Abstract
We report a 4 year old child referred for routine cardiology evaluation as part of evaluation of murmur with scoliosis. On examination, there was mild duskiness. Echocardiography revealed bilateral superior vena cavae, a small innominate vein, a left superior vena cava to the left atrium and an intact coronary sinus. The findings were confirmed on computed tomography angiography. Percutaneous closure of the left superior vena cava by an Amplatzer vascular plug was done successfully. Although the patient was apparently asymptomatic, the procedure was done to prevent risk of cerebral emboli.
MeSH: cyanosis, left superior vena cava abnormalities, vascular plug, percutanoeus closure
Introduction
Persistent left superior vena cava (LSVC) is the most common variation of the thoracic venous system prevalent in 0.3% of the population, 3-10 % with congenital heart defects.1–4 In isolation, it does not carry any haemodynamic significance. Isolated left superior vena cava to left atrium with intact coronary sinus is an extremely rare entity and is a rare cause of systemic arterial desaturation. LSVC to left atrium (LA) needs correction to prevent increasing cyanosis, decreased exercise tolerance due to increasing hypoxia during activity and to eliminate the possibility of cerebral embolism/brain abscess. Here we describe a child who was referred to us for cardiac evaluation for murmur detected as part of work up for scoliosis. He was diagnosed with an extremely rare cause of cyanosis, LSVC to left atrium with intact coronary sinus. He underwent percutaneus closure of LSVC with an Amplatzer vascular plug.
Case description
The patient was a 4 year old child, weighing 14 kg, from Iraq, the product of full-term normal vaginal delivery to 2nd gravid mother. Antenatal, perinatal and post-natal periods were uneventful. The child was evaluated for scoliosis at one year of age and was followed up by a local neurosurgeon. The child was brought to India for further consultation for scoliosis and on evaluation, a murmur was detected. On cardiac evaluation, he found dusky (resting oxygen saturation 90%, 80% after walking) ,first and second heart sounds were normal, left ventricle (LV) S3 was present, as well as a grade 2/6 systolic murmur. Chest X-ray (postero-anterior view) showed scoliosis to the right, no cardiomegaly and normal pulmonary blood flow (figure 1).
Figure 1.
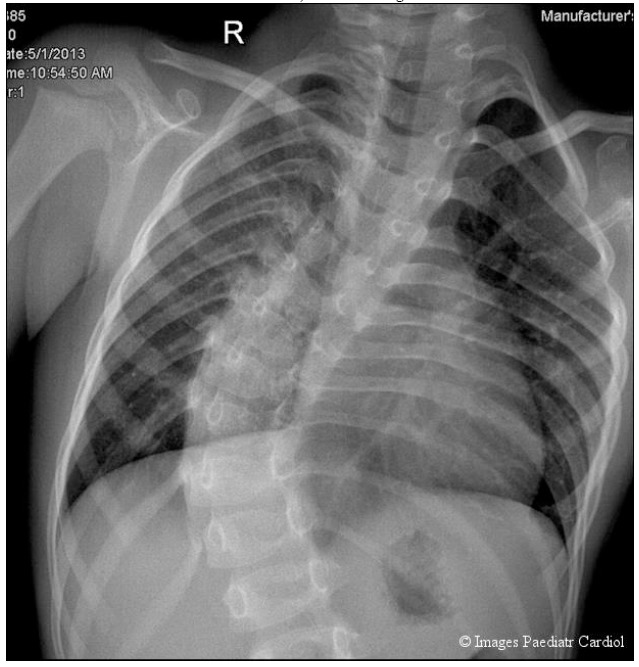
Figure. 1 Chest X-ray postero-anterior showing no cardiomegaly, normal pulmonary vasculature, scoliosis to right
Twelve lead electrocardiogram showed sinus rhythm, normal ‘P’ wave, QRS axis +90. Echocardiography including contrast injection with agitated saline from left upper arm showed LSVC connecting to LA, a small innominate vein and right SVC to right atrium (RA) (figure 2).
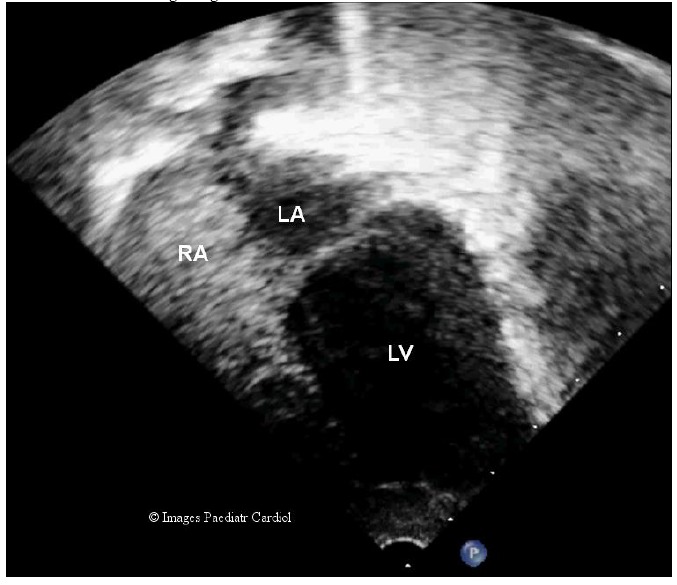
Figure 2.
Echocardiography evaluation
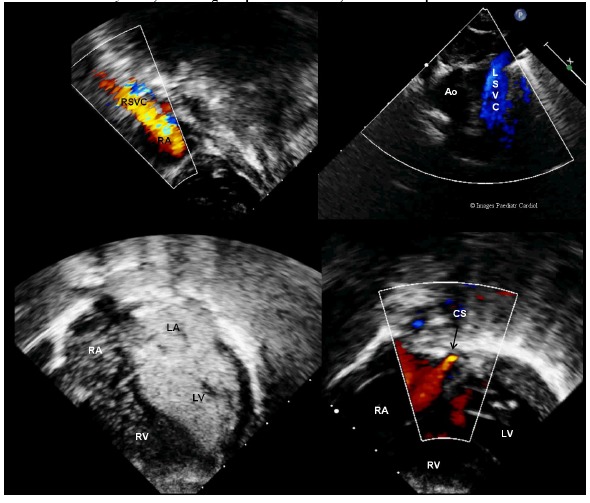
a. Subcostal sagittal view showing right superior vena cava (RSVC) to right atrium (RA) (Top left)
b. Suprasternal short axis view showing left superior vena cava(LSVC) to left atrium (LA) (Top right)
c. Apical 4 chamber view with injection of agitated saline via left brachial vein showing immediate filling of left atrium and left ventricle (LV) with some filling of right atrium and right ventricle (RV) confirming connection of left superior vena cava to left atrium (Bottom left)
d. Apical four chamber view on color flow mapping in most posterior plane showing intact coronary sinus (CS) (marked by arrow) (bottom right).
Abbreviations-RA right atrium, LA-left atrium, RV-right ventricle, LV-left ventricle, Ao-aorta, CS-coronary sinus, RSVC-right superior vena cava, LSVC- left superior vena cava
There was no intracardiac defect. Ventricular dimensions and functions were within normal limits. The coronary sinus was not dilated and was intact, a rare finding in this situation (figure 2d).
Echocardiography windows were very poor due to scoliosis so CT angiography was done to further delineate the anatomy and showed the same findings (figure 3a-b). The LSVC was not connected to the coronary sinus, but led directly to the left atrium; the result was mild, asymptomatic hypoxia.
Figure 3.
Computed tomographic angiogram
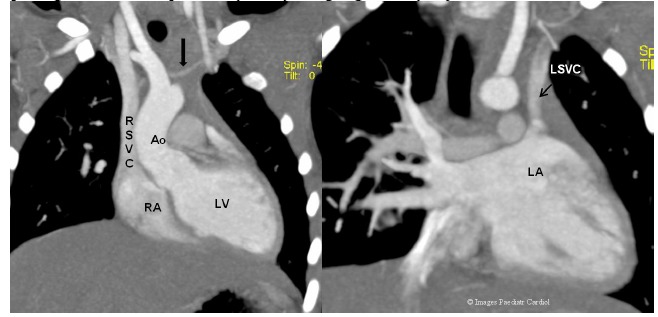
a. Right SVC connecting right atrium. There was a small connecting vein between the right and left SVCs (marked by dark arrow).
b. Left SVC connecting to roof of left atrium (instead of the coronary sinus).It was passing anterior to left pulmonary artery and going medially to join roof of left atrium.
Indications for correction of LSVC to left atrium re prolonged, chronic hypoxia and the chances of systemic embolism, commonly cerebral. Though child was apparently asymptomatic but there was a definite fall in oxygen saturation after walking and so family was counselled about the indication of elective closure. As there was small innominate vein we planned for cardiac catheterization, occlusion test of the LSVC and if there no significant rise in SVC pressure, device closure of LSVC.
Procedure: Percutaneous closure of LSVC was done under sedation, prophylactic intravenous antibiotic as per protocol and systemic heparization. Special care was taken to avoid air embolization during the procedure. The procedure was performed from right femoral vein access while left sided venous pressure was monitored via left brachial vein access (figure 4a).
Figure 4.
During cardiac catheterization,
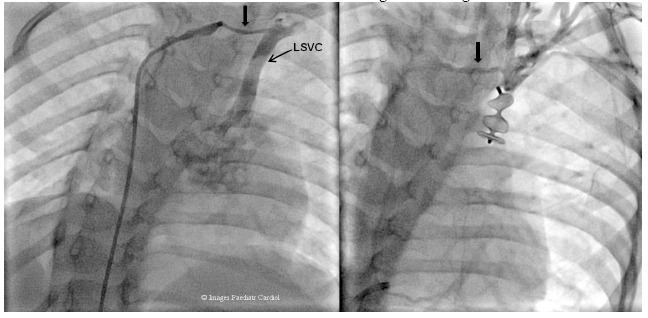
a. Injection in innominate vein showing LSVC connecting to left atrium.
b. Amplatzer vascular plug deployed in left SVC. Post vascular plug deployment, injection in left brachial vein showed filling of right SVC and complete occlusion of left SVC. Innominate vein is taking blood to right SVC
The diameter of the LSVC was 6.6 mm, a 10 mm Amplatzer vascular plug was deployed successfully after hemodyanamic assessment (table 1).
Table 1.
Hemodyanamic data: Basal
| Site | Sys | Dia | Mean | Sat | PO2 |
|---|---|---|---|---|---|
| Right SVC | a8 | v4 | 3 | 69 | |
| RA | a8 | v3 | 3 | 70 | |
| RV | 22 | 8 | - | 70.5 | |
| PA | 12 | 5 | 6 | 69.4 | |
| Femoral Artery | 115 | 82 | 95 | 90 | 72 |
| Left brachial vein | a7 | v4 | 3 |
Post device deployment venous pressure was 7 mmHg (table 2) and on contrast injection in the left brachial vein, there was no flow through the device, no evidence of venous congestion and good flow in innominate vein to right SVC (figure 4b).
Table 2.
Hemodyanamic data: Post device deployment
| Site | Sys | Dia | Mean | Sat | PO2 |
|---|---|---|---|---|---|
| Right SVC | 9 | 4 | 4 | 71 | |
| Femoral artery | 115 | 82 | 95 | 99 | 108 |
| Left brachial vein | 12 | 6 | 7 |
Post procedure echocardiography with contrast injection of agitated saline in left arm showed filling of right SVC to right atrium with no filling of left atrium (figure 5). The child was discharged on anti-platelet therapy (Tab ecospirin 50 mg once daily).
Figure 5.
Contrast echocardiography with agitated saline from left arm after the procedure showed filling of right atrium and no evidence of contrast in left atrium.
Discussion
Persistent LSVC is the most common variation of systemic venous system.1–4 In general, only cases with abnormal drainage and resultant right to left shunting are of clinical significance. The majority (90%) of persistent LSVCs drain into the coronary sinus, with a small portion of the remainder (0.03% of the population) draining into the left atrium because of partial or total unroofing of the coronary sinus.1,5 The condition is usually an incidental finding during central venous access for device therapy or during echocardiography, when an enlarged coronary sinus appears unexpectedly. When a LSVC is connected to left atrium, it is detected as part of evaluation for cyanosis or cerebrovascular accident.6,7
In our patient, a LSVC connected to the roof of the left atrium with intact coronary sinus. It is thought that the embryological anomaly of the left superior vena cava connecting into the left atrium cannot exist with a normal coronary sinus.5,8,9 LVSC is produced when the left common cardinal vein and the left sinus horn are incorporated into the right atrium during invagination of the sinus horns and the left atrium. Failure of this invagination allows the left superior vena cava to remain connected to the left atrium and makes development of the coronary sinus impossible. If this were true then an atrial septal defect of the coronary sinus type should be present in every case. This finding is not present in all reported cases. On reviewing the literature we could find only two cases reported by Wiles HB.10 In the discussion, he explained the association of left superior vena cava with left atrium and normal coronary sinus. A connection between the left cardinal vein and left atrium remains (similar to an unroofed coronary sinus) while the distal coronary sinus develops normally. The left superior vena cava retains this connection to the left atrium but loses its connection to the coronary sinus. There is no obvious reason for the coronary sinus to become involved when the left common cardinal vein retains a connection with the left atrium.
To differentiate this systemic vein which we are labelling as true left superior vena cava from ‘vertical vein’ and ‘levoatriocardinal vein’:
LSVC connected to the roof of the left atrium, did not connect to or drain the pulmonary veins,
LSVC passed in front of the left pulmonary artery and aortic arch, and
LSVC connected to the left subclavian vein and with small innominate connecting it to right SVC.
“Vertical veins” and “levoatriocardinal veins” do not have these characteristics. In addition, the coronary sinus was clearly seen by echocardiography.
We thus report one patient with a truly persistent left superior vena cava connected directly to the left atrium in association with a normally formed coronary sinus and no other structural cardiac defect. The hemodynamic result of right to left shunt was mild desaturation at rest which increased after exercise. Treatment options were: 1. Medical follow up, 2. surgical rerouting of LSVC to right atrium/left sided Glenn and 3. Device closure of LSVC after occlusion test. We planned to close the LSVC percutaneously as it is less invasive with less morbidity and good success rates. Percutaneous closure of the LSVC was done by Amplatzer vascular plug successfully.
Conclusion
Isolated LSVC to left atrium with intact coronary sinus is an extremely rare cause of systemic desaturation without significant murmur. Closure/rerouting is needed to correct systemic desaturation and avoid the risk of cerebrovascular embolism. Percutaneous closure is a less invasive option to correct the anomaly but documenting normal RSVC and balloon occlusion test is must before closing the LSVC.
References
- 1.Perloff JK. Congenital anomalies of vena caval connection. In: The clinical recognition of congenital heart disease. 4th ed. Philadelphia: WB Saunders; 1994. p. 703–14. [Google Scholar]
- 2.Pahwa R, Kumar A. Persistent left superior vena cava: an intensivist’s experience and review of the literature. South Med J 2003;96(5):528–9. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Juanatey C, Testa A, Vidan J, Izquierdo R, Garcia-Castelo A, Daniel C, Armesto V. Persistent left superior vena cava draining into the coronary sinus: report of 10 cases and literature review. Clin Cardiol 2004;27(9):515–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campbell M, Deuchar DC. The left-sided superior vena cava. Br Heart J 1954;16:423-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raghib G, Ruttenberg HD, Anderson RC, Amplatz K, Adams P Jr, Edwards JE. Termination of left superior vena cava in left atrium, atrial septal defect, and absence of coronary sinus; a developmental complex. Circulation 1965; 31:906–18. [DOI] [PubMed] [Google Scholar]
- 6.Meadows WR, Sharp JT. Persistent left superior vena cava draining into the left atrium without arterial oxygen unsaturation. Am J Cardiol 1965;16:273–9. [DOI] [PubMed] [Google Scholar]
- 7.Dehghani P, Benson LN, Horlick EM. Transcatheter closure of persistent left sided superior vena cava draining into left atrium - importance of balloon test occlusion. J Invasive Cardiol 2009; 21(7):E122–5. [PubMed] [Google Scholar]
- 8.Lucas RV. Anomalous venous connections, pulmonary and systemic. In: Adams FH, Emmanouilides GC, eds. Moss’ heart disease in infants, children, and adolescents. 3rd ed. Baltimore: Williams and Wilkins, 1983:458-91. [Google Scholar]
- 9.Sherman FE. An atlas of congenital heart disease. Philadelphia:Lea and Febiger, 1963:67-8. [Google Scholar]
- 10.Wiles H B. Two cases of left superior vena cava draining directly to a left atrium with a normal coronary sinus. Br Heart J 1991; 65:158-60 [DOI] [PMC free article] [PubMed] [Google Scholar]


