Abstract
Introduction
Although burnout in paediatric nurses has been addressed in previous research, the heterogeneous nature of the results obtained and of the variables studied highlights the need for a detailed analysis of the literature.
Objective
The aim of this study was to analyse the literature on burnout characteristics, reported prevalence, severity and risk factors, to achieve a better understanding of the risk of emotional exhaustion, depersonalisation and feelings of low personal accomplishment.
Method
For this purpose, we carried out a systematic review and meta-analysis of the literature. The databases consulted were CINAHL, LILACS, PubMed, the Proquest Platform (Proquest Health & Medical Complete), Scielo and Scopus. This study used the search equation “burnout AND “pediatric nurs*””, and was conducted in July 2017.
Results
The search produced 34 studies targeting burnout in paediatric nurses, with no restrictions on the date of publication. Many of these studies detected moderate-high values for the three dimensions of burnout, and highlighted sociodemographic, psychological and job-related variables associated with this syndrome. The sample population for the meta-analysis was composed of 1600 paediatric nurses. The following prevalence values were obtained: (i) emotional exhaustion, 31% (95% CI: 25–37%); (ii) depersonalisation, 21% (95% CI: 11–33%); (iii) low personal accomplishment, 39% (95% CI: 28–50%).
Conclusions
A significant number of paediatric nurses were found to have moderate-high levels of emotional exhaustion and depersonalisation, and low levels of personal accomplishment. These nurses, therefore, were either experiencing burnout or at high risk of suffering it in the future. These results support the need for further study of the risk factors for burnout in paediatric nurses. They also highlight the importance of developing interventions or therapies to help prevent or attenuate the above symptoms, thus helping nurses cope with the workplace environment and with situations that may lead to burnout.
Introduction
In recent years, the question of occupational burnout has caught the attention of researchers and professionals [1], who have used various instruments to analyse and measure the factors associated with this condition [2–11]. Burnout syndrome among paediatric nurses is characterised by the following effects: (i) emotional exhaustion (EE) with progressive loss of energy; (ii) depersonalisation (D), reflected in negative attitudes towards patients and co-workers; (iii) feelings of low personal accomplishment (PA) or loss of confidence [12, 13]. Workers may be continuously subjected to stressors both at work and in the home. The syndrome is more prevalent in service professions such as teaching, the police and health care [14].
Healthcare professionals, especially nurses, are a high-risk group that is especially prone to the syndrome [15, 16]. The nursing profession demands high levels of social responsibility, and problems that can arise on a daily basis include work overload, lack of autonomy or authority to make decisions, and difficulty in reconciling family life and work. All of these factors can trigger burnout syndrome, generating symptoms such as fatigue, memory problems, depression, anxiety, sleep disorders, irritability or substance abuse [17]. Other stressful situations that nurses must routinely cope with include obligatory rotating shifts, work overload because of understaffing and, in certain cases, care of the terminally ill [17].
All of these factors make nursing professionals particularly vulnerable to burnout. When nurses experience this syndrome, the healthcare institution is also negatively affected because of increased workplace absenteeism and nursing turnover [18,19]. The resulting deterioration in the quality of healthcare is, in turn, detrimental to the users of healthcare services [20].
There is a high prevalence of burnout among nursing professionals [21]. Nurses working in oncology and critical care units are generally regarded as being most susceptible to developing this syndrome [15, 22–24]. However, those in paediatric and neonatal units are also subject to high levels of stress and are at risk of burnout [3, 25, 26]. Detailed knowledge of the variables related to this syndrome, an estimation of the prevalence of each of its dimensions, and an understanding of the context in which these professionals work are all essential elements in the design and implementation of strategies for the treatment and prevention of burnout. Appropriate strategies in this regard would help improve the occupational health of paediatric nurses and the quality of care received by their patients and also contribute to optimising work conditions [27, 28].
In summary, the aim of this study was to determine burnout prevalence, levels and risk factors in paediatric nurses and to conduct a meta-analysis to estimate the prevalence of emotional exhaustion and depersonalisation and of feelings of inadequate personal accomplishment.
Materials and methods
Data sources, search equation and inclusion criteria
A systematic review and meta-analysis were performed according to the PRISMA guidelines [29]. The first step in this process was to search the following electronic databases: CINAHL, LILACS, PubMed, the Proquest Platform (Proquest Health & Medical Complete), Scielo and Scopus. The search equation used was “burnout AND “pediatric nurs*”. To minimise publication bias, no restrictions were placed on publication date, study methods, language or sample size. The databases also included grey literature. The second step was to review all the previous meta-analytic studies and systematic reviews of this topic. Finally, all the references included in the selected studies were also reviewed.
The following inclusion criteria were applied: (a) primary quantitative studies; (b) studies that assessed burnout risk factors, measured burnout in the sample or specified the number or proportion of subjects with burnout; (c) sample of paediatric or neonatal nurses; (d) language used in the paper (Spanish, English, Portuguese or Italian); (e) studies using the Maslach Burnout Inventory (MBI) were included in the meta-analysis.
The exclusion criteria were: (a) sample of paediatric resident nurses; (b) studies with mixed samples that did not provide independent information for paediatric or neonatal nurses.
Codification of results and data analysis
The variables were recorded on a data definition log. Two members of the research team independently performed the search, selection and detailed reading of the publications. In case of disagreement, a third researcher was consulted. The following variables were considered:
Publication variables: (a) authors; b) year of publication; (c) country of publication; (d) language (Spanish, English, Portuguese or Italian); (e) sample size; (f) percentage of female nurses in the sample; (g) age in years of the sample population (mean, standard deviation, median or range).
Methodological variables: (h) burnout measurement instrument; (i) in the case of the MBI, specification of subtype (MBI, MBI-HSS, MBI-GS); (j) use of original instrument or an adapted version; (k) reliability index, either calculated or derived from other studies; (l) estimated reliability coefficient of the instrument.
Burnout measurement variables: main results for the presence of burnout in paediatric nurses, including: (i) the prevalence of low, medium and high levels of each burnout dimension (emotional exhaustion, depersonalisation and personal accomplishment); (ii) mean value and standard deviation of the score for each burnout dimension; (iii) prevalence of nursing professionals with burnout.
Data analysis
A descriptive analysis was made of the study variables included, reporting on the quality of the publications selected, based on the levels of evidence and grades of recommendation proposed by the Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence Working Group [30].
A sensitivity analysis was also performed to ascertain whether any of the studies in the meta-analysis produced a variation in the estimate of the mean effect size. Publication bias, which refers to the higher probability of studies with statistically significant results being published, was assessed by Egger’s linear regression test. The Q test and the I2 index were used to evaluate the heterogeneity that is not explained by the chance. The analyses were performed using StatsDirect Version 2.8.0 (2013), a statistical software package for general health science users.
Results
Description of the search and the studies included
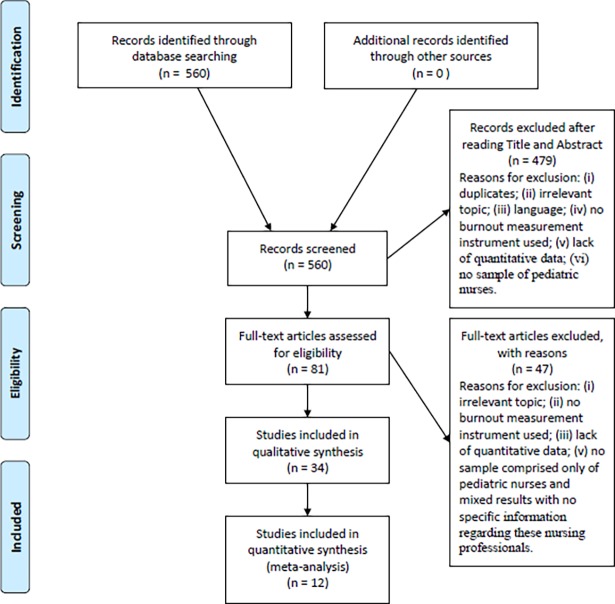
The search was performed in July 2017. After applying the corresponding inclusion and exclusion criteria, a total of 34 studies were selected. The sample population was composed of 9,075 paediatric and neonatal nurses (Fig 1).
Fig 1. Flow diagram of the publication search process.
Almost half of the studies included were published from 2013 to 2016 [2, 5, 31–40] and over 70% were from the US or Canada. Other studies reflected work carried out in Brazil, Egypt, Greece, Pakistan, Peru, Taiwan, Turkey and Venezuela (Table 1).
Table 1. Main results of the studies included in the review.
| Authors (publication year), country. | Burnout instrument (Instrument Reliability, Cronbach Alpha) |
n | Gender and mean age | Burnout-related variables |
OCBEM a |
|---|---|---|---|---|---|
| Adwan (2014) [31], USA. | MBI-HSS | 120 | 95% Female Age = 34(10) Min-max: 23−62 |
High levels of grief correlate positively with EE | LE: 2C GE: B |
| Akman et al., (2016) [52], Turkey. | MBI-HSS | 165 | Age = 28.95(6) | Job satisfaction, marital status, age and number of assigned patients are all related to burnout. Young, married nurses who work the day shift are most vulnerable to burnout. | LE: 2C GE: B |
| Alves & Guirardello (2016) [32], Brazil. | MBI-HSS (EE = .87) |
267 | 91.8% Female Age = 34.9 (7.9) |
High levels of EE correlate with low levels of job satisfaction and patient safety |
LE: 2C GE: B |
| Aytekin et al., (2013) [51] Turkey. | MBI-HSS (EE = .78, D = .55, PA = .76) |
80 | Age = 22−29: 37.5% 30−35: 36.2% |
PA increases with the nurses’ age and the number of years that they have worked in the paediatric unit. Their quality of life worsens as burnout becomes more intense. | LE: 2C GE: B |
| Battles (2000) [53], USA. | MBI-HSS (EE = .90, D = .78, PA = .76) |
148 | 98.6% Female Age = 40.3(8.9) |
Burnout levels are lower in nurses who spend most of their time in direct contact with the patient, who have fewer patients under their care, and who participate in clinical studies. | LE: 2C GE: B |
| Berger et al., (2015) [2], USA. | Professional Quality of Life Scale, Version 5 | 239 | 97.9% Female Age = >40 (52.1%) |
Younger nurses are more prone to burnout | LE: 2C GE: B |
| Berkowitz (1993) [58], USA & Puerto Rico. | MBI-HSS (EE = .91, D = .75, PA = .78) |
518 | 95% Female | The variables, refusal to care for the patient, the feeling of uselessness, fear and anxiety all correlate positively with EE and D, and negatively with PA. | LE: 2C GE: B |
| Bilal & Ahmed (2016) [33], Pakistan. | MBI-HSS (EE = .75) | 113 | 72% Female Age = 43.56 |
High EE correlates negatively with participation in decision-making, communication skills and opportunities for promotion. | LE: 2C GE: B |
| Budnik (2003) [57], USA. | MBI-HSS | 20 | - | Emotional intelligence correlates negatively with EE and D, and positively with PA. | LE: 2C GE: B |
| Czaja et al., (2012) [20], USA. | MBI-HSS | 173 | 93% Female Age: 35(9) |
Burnout is associated with the idea of changing job/profession. | LE: 2C GE: B |
| Davis et al., (2013) [34], USA. | MBI-HSS | 15 | - | EE correlates negatively with job satisfaction and positively with the nurses’ age. | LE: 2C GE: B |
| Downey et al., (1995) [3], USA. | Adaptation of Popoff and Funkhouser´s survey of nurses | 59 | 58 Females | Burnout is positively associated with stress. | LE: 2C GE: B |
| Edmonds et al., (2012) [59], USA. | MBI-HSS | 88 | - | Burnout is associated with the nurses’ age. | LE: 2C GE: B |
| Estabrooks et al., (2011) [27], Canada. | MBI-GS | 844 | - | EE is negatively related to job satisfaction. | LE: 2C GE: B |
| Gallagher & Gormley (2009) [17], USA. | MBI-HSS | 30 | - | Length of experience in the profession and working in the medical unit both correlate negatively with EE and D, and positively with PA. | LE: 2C GE: B |
| Hawes (2009) [56], USA. |
MBI-HSS (EE = .90, D = .56, PA = .83) |
75 | 98.7% Female | Stress correlates positively with EE and D, and negatively with PA. The work environment is negatively related to EE and D, and positively to PA. | LE: 2C GE: B |
| Jacobs et al., (2012) [4], USA. | MBI-HSS & Copenhagen Burnout Inventory | 47 | - | Gender correlates with burnout. | LE: 2C GE: B |
| Li et al., (2014) [5], USA. | Compassion Satisfaction Burnout Inventory (Burnout subscale: α = .90) |
251 | 231 Females | Nurses with higher levels of stress present higher levels of burnout. | LE: 2C GE: B |
| Liakopoulou et al., (2008) [24], Greece. | MBI-HSS (EE = .80, D = .60, PA = .67) |
37 | - | Burnout is positively associated with being childless, having less job experience, and lacking a clear professional role. | LE: 2C GE: B |
| Lin et al., (2016) [6], Taiwan. | Occupational Burnout Inventory (Burnout = .94) |
144 | 100% Female Age = 35.72 (7.10) |
There is a positive association between stress, burnout and depression. | LE: 2C GE: B |
| Messmer et al., (2011) [41], USA. | MBI-HSS (α = .90) |
33 | 82% Female Age = 21−27(76%) |
Burnout correlates negatively with job satisfaction. | LE: 2C GE: B |
| Meyer et al., (2015) [8], USA. | Compassion Fatigue Self-Test (Burnout subscale α = .90) |
251 | 231 Females Age = Between 23−30 years (60.1%) |
Stress is positively related to burnout in paediatric nurses. | LE: 2C GE: B |
| Moussa & Mahmood (2013) [54], Egypt. | MBI-HSS | 55 | Age = 30.3 (7.4) | Age, length of professional experience, and experience in the medical unit all correlate negatively with EE and D, and positively with PA. Lack of work information correlates positively with EE. | LE: 2C GE: B |
| Oehler et al., (1991) [43], USA. | MBI-HSS | 49 | 100% Female Age = 29.9 |
Burnout is related to higher levels of work stress and anxiety, the perceived lack of supervision, and less work experience. | LE: 2C GE: B |
| Oehler & Davidson (1992) [42], USA. | MBI-HSS | 121 | 100% Female Age = 30.51 |
Burnout is related to professional experience. Nurses with less experience present higher levels of burnout. | LE: 2C GE: B |
| Pagel & Wittmann (1986) [9], USA. | Tedium Measure | 74 | 100% Female | There is a positive association between burnout and caring for children with behaviour problems. | LE: 2C GE: B |
| Parada et al., (2005) [55], Venezuela. | MBI-HSS | 104 | 93.3% Female Age = >40(56.73%) |
Burnout levels are higher among younger nurses with less work experience, and among those who spend more time caring for patients. |
LE: 2C GE: B |
| Sekol & Kim (2014) [35], USA. | Professional Quality of Life Scale version V (ProQOL-V) (Burnout subscale: α = .75) |
240 | 94.2% Female | Nurses in a unit with a special quality of life and care programme for patients have lower levels of burnout. | LE: 2C GE: B |
| Shoffner (1988) [10], USA. | Staff Burnout Scale for Health Professionals (α = .93) |
18 | - | Nurses on the day shift and those on 12-hour shifts have higher levels of burnout. | LE: 2C GE: B |
| Squires et al., (2013) [36], Canada. | MBI-GS | 735 | 94.1% Female Age = 20−29(34.1%) |
The level of depersonalisation is negatively correlated with the application of research information in the work context. | LE: 2C GE: B |
| Stimpfel et al., (2013) [37], USA. | MBI-HSS | 3710 | Age = 44 Nearly all nurses were female |
- | LE: 2C GR: B |
| Vásquez-Manrique et al., (2014) [38], Peru. | MBI-HSS | 16 | - | Depersonalisation is positively related to the nurse’s job experience and whether their spouse is in employment. Personal accomplishment is correlated with gender and type of contract. | LE: 2C GR: B |
| Wilkinson (2014) [39], Canada. | MBI-HSS (EE = .91, D = .73, PA = .81) |
171 | 96% Female Age = 26−60 |
Nurses’ resilience is negatively correlated with levels of emotional exhaustion and depersonalisation, and positively so with PA. | LE: 2C GR: B |
| Zanatta & Lucca (2015) [40], Brazil. | MBI-HSS | 65 | - | Burnout is related to being married and to the presence of occupational health problems. | LE: 2C GR: B |
EE [Emotional Exhaustion]; D [Depersonalisation]; PA [Personal Accomplishment].
LE [Level of evidence]; GR [Grade of recommendation].
aOCEBM [Levels of evidence of the Oxford Centre for Evidence-Based Medicine].
The nurses studied worked in the following areas: paediatrics (n = 27 studies), neonatal (n = 6) and both services (n = 1). Most of these nurses were female, in proportions ranging from 82% [41] to 100% [42, 43]. The ages of the nurses ranged from 23 to 62 years, but 60% were aged 23–30 years [8]. Over 75% of the studies included used the MBI to measure burnout [44–48] (Table 1).
Reliability coefficients of the burnout questionnaires were estimated in 14 of the studies, while the others used reliability induction [49, 50]. The reliability estimates ranged from 0.55 [51] to 0.94 [6], with values higher than 0.7 being considered acceptable (Table 1).
Burnout risk factors in paediatric services
The development of burnout in paediatric nurses may be influenced by a wide variety of psychological, occupational and sociodemographic factors [23].
Sociodemographic factors: Few studies have analysed the relation between nurses’ age and marital status and burnout. According to the publications analysed, married status is associated with lower levels of burnout [52], while age is inversely related to burnout levels, with younger nurses being more prone to this condition [2, 39, 52], although one study [34] reported a positive correlation between age and EE.
Occupational factors: Various occupational factors are related to the development of burnout syndrome. Some reports observe that high levels of job satisfaction are correlated with low burnout in paediatric nurses [52, 35]. A negative correlation has also been recorded between EE and job satisfaction [34].
Another factor identified as a burnout risk factor is that of the length of the working day. Nurses with a workday longer than eight hours are reported to have higher levels of job dissatisfaction and burnout than those with a shorter working day [37]. The number of patients assigned to each nurse, too, is directly related to burnout levels; thus, the more patients the nurses must attend, the higher the level of burnout [52, 53]. Finally, factors such as greater difficulty in accessing information at the workplace and less professional experience also make nurses more vulnerable to burnout syndrome [42, 54, 55].
Psychological factors. Exposure to stress and anxiety, lack of emotional intelligence and a perceived lack of supervision are associated with higher levels of burnout [8, 42, 56–58], as is a poorer quality of life [51].
Prevalence and levels of burnout in paediatric nursing
The studies considered estimated burnout, measured as the mean score and standard deviation, both as a total measure and for the subscales, and also included the level of burnout (low, medium, or high). The mean scores varied considerably, in all three dimensions of burnout. Thus, the emotional exhaustion scores ranged from 9.64 to 30.25 [56, 57], the depersonalisation values from 3.37 to 7.43 [56, 57] and those for personal accomplishment from 10.94 to 40.21 [54, 55] (Table 1).
Large variations were also observed in the prevalence of burnout symptoms. Thus, the prevalence of high levels of emotional exhaustion ranged from 12.5 to 56.4. [38, 54], and of depersonalisation, from 5.5 to 74.5 [53, 55], while the prevalence of low levels of personal accomplishment ranged from 6.67 to 85.5 [34, 54] (Table 2).
Table 2. Prevalence of high EE, high D and low PA.
| Authors (publication year), country | n | High EE | High D | Low PA |
|---|---|---|---|---|
| Alves & Guirardello (2016) [32], Brazil. | 267 | 27.3% | - | - |
| Battles (2000) [53], USA. | 148 | 31.7% | 5.5% | 50.3% |
| Berkowitz (1993) [58], USA & Puerto Rico. | 518 | 24% | 10% | 51% |
| Czaja et al., (2012) [20], USA. | 173 | 45% | 38% | 46% |
| Davis et al., (2013) [34], USA. | 15 | - | - | 6.67% |
| Edmonds et al., (2012) [59], USA. | 88 | 34.1% | 25% | 30.7% |
| Gallagher & Gormley (2009) [17], USA. | 30 | 26.7% | 3.3% | 16.7% |
| Moussa & Mahmood (2013) [54], Egypt. | 55 | 56.4% | 74.5% | 14.5% |
| Oehler & Davidson (1992) [42], USA. | 121 | 32.7% | 11.9% | 36.6% |
| Parada et al., (2005) [55], Venezuela. | 104 | 16.35% | 22.12% | 13.46% |
| Vásquez-Manrique et al., (2014) [38], Peru. | 16 | 12.5% | 12.5% | 62.5% |
| Zanatta & Lucca (2015) [40], Brazil. | 65 | 24.6% | 29.8% | 22.8% |
EE [Emotional Exhaustion]; D [Depersonalisation]; PA [Personal Accomplishment].
Results of the meta-analysis
The sensitivity analysis, conducted to determine whether any of the studies influenced the overall result, revealed no statistically significant changes in burnout prevalence when each study in turn was excluded from the analysis. Nor did the assessment of publication bias detect any statistically significant results.
The following results were obtained by the Cochran’s Q test: emotional exhaustion, 58.73 (p<0.001); depersonalisation, 186.64 (p<0.001); personal accomplishment, 146.19 (p<0.001). The I2 was indicative of a high level of heterogeneity with values of 83% for emotional exhaustion; 95.2% for depersonalisation; and 93.2% for personal accomplishment.
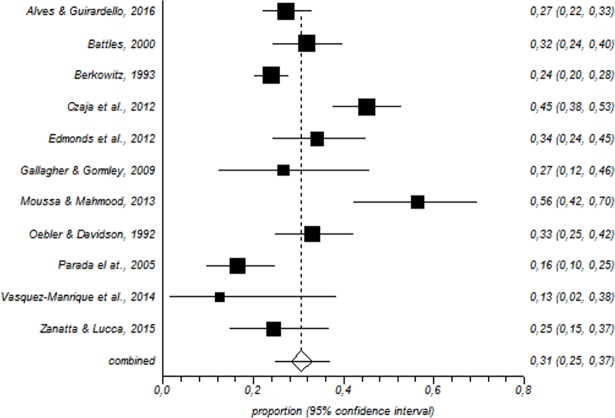
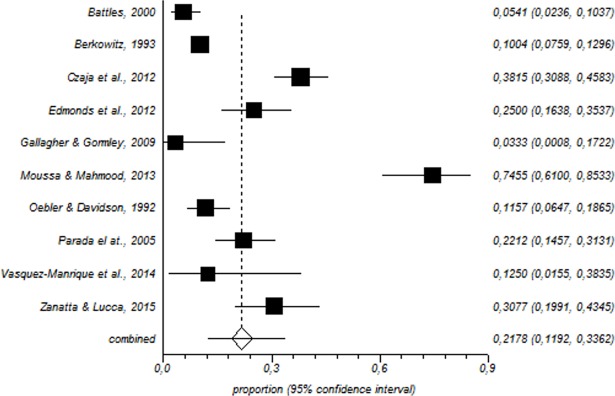
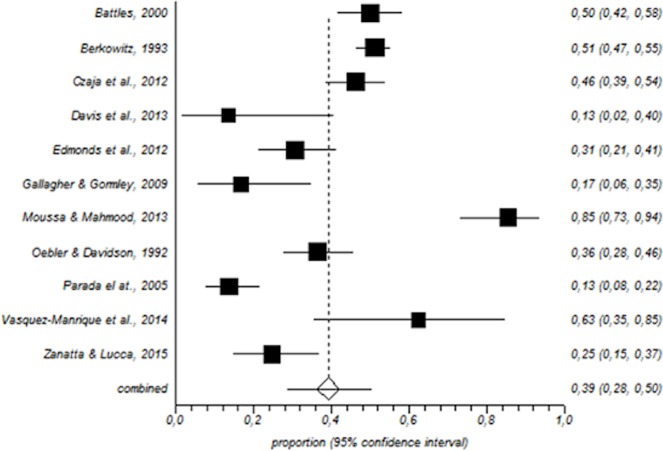
In total, 1600 paediatric nurses were included in the meta-analysis. Among this population, the prevalence of a high level of emotional exhaustion was 31% (95% CI = 25–37%) (Fig 2); for depersonalisation, the corresponding values were 21% (95% CI = 11–33%) (Fig 3) and for low personal accomplishment, 39% (95% CI = 28–50%) (Fig 4).
Fig 2. Forest plot for high emotional exhaustion.
Fig 3. Forest plot for high depersonalisation.
Fig 4. Forest plot for low personal accomplishment.
Burnout prevention measures
Some studies assessed the effectiveness of different interventions for reducing burnout. Thus, Edmonds et al. [59] reported that the Care for the Professional Caregiver Program (including confidentiality discussion, presentation of the model of vicarious trauma and loss, hands-on stress reduction techniques, etc.) was effective in reducing emotional exhaustion [59]. Other authors informed that head nurses should foment group cohesion, seeking to reduce burnout levels [5].
Adwan recommended the implementation and evaluation of intervention programmes [31]. According to Mousa & Mahmood [54], there is an urgent need to establish educational programmes to improve the communication skills of paediatric nurses, which would contribute to reducing burnout. Other authors have concluded that burnout levels could be reduced by restructuring and facilitating the administrative work performed by nurses [53].
Discussion
To our knowledge, this is the first meta-analysis focused on burnout syndrome in paediatric nurses. This analysis revealed a prevalence ranging from 30.77% to 73.70% for EE, from 26.20% to 73.70% for depersonalisation and from 46% to 85.50% for low PA.
Similar values for emotional exhaustion have been identified in oncology nurses [60], while emergency nurses have shown higher levels of emotional exhaustion [61]. The prevalence of depersonalisation is 6% lower in oncology nurses [60], and 15% higher in emergency nurses [61]. However, compared to both these groups, paediatric nurses present a higher prevalence of low personal accomplishment.
The results obtained are subject to variability in methodological factors such as sample size, measurement instrument used and application of reliability induction. The studies based on larger samples reported less extreme burnout scores, possibly due to the non-probabilistic nature of the sample and/or biases that may have affected the results.
Although we cannot affirm that the country in which the study was carried out is a key factor in burnout levels, this variable should be taken into account, because the characteristics of the health system in question and the culture and language of the country may influence the prevalence and severity of the syndrome. For example, although the sample was small, the study carried out in Egypt recorded high levels of burnout. The interpretation and extrapolation of these results should take into account aspects such as the validation of the measurement instrument, the understanding of the concept of burnout in Egypt, and the working conditions of paediatric nurses in that country [54].
The burnout measurement instrument and the psychometric data included in the research that we reviewed were also subject to some variability; the most frequently used scale was the Maslach Burnout Inventory (MBI), but many authors used alternative measures. Relatively few studies published reliability coefficients of the measuring instruments, although these data are very important to facilitate the generalisation of the results obtained. Some authors performed a reliability induction in their studies, which in certain cases could be deceptive [49, 50, 62].
Conclusions
A significant number of the paediatric nurses in the sample were found to have medium or high levels of emotional exhaustion and depersonalisation, together with low levels of personal accomplishment. This caused them to suffer burnout or placed them at high risk of developing the syndrome. Certain sociodemographic variables (age), work variables (job satisfaction and workday duration) and psychological variables (stress) should be taken into account in designing measures to prevent the development of burnout syndrome.
Other factors to be considered in evaluating studies of burnout (as well as the interpretation of the results and their possible application to the professional field) include sample size and selection, the adaptation/validation of the measurement instruments used, whether a reliability induction was performed, the health system in the country where the study was carried out, and how the people in that country understand the concept. Finally, other areas such as burnout among paediatricians, and interventions aimed at preventing burnout, directed at all those working in paediatric units, should also be assessed.
Implications for nursing management
This systematic review contributes valuable information concerning burnout among paediatric nurses. it is highly relevant to the scientific community as a whole, but particularly to workers in public health systems. The results obtained show that the prevalence of this syndrome is medium to high, according to the burnout dimension considered, which suggests that a significant number of paediatric nurses are either affected by burnout or liable to develop it in the near future.
In view of the findings presented in this review, further longitudinal studies should be conducted, focusing on burnout risk factors, measures to attenuate the symptoms observed and coping strategies. A better understanding of these questions would significantly contribute to preventing burnout syndrome among paediatric nurses.
Policy and practice implications
The results we present show that interventions should be undertaken to reduce the exhaustion that affects many paediatric nurses and to strengthen their resilience regarding the work, patients and co-workers. Nursing supervisors and managers need to be more aware of the fact that working in a paediatric unit can provoke burnout among nurses. Thus, providing better workplace conditions [61], and the introduction of interventions like mindfulness [63] or support groups where nurses can talk about their feelings [60], can have a positive impact in alleviating this syndrome. If this can be achieved, it will have a positive effect not only on the nurses but also on the quality of care provided and on patient satisfaction.
Supporting information
(PDF)
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The research was carried out within the framework of Research Project P11HUM-7771, directed by PhD Emilia I. De la Fuente and funded by the Regional Government of Andalusia (Spain). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Schaufeli WB, Leiter MP, Maslach C. Burnout: 35 years of research and practice. Career Development International 2009; 14(3): 204–20. doi: 10.1108/13620430910966406 [Google Scholar]
- 2.Berger J, Polivka B, Smoot EA, Owens H. Compassion fatigue in pediatric nurses. Journal of Pediatric Nursing 2015; 30(6): 11–7. doi: 10.1016/j.pedn.2015.02.005 [DOI] [PubMed] [Google Scholar]
- 3.Downey V, Bengiamin M, Heuer L, Juhl N. Dying babies and associated stress in NICU nurses. Neonatal Network 1995; 14(1): 41–6. [PubMed] [Google Scholar]
- 4.Jacobs LM, Nawaz MK, Hood JL, Bae S. Burnout among workers in a pediatric health care system. Workplace Health and Safety 2012; 60(8): 335–44. doi: 10.3928/21650799-20120726-03 [DOI] [PubMed] [Google Scholar]
- 5.Li A, Early SF, Mahrer NE, Klaristenfel JL, Gold JI. Group cohesion and organizational commitment: protective factors for nurse residents' job satisfaction, compassion fatigue, compassion satisfaction, and burnout. Journal of Professional Nursing 2014; 30(1): 89–99. doi: 10.1016/j.profnurs.2013.04.004 [DOI] [PubMed] [Google Scholar]
- 6.Lin TC, Lin HS, Cheng SF, Wu LM, Ou-Yang MC. Work stress, occupational burnout and depression levels: a clinical study of paediatric intensive care unit nurses in Taiwan. Journal of Clinical Nursing 2016; 25(7–8), 1120–30. doi: 10.1111/jocn.13119 [DOI] [PubMed] [Google Scholar]
- 7.Maslach C, Jackson SE. The Maslach Burnout Inventory. Research Edition, Palo Alto, C.A.: Consulting Psychologist Press; 1981. [Google Scholar]
- 8.Meyer RML, Li A, Klaristenfeld J, Gold JI. Pediatric novice nurses: Examining compassion fatigue as a mediator between stress exposure and compassion satisfaction, burnout, and job satisfaction. Journal of Pediatric Nursing 2015; 30(1):174–83. doi: 10.1016/j.pedn.2013.12.008 [DOI] [PubMed] [Google Scholar]
- 9.Pagel I, Wittmann ME. Relationship of burnout to personal and job-related variables in acute-care pediatric settings. Issues in Comprehensive Pediatric Nursing 1986; 9(2): 131–43. [DOI] [PubMed] [Google Scholar]
- 10.Shoffner DH. Communication with patients and professional burnout in pediatric nurses [dissertation] University of Tennessee; 1988. [Google Scholar]
- 11.Stamm BH. Measuring compassion satisfaction as well as fatigue: Developmental history of the Compassion Satisfaction and Fatigue Test In Figley CR, editor. Treating Compassion Fatigue. New York, NY: Brunner-Routledge; 2002. p. 107–22. [Google Scholar]
- 12.Freudenberger HJ. Staff Burnout. Journal of Social Issues 1974; 30(1): 159–65. doi: 10.1111/j.1540-4560.1974.tb00706.x [Google Scholar]
- 13.Maslach C, Jackson S.E. The measurement of experienced burnout. Journal of Occupational Behavior 1981; 2(2): 99–113. doi: 10.1002/job.4030020205 [Google Scholar]
- 14.Cañadas-de la Fuente GA. Medida e identificación de factores de riesgo de padecimiento del síndrome de burnout en personal de enfermería [Dissertation] Madrid, UNED: 2012. [Google Scholar]
- 15.Adriaenssens J, de Gucht V, Maes S. Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. International Journal of Nursing Studies 2015; 52(2): 649–61. doi: 10.1016/j.ijnurstu.2014.11.004 [DOI] [PubMed] [Google Scholar]
- 16.Cañadas-de la Fuente GA, San Luis C, Lozano LM, Vargas C, García I, de la Fuente EI. Evidencia de validez factorial del Maslach Burnout Inventory y estudio de los niveles de burnout en profesionales sanitarios. Revista Latinoamericana de Psicología 2014; 46(1): 44–52. doi: 10.1016/S0120-0534(14)70005-6 [Google Scholar]
- 17.Gallagher R, Gormley DK. Perceptions of stress, burnout, and support systems in pediatric bone marrow transplantation nursing. Clinical Journal of Oncology Nursing 2009; 13(6): 681–5. doi: 10.1188/09.CJON.681-685 [DOI] [PubMed] [Google Scholar]
- 18.Leiter MP, Maslach C. Nurse turnover: the mediating role of burnout. J Nurs Manag. 2009; 17(3):331–339. doi: 10.1111/j.1365-2834.2009.01004.x [DOI] [PubMed] [Google Scholar]
- 19.Gasparino RN Burnout syndrome in the nursing team of a teaching hospital. Cogitare de Enfermagem 2014; 19(2): 210–216. [Google Scholar]
- 20.Czaja AS, Moss M, Mealer M. Symptoms of Posttraumatic Stress Disorder Among Pediatric Acute Care Nurses. Journal of Pediatric Nursing 2012; 27(4): 357–65. doi: 10.1016/j.pedn.2011.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cañadas-De la Fuente GA, Vargas C, San Luis C, García I, Cañadas GR, de la Fuente EI. Risk factors and prevalence of burnout syndrome in the nursing profession. International Journal of Nursing Studies 2015; 52(1): 240–9. doi: 10.1016/j.ijnurstu.2014.07.001 [DOI] [PubMed] [Google Scholar]
- 22.Albendín-García L, Gómez-Urquiza JL, Cañadas-de la Fuente GA, Cañadas GR, San Luis C, Aguayo-Estremera R. Prevalencia bayesiana y niveles de burnout en enfermería de urgencias. Una revisión sistemática. Revista Latinoamericana de Psicología 2016; 48(2): 137–45. doi: 10.1016/j.rlp.2015.05.004 [Google Scholar]
- 23.Gómez Urquiza JL, Aneas-López AB, de la Fuente-Solana EI, Albendín-García L, Díaz-Rodríguez L, Cañadas-de la Fuente GA. Prevalence, risk factors and levels of burnout amongst oncology nurses: A systematic review. Oncology Nursing Forum 2016; 43(3): 301–17. doi: 10.1188/16.ONF.E104-E120 [DOI] [PubMed] [Google Scholar]
- 24.Liakopoulou M, Panaretaki I, Papadakis V, Katsika A, Sarafidou J, Laskari H, Anastasopoulos I, Vessalas G, Bouhoutsou D, Papaevangelou V, Polychronopoulou S, Haidas S. Burnout, staff support, and coping in pediatric oncology. Support Care Cancer 2008; 16(2): 143–150. doi: 10.1007/s00520-007-0297-9 [DOI] [PubMed] [Google Scholar]
- 25.Hecktman HM. Stress in pediatric oncology nurses. Journal of Pediatric Oncology Nursing 2012; 29(6): 356–61. doi: 10.1177/1043454212458367 [DOI] [PubMed] [Google Scholar]
- 26.Robins PM, Meltzer L, Zelikovsky N. The experience of secondary traumatic stress upon care providers working within a children's hospital. Journal of Pediatric Nursing 2009; 24(4): 270–79. doi: 10.1016/j.pedn.2008.03.007 [DOI] [PubMed] [Google Scholar]
- 27.Estabrooks CA, Squires JE, Hutchinson AM, Scott S, Cummings GG, Kang SH, Midodzi WK., Stevens B. Assessment of variation in the Alberta context tool: the contribution of unit level contextual factors and specialty in Canadian pediatric acute care settings. BMC Health Services Research 2011; 11, 251 doi: 10.1186/1472-6963-11-251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jofré AV, Valenzuela SS. Burnout en personal de enfermería de la Unidad de Cuidados Intensivos Pediátricos. Aquichán 2005; 5(1): 56–63. [Google Scholar]
- 29.Moher D, Shamseer L, Clarke M, Ghersi D, Petticrew M, Shekelle P, Steward LA, PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews 2015; 4, 1 doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.OCEBM Levels of Evidence Working Group The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. 2011. Disponible en: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/
- 31.Adwan J Z. Pediatric nurses' grief experience, burnout and job satisfaction. Journal of Pediatric Nursing 2014; 29(4): 329–36. doi: 10.1016/j.pedn.2014.01.011 [DOI] [PubMed] [Google Scholar]
- 32.Alves DF, Guirardello EB. Safety climate, emotional exhaustion and job satisfaction among Brazilian paediatric professional nurses. International Nursing Review 2016; 63(3): 328–35. doi: 10.1111/inr.12276 [DOI] [PubMed] [Google Scholar]
- 33.Bilal A, Ahmed HM Organizational structure as a determinant of job burnout: an exploratory study on Pakistani pediatric nurses. Workplace, Health & Safety 2016; 65(3): 118–28. doi: 10.1177/2165079916662050 [DOI] [PubMed] [Google Scholar]
- 34.Davis S, Bonnie KL, Sorensen C. A comparison of burnout among oncology nurses working in adult and pediatric inpatient and outpatient settings. Oncology Nursing Forum 2013; 40(4): E303–E311. doi: 10.1188/13.ONF.E303-E311 [DOI] [PubMed] [Google Scholar]
- 35.Sekol MA, Kim SC. Job satisfaction, burnout, and stress among pediatric nurses in various specialty units at an acute care hospital. Journal of Nursing Education and Practice 2014; 4(12): 115–24. doi: 10.5430/jnep.v4n12p115 [Google Scholar]
- 36.Squires JE, Estabrooks CA, Scott SD, Cummings GG, Hayduk L, Kang SH, Stevens B. The influence of organizational context on the use of research by nurses in Canadian pediatric hospitals. BMC Health Services Research 2013; 13: 351 doi: 10.1186/1472-6963-13-351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stimpfel AW, Lake ET, Barton S, Gorman KC, Aiken LH. How differing shift lengths relate to quality outcomes in pediatrics. Journal of Nursing Administration 2013; 43(2): 95–100. doi: 10.1097/NNA.0b013e31827f2244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vásquez-Manrique JF, Maruy-Saito A, Verne-Martin E. Frecuencia del síndrome de burnout y niveles de sus dimensiones en el personal de salud del servicio de emergencia de pediatría del Hospital Nacional Cayetano Heredia en el año 2014: Lima, Perú. Revista de Neuro-Psiquiatría 2014; 77(3): 168–174. doi: 10.20453/rnp.2014.2031 [Google Scholar]
- 39.Wilkinson SA. Nurses caring for children and children and families: stress, hardiness and burnout [dissertation] University of British Columbia, Vancouver, Canada; 2014. [Google Scholar]
- 40.Zanatta AB, Lucca SR Prevalence of Burnout syndrome in health professionals of an onco-hematological pediatric hospital. Revista da Escola de Enfermagem da USP 2015; 49(2): 0253–8. doi: 10.1590/S0080-62342015000020001 [DOI] [PubMed] [Google Scholar]
- 41.Messmer PR, Bragg J, Williams PD. Support programs for new graduates in pediatric nursing. Journal of Continuing Education in Nursing 2011; 42(4): 182–92. doi: 10.3928/00220124-20110324-05 [DOI] [PubMed] [Google Scholar]
- 42.Oehler JM, Davidson MG. Job stress and burnout in acute and nonacute pediatric nurses. American Journal of Critical Care 1992; 1(2):81–90. [PubMed] [Google Scholar]
- 43.Oehler J, Davidson MG, Starr LE, Lee DA. Burnout, job stress, anxiety, and perceived social support in neonatal nurses. Heart & Lung: The Journal of Critical Care 1991; 20(5): 500–5. [PubMed] [Google Scholar]
- 44.Jones JW. The staff burnout scale for health professionals: Preliminary test manual Park Ridge, Illinois: London House Management; 1980. [Google Scholar]
- 45.Krafy D, Pines A. The tedium measure Department of Psychology, University of California, Berkeley, California; 1979. [Google Scholar]
- 46.Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress 2005; 19: 192–207. doi: 10.1080/02678370500297720 [Google Scholar]
- 47.Popoff D, Funkhouser GR. What are your feelings about death and dying? Nursing 1975; 5(8): 15–24. [DOI] [PubMed] [Google Scholar]
- 48.Stamm BH. The concise ProQOL manual (2nd ed.). Pocatello, ID: ProQOL.org; 2010. [Google Scholar]
- 49.Aguayo R, Vargas C, de la Fuente EI, Lozano LM. A meta-analytic reliability generalization study of the Maslach Burnout Inventory. International Journal of Clinical and Health Psychology 2011; 11(2): 343–61. [Google Scholar]
- 50.Sánchez-Meca J, López-López JA, López-Pina JA. Some recommended statistical analytic practices when reliability generalization (RG) studies are conducted. British Journal of Mathematical and Statistical Psychology 2013; 66(3): 402–25. doi: 10.1111/j.2044-8317.2012.02057.x [DOI] [PubMed] [Google Scholar]
- 51.Aytekin A, Yilmaz F, Kuguoglu S. Burnout levels in neonatal intensive care nurses and its effects on their quality of life. Australian Journal of Advanced Nursing 2013; 31(2): 39–48. [Google Scholar]
- 52.Akman O, Ozturk C, Bektas M, Ayar D, Armstrong MA. Job satisfaction and burnout among paediatric nurses. Journal of Nursing Management 2016; 24(7): 923–33. doi: 10.1111/jonm.12399 [DOI] [PubMed] [Google Scholar]
- 53.Battles HB. Professional self-efficacy as a moderator of the relationship between stress and burnout among pediatric HIV/AIDS health care providers (Immune deficiency) [Dissertation] George Washington University; 2000. [Google Scholar]
- 54.Moussa M, Mahmood A. The relationship between nurses’ burnout and mothers’ satisfaction with pediatric nursing care. International Journal of Current Research 2013; 5(7): 1902–7. [Google Scholar]
- 55.Parada ME, Moreno R, Mejías Z, Rivas A, Cerrada J, Rivas F. Satisfacción laboral y síndrome de Burnout en el personal de enfermería del instituto autónomo hospital universitario los andes. Revista Facultad Nacional de Salud Pública 2005; 23(1): 33–45. [Google Scholar]
- 56.Hawes K. Nurse job stress, burnout, practice environment and maternal satisfaction in the neonatal intensive care unit [dissertation] University of Rhoden Island; 2009. [Google Scholar]
- 57.Budnik MF. Emotional intelligence and burnout: Influence on the intent of staff nurses to leave nursing [dissertation] University of Phoenix; 2003. [Google Scholar]
- 58.Berkowitz NF. Nurses' attitudes toward caring for HIV-infected children [Dissertation] Boston College; 1993. [Google Scholar]
- 59.Edmonds C, Lockwoo GM, Bezjak A, Nyhof-Young J. Alleviating emotional exhaustion in oncology nurses: an evaluation of Wellspring’s “Care for the Professional Caregiver Program”. Journal of Cancer Education 2012; 27(1): 27–36. doi: 10.1007/s13187-011-0278-z [DOI] [PubMed] [Google Scholar]
- 60.Cañadas-De la Fuente GA, Gómez-Urquiza JL, Ortega-Campos EM, Cañadas GR, Albendín-García L, De la Fuente-Solana EI. Prevalence of burnout syndrome in oncology nursing: a meta-analytic study. Psychooncology. 2018; In press. doi: 10.1002/pon.4632 [DOI] [PubMed] [Google Scholar]
- 61.Gómez-Urquiza JL, De la Fuente‐Solana EI, Albendín‐García L, Vargas‐ Pecino C, Ortega‐Campos EM, Cañadas‐De la Fuente GA. Prevalence of burnout syndrome in emergency nurses: a meta‐analytic study. Crit Care Nurse. 2017;37(5):e1‐e9. doi: 10.4037/ccn2017508 [DOI] [PubMed] [Google Scholar]
- 62.Vacha-Haase T, Kogan LR, Thompson B. Sample compositions and variabilities in published studies versus those in test manuals. Educational and Psychological Measurement 2000; 60(4): 509–22. doi: 10.1177/00131640021970682 [Google Scholar]
- 63.Gracia-Gracia P, Oliván-Blázquez B. Burnout and mindfulness self-compassion in nurses of intensive care units: cross-sectional study. Holistic Nursing Practice; 2017: 31(4):225–233. doi: 10.1097/HNP.0000000000000215 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.