleomorphic with prominent hyperchromatic nuclei [Figure 5]
At the periphery, palatine salivary glands were evident [Figure 6]
Perineural invasion was also noted [Figure 7].
Figure 2.
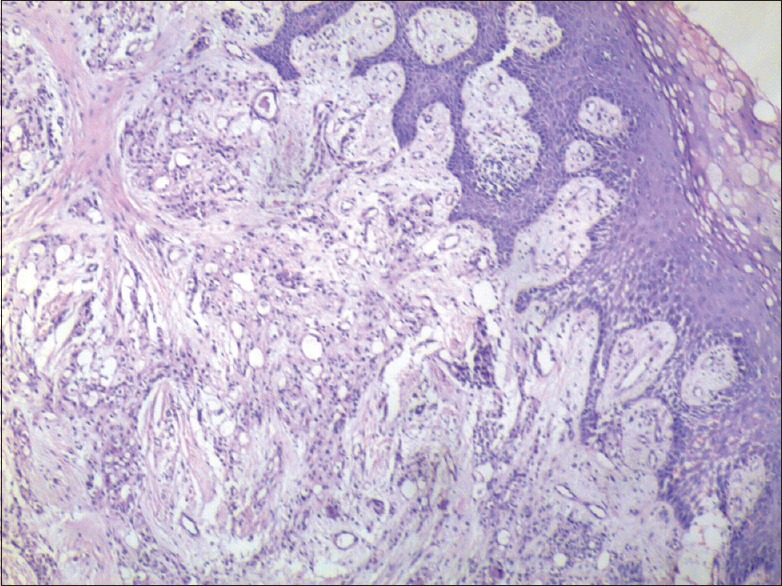
Photomicrograph of overlying palatine epithelium with underlying connective tissue showing clear cells (H&E, ×40)
Figure 3.
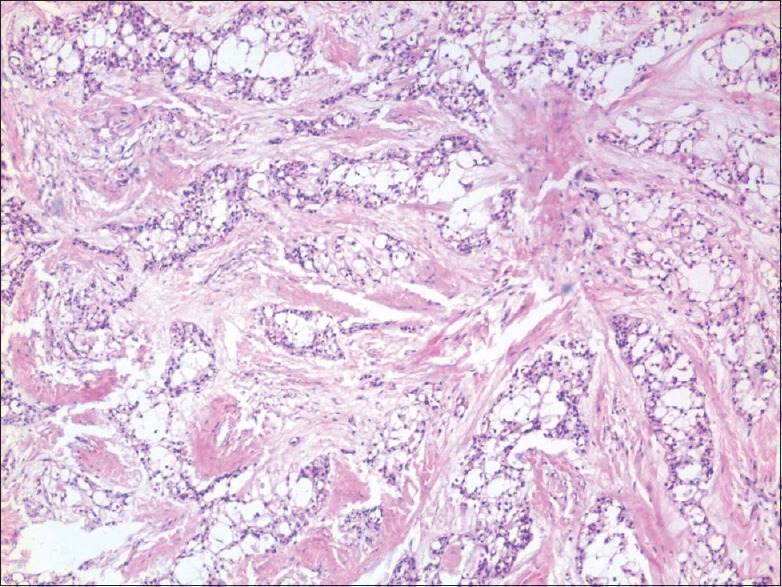
Photomicrograph of clear cells and small eosinophilic cells in sheets and islands separated by fibrocellular connective tissue septa (H&E, ×40)
Figure 4.
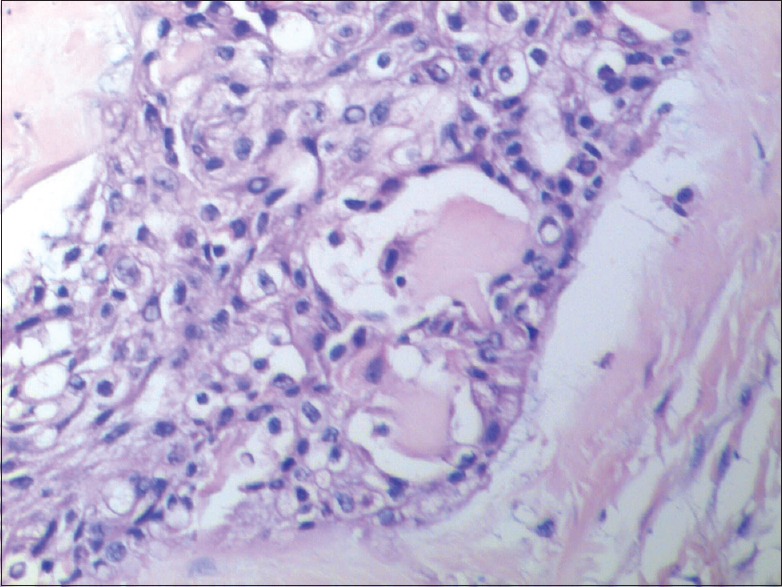
Photomicrograph of island of clear cells and eosinophilic cells with duct-like structures (H&E, ×200)
Figure 5.
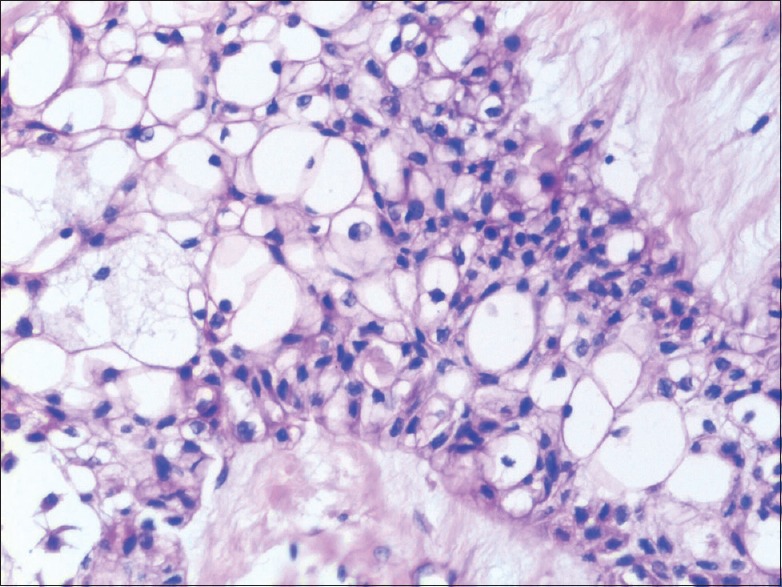
Photomicrograph of island of pleomorphic clear cells and eosinophilic cells (H and E, ×200)
Figure 6.
Photomicrograph of palatine salivary gland at the periphery of the mass (H&E, ×40)
Figure 7.
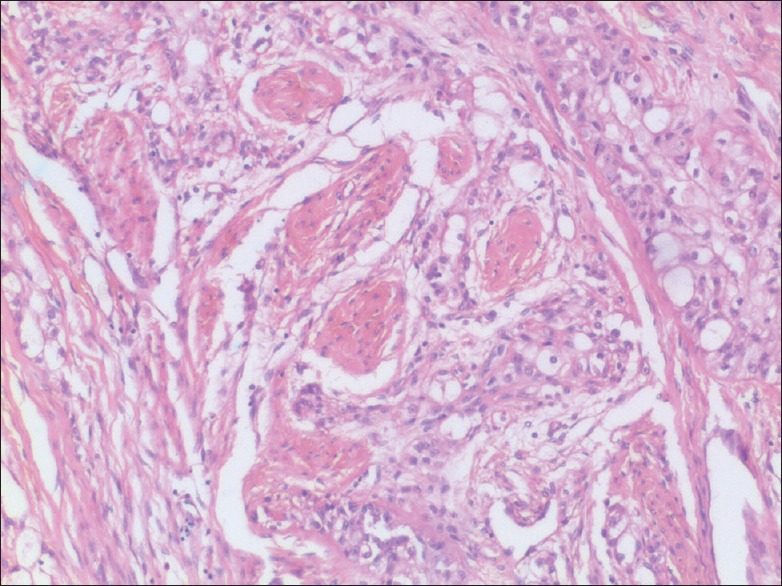
Photomicrograph of infiltration of nerve fiber bundles at the periphery of the tumor (H&E, ×100)
The presence of clear cells in hematoxillin and eosin sections justified the need to perform special stains and immunohistochemistry (IHC) to arrive at definitive diagnosis.
SPECIAL STAINS
Mucicarmine (residual salivary glands at the periphery showed positive stain) [Figure 8], alcian blue, periodic acid–Schiff reagent (PAS), phosphotungstic acid hematoxillin (PTAH), Congo red and oil red O stain showed a negative reaction for the tumor.
Figure 8.
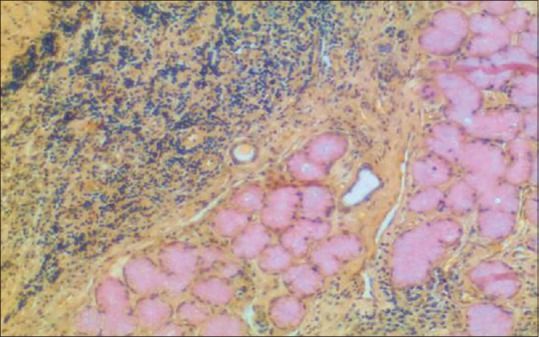
Photomicrograph of negative mucicarmine staining of the clear cells except the palatine salivary (H&E, ×40)
IMMUNOHISTOCHEMISTRY
Tumor cells showed positivity for cytokeratin panel CK, CK5/6 (CK5-basal cell marker with myoepithelial markers CK6) [Figure 9]
P63-small eosinophillic cells showed positive reaction indicative of proliferation, whereas clear cells showed no reaction [Figure 10]
Eosinophilic cells showed S100-positive reaction [Figure 11]
Negative reaction for CK8, CK19, smooth muscle actin (SMA), CD10 (metastasis) and Vimentin markers.
Figure 9.
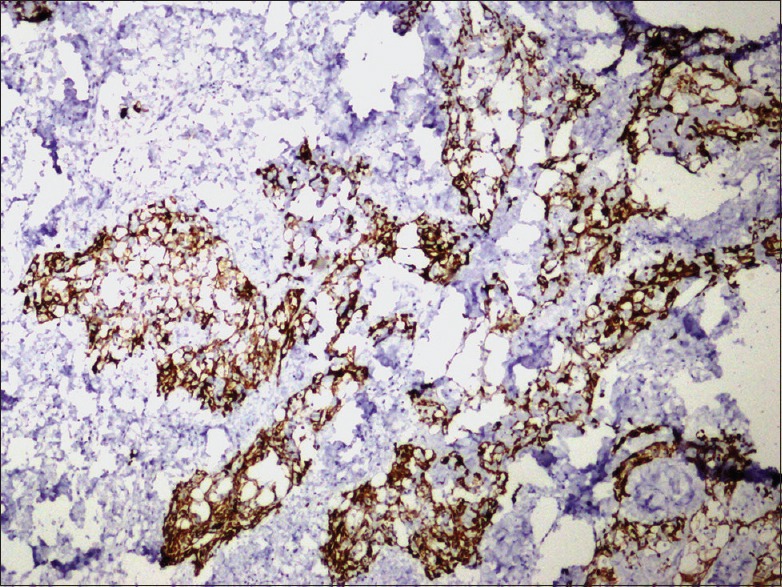
Photomicrograph of immunostaining of the clear cells by the cytokeratin 5/6 (×100)
Figure 10.
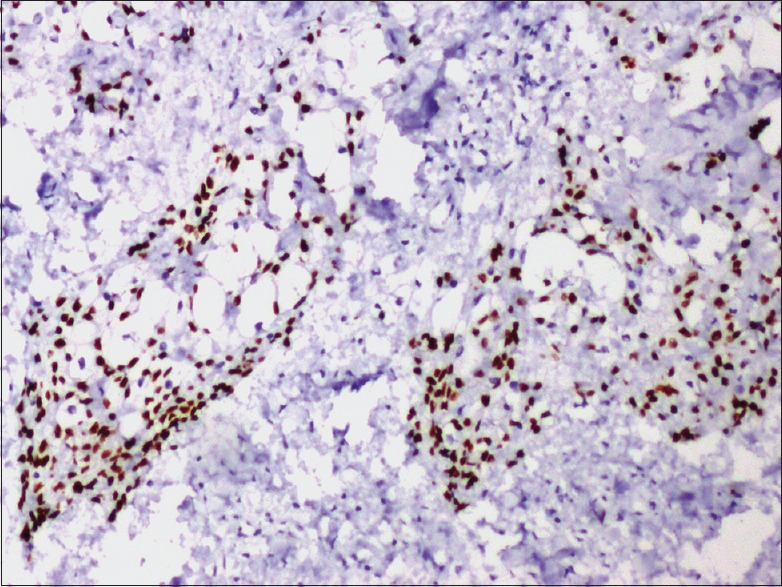
Photomicrograph of immunostaining of the small eosinophilic cells by the proliferative marker P63 (×100)
Figure 11.
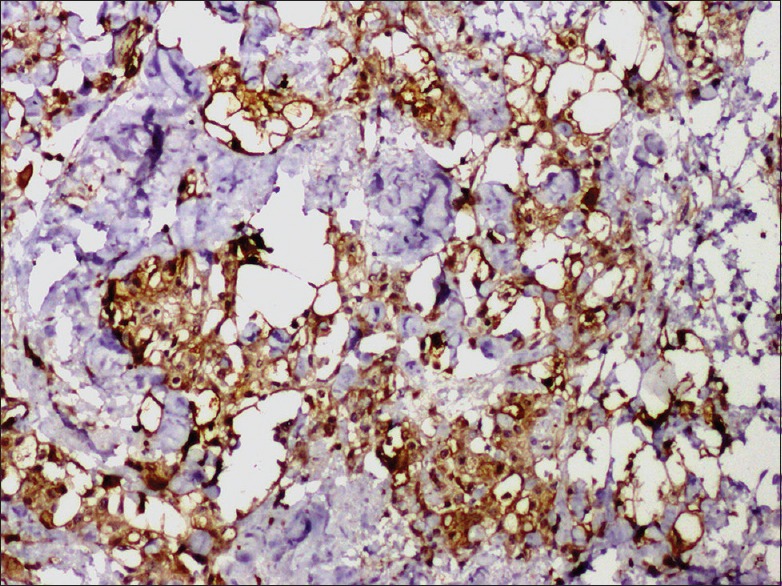
Photomicrograph of immunostaining of the clear cells by the s100 (×100)
DIFFERENTIAL DIAGNOSIS
Clear cell variants of primary salivary gland tumors
Mucoepidermoid carcinomas – they show PAS positive, diastase-resistant cytoplasmic granules. Mucous cells demonstration by mucicarmine, alcian blue and IHC staining for MUC5AC helps in diagnosis[2,3]
Acinic cell carcinoma – degenerative clear cell changes account for < 95% of tumor cells. They show PAS positive, diastase-resistant cyplasmic granules, negative with mucicarmine and alcian blue. IHC staining for CK7 and CK 8 positive[2,3]
Oncocytoma – positive with PAS and PTAH (blue cytoplasmic granules under oil immersion). Negative with digested PAS and Alcian blue[2]
Epithelial-myoepithelial carcinoma – characteristic biphasic pattern with inner cell expressing epithelial markers (low-molecular-weight cytokeratin Cam 5.2, European medicines agency and AE1/AE3), surrounded by an outer layer of cells showing positive staining with myoepithelial markers such as SMA, calponin, vimentin and S-100. PAS-positive basement membrane separating the tumor island from stroma[1,2,3]
Myoepithelial carcinomas – clear cells negative with mucicarmine staining. Myxoid matrix is positive with alcian blue staining. Tumor cells are positive with myoepithelial markers calponin, vimentin, SMA, S-100, CK7 and CK14.[1,2,3]
Clear cell lesions of odontogenic origin
Clear cell odontogenic carcinoma shows lobulated growth pattern, presence of osteodentin, and more likely to be intraosseous in origin. The clear cells are PAS positive with diastase sensitive cytoplasmic granules. They are negative with mucin, vimentin and muscle actin. Positive with CK8 and CK19[4]
Clear cell variants of calcifying epithelial odontogenic tumor – presence of calcifications – Liesegang rings and Congo red stain positive for amyloid deposition in connective tissue.[4]
Metastatic clear cell lesions
FINAL DIAGNOSIS
Based on clinicoradiological findings and immunohistochemical profile of the microscopic features, the diagnosis of clear cell carcinoma of minor salivary gland of hard palate was given.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yang S, Zhang J, Chen X, Wang L, Xie F. Clear cell carcinoma, not otherwise specified, of salivary glands: A clinicopathologic study of 4 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:712–20. doi: 10.1016/j.tripleo.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 2.Said-Al-Naief N, Klein MJ. Clear cell entities of the head and neck: A selective review of clear cell tumors of the salivary glands. Head Neck Pathol. 2008;2:111–5. doi: 10.1007/s12105-008-0052-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gnepp DR. Diagnostic Surgical Pathology of the Head and Neck. Philadlphia: Saunders Elsevier; 2001. [Google Scholar]
- 4.Loyola AM, Cardoso SV, de Faria PR, Servato JP, Barbosa de Paulo LF, Eisenberg AL, et al. Clear cell odontogenic carcinoma: Report of 7 new cases and systematic review of the current knowledge. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:483–96. doi: 10.1016/j.oooo.2015.06.005. [DOI] [PubMed] [Google Scholar]


