Abstract
Background
Globally, adolescent girls’ physical activity (PA) levels are low. The ‘Girls Active’ secondary school-based programme, developed by the Youth Sport Trust, aims to increase PA in adolescent girls. This paper explores the effectiveness of the ‘Girls Active’ school-based PA programme.
Methods
A random sample of girls aged 11–14 from 20 secondary schools (Midlands, UK) participated in a two-arm cluster randomised controlled trial. Ten schools received Girls Active and 10 continued with usual practice. Measurements were taken at baseline, seven- and 14-month follow-up. Primary outcome: wrist-worn accelerometer measured moderate- to vigorous-intensity PA (MVPA). Secondary outcomes: overall PA, light PA, sedentary time, body composition, and psychosocial outcomes. Generalised estimating equations, adjusted for school cluster and potential confounders, were used and A priori subgroup analysis was undertaken. Micro-costing and cost-consequence analyses were conducted using bespoke collection methods on programme delivery information. Outcomes for the cost-consequence analysis were health related quality of life measured by the Child Health Utility-9D and service use.
Results
Overall, 1752 pupils participated, 1211 (69.1%) provided valid 14-month accelerometer data. No difference in MVPA (mins/day; 95% confidence intervals) was found at 14 months (1.7; -0.8 to 4.3), there was at seven months (2.4; 0.1 to 4.7). Subgroup analyses showed significant intervention effects on 14-month in larger schools (3.9; 1.39 to 6.09) and in White Europeans (3.1; 0.60 to 6.02) and in early maturers (5.1; 1.69 to 8.48) at seven months. The control group did better in smaller schools at 14-months (-4.38; -7.34 to -1.41). Significant group differences were found in 14-month identified motivation (-0.09; -0.18 to -0.01) and at seven months in: overall PA (1.39 mg/day; 0.1 to 2.2), after-school sedentary time (-4.7; -8.9 to -0.6), whole day (5.7; 1.0 to 10.5) and school day (4.5; 0.25 to 8.75) light PA, self-esteem. Small, statistically significant, differences in some psychosocial variables favoured control schools. Micro-costing demonstrated that delivering the programme resulted in a range of time and financial costs at each school. Cost-consequence analysis demonstrated no effect of the programme for health related quality of life or service use.
Conclusions
Compared with usual practice, ‘Girls Active’ did not affect 14-month MVPA.
Trial registration
Keywords: Intervention, Physical education, Teacher, Adolescent female
Background
Youth physical activity (PA) levels worldwide [1] and in the UK [2] are low despite the physiological and psychological benefits [3]. Adolescent females have been highlighted as a particular group at risk of declining PA with recent data showing that only 16% and 9% of girls aged 11–12 and 13–15 years, respectively, are sufficiently active [2]. Although the decline in PA may begin prior to the transition between primary and secondary (high) school, and occurs in both boys and girls [4], there is a need to identify ways to stem the decline in PA in girls once they enter secondary schools as the decline is steeper and faster in girls than boys. Schools have been highlighted as a setting to tackle the inactivity crisis [5–7] using a variety of strategies [8–12]. Effects are generally small and short-term [11, 13]. Furthermore, potential mediators of physical activity changes (i.e. to help explain effectiveness) are not robustly or routinely assessed [14]. Reviews have identified that much of the evidence comes from the US, [8, 9] and there is an absence of robust “proven” or “promising” practice within the UK [15].
In an effort to tackle youth inactivity the Youth Sport Trust (YST; the largest non-profit organisation focussing on youth sport and activity in the UK) have developed programmes designed to support schools in engaging girls in PA. ‘Girls Active’ is one such programme which uses peer leadership and marketing to empower adolescent girls to influence school decisions, develop themselves as role models, and promote PA to peers. Schools are provided with training and resources to review the their PA, sport and physical education (PE) provision, culture and practices to girls and to create action plans for how they will implement changes. The programme had not been robustly or independently evaluated.
The aim of this study was to assess the effectiveness of the Girls Active PA programme in UK secondary schools.
Methods
Ethics approval and study sponsorship were obtained from the University of Leicester. The sponsor had no role in the design, undertaking or reporting of the study. School principals provided written consent for their school to participate. Parents/guardians were provided with an opt out consent form and only pupils who did not return the opt out consent form participated. Participants provided verbal assent prior to each measurement session and could withdraw at any time.
Design
This cluster RCT had follow-up at seven and 14 months. Following baseline measurements, schools were randomised by an independent statistician to one of two groups stratified by school size (pupil median: < 850, ≥850) and percent black and minority ethnicity (BME) pupils (median: < 20%, ≥20%). Sequentially numbered sections within a folder were used to implement the group allocations. The investigator team were not aware of the sequence until after randomisation. Measurement team members, except the team lead for the day, were blinded to group randomisation. The trial statistician was not blinded. However, the statistical analysis plan was signed off prior to database lock and any deviations from the analysis plan are reported herein.
Stakeholder involvement
Girls Active is built on over 10 years of work by the YST that includes consultations with school senior leaders, teachers, young people, national agencies and corporate partners. This extended to consultations with adolescent girls and their teachers in order to refine the programme prior to this evaluation study. The research team consulted with two groups (n = 8 and n = 6) of adolescents and PE teachers (n = 3) at local schools in Leicester City ahead of the funding application. This informed the decision around outcome measures: i.e. preference of a wrist worn accelerometer over one worn on the hip or the thigh, economic evaluation cost diaries and process evaluation themes and questions. Key stakeholders were involved in the study as two lay members sat on the trial steering committee (TSC). Lead teachers co-designed their own school reports so that anonymised baseline data specific to their school could be used within their schools. Further dissemination will be undertaken to the study participant through a further anonymised school level report as well as a briefing event for school leads and other personnel involved in education, sport and physical activity decision making. Stakeholders were not involved in decisions around study design, recruitment or conduct of the study and the burden of the programme was not assessed.
Participants and school clusters
All state (government funded) secondary schools in Leicester City, Leicestershire and Rutland (LLR), UK (n = 56) with a Key Stage 3 (KS3: age 11–14 years) were eligible and were sent a letter of invitation to the study. Of these, 25 agreed to come to a briefing event about the study, 15 attended of which 14 obtained consent from the school principal for their school to participate. In tandem, a further 26 state schools that were geographically close to LLR but in neighbouring counties were approached and 6 of these consented to participate. Schools provided the research team a list of all eligible girls between the ages of 11 and 14 years and in years 7, 8 and 9. All eligible pupils were provided with an information pack that contained a separate participant and parent/guardian information sheet and opt out consent form as well as an invitation letter. Pupils had two weeks to return the opt out consent form. Using a random number generator, 90 girls from each school were chosen at random (split between year groups).
Sample size
This study was designed to provide adequate power to detect a meaningful group difference [16] in MVPA of 10 mins/day assuming a standard deviation of 18 mins/day in MVPA [17], a power of 90%, a significance of 0.05, a cluster size of 56 girls and an intra-class correlation of 0.1. Twenty schools and ≥ 80 girls/cluster allowed for cluster attrition and 30% loss to follow-up and non-compliance with accelerometer wear.
Participant assessments
Measurement sessions took place at school during the school day. There was an explanation of methods, the assent process, question and answers and the accelerometer protocol.
Objective PA
Methods used in this study have been described in the protocol paper [18]. Briefly, girls wore a GENEActiv accelerometer 24 h/day for seven days on their non-dominant wrist at all time-points and were given a £5 gift voucher on return of the device with at least 4 days of data collected. The GENEActiv devices were initialised with a sampling frequency of 100 Hz and set to start recording at midnight on the first day of data collection and stop recording at midnight seven days later.
Data processing
GENEActiv .bin files were analysed with R-package GGIR v1.2–11 (http://cran.r-project.org) [19, 20]. Variables of interest were calculated over the 24 h day using published thresholds: MVPA, overall PA (average acceleration; derived using the Euclidean Norm Minus One method), light PA and sedentary time [21, 22]. Sedentary time was partitioned out from sleep using the nocturnal sleep detection algorithm in GGIR [23]. The meeting of PA guidelines [24] was calculated as those achieving ≥ 60 mins MVPA on each measurement day. Accelerometer variables were calculated for the whole day and by specific periods: during school, after school (up to 9 pm), school days and non-school days. Each school’s own start and end times were used to define school hours variables. PA data analysis include participants with ≥ 16 h of wear-time during each 24 h period [25] on ≥ 2 days including ≥ 1 school day.
Psychological outcomes
A range of psychological factors that may mediate PA participation were self-reported on a paper-based questionnaire as described in the protocol paper [18]: intentions and motivation to be active; attitudes to PA; perceived family, peer and teacher social support for PA; perceptions of the school social and physical environment; PA self-efficacy and enjoyment; perceived importance of PA, and physical self-perceptions (self-esteem, body attractiveness and physical self-worth).
Anthropometric and body composition measurements
Standing and sitting heights (Seca 213 stadiometer, Seca, Birmingham, UK) and weight (Tanita SC-330ST, Tanita Europe BV, Middlesex, UK) were assessed to the nearest 0.1 cm and 0.1 kg, respectively, using standardised procedures. Body mass index (BMI) was calculated and converted into z-scores relevant to the UK population [26]. Percentage body fat was estimated using pediatric scales (Tanita SC-330ST, Tanita Europe BV, Middlesex, UK).
Potential covariates
Participant age (in months) was calculated from date of birth, year group was self-reported, and socioeconomic status was represented by calculating the index of multiple deprivation (IMD) from participants’ self-reported postcode. Age at peak height velocity (APHV) was used as an indicator of biological maturity category [27].
School level data
School level socioeconomic position/deprivation was represented by the percentage of pupils eligible for free school meals (%FSME) from the relevant 2015 school census [28]. School pupil numbers were reported by the lead teacher and verified by 2015 school census data.
Intervention group – Girls Active programme
Details of the Girls Active programme have been described in the protocol paper [18]. The aim of Girls Active is to provide a support framework for schools to review and change their PA, PE and school sport culture and practices with the support of the YST and a hub school. Teachers completed a school self-review and attended an initial training day delivered by a YST national tutor. At this day, teachers discussed the programme elements (including establishing a peer leader group) and started developing their school action plan. They received a folder of case studies and electronic versions of marketing materials for promotion within their school. One of the key elements to the programme was the formation of a girls leadership and peer marketing group to empower girls to influence PE, sport and PA in their school, develop as role models, and promote and market PA to other girls. Over the course of the programme, resources for lead teachers were uploaded to an online file sharing system. School leads attended a peer review day to share practice with other teachers facilitated by the development coach and a hub school teacher. Lead teachers were offered in-person or phone support through the hub school or development coach. Lead teachers were free to implement the programme flexibly in whatever way they wished but were encouraged to set up a peer leader group who were to market PA to their peers and help prioritise PA decisions within their school. Teachers were encouraged to identify pupils that are not necessarily the sporty pupils but those who bring a range of perspectives and could communicate with, and motivate their peers. They were provided with two £500 capacity funding instalments to coincide with action plan submission. The programme was delivered in the same manner as would have been done in the real-world setting and, in theory, Girls Active has the potential to continue on in schools if implemented with sustainability and embedding in mind. The elements of the “off-the-shelf” programme which was originally developed without specific reference to theory were mapped to constructs in social cognitive theory post-hoc by the academic team (Fig. 1). Seven core components of Girls Active were identified: submission of the first self-review and action plans; attendance of lead teacher at initial training; use of package of resources or use of an alternative; engagement of young people as peer leaders; use of online, in person or phone support of hub and/or development coach; lead teacher attendance at peer review day; and submission of the second mission analysis. The intervention was delivered at the cluster level but the participant data reported herein were collected at the individual level.
Fig. 1.
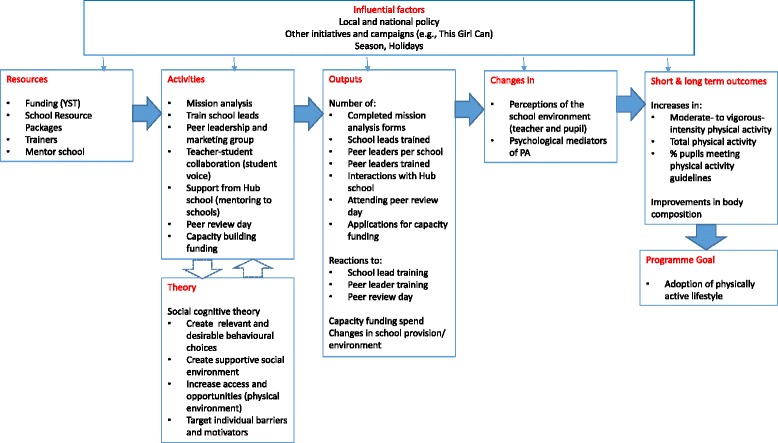
Proposed logic model for the Girls Active programme
Control group - usual practice
Control arm schools were not given any specific guidance or advice and were assumed to carry on with their usual practice of PE and sport provision.
Primary and secondary outcomes
The primary outcome was difference in the change in mean mins/day of MVPA at 14-month follow-up between groups. Secondary outcomes included: overall PA; sedentary time; and all PA outcomes split by weekday and weekend day, and during school hours and after school hours; BMI z-score; percentage body fat; and psychological factors that may mediate PA participation as described above.
Economic analysis
A full description of the economic assessment methods of the Girls Active trial are available [29]. Briefly, micro-costing methodology [30] was applied to calculate the costs of delivering the programme over a whole school year for the intervention arm schools. This provides a mean cost per school. Money and time spent on delivering Girls Active were self-reported by lead teachers using two types of bespoke cost diaries and a questionnaire and, if needed, these were followed up with a phone call for clarification. The cost-consequence analysis was conducted from a public sector, multi-agency perspective. Health related quality of life measured by the Child Health Utility-9D [31] was used as the measure of effect. Use of GP and school based services (school nurse and school counsellor) were used as the measure of costs. These were all self-reported by participants at each timepoint.
Statistical analysis
The results are reported according to the CONSORT statement for cluster RCTs [32]. Primary and secondary outcome analyses were based on a complete case analysis. Intention to treat (ITT; all schools and recruited pupils were analysed in the group they were randomised to) and per protocol analyses were also undertaken for the primary outcome as sensitivity analyses. The per protocol population included schools that engaged with 70% of the seven core components (as detailed above) of the programme over the 14 months and had complete data for the analysis concerned on ‘by analysis’ basis. In the control arm, the per protocol population included all schools/pupils randomised to that arm.
Generalised estimating equations, accounting for school level clustering, and adjusting for baseline MVPA, stratification factors of school size (< 850, ≥ 850) and % of non-White pupils (< 20%, ≥ 20%), %FSME and participant year group, were employed. Subgroup analyses involved within subgroup stratification and between subgroup interactions effects between the intervention arm and pre-specified subgroups: baseline school (social deprivation and size) and pupil (ethnicity, maturation status, year group, PA level) characteristics. Sensitivity analyses explored the effect of the number of valid accelerometer days and the season of data collection. All analyses were performed using Stata (v.14.0), with statistical significance set as p < 0.05. Changes from the agreed statistical analysis plan included the addition of %FSME (school SES) and participant year group as covariates in the primary and secondary outcomes analyses.
Results
In Spring 2015, 20 secondary schools were recruited (Fig. 2). Of these, 18 schools agreed to be followed-up at seven months, and 19 at 14 months. From these schools, 1752 adolescent girls provided assent and participated at baseline (Feb – April 2015), 1405 (80.2%) at seven months (Sept – Nov 2015), and 1361 (77.7%) at 14 months (April – June 2016). Tables 1 and 2 present the baseline characteristics of the schools and participants, respectively. Participants who did not complete the 14 month assessment (n = 301) were older (p < 0.001), had a higher BMI z-score (p = 0.021) and provided 0.2 days less accelerometer data (p < 0.001) at baseline (Table 3). Complete accelerometer data (i.e., ≥ 2 valid days, including at least one school day at baseline and 14 months) was available for 1211 participants (69.1%) for the primary outcome analysis at 14-month follow-up. No serious adverse events/reactions were reported.
Fig. 2.
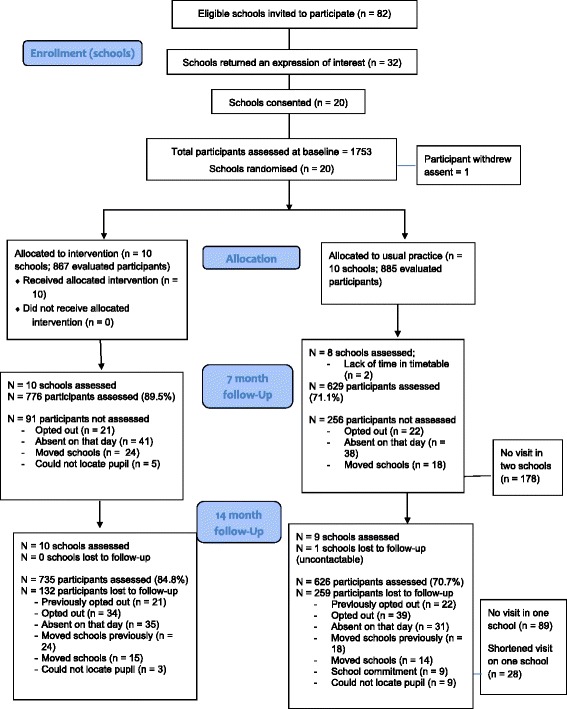
CONSORT flow chart for the Girls Active cluster randomised controlled trial
Table 1.
Baseline characteristics of each school (cluster) by randomised group; usual practice (control) or the Girls Active programme (intervention)
| Characteristics | Control (n = 10) |
Intervention (n = 10) |
Total (n = 20) |
|---|---|---|---|
| Cluster Level | |||
| Number of participants, n (SD) | 89 (2.0) | 87 (3.0) | 88 (2.0) |
| Non-White participants, % (SD) | 21.3 (27.7) | 19.3 (24.1) | 20.3 (25.3) |
| Overall School Characteristics | |||
| Full-time pupils, n (SD) | 977 (199) | 859 (386) | 918 (305) |
| Non-White pupils, % (SD) | 25.4 (34.2) | 21.6 (28.0) | 23.5 (30.5) |
| FSME, % (SD) | 9.7 (6.2) | 13.3 (5.6) | 11.5 (6.1) |
| IMD decile score, score (SD)a | 7.2 (2.3) | 6.1 (2.5) | 6.7 (2.4) |
| IMD rank score, score (SD) | 21,840 (8013) | 18,949 (7860) | 20,395 (7866) |
| Schools ≥ 850 pupils, n (%) | 8 (80.0) | 6 (60.0) | 14 (70.0) |
All values, unless otherwise stated, are presented as a mean and standard deviation (SD) across schools; Values are presented as means (standard deviation) for continuous variables and number (%) for categorical variables. FSME Free School Meal Eligibility; IMD Index of Multiple Deprivation
aIMD 2015 decile score ranges 1–10, where 1 is the least deprived and 10 the most deprived
Table 2.
Baseline characteristics at the individual participant level by randomised group; usual practice (control) or the Girls Active programme (intervention)
| Individual level characteristics | Control (n = 885) |
Intervention (n = 867) |
Total (n = 1752) |
|---|---|---|---|
| Age, years (SD) | 12.8 (0.8) | 12.8 (0.8) | 12.8 (0.8) |
| Year group categories, n (%) | |||
| Year 7 | 356 (40.2) | 318 (36.7) | 674 (38.5) |
| Year 8 | 355 (40.1) | 365 (42.1) | 720 (41.1) |
| Year 9 | 174 (19.7) | 184 (21.2) | 358 (20.4) |
| Ethnicity categories, n (%) | |||
| White European | 669 (75.9) | 673 (77.1) | 1342 (76.8) |
| South Asian | 123 (14.0) | 81 (9.4) | 204 (11.7) |
| Other | 90 (10.2) | 112 (12.9) | 202 (11.6) |
| IMD decile, score (SD)a | 6.5 (2.8) | 5.1 (2.7) | 5.8 (2.8) |
| IMD rank, score (SD) | 19,649 (9395) | 15,322 (8840) | 17,505.8 (9375) |
| Biometric Measurements | |||
| Average standing height, cm (SD) | 156.1 (7.9) | 155.8 (7.8) | 156.0 (7.9) |
| Average sitting height, cm (SD) | 81.5 (4.6) | 81.1 (4.6) | 81.3 (4.6) |
| Body mass, kg (SD) | 48.7 (12.4) | 48.9 (12.4) | 48.8 (12.4) |
| BMI, z-score (SD) | 0.14 (1.3) | 0.22 (1.3) | 0.18 (1.3) |
| Percent body fat, % (SD) | 23.9 (7.6) | 24.2 (7.8) | 24.1 (7.7) |
| APHV, years (SD) | 12.1 (0.5) | 12.1 (0.5) | 12.1 (0.5) |
| BMI categories, n (%) | |||
| Underweight | 136 (15.7) | 129 (15.2) | 265 (15.4) |
| Normal weight | 543 (62.6) | 530 (62.4) | 1073 (62.5) |
| Overweight | 154 (17.7) | 149 (17.5) | 303 (17.6) |
| Obese | 35 (4.0) | 42 (4.9) | 77 (4.5) |
| Biological maturity categories, n (%) | |||
| Early | 139 (16.4) | 125 (15.0) | 264 (15.7) |
| Average | 576 (68.0) | 570 (68.5) | 1146 (68.3) |
| Late | 132 (15.6) | 137 (16.5) | 269 (16.0) |
| Accelerometer variables | |||
| MVPA, mins/day [IRQ] | 43.9 [30.6-58.0] | 41.8 [29.2-56.1] | 42.6 [29.9-57.0] |
| Light PA, mins/day [IRQ] | 279.5 [247.8-307.0] | 272.5 [244.5-302.7] | 275.8 [246.1-305.0] |
| Sedentary, mins/day [IRQ] | 549.4 [508.5-592.1] | 552.6 [516.0-594.3] | 550.6 [511.7-593.5] |
| Overall PA, mg (SD) | 36.7 (8.9) | 35.7 (8.8) | 36.2 (8.9) |
| Valid days, number (SD) | 6.6 (1.1) | 6.8 (0.9) | 6.7 (1.0) |
| Pupil’s achieving ≥ 60 mins MVPA on every valid day, n (%) | 20 (2.3) | 20 (2.4) | 40 (2.3) |
Values are presented as means (standard deviation) or median [interquartile range] for continuous variables and number (%) for categorical variables
aIMD 2015 decile score ranges 1–10, where 1 is the least deprived and 10 the most deprived
IMD index of multiple deprivation; BMI body mass index; APHV age at peak height velocity; MVPA moderate- to vigorous-intensity physical activity; PA physical activity
Missing data: 2 age; 4 ethnicity; 123 pupils social deprivation score; 30 standing height; 50 sitting height; 7 body weight; 34 BMI; 33 percentage body fat; 73 APHV, biological maturity; 44 MVPA, light PA; 46 pupils meeting PA guidelines, number of valid days; 58 sedentary; 0 all other variables
Table 3.
Baseline characteristics of completers versus non-completers at 14 month follow-up
| Characteristics | Completers (n = 1361) |
Non-completers (n = 301) |
P-valuea |
|---|---|---|---|
| Age, years (SD) | 12.8 (0.8) | 13.1 (0.8) | < 0.001 |
| Year group categories, n (%) | |||
| Year 7 | 571 (41.9) | 73 (24.2) | |
| Year 8 | 544 (39.9) | 147 (48.8) | |
| Year 9 | 247 (18.1) | 81 (26.9) | < 0.001 |
| Ethnicity categories, n (%) | |||
| White European | 1014 (74.6) | 244 (81.1) | |
| South Asian | 175 (12.9) | 28 (9.3) | |
| Other | 170 (12.5) | 29 (9.6) | 0.060 |
| IMD decile, score (SD)b | 5.8 (2.8) | 5.8 (3.0) | 0.678 |
| Biometric measurements | |||
| Average standing height, cm (SD) | 155.6 (7.9) | 157.8 (7.0) | < 0.001 |
| Average sitting height, cm (SD) | 81.1 (4.6) | 82.2 (4.1) | < 0.001 |
| Body mass, kg (SD) | 48.1 (12.2) | 51.3 (12.7) | < 0.001 |
| BMI, z-score (SD) | 0.13 (1.3) | 0.33 (1.3) | 0.021 |
| APHV, years (SD) | 12.1 (0.5) | 12.1 (0.5) | 0.600 |
| Accelerometer variables | |||
| MVPA, mins/day [IRQ] | 42.5 [30.2-55.6] | 40.8 [30.1-60.2] | 0.598 |
| Light PA, mins/day [IRQ] | 275 [246-305] | 274.9 [246-304] | 0.634 |
| Sedentary, mins/day [IRQ] | 550 [511-593] | 550.7 [514-595] | 0.600 |
| Valid days, number (SD) | 6.7 (0.9) | 6.5 (1.2) | < 0.001 |
| Pupils achieving ≥60 mins MVPA on every valid day, n (%) | 32 (2.4) | 5 (2.0) | 0.597 |
IMD index of multiple deprivation; BMI body mass index; APHV age at peak height velocity; MVPA moderate- to vigorous-intensity physical activity; PA physical activity
Missing data: 2 age; 2 ethnicity; 110 pupils social deprivation score; 29 standing height; 50 sitting height; 6 body weight; 33 BMI, BMI categories; 56 percentage body fat; 72 APHV, biological maturity; 41 light PA, 43 pupils meeting PA guidelines, 41 number of valid days; 52 sedentary; 0 all other variables
NOTE: Completers included all those who assented at the 14 month visit from all 18 completing schools and the one school with the modified 14 month visit. Non-completers included all those who did not provide assent at the 14 month visit from all 18 completing schools and the one school with the modified 14 month visit. Participants from one school lost to follow-up were not included in either group
aP-values test for the difference between completers and non-completers and were estimated using either two sample t-test, Chi-squared test or Wilcoxon rank sum test, as appropriate
bIMD 2015 decile score ranges 1–10, where 1 is the least deprived and 10 the most deprived
Primary outcome analysis
There were no differences between intervention and control groups at 14 months for the change in mean mins/day of MVPA in the complete case (1.8 mins/day; 95% C.I. -0.8 to 4.3; p = 0.178), intention-to-treat (1.7 mins/day; 95% C.I. -0.6 to 3.9; p = 0.158) or per protocol (1.7 mins/day; 95% C.I. -1.15 to 4.48; p = 0.246) analyses (Table 4). At seven months, a difference in MVPA between groups was found in the complete case (2.4 mins/day; 95% C.I 0.1 to 4.7; p = 0.039), intention-to-treat (2.3 mins/day; 95% C.I. 0.2 to 4.3; p = 0.028) and per-protocol (3.1 mins/day; 95% C.I. 0.93 to 5.35; p = 0.005) analyses.
Table 4.
Changes in minutes per day of MVPA at 7 and 14 (primary outcome) month follow-up between participants randomised to usual practice (control) or to the Girls Active programme (intervention)a
| Number of schools | pupils | Mean change from baseline (95% C.I.) | Adjusted difference at follow-upb | |||||
|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Coefficient (95% C.I.) | P-value | ICC | |
| Complete casec | |||||||
| 7 months | 8 | 572 | 10 | 730 | -6.18 (-7.30 to -5.06) | -2.45 (-3.50 to -1.41) | 2.42 (0.13 to 4.72) | 0.039 | 0.03 |
| 14 months | 9 | 539 | 10 | 672 | -3.47 (-4.91 to -2.03) | -2.09 (-3.27 to -0.90) | 1.75 (-0.80 to 4.29) | 0.178 | 0.02 |
| Per protocold | |||||||
| 7 months | 8 | 572 | 8 | 586 | -6.18 (-7.30 to -5.06) | -1.91 (-3.11 to -0.72) | 3.14 (0.93 to 5.35) | 0.005 | 0.02 |
| 14 months | 9 | 539 | 8 | 549 | -3.47 (-4.91 to -2.03) | -1.46 (-2.74 to -0.18) | 1.67 (-1.15 to 4.48) | 0.246 | 0.02 |
| Intention-to-treate | |||||||
| 7 months | 10 | 885 | 10 | 867 | -5.92 (-7.05 to -4.78) | -2.50 (-3.57 to -1.44) | 2.30 (0.25 to 4.35) | 0.028 | - |
| 14 months | 10 | 885 | 10 | 867 | -3.63 (-5.03 to -2.23) | -2.01 (-3.20 to -0.81) | 1.65 (-0.64 to 3.94) | 0.158 | - |
CI confidence interval; ICC intra-class correlation; MVPA moderate- to vigorous-intensity physical activity
aIncluding pupils who have worn the accelerometer with a minimum of two valid days with at least one school day at baseline and 7 months, and at baseline and 14 months
bDifference in the mean MVPA at follow-up adjusted for cluster effect, baseline MVPA value, participant year group, school percentage free school meal eligibility and stratification categories (school size and percentage of non-White pupils)
cThose with missing outcome data or missing variables required for the model adjustment are excluded
dSchools that did not engage with 70% of the programme have been excluded from this analysis
eMissing data imputed using multiple imputation
Subgroup analysis
Between subgroup interaction effects revealed subgroup effects (i.e. the programme had a differing effect depending on certain baseline characteristics) at 14 and seven months (Figs. 3 and 4, respectively). At 14 months, the between subgroup interaction effects (p < 0.001) revealed a difference between randomised arms of 3.9 mins/day (95% C.I. 1.39 to 6.09; p < 0.001) favouring the intervention arm in larger schools (≥ 850 pupils). In smaller schools (< 850 pupils) there was a difference between randomised arms of -4.4 mins/day (95% C.I. -7.34 to -1.41; p = 0.004) favouring the control arm. At seven months, in White European and early maturers there was a difference between randomised arms of 3.1 mins/day (95% C.I. 0.60 to 6.02; p = 0.017) and 5.1 mins/day (95% C.I. 1.69 to 8.48; p = 0.003), respectively, favouring the intervention arm.
Fig. 3.
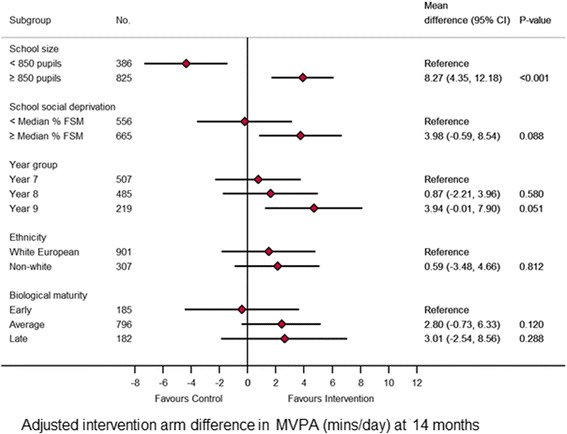
Forest plot of the effect of the intervention at 7 months on the primary endpoint by subgroups
Fig. 4.
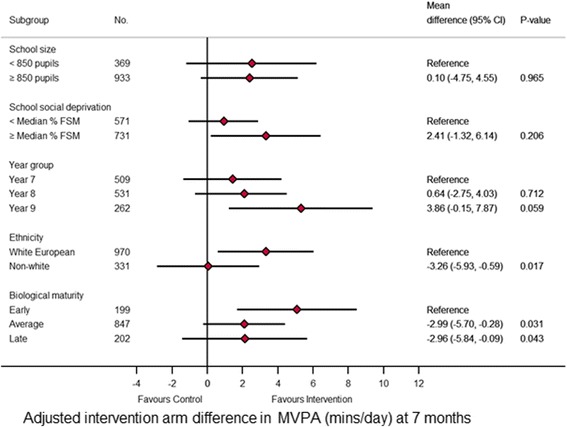
Forest plot of the effect of the intervention at 14 months on the primary endpoint by subgroup
Accelerometer secondary outcomes
No differences were found in the MVPA variables at seven or 14 months when stratified by weekday/weekend or time of day (Table 5). Generally, there were no changes in the other accelerometer variables at seven or 14 months except a significant difference in total PA at seven months (1.4 mg; 95% C.I. 0.1 to 2.2; p = 0.030), in sedentary time during the after school period at seven months (-4.7 mins/day; 95% C.I. -8.9 to -0.6; p = 0.026), in total light PA at seven months (5.7 mins/day; 95% C.I 1.0 to 10.5; p = 0.018), and light PA on school days at 7 months (4.5 mins/day; 0.3 to 8.8; p = 0.038). No differences were found in the proportions of participants active at least 60 min over the measurement period at either seven or 14 months.
Table 5.
Objectively measured activity variables at follow-up between participants randomised to usual practice (control) or to the Girls Active programme (intervention)a
| Number of schools | pupils | Adjusted difference at follow-upb | ||||
|---|---|---|---|---|---|
| Control | Intervention | Coefficient (95% C.I.) | P value | ICC | |
| MVPA (mins/day) | |||||
| School days | |||||
| Baseline | 10 | 854 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 746 | 1.84 (-0.52 to 4.20) | 0.126 | 0.02 |
| 14 months | 9 | 578 | 10 | 693 | 1.79 (-1.27 to 4.85) | 0.251 | 0.02 |
| Weekend | |||||
| Baseline | 10 | 828 | 10 | 827 | |||
| 7 months | 8 | 561 | 10 | 702 | 2.78 (-2.37 to 7.92) | 0.290 | 0.04 |
| 14 months | 9 | 503 | 10 | 637 | 0.99 (-3.54 to 5.51) | 0.669 | 0.02 |
| During school hours | |||||
| Baseline | 10 | 855 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 746 | 0.73 (-0.84 to 2.30) | 0.360 | 0.05 |
| 14 months | 9 | 578 | 10 | 693 | 0.84 (-0.50 to 2.18) | 0.218 | 0.02 |
| After-school hours | |||||
| Baseline | 10 | 855 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 746 | 0.51 (-0.79 to 1.78) | 0.443 | 0.02 |
| 14 months | 9 | 578 | 10 | 693 | 0.39 (-1.61 to 2.39) | 0.701 | 0.03 |
| Average acceleration (ENMO; mg/day) | |||||
| All days | |||||
| Baseline | 10 | 858 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 747 | 1.39 (0.09 to 2.18) | 0.033 | 0.03 |
| 14 months | 9 | 578 | 10 | 694 | 0.66 (-0.62 to 1.95) | 0.314 | 0.02 |
| School days | |||||
| Baseline | 10 | 854 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 747 | 0.89 (-0.18 to 1.95) | 0.102 | 0.03 |
| 14 months | 9 | 578 | 10 | 693 | 0.46 (-0.91 to 2.02) | 0.460 | 0.03 |
| Weekend | |||||
| Baseline | 10 | 828 | 10 | 827 | |||
| 7 months | 8 | 559 | 10 | 702 | 1.39 (-1.13 to 3.92) | 0.280 | 0.05 |
| 14 months | 9 | 503 | 10 | 637 | 0.51 (-1.49 to 2.51) | 0.619 | 0.02 |
| Sedentary time (mins/day) | |||||
| All days | |||||
| Baseline | 10 | 848 | 10 | 846 | |||
| 7 months | 8 | 588 | 10 | 732 | -5.76 (-12.90 to 1.38) | 0.114 | 0.01 |
| 14 months | 9 | 565 | 10 | 680 | -2.64 (-13.03 to 7.75) | 0.618 | 0.01 |
| School days | |||||
| Baseline | 10 |840 | 10 | 844 | |||
| 7 months | 8 | 586 | 10 | 726 | -4.17 (-10.74 to 2.40) | 0.213 | 0.01 |
| 14 months | 9 | 559 | 10 | 676 | -0.08 (-12.72 to 12.55) | 0.990 | 0.02 |
| Weekends | |||||
| Baseline | 10 | 815 | 10 | 806 | |||
| 7 months | 8 | 553 | 10 | 680 | -9.73 (-27.41 to 7.95) | 0.281 | 0.02 |
| 14 months | 9 | 485 | 10 | 619 | -10.27 (-20.63 to 0.10) | 0.052 | < 0.001 |
| During school hours | |||||
| Baseline | 10 | 855 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 746 | 3.83 (-4.13 to 11.78) | 0.356 | 0.08 |
| 14 months | 9 | 578 | 10 | 693 | 2.49 (-4.84 to 9.81) | 0.506 | 0.06 |
| After-school hours | |||||
| Baseline | 10 | 855 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 746 | -4.72 (-8.89 to -0.56) | 0.026 | 0.02 |
| 14 months | 9 | 578 | 10 | 693 | -1.38 (-6.68 to 3.92) | 0.610 | 0.02 |
| Time spent in light PA (mins/day) | |||||
| All days | |||||
| Baseline | 10 | 858 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 747 | 5.71 (0.96 to 10.46) | 0.018 | 0.01 |
| 14 months | 9 | 578 | 10 | 694 | 1.50 (-5.93 to 8.94) | 0.692 | 0.01 |
| School days | |||||
| Baseline | 10 | 854 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 746 | 4.50 (0.25 to 8.75) | 0.038 | < 0.01 |
| 14 months | 9 | 578 | 10 | 694 | 0.30 (-8.49 to 9.09) | 0.947 | 0.03 |
| Weekends | |||||
| Baseline | 10 | 828 | 10 | 827 | |||
| 7 months | 8 | 561 | 10 | 702 | 8.85 (-5.52 to 23.22) | 0.227 | 0.05 |
| 14 months | 9 | 503 | 10 | 637 | 3.21 (-6.90 to 13.32) | 0.534 | 0.001 |
| During school hours | |||||
| Baseline | 10 | 855 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 746 | 5.38 (-10.01 to 20.77) | 0.493 | 0.65 |
| 14 months | 9 | 578 | 10 | 693 | 4.08 (-7.55 to 15.72) | 0.492 | 0.54 |
| After-school hours | |||||
| Baseline | 10 | 855 | 10 | 850 | |||
| 7 months | 8 | 602 | 10 | 746 | 1.70 (-1.30 to 4.69) | 0.268 | 0.01 |
| 14 months | 9 | 578 | 10 | 693 | 0.07 (-4.70 to 4.85) | 0.976 | 0.03 |
| Proportion achieving 60 mins/day of MVPA | |||||
| All days | |||||
| Baseline | 10 | 857 | 10 | 849 | |||
| 7 months | 8 | 594 | 10 | 742 | 0.78 (0.23 to 2.65) | 0.688 | < 0.001 |
| 14 months | 9 | 573 | 10 | 686 | 0.65 (0.23 to 1.85) | 0.420 | 0.01 |
CI confidence interval; ICC intra-class correlation; PA physical activity; MVPA moderate- to vigorous-intensity physical activity
aBased on a complete case analysis
bAdjusted difference at follow-up between randomised groups with 95% confidence interval, P value, and ICC for schools; adjusted for cluster effect, baseline value, participant year group, school %free school meal eligibility and stratification categories (school size and percentage of non-White pupils)
Body composition secondary outcomes
No differences between the groups were seen for BMI z-score at either seven (0.003 kg/m2; 95% C.I. -0.06 to 0.07; p = 0.908) or 14 months (0.02 kg/m2; 95% C.I. -0.06 to 0.09; p = 0.636). Similarly, no differences between the groups were seen for % body fat at either seven (-0.15%; 95% C.I.-0.83 to 0.52; p = 0.656) or 14 months (0.25%; 95% C.I. -0.68 to 1.17; p = 0.600).
Psychosocial secondary outcomes
There was no pattern in the differences found and they were sporadic (Table 6) and slight (questionnaire scales were on a five or seven point scale). At 14 months there was a difference in intentions to being active in favour of the control group (-0.21; 95% C.I. -0.37 to -0.05; p = 0.012). At seven months there was a difference in perceived importance in favour of control group (-0.42; 95% C.I. -0.66 to -0.18; p < 0.001). At 14 months there was a difference in participants confidence in being active in favour of the control group (-0.08; 95% C.I. -0.14 to -0.02; p = 0.013). A significant difference in self-esteem was seen at seven months (0.06; 95% C.I. 0.01 to 0.11; p = 0.025) in favour of the intervention group. At 14 months there was a difference between groups perceptions of their school physical environment in favour of the control group (-0.13; 95% C.I. -0.24 to -0.01; p = 0.032). At 14 (-0.09; 95% C.I. -0.18 to -0.01; p = 0.032) months there was a difference in identified motivation (motivated by engaging in activities that are a means to an end) in favour of the intervention group.
Table 6.
Scores for psychosocial measures at follow-up for participants randomised to usual practice (control) or to the Girls Active programme (intervention)
| Number of schools | pupils | Adjusted difference at follow-upa | ||||
|---|---|---|---|---|---|
| Control | Intervention | Coefficient (95% C.I.) | P value | ICC | |
| Intentions to be physically activeb | |||||
| Baseline | 10 | 871 | 10 | 842 | |||
| 7 months | 8 | 623 | 10 | 776 | -0.15 (-0.33 to 0.03) | 0.094 | < 0.001 |
| 14 months | 9 | 569 | 10 | 734 | -0.21 (-0.37 to -0.05) | 0.012 | < 0.001 |
| Perceived importance of PAc | |||||
| Baseline | 10 | 849 | 10 | 828 | |||
| 7 months | 8 | 621 | 10 | 768 | -0.42 (-0.66 to -0.18) | < 0.001 | < 0.001 |
| 14 months | 9 | 557 | 10 | 729 | -0.13 (-0.41 to 0.15) | 0.350 | < 0.001 |
| Attitudes towards being physically actived | |||||
| Positive | |||||
| Baseline | 10 | 877 | 10 | 863 | |||
| 7 months | 8 | 626 | 10 | 775 | -0.02 (-0.13 to 0.09) | 0.775 | 0.01 |
| 14 months | 9 | 573 | 10 | 737 | -0.03 (-0.07 to 0.02) | 0.250 | < 0.001 |
| Negative | |||||
| Baseline | 10 | 877 | 10 | 863 | |||
| 7 months | 8 | 627 | 10 | 775 | 0.01 (-0.05 to 0.08) | 0.661 | 0.003 |
| 14 months | 9 | 573 | 10 | 737 | 0.04 (-0.04 to 0.11) | 0.359 | 0.001 |
| Whole | |||||
| Baseline | 10 | 877 | 10 | 863 | |||
| 7 months | 8 | 627 | 10 | 775 | -0.02 (-0.10 to 0.06) | 0.667 | 0.01 |
| 14 months | 9 | 573 | 10 | 737 | -0.03 (-0.08 to 0.02) | 0.267 | < 0.001 |
| Social support for PA from familye | |||||
| Baseline | 10 | 876 | 10 | 863 | |||
| 7 months | 8 | 626 | 10 | 774 | 0.03 (-0.05 to 0.12) | 0.445 | < 0.001 |
| 14 months | 9 | 571 | 10 | 735 | -0.05 (-0.11 to 0.01) | 0.105 | < 0.001 |
| Social support for PA received from peerse | |||||
| Baseline | 10 | 874 | 10 | 863 | |||
| 7 months | 8 | 626 | 10 | 773 | -0.01 (-0.12 to 0.10) | 0.880 | 0.01 |
| 14 months | 9 | 567 | 10 | 734 | 0.01 (-0.07 to 0.09) | 0.762 | 0.01 |
| School-based social support for PA | |||||
| Physical environmente | |||||
| Baseline | 10 | 878 | 10 | 862 | |||
| 7 months | 8 | 627 | 10 | 773 | 0.03 (-0.10 to 0.15) | 0.684 | 0.03 |
| 14 months | 9 | 571 | 10 | 734 | -0.13 (-0.24 to -0.01) | 0.032 | 0.04 |
| Social environmente | |||||
| Baseline | 10 | 878 | 10 | 861 | |||
| 7 months | 8 | 626 | 10 | 773 | -0.01 (-0.10 to 0.07) | 0.758 | 0.026 |
| 14 months | 9 | 570 | 10 | 734 | -0.07 (-0.15 to 0.01) | 0.080 | 0.009 |
| PE teachersf | |||||
| Baseline | 10 | 874 | 10 | 859 | |||
| 7 months | 8 | 624 | 10 | 774 | -0.03 (-0.23 to 0.16) | 0.733 | 0.026 |
| 14 months | 9 | 567 | 10 | 731 | -0.21 (-0.45 to 0.02) | 0.074 | 0.018 |
| Confidence to take part in PA (self-efficacy)d | |||||
| Baseline | 10 | 879 | 10 | 853 | |||
| 7 months | 8 | 625 | 10 | 774 | -0.02 (-0.09 to 0.04) | 0.472 | < 0.001 |
| 14 months | 9 | 568 | 10 | 733 | -0.08 (-0.14 to -0.02) | 0.013 | < 0.001 |
| Enjoyment of PAg | |||||
| Baseline | 10 | 876 | 10 | 851 | |||
| 7 months | 8 | 625 | 10 | 772 | -0.03 (-0.14 to 0.08) | 0.592 | 0.140 |
| 14 months | 9 | 566 | 10 | 731 | -0.04 (-0.12 to 0.04) | 0.361 | < 0.001 |
| Motivation to take part in PAg | |||||
| Extrinsic | |||||
| Baseline | 10 | 877 | 10 | 842 | |||
| 7 months | 8 | 626 | 10 | 771 | -0.02 (-0.11 to 0.07) | 0.680 | < 0.001 |
| 14 months | 9 | 568 | 10 | 735 | -0.01 (-0.15 to 0.13) | 0.919 | 0.009 |
| Introjected | |||||
| Baseline | 10 | 878 | 10 | 842 | |||
| 7 months | 8 | 626 | 10 | 771 | -0.05 (-0.11 to 0.02) | 0.143 | < 0.001 |
| 14 months | 9 | 568 | 10 | 735 | -0.05 (-0.14 to 0.04) | 0.260 | < 0.001 |
| Identified | |||||
| Baseline | 10 | 878 | 10 | 842 | |||
| 7 months | 8 | 626 | 10 | 771 | -0.02 (-0.15 to 0.10) | 0.700 | 0.020 |
| 14 months | 9 | 568 | 10 | 735 | -0.09 (-0.18 to -0.01) | 0.032 | < 0.001 |
| Intrinsic | |||||
| Baseline | 10 | 878 | 10 | 842 | |||
| 7 months | 8 | 626 | 10 | 771 | -0.01 (-0.18 to 0.18) | 0.990 | 0.028 |
| 14 months | 9 | 568 | 10 | 735 | -0.06 (-0.16 to -0.04) | 0.243 | 0.002 |
| Amotivation | |||||
| Baseline | 10 | 877 | 10 | 841 | |||
| 7 months | 8 | 626 | 10 | 771 | -0.03 (-0.15 to 0.09) | 0.578 | 0.007 |
| 14 months | 9 | 568 | 10 | 735 | -0.02 (-0.14 to 0.09) | 0.684 | 0.002 |
| Physical self-perceptione | |||||
| Self-esteem | |||||
| Baseline | 10 | 760 | 10 | 700 | |||
| 7 months | 8 | 622 | 10 | 769 | 0.06 (0.01 to 0.11) | 0.025 | < 0.001 |
| 14 months | 9 | 535 | 10 | 730 | -0.06 (-0.13 to 0.01) | 0.086 | < 0.001 |
| Physical self-worth | |||||
| Baseline | 10 | 760 | 10 | 699 | |||
| 7 months | 8 | 622 | 10 | 769 | -0.01 (-0.07 to 0.05) | 0.742 | 0.007 |
| 14 months | 9 | 535 | 10 | 730 | -0.03 (-0.09 to 0.03) | 0.322 | 0.006 |
| Body attractiveness | |||||
| Baseline | 10 | 760 | 10 | 699 | |||
| 7 months | 8 | 622 | 10 | 769 | -0.05 (-0.12 to 0.03) | 0.195 | < 0.001 |
| 14 months | 9 | 535 | 10 | 730 | 0.02 (-0.05 to 0.08) | 0.630 | < 0.001 |
IQR interquartile range; CI confidence interval; ICC intra-class correlation; PA physical activity
aBased on a complete case analysis, adjusted difference at follow-up between randomised groups with 95% confidence interval, p value and ICC for schools; adjusted for cluster effect, baseline value, participant year group, school %free school meal eligibility and stratification categories (school size and percentage of non-White pupils)
bScore ranges from 1 = ‘very unlikely’ to 7 = ‘very likely’
cScale ranges from 1 = ‘very unimportant’ to 10 = ‘very important’
dScore ranges from 1 = ‘disagree a lot’ to 5 = ‘agree a lot’
eScore ranges from 1 = ‘strongly disagree’ to 5 = ‘strongly agree’
fScore ranges from 1 = ‘strongly disagree’ to’ 7 = ‘strongly agree’
gScore ranges from 1 = ‘no not at all’ to 5 = ‘yes a lot’
Sensitivity analyses
Sensitivity analyses showed similar results to the main analysis with no differences between groups at 14 months when the various levels of accelerometer data provision were used. The differences found at 7 months in the main analysis were similar when accelerometer data provision was one day or more (2.4 mins/day; 95% C.I 0.13 to 4.62; p = 0.038), any 2 days or more (2.4 mins/day; 95% C.I 0.12 to 4.72; p = 0.039), and any 3 days or more (2.4 mins/day; 95% C.I 0.02 to 4.7; p = 0.048), any 4 or more days (2.3 mins/day; 95% C.I. -0.03 to 4.7; P = 0.053) and any three weekdays plus one weekend day or more (2.2 mins/day; 95% C.I. -0.2 to 4.6; p = 0.078). The addition of baseline season of data collection to the analysis revealed a difference in MVPA change at 14 month of 0.8 mins/day (95% C.I. 1.2 to 3.5; p = 0.027) only. When follow-up season was included in the model there was a difference in MVPA change of 2.8 mins/day at seven months (95% C.I. 0.4 to 5.1; p = 0.020).
Economic analysis
Depending on how Girls Active was implemented costs ranged from an estimated £1054 per year to £3498 per year per school. There were no statistically significant differences found between the groups for health-related quality of life (CHU9D utility index scores) and frequencies and costs of GP and school service use.
Process evaluation
How each schools implemented the programme was addressed specifically within the process evaluation. In particular, how peer leaders identified and the groups established and run; the positive feelings lead teachers and pupils had about the programme; the challenges and opportunities to implementing a flexible programme within the current educational landscape and school-level constraints to implementation.
Discussion
Girls Active was designed by the YST to be, and is being delivered as, a flexible programme for UK schools. This paper investigated the effectiveness of the programme in impacting MVPA of adolescent females. PA of this population is of significant public health interest. The complete case, intention-to-treat and per protocol analyses found no evidence of a sustained intervention effect on MVPA between intervention and control groups after 14 months (primary outcome). At the shorter follow-up of seven months, significant differences in MVPA were observed between groups in the complete case, intention-to-treat and per protocol analyses, but the differences in change were small: 2.4, 2.3 and 3.1 mins/day, respectively. When observing MVPA changes in the per-protocol analysis it would seem that implementation of more of the seven core components (as presented in the methods) of Girls Active prevented the MVPA decline i.e. control schools declined by 6.2 mins/day while the intervention schools declined by 1.9 mins/day between baseline and seven months. Due to the flexible nature of the programme lead teachers spent a wide range of time and money on delivering and implementing Girls Active within their schools. The cost-consequence analysis showed no effect on health related quality of life or service use (typical measures utilised in health economic analysis).
The pre-specified subgroups analysis found that the intervention was effective at 14 months in larger schools (+ 3.9 mins/day) but caused an MVPA decrease in smaller schools (-4.4 mins/day). This warrants consideration when designing programmes for roll-out at scale. Although the relative success in larger schools makes intuitive sense, findings from the process evaluation of this study will provide information of the perceived challenges and opportunities in intervention schools. Different strategies within a programme, not necessarily different programmes, may be needed for non-White European girls and late maturing girls based on the findings of the sub-group analysis at seven months.
We saw some differences between groups at seven months for accelerometer variables in favour of the intervention group, but again these differences were relatively small. Little evidence of any changes in potential psychosocial mediators during the course of the programme were found. Process evaluation data will map out timelines of programme activity to help explain these findings.
Comparison with extant literature
School-based PA interventions targeting adolescents have shown limited success on objective measures of PA, particularly for older adolescents [33]. Recent evidence from school-based trials with a primary outcome of objectively measured MVPA from the UK [34–37], Australia [38, 39] and the Netherlands [40] has emerged. Of these, two were aimed at adolescent girls in secondary schools, [37, 39] and only one reported a significant effect on objective MVPA but in males only [38]. Other studies are currently underway in UK secondary schools which capitalise on influential pupils, mentors, or in-class peer leaders [41, 42].
The findings of this study add to evidence from well-designed, adequately powered trials on the lack of effectiveness of school-based PA programmes on objectively assessed PA [34, 37, 39]. When there is a significant effect, it is ‘small’ (a standardised mean difference ≤ 0.49) [33] highlighting the challenges with intervening on adolescents’ PA within the school setting. Although small effects are seen multi-component programmes and those underpinned by theory may be more effective [9, 13]. Extensive support may be required to show significant but modest intervention effects (e.g. PA4E1 [38]).
This was an evaluation of a programme currently implemented in UK secondary schools so addressing the limitations to the Girls Active programme itself was beyond the scope of this study. Accompanying process evaluation and cost-effectiveness papers will underscore barriers to implementing school-based PA programmes and also demonstrate what resources were actually used to implement the programme, which will be highly valuable for future research and roll-out at scale.
Strengths and limitations
The strengths of this evaluation study include a fully powered cluster RCT design. The sample was multi-ethnic, incorporating diverse schools. A random sample of 90 girls/schools were included in the evaluation to ensure it was not the “most active” girls who would sign-up. The baseline PA levels would shows that meeting PA levels are low (2.3%) the IQR of MVPA of 29.9–57.0 mins/day would suggest pupils with a wide variety of activity levels were included in this study. Overall, 25.9 to 78.2% of all KS3 girls/school (mean 37.2%) were included making our results generalisable to a whole school population in this age group. However, this may have also acted as a limitation in that over a 14 month period Girls Active is likely to only have had a modest reach, meaning our sample may have not been fully exposed to the intervention. A targeted evaluation sample may have yielded different results. Objective measurement of MVPA as the primary outcome was in line with public heath priorities and meets the need for “objective and comprehensive evaluation” methods for evaluating programmes [43]. Although flexible programme such as Girls Active may benefit from more pragmatic study designs, from a research methods standpoint the RCT design was well received by partners, schools and pupils. Overall, 24% of the schools that were contacted entered the trial (20 out of 82) and schools and pupils were recruited to target. There was good compliance with the accelerometer, low levels of missingness from questionnaires, and participant loss to follow-up was in line with other studies. A full economic analysis was also completed for the Girls Active trial. Based on best-practice, the methods used with schools were designed for this study and the methods used and results found add to the literature on the costs of delivering programmes in the school setting.
Conclusion
At 14 months, our primary measure of effectiveness was change in MVPA at 14 months. No difference in change in MVPA between Girls Active control and intervention schools was found. At seven months there was less of a decline in MVPA in the intervention schools compared to the control schools. Differences in sub-groups may mean the programme has potential in certain types of schools or pupils. Process evaluation and complete and detailed economic analysis papers will give context and detail of the delivery of such a flexible programme.
Acknowledgments
We thank all the pupils and lead teachers who took part in the Girls Active evaluation study. We thank all of the Girls Active project staff: Mrs. Kyla Harrington (project manager) and Mrs Harshada Chauhan (research administrator). We thank the individual members of the measurement teams that went into schools (comprising of staff and intern students from Leicester Diabetes Centre and the NIHR BRU and students from Loughborough University) and the Leicester CTU staff (data manager, database builder and the statistical team in particular Dr Laura Gray). We particularly thank the members of the Girls Active TSC for their advice and support over the course of the study: Angie Page (University of Bristol; chair), Esther van Sluijs (University of Cambridge), Siobhan Creanor (Plymouth University) and our public members Stephanie Dunkley (Leicester City Council) and Wayne Allsopp (New College, Leicester). Finally we thank the Youth Sport Trust for an inspiring collaboration: Chris Wright, Dominique Lammie, Paulina Skladanowska and Ali Goodall as well as YST tutors and hub school staff who brought the programme to life.
Funding
This project was funded by the NIHR Public Health Research programme (13/90/30). Professors Davies and Khunti are NIHR Senior Investigators. University of Leicester authors are supported by the NIHR Leicester-Loughborough Biomedical Research Unit (2012–2017), the NIHR Leicester Biomedical Research Centre (2017–2022) and the Collaboration for Leadership in Applied Health Research and Care (CLAHRC) East Midlands. This study was undertaken in collaboration with the Leicester Clinical Trials Unit a UKCRC-registered clinical trials unit in receipt of NIHR CTU support funding. The Youth Sport Trust or the aforementioned funders had no involvement in the TSC, the data analysis, data interpretation, data collection, or writing of this manuscript.
Availability of data and materials
Owing to the use of opt out consent, and not including any specific data sharing information in the participant and parent/guardians information sheets, there are no data that can be shared publically. Please contact the corresponding author for further details. Document relating to this study can be found on www.leicesterdiabetescentre.org.uk/girls-active-evaluation
Abbreviations
- APHV
Age at peak height velocity
- BME
Black and minority ethnicity
- BMI
Body mass index
- CI
Confidence interval
- FSME
Free school meal eligibility
- ICC
Intra-class correlation
- IMD
Index of multiple deprivation
- ITT
Intention to treat
- KS3
Key Stage three
- LLR
Leicester City, Leicestershire and Rutland
- MVPA
Moderate- to vigorous-intensity physical activity
- PA
Physical activity
- PE
Physical education
- RCT
Randomised controlled trial
- SD
Standard deviation
- SES
Socioeconomic status
- UK
United Kingdom
- YST
Youth Sport Trust
Authors’ contributions
DMH co-led the study, co-led the study design and methods development, conducted fieldwork, co-wrote the first draft of the manuscript, coordinated responses from all authors and obtained funds to complete the project. MJD had overall responsibility for the study as the primary investigator, led the study design development and obtained funds to complete the project. DB led the study design development, designed the statistical analysis plan, undertook subsequent rounds of statistical analysis and obtained funds to complete the project. JC conducted the economic analysis of the wider study and drafted the related sections of the manuscript. YC wrote the statistical analysis plan, cleaned and managed the data, undertook the first round of statistical analysis. TG contributed to methods development, drafted the related sections of the manuscript and obtained funds to complete the project. KK contributed to methods development and obtained funds to complete the project. TP conducted and led the fieldwork team and managed and analysed the accelerometer data. AR cleaned, managed and analysed the accelerometer data and drafted the related sections of the manuscript. LS contributed to methods development, conducted fieldwork, and obtained funds to complete the project. RTE designed and oversaw the economic analysis of the wider study and obtained funds to complete the project. TY contributed to study design and methods development and obtained funds to complete the project. CLE co-led the study, co-led the study design and methods development, conducted fieldwork, co-wrote the first draft of the manuscript, and obtained funds to complete the project. All authors made critical revisions to the manuscript a number of times. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethics approval was obtained from the College of Medicine, Biological Sciences and Psychology ethics representative at the University of Leicester. School principals provided written consent for their school to participate. Parents/guardians were provided with an opt out consent form and only pupils who did not return the opt out consent form participated. Participants provided verbal assent prior to each measurement session and could withdraw at any time.
Consent for publication
Not applicable.
Competing interests
All authors have completed the Unified Competing Interest form (available on request from the corresponding author) and declare: no support from any organisation for the submitted work, no financial relationships with any organisations that might have an interest in the submitted work in the previous three years and no competing interest related to this work. MJD and KK reports personal fees from Novo Nordisk, Sanofi-Aventis, Lilly, Merck Sharp & Dohme, Boehringer Ingelheim, AstraZeneca, Janssen, Servier, Mitsubishi Tanabe Pharma Corporation, Takeda Pharmaceuticals International Inc. and grants from Novo Nordisk, Sanofi-Aventis, Lilly, Boehringer Ingelheim, and Janssen. Outside of the submitted work, JC reports grants from Public Health Wales. CE reports grants from National Institute for Health Research Public Health Research during the conduct of the study. YC, TP, RTE, DB, TG, DMH, AR, LS and TY all have nothing to declare.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Deirdre M. Harrington, Phone: +44 116 258 8630, Email: dh204@le.ac.uk
Melanie J. Davies, Email: melanie.davies@uhl-tr.nhs.uk
Danielle H. Bodicoat, Email: dhm6@le.ac.uk
Joanna M. Charles, Email: j.charles@bangor.ac.uk
Yogini V. Chudasama, Email: yc244@le.ac.uk
Trish Gorely, Email: trish.gorely@uhi.ac.uk.
Kamlesh Khunti, Email: kk22@le.ac.uk.
Tatiana Plekhanova, Email: tp150@le.ac.uk.
Alex V. Rowlands, Email: alex.rowlands@le.ac.uk
Lauren B. Sherar, Email: L.B.Sherar@lboro.ac.uk
Rhiannon Tudor Edwards, Email: r.t.edwards@bangor.ac.uk.
Thomas Yates, Email: ty20@le.ac.uk.
Charlotte L. Edwardson, Email: ce95@le.ac.uk
References
- 1.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 2.Public Health England. Health Survey for England 2015, Trend Tables. Health and social care information Centre. Available from http://www.content.digital.nhs.uk/catalogue/PUB22610. Accessed 2 Jan 2018.
- 3.Janssen I, LeBlanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Activ. 2010;7:1–16. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farooq MA, Parkinson KN, Adamson AJ, Pearce MS, Reilly JK, Hughes AR, et al. Timing of the decline in physical activity in childhood and adolescence: Gateshead millennium cohort study. Br J Sports Med; 2017. Online first. 10.1136/bjsports-2016-096933. [DOI] [PMC free article] [PubMed]
- 5.UK Active Kids. Generation Active. Available from http://www.ukactive.com/downloads/managed/ON02629_UK_Active_Kids_report_online_spreads_FP.PDF. Accessed 2 Jan 2018.
- 6.Sport England. Sport England: Towards an Active Nation Strategy 2016–2021. London:Sport England. Available from https://www.sportengland.org/media/10629/sport-england-towards-an-active-nation.pdf. Accessed 2 Jan 2018.
- 7.Association for Physical Education. Health Position Paper. Available from http://www.afpe.org.uk/physical-education/wp-content/uploads/afPE_Health_Position_Paper_Web_Version2015.pdf. Accessed 2 Jan 2018.
- 8.Camacho-Miñano MJ, LaVoi NM, Barr-Anderson DJ. Interventions to promote physical activity among young and adolescent girls: a systematic review. Health Educ Res. 2011;26:1025–1049. doi: 10.1093/her/cyr040. [DOI] [PubMed] [Google Scholar]
- 9.van Sluijs EMF, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. Brit Med J. 2007;335:703. doi: 10.1136/bmj.39320.843947.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Libr. 2013;2:CD007651. doi: 10.1002/14651858.CD007651.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hynynen S, van Stralen M, Sniehotta F, Araújo-Soares V, Hardeman W, Chinapaw M, et al. A systematic review of school-based interventions targeting physical activity and sedentary behaviour among older adolescents. Int Rev Sport Exerc Psycho. 2016;9:22–44. doi: 10.1080/1750984X.2015.1081706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pearson N, Braithwaite R, Biddle SJ. The effectiveness of interventions to increase physical activity among adolescent girls: a meta-analysis. Acad Pediatr. 2015;15:9–18. doi: 10.1016/j.acap.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 13.Owen MB, Curry WB, Kerner C, Newson L, Fairclough SJ. The effectiveness of school-based physical activity interventions for adolescent girls: a systematic review and meta-analysis. Prev Med. 2017;105:237–249. doi: 10.1016/j.ypmed.2017.09.018. [DOI] [PubMed] [Google Scholar]
- 14.Lubans DR, Foster C, Biddle SJ. A review of mediators of behavior in interventions to promote physical activity among children and adolescents. Prev Med. 2008;47:463–470. doi: 10.1016/j.ypmed.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Public Health England. Identifying what works for local physical inactivity interventions. Waterloo Road, London: Public Health England. Available from http://researchinstitute.ukactive.com/downloads/managed/Identifying_what_works.pdf. Accessed 2 Jan 2018.
- 16.Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A, et al. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. J Am Med Assoc. 2012;307:704–712. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jago R, Sebire SJ, Cooper AR, Haase AM, Powell J, Davis L, et al. Bristol girls dance project feasibility trial: outcome and process evaluation results. Int J Behav Nutr Phys Activ. 2012;9:1–10. doi: 10.1186/1479-5868-9-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edwardson CL, Harrington DM, Yates T, Bodicoat DH, Khunti K, Gorely T, et al. A cluster randomised controlled trial to investigate the effectiveness and cost effectiveness of the ‘girls active’ intervention: a study protocol. BMC Public Health. 2015;15:526. doi: 10.1186/s12889-015-1886-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Hees VT, Fang Z, Langford J, Assah F, Mohammad A, da Silva IC, et al. Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: an evaluation on four continents. J Appl Physiol. 2014;117:738–744. doi: 10.1152/japplphysiol.00421.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Hees VT, Gorzelniak L, Leon ECD, Eder M, Pias M, Taherian S, et al. Separating movement and gravity components in an acceleration signal and implications for the assessment of human daily physical activity. PLoS One. 2013;8:e61691. doi: 10.1371/journal.pone.0061691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hildebrand M, Van Hees VT, Hansen BH, Ekelund U. Age group comparability of raw accelerometer output from wrist-and hip-worn monitors. Med Sci Sports Exerc. 2014;46:1816–1824. doi: 10.1249/MSS.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 22.Hildebrand M, Hansen BH, van Hees VT, Ekelund U. Evaluation of raw acceleration sedentary thresholds in children and adults. Scand J Med Sci Spor. 2017;27:1814–23. [DOI] [PubMed]
- 23.van Hees VT, Sabia S, Anderson KN, Denton SJ, Oliver J, Catt M, et al. A novel, open access method to assess sleep duration using a wrist-worn accelerometer. PLoS One. 2015;10:e0142533. doi: 10.1371/journal.pone.0142533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.UK Chief Medical Officers. Start Active, Stay Active: A report on physical activity for health from the four home countries’ Chief Medical Officers. Department of Health. Available from www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_128209. Accessed.
- 25.da Silva IC, van Hees VT, Ramires VV, Knuth AG, Bielemann RM, Ekelund U, et al. Physical activity levels in three Brazilian birth cohorts as assessed with raw triaxial wrist accelerometry. Int J Behav Nutr Phys Activ. 2014;43:1959–1968. doi: 10.1093/ije/dyu203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Childhood. 1995;73:25–29. doi: 10.1136/adc.73.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Malina RM, Bouchard C, Bar-Or O. Growth, maturation and physical activity. Champaign: Human Kinetics; 2004. [Google Scholar]
- 28.UK Government. Schools, pupils and their characteristics: January 2015. London:UK National Statistics. Available from https://www.gov.uk/government/statistics/schools-pupils-and-their-characteristics-january-2015. Accessed 2 Jan 2018.
- 29.Harrington DM, Davies MJ, Bodicoat D, Charles JM, Chudasama YV, Gorely T, et al. Girls Active: a cluster randomised controlled trial, cost-effectiveness analysis and process evaluation of a school-based intervention to increase physical activity levels among 11- to 14- year-old girls. London:National Institute for Health Research. Available from. Accessed.
- 30.Charles JM, Edwards RT, Bywater T, Hutchings J. Micro-costing in public health economics: steps towards a standardized framework, using the incredible years toddler parenting program as a worked example. Prev Sci. 2013;14:377–389. doi: 10.1007/s11121-012-0302-5. [DOI] [PubMed] [Google Scholar]
- 31.Stevens KJ. Assessing the performance of a new generic measure of health related quality of life for children and refining it for use in health state valuation. Am J Pub Health. 2011;9:157–169. doi: 10.2165/11587350-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 32.Campbell MK, Piaggio G, Elbourne DR, Altman DG, for the CONSORT Group Consort 2010 statement: extension to cluster randomised trials. Brit Med J. 2012;345:e5661. doi: 10.1136/bmj.e5661. [DOI] [PubMed] [Google Scholar]
- 33.Borde R, Smith J, Sutherland R, Nathan N, Lubans D. Methodological considerations and impact of school-based interventions on objectively measured physical activity in adolescents: a systematic review and meta-analysis. Obes Rev. 2017;18:476–490. doi: 10.1111/obr.12517. [DOI] [PubMed] [Google Scholar]
- 34.Tymms PB, Curtis SE, Routen AC, Thomson KH, Bolden DS, Bock S, et al. Clustered randomised controlled trial of two education interventions designed to increase physical activity and well-being of secondary school students: the MOVE project. Brit Med J Open. 2016;6:e009318. doi: 10.1136/bmjopen-2015-009318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fairclough SJ, McGrane B, Sanders G, Taylor S, Owen M, Curry W. A non-equivalent group pilot trial of a school-based physical activity and fitness intervention for 10–11 year old english children: born to move. BMC Public Health. 2016;16:861. doi: 10.1186/s12889-016-3550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: active for life year 5 (AFLY5) school based cluster randomised controlled trial. Brit Med J. 2014;348:g3256. doi: 10.1136/bmj.g3256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jago R, Edwards MJ, Sebire SJ, Tomkinson K, Bird EL, Banfield K, et al. Effect and cost of an after-school dance programme on the physical activity of 11–12 year old girls: the Bristol girls dance project, a school-based cluster randomised controlled trial. Int J Behav Nutr Phys Activ. 2015;12:128. doi: 10.1186/s12966-015-0289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sutherland R, Campbell E, Lubans DR, Morgan PJ, Okely AD, Nathan N, et al. ‘Physical activity 4 Everyone’school-based intervention to prevent decline in adolescent physical activity levels: 12 month (mid-intervention) report on a cluster randomised trial. Brit J Sport Med. 2016;50:488–495. doi: 10.1136/bjsports-2014-094523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Okely AD, Lubans DR, Morgan PJ, Cotton W, Peralta L, Miller J, et al. Promoting physical activity among adolescent girls: the girls in sport group randomized trial. Int J Behav Nutr Phys Activ. 2017;14:81. doi: 10.1186/s12966-017-0535-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Kann D, Kremers S, de Vries N, de Vries S, Jansen M. The effect of a school-centered multicomponent intervention on daily physical activity and sedentary behavior in primary school children: the active living study. Prev Med. 2016;89:64–69. doi: 10.1016/j.ypmed.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 41.Sebire SJ, Edwards MJ, Campbell R, Jago R, Kipping R, Banfield K, et al. Update to a protocol for a feasibility cluster randomised controlled trial of a peer-led school-based intervention to increase the physical activity of adolescent girls (PLAN-A) Pilot Feasibility. 2016;2:68. doi: 10.1186/s40814-016-0110-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brown HE, Whittle F, Jong ST, Croxson C, Sharp SJ, Wilkinson P, Wilson EC, van Sluijs EM, Vignoles A, Corder K. A cluster randomised controlled trial to evaluate the effectiveness and cost-effectiveness of the GoActive intervention to increase physical activity among adolescents aged 13–14 years. BMJ Open. 2017:7:e014419. [DOI] [PMC free article] [PubMed]
- 43.All-Party Commission on Physical Activity. Tackling physical inactivity – a coordinated approach. London: All-Party Commission on Physical Activity. Available from https://parliamentarycommissiononphysicalactivity.files.wordpress.com/2014/04/apcopa-final.pdf. Accessed 2 Jan 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Owing to the use of opt out consent, and not including any specific data sharing information in the participant and parent/guardians information sheets, there are no data that can be shared publically. Please contact the corresponding author for further details. Document relating to this study can be found on www.leicesterdiabetescentre.org.uk/girls-active-evaluation


