Abstract
Objective
With the inclusion of a dissociative subtype, recent changes to the DSM-5 diagnosis of PTSD have emphasized the role of dissociation in the experience and treatment of the disorder. However, there is a lack of research exploring the clinical impact for highly dissociative groups receiving treatment for PTSD. The current study examined the presence and clinical impact of a dissociative subtype in a sample of individuals receiving treatment for chronic PTSD.
Method
This study utilized latent transition analyses (LTA), an expanded form of latent profile analyses (LPA), to examine latent profiles of PTSD and dissociation symptoms before and after treatment for individuals (N = 200) receiving prolonged exposure (PE) or sertraline treatment for chronic PTSD.
Results
The best fitting LTA model was one with a four class solution at both pre-treatment and post-treatment. There was a latent class at pre-treatment with higher levels of dissociative symptoms. However, this class was also marked by higher reexperiencing symptoms, and membership was not predicted by chronic child abuse. Further, while those in the class were less likely to transition to the responder class overall, this was not the case for exposure-based treatment specifically.
Conclusion
These findings are not in line with the dissociative-subtype theoretical literature that proposes those who dissociate represent a clinically distinct group that may respond worse to exposure-based treatments for PTSD.
Keywords: PTSD, dissociative subtype, reexperiencing, complex, prolonged exposure, sertraline
The most recent edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; APA, 2013) includes a dissociative subtype of PTSD marked by symptoms of derealization (e.g., feeling like you are in a dream) and depersonalization (e.g., feeling like you are outside of your body) and removes PTSD from the category of anxiety disorders. This change suggests that dissociation represents a type of pathology distinct from fear-based reactions to trauma. However, evidence is lacking demonstrating that those who dissociate are clinically distinct and that this distinction impedes their capacity to benefit from evidence-based treatments for PTSD. Foundational principles for creating a psychiatric diagnostic framework posit the necessity of clearly delineating symptoms to justify the demarcation of types of mental health syndromes (Robins & Guze, 1970). The current manuscript tests the theory that the dissociative subtype represents a distinct type of PTSD by examining how well dissociative symptoms discriminate from PTSD symptoms and whether those who dissociate share a distinct etiology and differential treatment response from those with PTSD alone.
Dissociation is a broad term encompassing alterations in thoughts, feelings, and behaviors thought to relate to an inability to integrate objective experience into conscious awareness (Putnam, 1991). Dissociative experiences include feelings of depersonalization, derealization, gaps in awareness of current or past events, and absorption, or reduced awareness of one’s current surroundings (Waller, Putnam, & Carlson, 1996). The DSM-5 definition of dissociation related to dissociative disorders is, “a disruption of and/or discontinuity in the normal integration of consciousness, memory, identity, emotion, perception, body representation, motor control, and behavior” (APA, 2013, p. 291).
For over a century, dissociation has been theorized to relate to trauma (see van der Hart & Horst, 1989) and higher rates of dissociation are found for those with trauma-related pathology (i.e., PTSD) compared to other pathological and non-pathological groups (e.g., Bremner et al., 1992; Carlson, Dalenberg, & McDade-Montez, 2012; Yehuda et al., 1996). Long-held clinical theory suggests that dissociation relates to fragmented trauma memories and leads to PTSD through disrupting processing of trauma memories (van der Kolk, van der Hart, & Marmar, 1996). However, a more recent review suggests there is weak evidence for the memory fragmentation hypothesis (see, Bedard-Gilligan & Zoellner, 2012). A theory derived from brain imaging studies suggests those with PTSD who dissociate show distinct neural processes reflective of an emotion regulation deficit, where the prefrontal cortex over-modulates the limbic system (for a review, see Lanius et al., 2010). These data are often referenced in support of a dissociative subtype (Dalenberg & Carlson, 2012; Lanius et al., 2010; Lanius, Brand, Vermetten, Frewen, & Spiegel, 2012; Steuwe, Lanius, & Frewen, 2012). However, because brain imaging studies generally measure state dissociative experiences, as opposed to chronic dissociation, and tend to have small sample sizes, it is difficult to generalize these findings to the broader dissociative subtype literature.
Alternative theories of dissociation suggest trauma processing does not play a causal role in the development of dissociative symptoms. For example some theories suggest that dissociation is unrelated to traumatic experience and instead reflective of cognitive deficits, poor sleep, or even a tendency toward fantasy (e.g., Lynn, Lilienfeld, Merckelbach, Giesbrecht, & van der Kloet, 2012). These theories point toward evidence that those who dissociate may be prone to pseudo memories of trauma (Giesbrecht, Lynn, Lilienfeld, & Merckelbach, 2008) or executive functioning deficits (Giesbrecht, Merckelbach, Geraerts, & Sweets, 2004) that suggest the link between retrospective report of trauma and dissociative symptoms is unreliable.
It may be difficult to establish a clear link between dissociation and PTSD because dissociation is often conceptualized in a variety of ways. For example, “detachment” symptoms of dissociation, like depersonalization and derealization, are thought to be separate from “compartmentalization” symptoms, like amnesia (Holmes et al., 2005), while other symptoms, like absorption and mindlessness, are conceptualized as phenomena distinct from pathological dissociative symptoms (Waller et al., 1996). However, high correlations between these separate dissociative symptom dimensions potentially refutes their distinction (Bernstein, Ellason, Ross, & Vanderlinden, 2001). Indeed, some have proposed that conceptualizing dissociation as a single spectrum of symptoms has more clinical utility than measuring separate dimensions of dissociation (Ruiz, Poythress, Lilienfeld, & Douglas, 2008). It remains unclear how exactly to best measure dissociative symptoms and conceptualize their relationship to PTSD symptoms. The dissociative subtype, as included in the DSM-5, is one such theorized conceptualization that suggests symptoms of depersonalization and derealization, specifically, indicate a different type of trauma-related disorder.
A recent line of research investigating a dissociative subtype in PTSD uses an advanced, iterative statistical approach known as finite mixture modeling (FMM). Two similar forms of FMM that are used to predict latent symptom distributions that are thought to reflect underlying classes of individuals are called latent class analyses (LCA) and latent profile analyses (LPA). A recent review identified eleven studies using LPA or LCA to examine latent profiles of PTSD and dissociative symptoms (Hansen, Ross, & Armour, 2017). A consistent finding throughout this literature is the identification of a class of individuals displaying greater symptoms of both PTSD and dissociative symptoms (Armour, Elklit, Lauterbach, & Elhai, 2014; Armour, Karstoft, & Richardson, 2014; Blevins, Weathers, Davis, Witte, & Domino, 2015; Frewen, Brown, Steuwe, & Lanius, 2015; Hansen, Hyland, & Armour, 2016; Hansen, Mullerova, Elklit, & Armour, 2016; Mullerova, Hansen, Contractor, Elhai, & Armour, 2016; Steuwe, Lanius, & Frewen, 2012; Wolf et al., 2012a; Wolf et al., 2012b; Wolf et al., 2017). This review concludes that there is evidence to substantiate the existence of the dissociative subtype based on the fact that a dissociative class was identified in the majority of the studies, and even though the evidence is sparse or mixed, the review also concludes that child abuse is a likely etiological factor and PE is a potentially effective treatment for those who dissociate.
Although Hansen et al. (2017) suggests that the presence of a latent class is synonymous with a subtype, the theoretical foundation for a dissociative subtype suggests additional evidence is needed to distinguish a latent class from a subtype of a disorder. To meet the standard of a dissociative subtype, it should be shown that the symptoms distinguishing the class (i.e., dissociation) are not simply a reflection of increased pathology of the broader construct (i.e., PTSD; Dalenberg & Carlson, 2012). Further, the class of individuals should be distinguished by a differing etiology and differential treatment response (Dalenberg, Glaser, & Alhassoon, 2012). However, contrary to these theoretical assumptions, multiple LPA studies have found the dissociative class to also be distinguished by higher PTSD severity (e.g., Armour et al., 2014; Armour et al., 2014; Frewen et al., 2015; Mullerova et al., 2016); no consistent etiological covariate has been identified thus far (see Hansen et al., 2017); and only one study has examined treatment response for the dissociative class (Wolf, Lunney, & Schnurr, 2016). Due to their prominence in the theoretical literature, but lack of clear evidence in the empirical literature, the current manuscript seeks to critically examine these assumptions in a clinical sample.
The most commonly proposed etiological risk factor for developing dissociative PTSD is the experience of chronic abuse in childhood (Cloitre et al., 2009; Cook et al., 2005; Pearlman & Courtois, 2005; van der Kolk, Roth, Pelcovitz, Sunday, & Spinazzola, 2005). Only three LPA studies found that the dissociative class showed higher rates of child abuse compared to the other classes (Frewen et al., 2015; Steuwe et al., 2012; Wolf, et al., 2012b), with one of those studies (Steuwe et al., 2012) being conducted with a majority child abuse sample. Three LPA studies found no differences for past child abuse (Armour et al., 2014; Blevins et al., 2015; Wolf et al., 2017), one found no differences for past sexual trauma (Wolf et al., 2012a) and two did not report past traumatization (Armour et al., 2014; Mullerova et al., 2016). These mixed results from LPA studies suggest more research is needed to fully substantiate past trauma as a predictor of a dissociative class of PTSD. Substantiating this etiological marker is especially important given concerns regarding retrospective reporting biases for those who dissociate and empirically-based models of dissociation that do not include traumatic experience (see Lynn et al., 2012).
The main theorized treatment implication for the dissociative subtype is a reduced tolerance of exposure-based treatment (e.g., Cloitre, Petkova, Wang, & Lu, 2012). Only one LPA examined treatment response for those in the dissociative class and found that while the dissociative class showed slightly reduced rates of PTSD change overtime for the sample as a whole, there were no moderating effects for treatment type (Wolf et al., 2016). Specifically, those in the dissociative class receiving an exposure-based intervention were just as likely as those receiving a non-exposure-based treatment to respond. Furthermore, both treatments in this study were effective in reducing dissociative symptoms along with PTSD symptoms for the highly dissociative class. An additional, non-LPA study showed that those with high dissociation maintained elevated dissociation after completing emotion regulation and exposure-based treatments, but there was no effect of baseline dissociation on post-treatment PTSD severity for any of the treatment groups (Cloitre et al., 2012). These findings are consistent with a larger body of literature showing that high levels of dissociation symptoms do not predict worse outcomes for exposure-based therapies for PTSD, above and beyond PTSD symptom severity (e.g., Hagenaars, van Minnen, & Hoogduin, 2010; Speckens, Ehlers, Hackmann, & Clark, 2006), and that dissociation reduces along with PTSD symptoms in response to evidence-based treatment approaches (e.g., Chard, 2005; Cloitre, Koenen, Cohen, & Han, 2002). In fact, some treatment outcome data suggests that those with high levels of dissociation may actually respond better than those with low dissociation to therapy that includes an exposure component (Resick, Suvak, Johnides, Mitchell, & Iverson, 2012).
Consistent with the cognitive-behavioral therapy literature, treatment of PTSD using pharmacotherapy, specifically paroxetine, has also been shown to reduce symptoms of dissociation (Marshall et al., 1998; Marshall et al., 2007), potentially arguing that dissociation is a symptom rather than a subtype of PTSD that is alleviated by effective treatments for PTSD. However, there is a lack of data examining a dissociative subtype or dissociative symptoms in general in samples of individuals receiving pharmacotherapy for PTSD. Given that sertraline is one of two FDA approved medications for PTSD and is generally considered efficacious (Ipser & Stein, 2012; Watts et al., 2013), it provides an ideal comparison treatment to assess whether mechanisms specific to exposure-based therapy impact dissociation in treatment for PTSD.
The largely cross-sectional LPA data suggestive of a dissociative subtype do not correspond to the emerging longitudinal treatment data showing little to no negative effects of dissociation on treatment outcome for PTSD. If the dissociative subtype is indeed resistant to exposure-based treatment, evidence should show that those classified in this subtype are less likely to respond to such treatments compared to non-exposure-based treatments. The current study combined LPA methods with longitudinal methods to explore transitions between latent classes across prolonged exposure (PE) versus sertraline treatment for PTSD.
The first aim of this study was to identify groups of individuals that differed based on PTSD and dissociation symptoms and determine whether past traumatic experience predicted membership in these groups. We hypothesized that similar to previous LPA findings, we would identify a latent class of individuals distinguished by high levels of dissociative and PTSD symptom severity. In addition, we hypothesized that the experience of chronic child abuse would predict membership in this highly dissociative latent class.
The second aim was to examine whether a dissociative latent class would respond differentially to exposure-based treatment compared to pharmacological intervention. In line with Resick et al.’s (2012) findings showing that higher dissociation predicted better outcomes in exposure-based therapy compared to non-exposure-based-therapy, we hypothesized that those in the dissociative latent class would be more likely to transition to a responder class, with low levels of PTSD and dissociation symptoms, in prolonged exposure compared to those in the dissociative latent class receiving sertraline.
Method
Participants
The sample consisted of 200 men and women with chronic PTSD. Demographics, trauma type, and baseline psychopathology information are presented in Table 1 and did not differ between treatment groups. Participants were recruited through community referrals, fliers and advertisements as part of a randomized controlled treatment trial examining the effect of treatment preference on treatment outcome for PE versus sertraline. Inclusion criteria for the treatment trial included: being between the ages of 18 and 65 years, and having a DSM-IV diagnosis of primary, chronic PTSD. Exclusion criteria included: current diagnosis of schizophrenia or delusional disorder; medically unstable bipolar disorder, depression with psychotic features, or severe enough to require immediate psychiatric treatment (e.g., actively suicidal); severe self-injurious behavior or suicide attempt within three months; no clear trauma memory or trauma before age of three; current diagnosis of alcohol/ substance dependence within three months; ongoing intimate relationship with assailant (in assault cases); unwilling or medically not advisable to stop current CBT or antidepressant, based on condition assignment; previous non-response to adequate trial of PE (8 sessions or more) or sertraline (150 mg/d; 8 wks); or medical contraindication for sertraline (e.g., pregnancy). Participants in the study who were on any psychotropic medications at baseline had to be stable for three months to be eligible. Participants in PE were asked to maintain, at the same level, current medications until the 10-week active treatment phase of the study was completed. Participants in sertraline who were already on an antidepressant were withdrawn from the medication under the supervision of their study psychiatrist, active treatment with sertraline began after participants had been free of psychotropic medications for 1 to 2 weeks.
Table 1.
Demographics and Trauma Type
| Variable | N /M | %/SD |
|---|---|---|
| Age (years) | 37.41 | 11.30 |
| Gender | ||
| Female | 151 | 76.0 |
| Male | 49 | 24.0 |
| Education | ||
| College Educated | 60 | 30.0 |
| Not College Educated | 140 | 70.0 |
| Ethnicity | ||
| Caucasian | 130 | 65.0 |
| Minority status | 70 | 35.0 |
| Primary Trauma Type | ||
| Adult sexual assault | 62 | 31.0 |
| Adult non-sexual assault | 45 | 23.0 |
| Childhood sexual assault | 35 | 18.0 |
| Childhood non-sexual assault | 13 | 06.0 |
| Other | 45 | 22.0 |
| Baseline Pathology | ||
| PTSD symptoms (PSS-I) | 29.57 | 6.69 |
| Dissociation symptoms (DES) | 16.59 | 13.67 |
Note. PSS-I = PTSD Symptom Scale Interview; DES = Dissociative Experiences Scale
Interview Measures
PTSD Symptom Scale-Interview (PSS-I; Foa, Riggs, Dancu, & Rothbaum, 1993)
The PSS-I was used to assess current PTSD diagnosis and severity. This 17-item interview measure uses DSM-IV symptom criteria measuring severity of PTSD symptoms related to a single, target trauma. Each item is rated on a four-point Likert scale ranging from 0 (not at all) to 3 (5 or more times per week/ very much) based on frequency and/or severity in the past two weeks, with higher levels indicating greater PTSD severity. The PSS-I demonstrates good convergent validity and excellent inter-rater reliability, ρ = .93 (Foa, Cashman, Jaycox, & Perry, 1997; Foa & Tolin, 2000). In the current study, over 10% of cases were rerated for inter-rater reliability; reliability was high for PTSD severity scores (ICC = .95) and PTSD diagnosis (κ = 1.00).
Structured Clinical Interview for DSM-IV (SCID-IV; First, Spitzer, Gibbon, & Williams, 2002)
The SCID-IV, a semi-structured interview, was used to determine eligibility and if other Axis I disorders were primary. This measure has good inter-rater reliability (Lobbestael, Leurgans, &Arntz, 2011). In the current study, 10% of the SCID-IVs were rerated for inter-rater reliability; reliability across current diagnoses was acceptable (κ = .80).
Prior Trauma History (adapted from Resnick, Best, Freedy, Kilpatrick & Falsetti, 1993)
This is a measure of past trauma experiences. History of chronic childhood assault (CCA) was defined as experiencing five or more separate assaults in childhood according to a count variable. Three variables were derived: experiencing chronic childhood physical assault (CCPA), chronic childhood sexual assault (CCSA), and any chronic childhood assault (CCA; physical, sexual or both). In our sample, 33% (n = 66) experienced a history of CCPA, 17% (n = 34) experienced a history of CCSA and 39% (n = 78) experienced a history of CCA. These chronic abuse variables derived from this measure were able to capture every individual in our sample who reported an instance of chronic child abuse as their index trauma (n = 28, 14%).
Self-report Measures
Dissociative Experiences Scale (DES- Bernstein & Putnam, 1986)
The DES is a 28-item self-report questionnaire designed to measure the continuum of dissociative experiences including disturbances in identity, memory, awareness, and cognitions as well as experiences of depersonalization, derealization, and absorption. Items are presented on a visual analogue scale. Individuals respond by making a slash across a 100 mm long line to indicate agreement with the item. No time frame is specified in the instructions, likely reflecting trait rather than acute dissociation. Scores are derived by averaging responses creating a total score between 0 and 100, with higher scores indicating greater pathology. Scores of 10 or below are believed to indicate non-pathological dissociation while scores of 30 or above indicate pathological dissociation (Bernstein, Putnam, & Ross, 1993). The DES has good test-retest reliability (r = .84), good split half reliability (Bernstein & Putnam, 1986), and adequate convergent validity (Carlson, Bernstein, Putnam, 1993). The depersonalization/derealization subscale of the DES (DES-D; Carlson et al., 1991) is comprised of individual items from the DES representing the symptoms specified in the DSM-5 as a marker for the dissociative subtype. The DES-Taxon (DES-T; Waller et al., 1996) is comprised of 8 items from the DES (including those items from the DES-D) that have been shown to have a taxometric distribution indicating a distinct type of severe dissociative experience. Main analyses were conducted using the DES-D in order to replicate previous findings and reflect the clinical description of the dissociative subtype.
Procedure
The study was approved by the Institutional Review Board of the academic centers affiliated with the authors and listed as a clinical trial on clinicaltrials.gov. Participants were initially screened over the phone using a semi-structured phone interview. Those who were potentially eligible then underwent an in-person intake interview to determine eligibility for the study. The intake interview consisted of informed consent and diagnostic assessments conducted by trained independent evaluators. Interview measures included the PSS-I to diagnose PTSD and the SCID-IV to diagnose other comorbid psychopathology. Participants also completed a battery of self-report questionnaires including the DES prior to starting treatment. Eligible individuals were randomized and then received 10 weekly sessions of PE or sertraline treatment. After acute treatment, a post-treatment assessment was conducted by an independent evaluator blind to treatment condition during which PTSD symptom severity (PSS-I) was assessed. Participants also completed self-report measures at their post-treatment assessment including the DES. Participants were reassessed at 3−, 6−, 12−, and 24-month follow up.
Overview of Treatment
Treatment consisted of either 10 sessions of psychotherapy or pharmacotherapy. For psychotherapy, clinicians had at least Master’s level clinical training. Clinicians received standardized clinical training, through multiple-day initial training workshops and ongoing clinical supervision. For pharmacotherapy, clinicians were board certified psychiatrists.
Psychotherapy
Prolonged exposure (PE; Foa, Hembree, & Dancu, 2002) consisted of 10 weekly, 90–120 min sessions, which included psychoeducation involving common reactions to trauma exposure, breathing retraining, approaching avoided situations outside of therapy (i.e., in vivo exposure) starting in Session 2, and approaching the memory of the trauma repeatedly (i.e., imaginal exposure) beginning at Session 3. Clients were assigned weekly homework including listening to their imaginal exposure tape and practicing in vivo exposure exercises. Trained, outside raters reviewed 10% of videotaped sessions, assessing essential treatment components and protocol violations. PE therapists completed 90% of essential components, and there were no protocol violations observed.
Pharmacotherapy
Pharmacotherapy consisted of 10 weeks of sertraline, monitored by a study psychiatrist. Each session was approximately 30 min, with the first session lasting approximately 45 min. Sertraline was adjusted based on a standardized titration algorithm (Brady et al., 2000), starting at 25mg/day and proceeding up to 200mg/day, if indicated. During visits, the psychiatrist monitored side effects and adjusted medication dosage as well as provided general encouragement and support. For treatment responders, the final dosage was maintained and monitored through follow-up. Trained raters reviewed 10% of videotaped sessions, assessing essential treatment components and protocol violations. Pharmacotherapists completed 96% of essential components, and there were no protocol violations observed.
Data Analyses
Latent transition analysis (LTA) was conducted to identify transition probabilities between latent variables at pre- and post-treatment, controlling for the effect of treatment type, using Mplus 7 (Muthén & Muthén, 2015). Specifically, a three-step LTA approach (Asparouhov & Muthén, 2014) was used in which: first, latent profile analysis (LPA) was used to identify latent class estimates; second, individuals were assigned to their most probable latent class; and third, LTA was conducted to identify transition probabilities between classes controlling for the misclassification rate within each latent class and any covariates in the model. Indices of model fit were used to compare LPA class solutions, using a sample adjusted Bayesian information criteria (BIC), Akaike information criteria (AIC), the bootstrap likelihood ratio test (BLRT), and the Lo-Mendell-Ruben adjusted likelihood ratio test (LMR-A). Both BLRT and LMR-A compare the fit of a given model with a model of one fewer classes. Additionally, entropy was assessed using a summary measure of the probability of membership in the most-likely class for each individual. Entropy values range from 0 to 1.0, and values closer to 1.0 represent better classification and thus a smaller likelihood that individuals will be misclassified as they are not likely to be close to the borderline of a given class parameter. Previous research suggests that BIC and BLRT are superior fit indices (Nylund, Asparouhov, & Muthén, 2007). Thus, the best approach when interpreting LPA is to first identify the lowest BIC value for a model and then see if the BLRT is significant and examine entropy.
LPA was first used to identify the best fitting model for baseline scores. The best fitting baseline model was then extended into an LTA model, in which pre-treatment class structure was fixed according to the baseline LPA solution, while the post-treatment class structure was estimated based on the LTA model. This LTA model included the pre-treatment nominal class variable as well as the dummy coded grouping variable of treatment type (PE or sertraline). The best fitting LTA model was identified based on comparisons using the likelihood ratio test (Nylund, 2007). By modeling the post-treatment latent variable in the LTA model (as opposed to a separate LPA model in step-1), we were able to estimate post-treatment parameters for the entire intent-to-treat sample. Posthoc logistic regression analyses were conducted to examine the effect of pre-treatment class membership on post-treatment class membership. Power to detect effects was determined based on simulation studies (Dziak, Lanza, & Tan, 2014; Tein, Coxe, & Cham, 2013) suggesting that given the large number of indicators in our LPA (18) in conjunction with the degree of separation between classes (Cohen’s d = 0.46), and the relatively small influence of sample size on statistical power in LPA, our sample size of 200 was sufficiently powered to detect effects and to replicate previous findings.
Results
Baseline LPA
In the first step of the analyses, each individual item from the PSS-I and the average score from the DES-D at baseline were entered into separate LPAs testing model fit for two, three, four and five class solutions. Fit statistics for each class solution from the baseline model are presented in Table 2. The four-class solution was the best-fitting model for the data as it showed the lowest BIC value, a significant BLRT value, and high entropy, suggesting that the classes derived from this model were structurally sound and that there were few people with ambiguous class membership estimates. The best log-likelihood value was not replicated in the five-class solution even with increased random starts, suggesting that this model was attempting to extract too many classes. Although the DES-D was utilized for all analyses, it should be noted that the DES-total score and DES-Taxon score produced very similar parameter estimates and class sizes in separate LPAs compared to the DES-D score and were similarly correlated to PTSD symptoms at baseline (r = .30 for DES-total, .25 for DES-taxon, and .28 for DES-D), suggesting these multiple symptom factors reflected a similar dissociative phenomenon in this sample.
Table 2.
Fit of Competing Class Models for DES-D and PSS-I
| Model | Log-Likelihood | AIC | BIC-adj | Entropy | BLRT p-value |
LMR-A p-value |
|---|---|---|---|---|---|---|
| 3 Class | −5418.216 | 10,984.432 | 10,994.068 | .80 | <.001 | .47 |
| 4 Class | −5353.534 | 10,893.068 | 10,905.177 | .89 | <.001 | .42 |
| 5 Class | Best Log-Likelihood was NOT replicated | |||||
Note. AIC = Akaike information criteria; BIC-adj = Bayesian information criteria-sample size adjusted; BLRT = bootstrap likelihood ratio test; LMR-A = Lo-Mendell-Rubin, adjusted likelihood ratio test
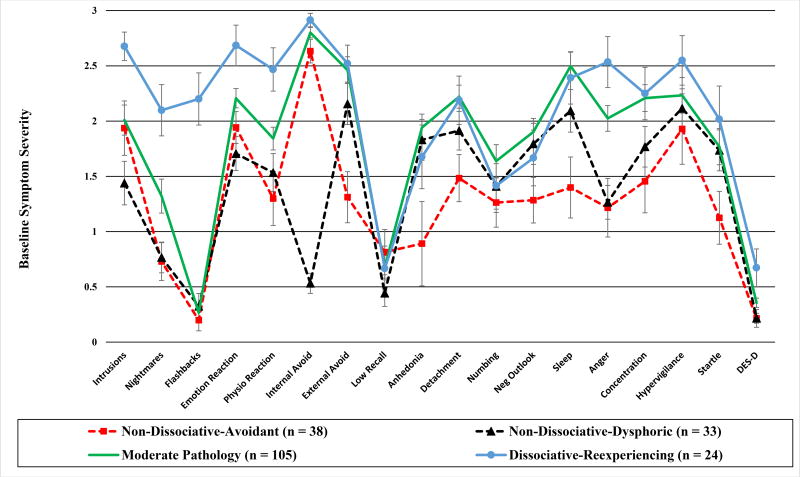
Symptom Profiles
In the second step, a nominal class variable was created which assigned individuals to their most probable latent class. Figure 1 depicts the estimated profiles for each of the 4 latent classes at baseline. Each class was labeled based on their profile. At baseline, two classes were identified with low dissociation but different PTSD symptom profiles. The first, labeled non-dissociative-avoidant, made up 19% of the sample and the other, labeled non-dissociative-dysphoric, made up 17% of the sample. The majority of the sample (52%) was captured in a class labeled moderate psychopathology due to higher severity of dissociation and several PTSD symptoms compared to the two non-dissociative classes. The final class was the smallest class (12%) and showed higher dissociation and re-experiencing symptoms compared to the next adjacent class (see Table 3) and was thus labeled the dissociative-reexperiencing class.
Figure 1.
Estimated Baseline Latent Profiles for PTSD and Dissociation Symptoms
Note. DES-D = Dissociative Experiences Scale-Depersonalization/Derealization subscale. It was rescaled from 0–100 to 0–3 to be included in the figure
Table 3.
Separation between Moderate-Pathology and Dissociative-Reexperiencing Classes
| LPA Indicators | Mean (SD) Moderate- Psychopathology (n = 105) |
Mean (SD) Dissociative- Reexperiencing (n = 24) |
Magnitude of difference (Cohen’s d) |
|---|---|---|---|
| Intrusions | 2.01 (1.39)a | 2.68 (0.62)b | 0.62 |
| Nightmares | 1.32 (1.58)a | 2.10 (1.11)b | 0.57 |
| Flashbacks | 0.27 (0.67)a | 2.20 (1.13)b | 2.08 |
| Emotional Reaction | 2.21 (0.89)a | 2.69 (0.88)b | 0.54 |
| Physical Reaction | 1.84 (1.06)a | 2.47 (0.94)b | 0.62 |
| Internal Avoidance | 2.80 (0.48)a | 2.91 (0.29)a | 0.29 |
| External Avoidance | 2.46 (1.24)a | 2.52 (0.80)a | 0.06 |
| Low Recall | 0.68 (1.05)a | 0.67 (0.97)a | 0.01 |
| Anhedonia | 1.94 (1.25)a | 1.68 (0.54)a | 0.28 |
| Detachment | 2.22 (1.07)a | 2.19 (1.05)a | 0.03 |
| Numbing | 1.64 (1.53)a | 1.41 (1.16)a | 0.16 |
| Negative Outlook | 1.90 (1.25)a | 1.67 (1.21)a | 0.19 |
| Sleep | 2.50 (1.29)a | 2.39 (1.14)a | 0.09 |
| Anger | 2.02 (1.19)a | 2.53 (1.11)a | 0.44 |
| Concentration | 2.21 (1.24)a | 2.25 (1.14)a | 0.03 |
| Hypervigilance | 2.23 (1.65)a | 2.55 (1.07)a | 0.23 |
| Startle | 1.77 (1.68)a | 2.02 (1.44)a | 0.16 |
| DES-D | 11.87 (14.47)a | 22.42 (27.01)b | 0.49 |
Note. Subscripts reflect statistically significant difference.
Although the dissociative-reexperiencing class demonstrated higher severity for each reexperiencing symptom compared to the moderate psychopathology class, the flashback symptom was especially pronounced (Cohen’s d = 2.08, see Table 3). Because flashback symptoms have been shown to load onto a dissociative class in previous studies (Steuwe et al., 2012), separate LPAs were conducted removing dissociation symptoms (DES-D) and flashback symptoms. These findings showed that parameter estimates and sample sizes for each class remained nearly identical when the DES-D symptoms were removed from the analysis. However, when flashback symptoms were removed, there was a large shift in parameter estimates and sample sizes for each class, with the dissociative-reexperiencing class now making up half of the sample (n = 100), with a lower parameter estimate for average dissociation score (M = 14.07, SD = 1.72) and a small effect size difference in dissociative symptoms compared to the moderate psychopathology class (Cohen’s d = 0.09). Taken together these findings suggest that flashbacks, and not chronic dissociation symptoms contribute to the presence of the dissociative-reexperiencing class in this sample.
History of Chronic Child Abuse and Baseline Symptom Profiles
To examine the impact of child abuse on class structure, indices of chronic child abuse (CCSA, CCPA, CCA) were included as dummy coded covariates in three separate LPA analyses regressing the class variable on the covariate, controlling for misclassification rates within each class. Individual regression coefficients and corresponding significance values for the child abuse variables predicting baseline class membership, with the dissociative-reexperiencing class as the reference class, are summarized in Table 4. Contrary to our hypothesis, none of the child abuse variables predicted membership in any baseline latent class.
Table 4.
Logistic Regression of Chronic Child Abuse on Baseline Latent Symptom Profiles
| Coefficients for Categorical Latent Variable Regression (reference class = Dissociative-Reexperiencing) |
|||
|---|---|---|---|
| Estimate | Standard Error | Odds Ratio | |
| Chronic Childhood Physical Assault (CCPA) | |||
| Non-Dissociative-Avoidant | −0.378 | 0.612 | 0.685 |
| Non-Dissociative-Dysphoric | −1.155 | 1.014 | 0.315 |
| Moderate Psychopathology | 0.266 | 0.525 | 1.305 |
| Chronic Childhood Sexual Assault (CCSA) | |||
| Non-Dissociative-Avoidant | −0.567 | 0.695 | 0.568 |
| Non-Dissociative-Dysphoric | −1.976 | 1.842 | 0.139 |
| Moderate Psychopathology | −0.324 | 0.586 | 0.723 |
| CCPA, CCSA or Both | |||
| Non-Dissociative-Avoidant | −0.413 | 0.580 | 0.661 |
| Non-Dissociative-Dysphoric | −1.158 | 0.881 | 0.314 |
| Moderate Psychopathology | 0.051 | 0.506 | 1.053 |
Note. No estimates were statistically significant at the .05 level.
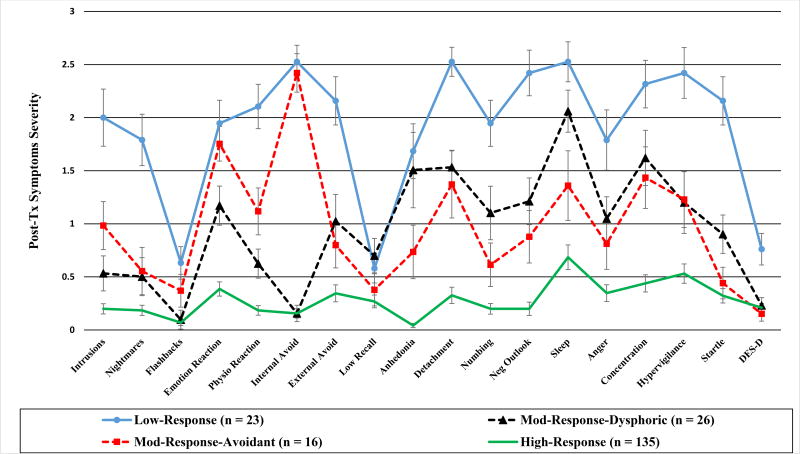
Treatment Effects on Symptom Profiles
In the final step of the LTA, the probability of transitioning out of the dissociative latent class from pre- to post-treatment was examined. Parameters for the baseline model of the LTA were fixed to the 4-class solution identified by the baseline LPA, while the post-class solution was estimated by the LTA model. Separate LTAs were conducted for a model with 2, 3, 4 and 5 class solutions for post-treatment. The best fitting model for the LTA was chosen according to previous methods (Nylund, 2007) by using the likelihood ratio test to compare each LTA model to that of a nested model with one less class at post-treatment. This approach determined the best fitting LTA model was one with a 4-class solution at post-treatment. The profiles for each class at post-treatment are shown in Figure 2. The majority of the intent-to-treat sample at post-treatment (68%) was captured in a class characterized by low PTSD and low dissociative symptoms and was thus labeled the high-response class. The remaining three classes, although similar in structure to pre-treatment classes (e.g., low dissociation and high avoidance), showed reduced PTSD severity rates compared to baseline classes, fundamentally shifting the pathological nature of each class. As such, post-treatment classes are labeled based on their relationship to response (e.g., high response vs low response) as opposed to symptom severity profile.
Figure 2.
Estimated Post-Treatment Latent Profiles for PTSD and Dissociation Symptoms
Note. DES-D = Dissociative Experiences Scale-Depersonalization/Derealization subscale. It was rescaled from 0–100 to 0–3 to be included in the figure
Latent transition probabilities for the likelihood of transitioning from each pre-treatment class to each post-treatment class for the intent-to-treat sample within both treatment conditions are provided in Table 5. Posthoc logistic regression analyses were conducted examining the relationship between being in the dissociative-reexperiencing class at baseline (member vs non-member) and transitioning to the high-response class after treatment (member vs non-member). For the overall intent-to-treat sample, being in the dissociative-reexperiencing class related to a reduced likelihood of transitioning to the high-response class, χ2 (1, N = 200) = 8.297, p = .004. There was a moderation effect of treatment type, OR = 7.24, Wald χ2 (1, N = 200) = 5.81, p = .02, indicating this effect of baseline class on post-treatment class was found for those receiving sertraline, Wald χ2 (1, N = 84) = 1034, p = 001, and not those receiving PE, Wald χ2 (1, N = 116) = 0.03, ns. Sixty-seven percent (8 out of 12) of those assigned to the dissociative-reexperiencing class at baseline, receiving PE would be estimated to transition to the high-response class, while only 17% (2 out of 12) of those in sertraline would follow the same trajectory. However, given the small cell sizes corresponding to the dissociative-reexperiencing transition probabilities (Table 5), caution is warranted when interpreting differences between treatments. This is especially true given that the overall likelihood of transitioning to the high-response class was similar for sertraline (55/84, 65.48%) and PE (80/116, 68.97%), suggesting benefits of sertraline for the other classes may have compensated for any deficiency for the dissociative-reexperiencing class.
Table 5.
Likelihood of Transitioning (Proportion) Between Latent Classes from Pre- to Post-Treatment
| Post-Treatment Symptom Profiles
|
||||
|---|---|---|---|---|
| Mod- Response- Avoidant |
Mod- Response- Dysphoric |
Low- Response |
High- Response |
|
| Prolonged Exposure (116) | ||||
| Non-Dissociative-Avoidant (26) | .15 (4) | .08 (2) | ..04 (1) | .73 (19) |
| Non-Dissociative-Dysphoric (18) | .00 | .11 (2) | .00 | .89 (16) |
| Moderate Psychopathology (60) | .10 (6) | .22 (13) | .07 (4) | .62 (37) |
| Dissociative-Reexperiencing (12) | .17 (2) | 0.00 | .17 (2) | .67 (8) |
| Sertraline (84) | ||||
| Non-Dissociative-Avoidant (12) | .00 | .00 | 0.00 | 1.00 (12) |
| Non-Dissociative-Dysphoric (15) | .07 (1) | .47 (7) | 0.00 | .47 (7) |
| Moderate Psychopathology (45) | .07(3) | .02 (1) | .16 (7) | .76 (34) |
| Dissociative-Reexperiencing (12) | .00 | .08 (1) | .75 (9) | .17 (2) |
Note. Table reflects proportion of baseline class that transitioned to each post-treatment class. Parentheses indicate number of estimated cases corresponding to the estimated probability
In order to supplement the LTA, established indicators of treatment response were compared between baseline and post-treatment classes, with dropouts defined as non-responders. These findings showed that while those in the dissociative-reexperiencing class at baseline were less likely to lose their PTSD diagnosis (37.5%) compared to the rest of the sample (66.5%), χ2 (1, N = 200) = 7.608, p = .006, they did not differ in terms of PTSD symptom severity change across treatment, with an average reduction of 14.38 (SD = 14.64) points compared to 13.81 points (SD = 11.76) points for the rest of the sample, t(198) = 0.21, ns, Cohen’s d = 0.04. Further, this class did not significantly differ in rate of reliable improvement (54.2%) compared to the rest of the sample (65.3%), χ2 (1, N = 200) = 1.15, ns, as measured with a reliable change index for the PSS-I (Jayawickreme et al., 2014), suggesting that those in a dissociative class responded well to treatment. At post-treatment, as expected, the high-response class showed significantly greater reductions in PTSD symptom severity (M = 16.84, SD = 12.64) compared to the rest of the sample (M = 7.74, SD = 8.00), t (198) = 6.18, p < .001, Cohen’s d = 0.86, with high percentages of individuals in the class showing reliable change (71%) and loss of diagnosis (71%).
Discussion
In the present study, four classes of individuals with distinct PTSD and dissociative symptom profiles were identified at baseline, with one class displaying significantly higher reexperiencing and dissociative symptom severity and reduced likelihood of transitioning to a high response class after treatment. Although this class was distinct and clinically informative, additional analyses were not able to fully substantiate this dissociative class as a subtype.
Specifically, the baseline dissociative class was also distinguished by re-experiencing symptoms, which is not in line with the theoretical literature proposing a dissociative subtype that emphasizes the need for dissociation to be a “salient” feature of a subtype, above and beyond PTSD symptom severity (Wolf et al., 2012). The present findings instead showed that removing dissociative symptoms from the model did not alter PTSD symptom profile structure, but removing flashbacks did, suggesting that PTSD symptoms, especially flashbacks, are having a larger effect on baseline class profiles. These findings are in line with recent LPA results for acute stress disorder that found an intrusive class with high dissociation, as opposed to a purely dissociative class, for those recently traumatized (Armour & Hansen, 2015). This is potentially consistent with the view that dissociation may be a reaction to high levels of reexperiencing of a traumatic memory (e.g., Schauer & Elbert, 2015).
The higher rates of flashback symptoms found for the dissociative-reeexperiencing class are in line with factor analytic studies (e.g., Steuwe et al., 2012) that suggest flashbacks load onto dissociation and reexperiencing factors. Notably, significant flashback symptoms were rare in this sample (only predictive of the dissociative-reexperiencing class; 12%), hardly reflecting a commonly experienced symptom. Given the cross-sectional nature of these baseline analyses, it is not possible to determine whether chronic dissociation and flashback symptoms are correlated reactions to certain types of traumatic experiences or whether those prone to dissociation are also prone to highly immersive reexperiencing of a traumatic event. What is clear from these data is that the tendency for dissociation does not interfere with the capacity to engage with a traumatic memory as dissociative individuals report high levels of immersive reexperiencing (i.e., flashbacks). Further, individuals who would be identified as part of the dissociative subtype according to the DSM-5 could just as easily be identified using the standard PTSD criteria (e.g., intrusive memories and flashbacks), calling into question the clinical relevance of the dissociative subtype. Further research is needed examining the temporal relationship between reexperiencing and dissociative symptoms following a trauma, as the current literature is unable to identify whether flashbacks and reexperiencing are a result of dissociation or vice versa.
Chronic abuse, especially in childhood, is often put forward as a possible etiological predictor of dissociative symptoms in proposed new PTSD diagnoses, such as complex PTSD in adults (Cloitre et al., 2009; Maercker et al., 2013) or developmental trauma disorder in children (van der Kolk, 2005). In the current study, the experience of chronic child abuse did not predict membership in a dissociative class, suggesting that this is not a strong etiological marker for a more dissociative type of PTSD. Identification of etiological markers for dissociative PTSD are needed, as this is a key factor to distinguish a subtype model from a component model where dissociation is thought of as an additional symptom of PTSD without unique etiology (Dalenberg & Carlson, 2012). The present findings add to the growing body of null findings (e.g., Armour et al., 2014; Blevins et al., 2015; Wolf et al., 2012a; Wolf et al., 2015), suggesting that chronic child abuse does not predict dissociative PTSD. Yet, null findings do not provide evidence for or against a component model or a subtype model of dissociation in PTSD, given that an untested etiological factor could be explaining dissociative symptoms. Until such a factor is identified, it will not be possible to determine whether a symptom is related to the syndrome of PTSD or represents a distinct subtype of the disorder presentation. However, comparable correlations across dissociative (r = .28) and PTSD symptoms (r = .17 – .46) to overall PTSD severity in this sample, suggests dissociation may be adequately captured by the syndrome of PTSD, at least as well as other PTSD symptoms.
To our knowledge, this study is the first to use LTA to examine differential response of a dissociative class to evidence-based treatments for PTSD. The majority of individuals in the intent-to-treat sample transitioned to the high-response class after receiving either PE or sertraline, and the estimates for PTSD symptom severity parameters reduced for all classes from baseline to post-treatment, indicating efficacy for both treatments. Individuals in the dissociative-reexperiencing class were less likely to transition to the high-response class when receiving sertraline but not in PE. Given the sample size limitations, it is difficult to interpret this interaction effect and replication with larger sample sizes is needed to substantiate treatment comparison findings. For the sample as a whole, individuals in the dissociative re-experiencing class were less likely to transition to the high-response class and to lose their PTSD diagnosis compared to the rest of the sample. However, they demonstrated similar reductions in PTSD symptoms compared to the next most pathological group, suggesting a similar capacity to benefit from evidence-based treatment. The higher baseline PTSD severity for this group made it more difficult for them to reach high-response status even with similar rates of change. In addition, exposure therapy did not lead to a reduced likelihood to transition to the high-response class compared to a non-exposure-based therapy for those who dissociated, suggesting that the recommendation for additional treatment prior to exposure (Cloitre et al., 2012) may not be necessary, in line with other findings (Resick et al., 2012) and recommendations (De Jongh et al, 2016).
These results should be interpreted with several limitations in mind. We used a comprehensive self-report measure of dissociation, as opposed to dissociative items added to a PTSD diagnostic measure. Although the DES shows strong predictive validity for dissociative disorders and traumatic experiences, it shows poor discriminant validity as non-pathological groups also score high. Further, as a face valid self-report measure, it is subject to response biases, such as malingering and participant IQ (van Ijzendoorn & Schuengel, 1996). However, the DES is a well-validated measure of the specific construct proposed in theoretical models of dissociative PTSD. Furthermore, the observed baseline symptom profiles largely match up with previous LPA studies suggesting that we are replicating and expanding upon these earlier findings, and most individuals in the dissociative-reexperiencing class transitioned to a non-dissociative class after treatment, suggesting both PTSD and dissociative symptom measures were sensitive to change. Additionally, this sample was a PTSD treatment-seeking sample, which may limit generalization of the symptom profiles to the total population of individuals with PTSD or the total population of traumatized individuals with and without PTSD. However, a PTSD treatment-seeking sample is reflective of the population most important to clinicians looking for guidance on treating PTSD. Finally, the sample size for the current study was smaller than most other LPA studies. While there is a weak relationship between samples size and power in LPA (Tein, Coxe, & Cham, 2013), small cell sizes for individual classes make it difficult to interpret treatment effects and identify smaller but possibly clinically meaningful classes.
Similar to the current findings, the only other LPA study to examine treatment response for those who dissociate determined that dissociation was “not a contraindication for PE” (p. 99, Wolf et al., 2016). Proposals to develop new treatments or add additional components to existing treatments for theorized new types of PTSD should not be adopted without a strong empirical base. Additional symptoms and changes to the diagnostic algorithm for PTSD in the DSM-5 has led to a drastic increase in diagnostic complexity for this already heterogeneous disorder (Galatzer-Levy et al., 2013). Diagnostic specifiers, such as the dissociative subtype, add to this complexity and thus require a high degree of scientific scrutiny before being accepted in the nosology. The current findings suggest that individuals with chronic reexperiencing symptoms, especially those that are dissociative in nature such as flashbacks, are likely to also report increased dissociation. However, it is not clear that the dissociative class identified in FMM studies specifies a different type of disorder. A recent review of the FMM literature (Hansen et al., 2017) suggested that the presence of a dissociative class across PTSD samples supported the existence of the dissociative subtype. While the current findings are in line with the review’s conclusion that a class of highly dissociative individuals can be identified in PTSD samples, more evidence is needed to substantiate this class as a dissociative subtype, especially given that, as the review points out, a consistent etiological predictor of the class has not yet been identified. Further, the conclusion of the review that PE is indicated for the dissociative subtype, while in line with the current findings, is not in line with previous recommendations for stepped care for those who dissociate (Cloitre et al., 2012). Until these opposing treatment recommendations are reconciled with empirical data, the clinical utility of the subtype will remain unclear.
With the addition of the dissociative subtype of PTSD in the DSM-5 likely to increase clinical concern about dissociative symptoms, it is important for research to continue to examine the efficacy of evidence-based treatments for PTSD for those who report dissociative symptoms. Based on the current findings, dissociation symptoms are not a contraindication for exposure-based therapy such as PE and do not seem to impede evidence-based treatment above and beyond PTSD symptom severity. The study of dissociation in PTSD has sparked a much needed debate regarding the structure of PTSD symptoms and the benefits of evidence-based treatments, which should be carried forward to address the needs of those suffering from this debilitating disorder.
Public Health Significance Statement.
Individuals with dissociative symptoms in addition to severe PTSD symptoms respond well to exposure-based treatment. Clinical guidelines that recommend postponing exposure-based treatment for individuals who dissociate may not be warranted.
Acknowledgments
This research was funded by R01 MH066347 (PI: Zoellner); R01 MH066348 (PI: Feeny); K23 MH005324 (PI: Roy-Byrne); the William T. Dahms, M.D. Clinical Research Unit, funded under the Cleveland Clinical and Translational Science Award (UL1 RR024989); and Supplemental Grant (drug supply), Pfizer, Inc.
Contributor Information
Mark S. Burton, Department of Psychological Sciences, Case Western Reserve University
Norah C. Feeny, Department of Psychological Sciences, Case Western Reserve University
Arin M. Connell, Department of Psychological Sciences, Case Western Reserve University
Lori A. Zoellner, Department of Psychology, University of Washington
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text revision. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Armour C, Elklit A, Lauterbach D, Elhai JD. The DSM-5 dissociative-PTSD subtype: Can levels of depression, anxiety, hostility, and sleeping difficulties differentiate between dissociative-PTSD and PTSD in rape and sexual assault victims? Journal of Anxiety Disorders. 2014;28(4):418–426. doi: 10.1016/j.janxdis.2013.12.008. [DOI] [PubMed] [Google Scholar]
- Armour C, Hansen M. Assessing DSM-5 latent subtypes of acute stress disorder dissociative or intrusive? Psychiatry Research. 2015;225(3):476–483. doi: 10.1016/j.psychres.2014.11.063. [DOI] [PubMed] [Google Scholar]
- Armour C, Karstoft K, Richardson JD. The co-occurrence of PTSD and dissociation: Differentiating severe PTSD from dissociative-PTSD. Social Psychiatry and Psychiatric Epidemiology. 2014;49(8):1297–1306. doi: 10.1007/s00127-014-0819-y. [DOI] [PubMed] [Google Scholar]
- Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: Three-step approaches using M plus. Structural Equation Modeling: A Multidisciplinary Journal. 2014;21(3):329–341. [Google Scholar]
- Bedard-Gilligan M, Zoellner LA. Dissociation and memory fragmentation in post-traumatic stress disorder: An evaluation of the dissociative encoding hypothesis. Memory. 2012;20(3):277–299. doi: 10.1080/09658211.2012.655747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein E, Putnam FW, Ross CA. Validity of the dissociative experiences scale in screening for multiple personality disorder: A multicenter study. Am J Psychiatry. 1993;150:1030–1036. doi: 10.1176/ajp.150.7.1030. [DOI] [PubMed] [Google Scholar]
- Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. Journal of Nervous and Mental Disease. 1986;174(12):727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Bernstein IH, Ellason JW, Ross CA, Vanderlinden J. On the dimensionalities of the dissociative experiences scale (DES) and the dissociation questionnaire (DIS-Q) Journal of Trauma & Dissociation. 2001;2(3):103–123. doi: 10.1300/J229v02n03_07. [DOI] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM- 5 (PCL- 5): Development and initial psychometric evaluation. Journal of Traumatic Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Brady K, Pearlstein T, Asnis GM, Baker D, Rothbaum B, Sikes CR, Farfel GM. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: A randomized controlled trial. JAMA: Journal of the American Medical Association. 2000;283(14):1837–1844. doi: 10.1001/jama.283.14.1837. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick S, Brett E, Fontana A, Rosenheck R, Charney DS. Dissociation and posttraumatic stress disorder in vietnam combat veterans. The American Journal of Psychiatry. 1992;149(3):328–332. doi: 10.1176/ajp.149.3.328. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=1992-39390-001&site=ehost-live. [DOI] [PubMed] [Google Scholar]
- Carlson EB, Dalenberg C, McDade-Montez E. Dissociation in posttraumatic stress disorder part I: Definitions and review of research. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(5):479–489. doi: 10.1037/a0027748. 10.1037/a0027748.supp (Supplemental) [DOI] [Google Scholar]
- Carlson EB, Putnam FW, Ross CA, Anderson G, Clark P, Torem M, Dill D. Paper presented at the Proceedings of the Eighth International Conference on Multiple Personality and Dissociative States. Chicago: Rush; 1991. Factor analysis of the dissociative experiences scale: A multicenter study; p. 16. [Google Scholar]
- Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73(5):965–971. doi: 10.1037/0022-006X.73.5.965. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stolbach BC, Herman JL, Kolk Bvd, Pynoos R, Wang J, Petkova E. A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress. 2009;22(5):399–408. doi: 10.1002/jts.20444. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology. 2002;70(5):1067–1074. doi: 10.1037/0022-006X.70.5.1067. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Petkova E, Wang J, Lu (Lassell) F. An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depression and Anxiety. 2012;29(8):709–717. doi: 10.1002/da.21920. [DOI] [PubMed] [Google Scholar]
- Cook A, Spinazzola J, Ford J, Lanktree C, Blaustein M, Cloitre M, Van der Kolk B. Complex trauma. Psychiatric Annals. 2005;35(5):390–398. [Google Scholar]
- Dalenberg CJ, Glaser D, Alhassoon OM. Statistical support for subtypes in posttraumatic stress disorder: The how and why of subtype analysis. Depression and Anxiety. 2012;29(8):671–678. doi: 10.1002/da.21926. [DOI] [PubMed] [Google Scholar]
- Dalenberg C, Carlson EB. Dissociation in posttraumatic stress disorder part II: How theoretical models fit the empirical evidence and recommendations for modifying the diagnostic criteria for PTSD. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(6):551–559. doi: 10.1037/a0027900. [DOI] [Google Scholar]
- De Jongh A, Resick PA, Zoellner LA, van Minnen A, Lee CW, Monson CM, Bicanic IAE. Critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety. 2016;33(5):359–369. doi: 10.1002/da.22469. [DOI] [PubMed] [Google Scholar]
- Dziak JJ, Lanza ST, Tan X. Effect size, statistical power, and sample size requirements for the bootstrap likelihood ratio test in latent class analysis. Structural Equation Modeling. 2014;21(4):534–552. doi: 10.1080/10705511.2014.919819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Foa E, Hembree E, Dancu C. Prolonged exposure (PE) manual revised version. Unpublished Manuscript 2002 [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The posttraumatic diagnostic scale. Psychological Assessment. 1997;9(4):445. [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post- traumatic stress disorder. Journal of Traumatic Stress. 1993;6(4):459–473. [Google Scholar]
- Foa EB, Tolin DF. Comparison of the PTSD symptom scale-interview version and the clinician-administered PTSD scale. Journal of Traumatic Stress. 2000;13(2):181–191. doi: 10.1023/A:1007781909213. [DOI] [PubMed] [Google Scholar]
- Frewen PA, Brown MFD, Steuwe C, Lanius RA. Latent profile analysis and principal axis factoring of the DSM-5 dissociative subtype. European Journal of Psychotraumatology. 2015:6. doi: 10.3402/ejpt.v6.26406. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2015-23507-001&site=ehost-live. [DOI] [PMC free article] [PubMed]
- Galatzer-Levy IR, Bryant RA. 636,120 ways to have posttraumatic stress disorder. Perspectives on Psychological Science : A Journal of the Association for Psychological Science. 2013;8(6):651–662. doi: 10.1177/1745691613504115. [DOI] [PubMed] [Google Scholar]
- Giesbrecht T, Lynn SJ, Lilienfeld SO, Merckelbach H. Cognitive processes in dissociation: An analysis of core theoretical assumptions. Psychological Bulletin. 2008;134(5):617–647. doi: 10.1037/0033-2909.134.5.617. [DOI] [PubMed] [Google Scholar]
- Giesbrecht T, Merckelbach H, Geraerts E, Sweets E. Dissociation in undergraduate students: Disruptions in executive functioning. Journal of Nervous and Mental Disease. 2004;192(8):567–569. doi: 10.1097/01.nmd.0000135572.45899.f2. [DOI] [PubMed] [Google Scholar]
- Hagenaars MA, van Minnen A, Hoogduin KAL. The impact of dissociation and depression on the efficacy of prolonged exposure treatment for PTSD. Behaviour Research and Therapy. 2010;48(1):19–27. doi: 10.1016/j.brat.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Hansen M, Hyland P, Armour C. Does highly symptomatic class membership in the acute phase predict highly symptomatic classification in victims 6 months after traumatic exposure? Journal of Anxiety Disorders. 2016;40:44–51. doi: 10.1016/j.janxdis.2016.04.008. [DOI] [PubMed] [Google Scholar]
- Hansen M, Mullerová J, Elklit A, Armour C. Can the dissociative PTSD subtype be identified across two distinct trauma samples meeting caseness for PTSD? Social Psychiatry and Psychiatric Epidemiology. 2016;51(8):1159–1169. doi: 10.1007/s00127-016-1235-2. [DOI] [PubMed] [Google Scholar]
- Hansen M, Ross J, Armour C. Evidence of the dissociative PTSD subtype: A systematic literature review of latent class and profile analytic studies of PTSD. Journal of Affective Disorders. 2017;213:59–69. doi: 10.1016/j.jad.2017.02.004. [DOI] [PubMed] [Google Scholar]
- Holmes EA, Brown RJ, Mansell W, Fearon RP, Hunter ECM, Frasquilho F, Oakley DA. Are there two qualitatively distinct forms of dissociation? A review and some clinical implications. Clinical Psychology Review. 2005;25(1):1–23. doi: 10.1016/j.cpr.2004.08.006. [DOI] [PubMed] [Google Scholar]
- Ipser JC, Stein DJ. Evidence-based pharmacotherapy of post-traumatic stress disorder (PTSD) International Journal of Neuropsychopharmacology. 2012;15(6):825–840. doi: 10.1017/S1461145711001209. [DOI] [PubMed] [Google Scholar]
- Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, Spiegel D. Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. The American Journal of Psychiatry. 2010;167(6):640. doi: 10.1176/appi.ajp.2009.09081168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanius RA, Brand B, Vermetten E, Frewen PA, Spiegel D. The dissociative subtype of posttraumatic stress disorder: Rationale, clinical and neurobiological evidence, and implications. Depression and Anxiety. 2012;29(8):701–708. doi: 10.1002/da.21889. [DOI] [PubMed] [Google Scholar]
- Lobbestael J, Leurgans M, Arntz A. Inter- rater reliability of the structured clinical interview for DSM- IV axis I disorders (SCID I) and axis II disorders (SCID II) Clinical Psychology & Psychotherapy. 2011;18(1):75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- Lynn SJ, Lilienfeld SO, Merckelbach H, Giesbrecht T, van der Kloet Dissociation and dissociative disorders: Challenging conventional wisdom. Current Directions in Psychological Science. 2012;21(1):48–53. doi: 10.1177/0963721411429457. [DOI] [Google Scholar]
- Maercker A, Brewin CR, Bryant RA, Cloitre M, Reed GM, van Ommeren M, Saxena S. Proposals for mental disorders specifically associated with stress in the international classification of diseases-11. The Lancet. 2013;381(9878):1683–1685. doi: 10.1016/S0140-6736(12)62191-6. [DOI] [PubMed] [Google Scholar]
- Marshall RD, Lewis-Fernandez R, Blanco C, Simpson HB, Lin S, Vermes D, Liebowitz MR. A controlled trial of paroxetine for chronic PTSD, dissociation and interpersonal problems in mostly minority adults. Depression and Anxiety. 2007;24(2):77–84. doi: 10.1002/da.20176. [DOI] [PubMed] [Google Scholar]
- Marshall RD, Schneier FR, Fallon BA, Knight CBG, Abbate LA, Goetz D, Liebowitz MR. An open trial of paroxetine in patients with noncombat-related, chronic posttraumatic stress disorder. Journal of Clinical Psychopharmacology. 1998;18(1):10–18. doi: 10.1097/00004714-199802000-00003. [DOI] [PubMed] [Google Scholar]
- Mullerová J, Hansen M, Contractor AA, Elhai JD, Armour C. Dissociative features in posttraumatic stress disorder: A latent profile analysis. Psychological Trauma: Theory, Research, Practice, and Policy. 2016 doi: 10.1037/tra0000148. 10.1037/tra0000148.supp (Supplemental) [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Seventh. Los Angeles, CA: 2015. [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Structural Equation Modeling. 2007;14(4):535–569. [Google Scholar]
- Nylund KL. Latent Transition Analysis: Modeling Extensions and an Application to Peer Victimization. Doctoral dissertation, University of California Los Angeles; 2007. [Google Scholar]
- Pearlman LA, Courtois CA. Clinical applications of the attachment framework: Relational treatment of complex trauma. Journal of Traumatic Stress. 2005;18(5):449–459. doi: 10.1002/jts.20052. [DOI] [PubMed] [Google Scholar]
- Putnam FW. In: Dissociative phenomena. Tasman A, Goldfinger SM, editors. Arlington, VA US: American Psychiatric Association; 1991. pp. 145–160. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=1991-97920. [Google Scholar]
- Resick PA, Suvak MK, Johnides BD, Mitchell KS, Iverson KM. The impact of dissociation on PTSD treatment with cognitive processing therapy. Depression and Anxiety. 2012;29(8):718–730. doi: 10.1002/da.21938. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Best CL, Freedy CR, Kilpatrick DG, Falsetti SA. Trauma Assessment for Adults (TAA) Unpublished Manuscript 1993 [Google Scholar]
- Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: Its application to schizophrenia. The American Journal of Psychiatry. 1970;126(7):983–986. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- Ruiz MA, Poythress NG, Lilienfeld SO, Douglas KS. Factor structure and correlates of the dissociative experiences scale in a large offender sample. Assessment. 2008;15(4):511–521. doi: 10.1177/1073191108315548. [DOI] [PubMed] [Google Scholar]
- Schauer M, Elbert T. Dissociation following traumatic stress. Zeitschrift Für Psychologie/Journal of Psychology 2015 [Google Scholar]
- Speckens AEM, Ehlers A, Hackmann A, Clark DM. Changes in intrusive memories associated with imaginal reliving in posttraumatic stress disorder. Journal of Anxiety Disorders. 2006;20(3):328–341. doi: 10.1016/j.janxdis.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Steuwe C, Lanius RA, Frewen PA. Evidence for a dissociative subtype of PTSD by latent profile and confirmatory factor analyses in a civilian sample. Depression and Anxiety. 2012;29(8):689–700. doi: 10.1002/da.21944. [DOI] [PubMed] [Google Scholar]
- Tein J, Coxe S, Cham H. Statistical power to detect the correct number of classes in latent profile analysis. Structural Equation Modeling. 2013;20(4):640–657. doi: 10.1080/10705511.2013.824781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Kolk, Bessel A, Roth S, Pelcovitz D, Sunday S, Spinazzola J. Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress. 2005;18(5):389–399. doi: 10.1002/jts.20047. [DOI] [PubMed] [Google Scholar]
- van der Kolk, van der Hart, Marmar CR. In: Dissociation and information processing in posttraumatic stress disorder. van der Kolk BA, McFarlane AC, Weisaeth L, van der Kolk Bessel A, McFarlane AC, Weisaeth L, editors. New York, NY, US: Guilford Press; 1996. pp. 303–327. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=1996-98017-013&site=ehost-live. [Google Scholar]
- van der Hart, Horst R. The dissociation theory of pierre janet. Journal of Traumatic Stress. 1989;2(4):397–412. doi: 10.1002/jts.2490020405. [DOI] [Google Scholar]
- van IJzendoorn MH, Schuengel C. The measurement of dissociation in normal and clinical populations: Meta-analytic validation of the dissociative experiences scale (DES) Clinical Psychology Review. 1996;16(5):365–382. doi: 10.1016/0272-7358(96)00006-2. [DOI] [Google Scholar]
- Waller N, Putnam FW, Carlson EB. Types of dissociation and dissociative types: A taxometric analysis of dissociative experiences. Psychological Methods. 1996;1(3):300–321. doi: 10.1037/1082-989X.1.3.300. [DOI] [Google Scholar]
- Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, Friedman MJ. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. The Journal of Clinical Psychiatry. 2013;74(6):e551–e557. doi: 10.4088/JCP.12r08225. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Lunney CA, Miller MW, Resick PA, Friedman MJ, Schnurr PP. The dissociative subtype of PTSD: A replication and extension. Depression and Anxiety. 2012a;29(8):679–688. doi: 10.1002/da.21946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Lunney CA, Schnurr PP. The influence of the dissociative subtype of posttraumatic stress disorder on treatment efficacy in female veterans and active duty service members. Journal of Consulting and Clinical Psychology. 2016;84(1):95–100. doi: 10.1037/ccp0000036. 10.1037/ccp0000036.supp (Supplemental) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Reardon AF, Ryabchenko KA, Castillo D, Freund R. A latent class analysis of dissociation and posttraumatic stress disorder: Evidence for a dissociative subtype. JAMA Psychiatry. 2012b;69(7):698–705. doi: 10.1001/archgenpsychiatry.2011.1574. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2013-03107-008&site=ehost-live. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Mitchell KS, Sadeh N, Hein C, Fuhrman I, Pietrzak RH, Miller MW. The dissociative subtype of PTSD scale: Initial evaluation in a national sample of trauma-exposed veterans. Assessment. 2017;24(4):503–516. doi: 10.1177/1073191115615212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R, Elkin A, Binder-Brynes K, Kahana B, Southwick SM, Schmeidler J, Giller EL. Dissociation in aging holocaust survivors. The American Journal of Psychiatry. 1996;153(7):935–940. doi: 10.1176/ajp.153.7.935. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=1996-00459-012&site=ehost-live. [DOI] [PubMed] [Google Scholar]