Abstract
Rationale
Pulmonary artery enlargement (PAE) is associated with exacerbations in Chronic Obstructive Pulmonary Disease (COPD) and with survival in moderate to severe patients. The potential role of PAE in survival prediction has not been compared with other clinical and physiological prognostic markers.
Methods
In 188 patients with COPD, PA diameter was measured on a chest CT and the following clinical and physiological parameters registered: age, gender, smoking status, pack-years history, dyspnea, lung function, exercise capacity, Body Mass Index, BODE index and history of exacerbations in year prior to enrolment. Proportional Cox regression analysis determined the best predictor of all cause survival.
Results
During 83 months (±42), 43 patients died. Age, pack-years history, smoking status, BMI, FEV1%, six minute walking distance, Modified Medical Research Council dyspnea scale, BODE index, exacerbation rate prior to enrollment, PA diameter and PAE (diameter≥30mm) were associated with survival. In the multivariable analysis, age (HR: 1.08; 95%CI: 1.03–1.12, p<0.001) and PAE (HR: 2.78; 95%CI: 1.35–5.75, p = 0.006) were the most powerful parameters associated with all-cause mortality.
Conclusions
In this prospective observational study of COPD patients with mild to moderate airflow limitation, PAE was the best predictor of long-term survival along with age.
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a highly prevalent disease and one of the leading causes of death worldwide [1]. Several noninvasive tools have been described to evaluate COPD survival: 1. Physiological, including degree of airway obstruction [2] or lung hyperinflation [3] (Inspiratory to Total Lung Capacity ratio: IC/TLC); 2. Clinical, such as degree of dyspnea measured by the modified Medical Research Council (MMRC) scale [4], exercise capacity evaluated by the six minute walking distance (6MWD) [5], nutritional status measure by body mass index (BMI) or free fat mass index (FFMI) [6], and presence of exacerbations [7]; 3. Composite indexes, such as the BODE index [8] (Body mass index, Obstruction, Dyspnea and Exercise capacity) or the ADO index [9] (Age, Dyspnea and Obstruction) or 4. Radiological, such as the presence of emphysema [10], bronchiectasis [11] or Pulmonary Artery Enlargement (PAE) [12].
Pulmonary hypertension (PH) is a progressive, life threating condition defined by the presence of a mean pulmonary artery pressure ≥25 mm Hg [13]. It is usually associated to severe degree of airway obstruction with a prevalence of 25–35% in this group of patients, but it has also been described as frequent as 5–7% in patients with mild to moderate disease [14]. The gold standard for its diagnosis is the invasive measurement of the mean Pulmonary Artery Pressure (mPAP) by right heart catheterization [13]. Several noninvasive tools have been described for the screening for PH, including Transthoracic Doppler Ultrasound measurement of the systolic PAP from the peak tricuspid regurgitation jet or the detection of an enlarged PA in a chest CT defined by a main PA diameter >30mm or a main PA to ascending Aorta ratio>1 [15].
An enlarged PA, usually evaluated with an PA/Aorta ratio>1, has been associated with the number of exacerbations [16], exercise capacity (6MWD distance) [17] and just recently, with all-cause mortality but only in patients with moderate to severe disease [12].
The potential role of an enlarged PA (evaluated by a diameter≥30mm) as a prognostic marker of all degrees of airway limitation (AL) severity in COPD patients has not been compared with other well-consolidated prognostic markers of the disease.
We therefore prospectively recruited COPD patients that attend our pulmonary clinic in order to compare the prognostic value of an enlarged PA (diameter >30mm) detected in a chest CT against other well-established prognostic markers of COPD survival.
Methodology
This a prospective observational study of a COPD cohort attending a Pulmonary Clinic (ClinicalTrials.gov Identifier: NCT01122758).
Participants were ever smokers of at least 10 pack-years with previous spirometric diagnosis of COPD (post-bronchodilator FEV1/FVC ratio of less than 0.7 after the inhalation of 400μg of Salbutamol). All patients had to be clinically stable (no exacerbations) for 8 weeks and receiving optimal therapy [2]. Exclusion criteria were uncontrolled co-morbidities such as malignancy or other confounding diseases: severe congestive heart failure, obliterative bronchiolitis, or diffuse panbronchiolitis. Our Institution`s ethics committee (Clínica Universidad de Navarra) approved the study (IRB approval n° 28/2012) and all patients signed the informed consent form.
Clinical variables
At recruitment, trained personnel obtained sociodemographic information and smoking history, including age, gender, current smoking status, and intensity of exposure. Using these data, we calculated the total smoking exposure, in pack-years, of each participant.
Lung function and DLCO were measured according to the ATS/ERS guidelines [18]. The 6-min walking distance (6MWD) was performed according to ATS guidelines [19]. Patients`dyspnea was evaluated with the Modified Medical Research Council (MMRC) scale [20]. Body Mass Index (BMI) was calculated in kg/m2. FEV1% of predicted values, BMI, 6MWD and MMRC values were integrated into the BODE index [8] as previously described and also classified in quartiles. Degree of AL was classified according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria [2] into four groups: stage 1 (mild, post-bronchodilator FEV1≥80% predicted), stage 2 (moderate, post-bronchodilator FEV1 ≥50% to <80% predicted), stage 3 (severe, post-bronchodilator FEV1 <50% to ≥30% predicted), and stage 4 (very severe, post-bronchodilator FEV1 <30% predicted).
Exacerbations were defined by worsening of respiratory symptoms beyond normal daily variations that required the use of antibiotics, steroids or both, medical consultation or admission to hospital [2].
Survival was determined by direct follow-up with participants and/or their family.
CT image acquisition and reconstruction protocol
All individuals were imaged on a multidetector CT system (Somatom Definition and Somatom Sensation 64, Siemens Healthcare, Forchheim, Germany) at time zero of the follow up time. Most individuals (n = 143) underwent low dose chest CT (LDCT) examination with the following parameters: 120 kV, 40 mAs, 32×0.6 mm detector collimation, pitch 1. Images were reconstructed with 5 mm and 1 mm slice thickness using soft tissue (B31f) and high-resolution (B60f) reconstruction algorithms to evaluate the mediastinum and lung parenchyma, respectively. Intravenous contrast was administrated in 46 patients.
Assessment of rmphysema on CT
All images were read by two chest radiologists (A.E. and G.B.) for visual assessment of the presence of emphysema, using validated criteria [21]. In brief, the extent of emphysema was graded from 0 to 4, with a grade of 0 indicating no emphysema, and a grade of 4 indicating the presence of emphysema in 75% of the lung.
Measurement of pulmonary diameter
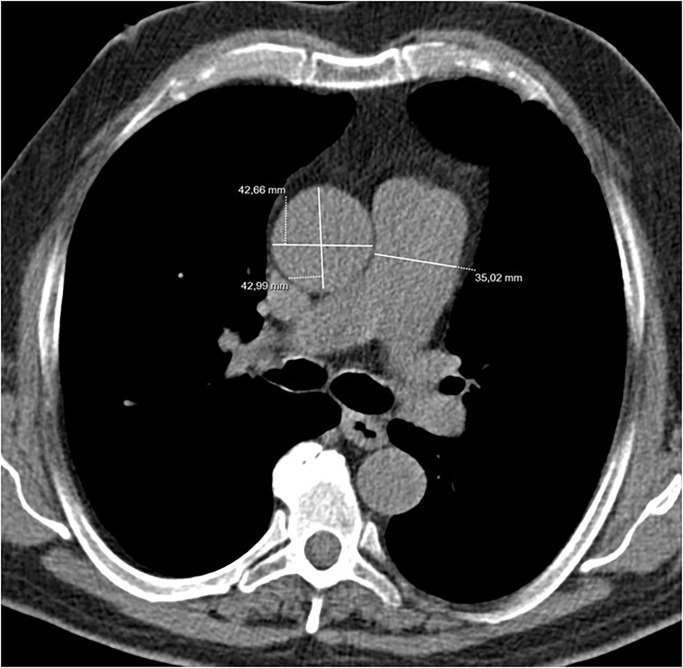
Two thoracic radiologists blinded to patients’ clinical data measured the main pulmonary artery (PA) diameter at the level of its bifurcation on transverse CT images (Fig 1)
Fig 1. LDCT examination.
Measurements of main Pulmonary Artery (PA) diameter and Ascending Aorta (AA) at the level of the bifurcation. The greatest diameter of the AA was used to calculate the PA/Aorta ratio.
The greatest diameter of the ascending aorta (AA) was also measured at the same level. A cut off value of ≥30 mm was employed for distinguishing between patients with and without pulmonary hypertension. The ratio of the main PA diameter to the diameter of ascending aorta (PA/Aorta ratio) was also determined and a ratio >1 was considered an indirect marker of pulmonary hypertension, as previously described in COPD patients [22].
Statistical analysis
Data was summarized as relative frequencies for categorical variables, mean (SD) for normally distributed variables. Pearson´s coefficient was calculated to explore the association between PA diameter and the prognostic variables.
A proportional Cox survival analysis first determined the independent association of each study parameter with all cause survival. Then, a multivariable analysis including all that had a statistical significant association in the univariable analysis determined the best predictor of all cause survival. Because some of the factors that were found to be independently associated with survival in the univariable analysis are part of the BODE index (BMI, FEV1%, MMRC and 6MWD), we only included this score representing all of them in the multivariable analysis, as this index showed to have the strongest prognostic power in previous studies. Significance level was established as a two-tailed p-Value ≤0.05. We used SPSS 22.0, Chicago, U.S.A. for the statistical analysis.
Results
From an initial sample of 215 patients, we were able to obtain appropriate radiological information in 188 individuals: 23 had different acquisition technique and in 4, PA measurement were not able to be performed (Fig 2).
Fig 2. Flowchart showing the inclusion of patients for the final statistical analysis.
Table 1 shows the clinical, physiological and radiological characteristics of the participants.
Table 1. Clinical, radiological and physiological characteristics of the patients.
| Patients characteristics | |
|---|---|
| n | 188 |
| Age (years) | 65 ± 8 |
| Follow up (months) | 83 ± 42 |
| Gender (%) male/female | 82/18 |
| Pack-year (units) | 51 ± 27 |
| Current Smoker (%) yes/no | 35/65 |
| FEV1/FVC (%) | 55 ± 10 |
| FEV1% | 70 ± 20 |
| FVC % | 98 ± 20 |
| TLC % | 102 ± 15 |
| DLCO | 70 ± 20 |
| MMRC 0-1-2-3-4 (%) | 36-41-1-8-2 |
| 6MWD (m) | 468 ± 112 |
| BMI (Kg/m2) | 26 ± 4 |
| BODE Quart 1–4 (%) | 80/10/8/2 |
| BODE | 1.3 ± 1.8 |
| Spirometric GOLD stages I-II-III-IV % | 36, 48, 14, 2 |
| Exacerbations in the year prior to enrollment n | 0.7 ± 0.9 |
| Pulmonary Artery diameter mm | 24.7 ± 4.1 |
| Pulmonary Artery diameter≥30mm n, % | 22, 12% |
| Pulmonary Artery diameter≥30mm by GOLD I+II / III+IV % | 10/23 |
| Pulmonary Artery/Aorta Artery ratio | 0.69 ± 0.11 |
| Pulmonary Artery/Aorta Artery ratio >1 n, % | 3, 0.01% |
| Pulmonary Artery/Aorta Artery ratio quartiles % | 29-21-30-20 |
| Emphysema severity (visual) 0-1-2-3% | 46-24-20-10 |
| Deaths n, % | 43, 23% |
| Deaths by GOLD I+II / III+IV % | 22/30 |
n = Number of participants; BMI = Body Mass Index; FEV1 = Forced Expiratory Volume in the first second; FVC = Forced Vital Capacity; TLC = Total Lung Capacity; MMRC = Modified Medical research Council; 6MWD = 6 Minute Walk Distance; BODE index: BMI, Obstruction, Dyspnea, Exercise capacity, X ± SD = means ± Standard Deviation
They were mainly men with mild to moderate COPD, followed for a mean time of almost 7 years. Most of them were just mildly symptomatic, slightly overweight with a good exercise capacity at the time of enrollment. They had a low BODE score and less than one exacerbation in the year prior to enrollment. Twenty two (12%) patients had a PA diameter ≥30mm and only 3 patients presented a PA/Aorta ratio>1. Fifty four percent of them had emphysema, 30% of them showing more than 50% of emphysema in their LDCT.
During the follow up time, 43 deaths occurred. As expected, patients with a greater degree of airway obstruction (22% vs. 30%) had higher mortality.
Table 2 shows the clinical, physiological and radiological characteristics of those patients with PAE (n = 22).
Table 2. Clinical, radiological and physiological characteristics of the patients diagnosed with and without PAE.
| Patients characteristics | ||
|---|---|---|
| With PAE | Without PAE | |
| n | 22 | 166 |
| Age (years) | 69 ± 6 | 64±8* |
| Follow up (months) | 62 ± 38 | 88±42* |
| Gender (%) male/female | 77/23 | 83/17* |
| Body Surface Area | 1.88±0.23 | 1.87±0.22 |
| Pack-year (units) | 65 ± 32 | 49±26 |
| Current Smoker (%) yes/no | 27/73 | 35/65* |
| FEV1/FVC (%) | 53 ± 12 | 56±10 |
| FEV1% | 55 ± 20 | 73±19* |
| FVC % | 80 ± 18 | 101±19* |
| TLC % | 88 ± 21 | 105±13 |
| DLCO | 62 ± 22 | 71±20* |
| MMRC 0-1-2-3-4 (%) | 14-50-14-18-4 | 42-37-12-5-4 |
| 6MWD (m) | 374 ± 129 | 482±103* |
| BMI (Kg/m2) | 28 ± 5 | 26±5 |
| BODE | 2.2 ± 2.3 | 1.1±1.7 |
| Spirometric GOLD stages I-II-III-IV % | 9, 59, 23, 9 | 40-46-12-2* |
| Exacerbations in the year prior to enrollment n | 1.2 ± 1.2 | 0.6±0.8* |
| Pulmonary Artery diameter mm | 32.9 ± 3.5 | 23.7±2.8* |
| Emphysema severity (visual) 0-1-2-3% | 64-18-14-4 | 44-25-21-10 |
| Deaths n, % | 12, 55% | 31, 18%* |
n = Number of participants; BMI = Body Mass Index; FEV1 = Forced Expiratory Volume in the first second; FVC = Forced Vital Capacity; TLC = Total Lung Capacity; MMRC = Modified Medical research Council; 6MWD = 6 Minute Walk Distance; BODE index: BMI, Obstruction, Dyspnea, Exercise capacity, X ± SD = means ± Standard Deviation
* statistically significant
Those with PAE were older, had higher consumption of tobacco, more likely to be women, had a higher BMI, more severe GOLD stage and BODE index, with a lesser burden of emphysema, a lower 6MWD and a higher degree of dyspnea.
Table 3 shows the association of the explored variables with PA diameter.
Table 3. Association between pulmonary artery diameter and other studied variables.
| Variables | Pearson coefficient | p value |
|---|---|---|
| Age | 0.28 | 0.001 |
| Pack-year | 0.18 | 0.013 |
| BMI | 0.28 | 0.001 |
| Exacerbations in the year prior to enrollment | 0.16 | 0.027 |
| FEV1% | -0.24 | 0.001 |
| DLCO | -0.12 | 0.13 |
| MMRC | 0.18 | 0.01 |
| 6MWD | -0.39 | 0.001 |
| BODE | 0.20 | 0.006 |
| Emphysema severity (visual) | -0.13 | 0.08 |
As previously described in the literature, an enlarged PA diameter was associated with 6MWD, BMI, MMRC, FEV1%, BODE and the number of exacerbations reported the year prior to enrollment. We did not find an association of this variable with pulmonary emphysema severity nor with DLCO values.
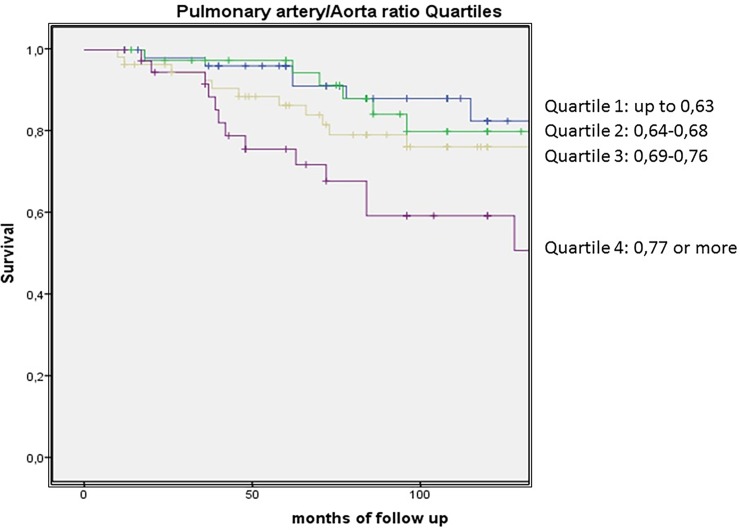
To select the best PA parameter that predicted survival in our cohort of patients, we firstly explored the association between PA enlargement (PAE) (previously defined as a diameter ≥30mm) and PA/Aorta ratio quartiles. Results showed a Polychoric correlation [23] of rho = 0.76; bootstrap bias corrected 95%CI: (0.58; 0.88). Then we explored with a Cox proportional analysis the independent association with survival, showing that both the PA/Aorta ratio quartiles and PAE were associated with survival (HR: 3.73; 95%CI: 1.43–9.74, p<0.001, p for trend 0.05 and HR: 4.52; 95%CI: 2.28–8.98, p<0.001). Comparing the highest PA/Aorta quartile vs the other PA/Aorta quartiles, the HR was 2.22; 95%CI: 1.16–4.24, p = 0.016. When we compared the predicted power of both measurements in a multivariable analysis, PAE was a stronger predictor of survival with a HR: 4.52; 95%CI: 2.28–8.98, p<0.001 than PA/Aorta ratio quartiles HR: 2.20; 95%CI 0.77–6.27, p = 0.13. Therefore, we used PAE as a predictor of survival in the final model.
Table 4 Panel A. shows the results of Cox proportional risk analysis exploring the association between the evaluated parameters and all-cause mortality.
Table 4. Panel A. Univariable analysis showing the independent association of each parameter with survival.
Panel B. Multivariable analysis showing those that remained in the model.
| Panel A. Univariable analysis exploring factors that predict survival | ||
| Variables | HR (95% IC) | p value |
| Age (for each year) | 1.09 (1.05–1.13) | 0.001 |
| Pack-year (for each pack-year) | 1.00 (1.01–1.02) | 0.06 |
| BMI (index) | 1.00 (0,94–1,07) | 0.80 |
| Gender (male as reference) | 0.45 (0.18–1.16) | 0.10 |
| Current Smoker (yes vs. no) | 2.12 (1.02–4.39) | 0.04 |
| FEV1% (for each %) | 0.97 (0.96–0.99) | 0.001 |
| MMRC (for each point) | 1.36 (1.07–1.70) | 0.01 |
| 6MWD (for each m) | 0.99 (0.98–0.99) | 0.001 |
| BODE (for each point) | 1.19 (1.04–1.35) | 0.007 |
| Pulmonary Artery diameter (for each mm) | 1.19 (1.12–1.27) | 0.001 |
| Pulmonary Artery diameter≥30mm (yes vs. no) | 4.52 (2.28–8.98) | 0.001 |
| Pulmonary artery quartiles (reference Q1) | ||
| Q2 vs Q1 | 0.94 (0.32–2.71) | 0.90 |
| Q3 vs Q1 | 1.26 (0.62–4.22) | 0.32 |
| Q4 vs Q1 | 5.36 (2.33–12.32) | 0.001 |
| Emphysema (yes vs no) | 0.88 (0.48–1.63) | 0.69 |
| Panel B. Multivariable analysis | ||
| Variables | HR (95%IC) | p value |
| Age (for each year) | 1.08 (1.04–1.13) | 0.001 |
| Pulmonary Artery diameter≥30mm (yes vs no) | 2.78 (1.35–5.75) | 0.006 |
Variables included in the model: age, BSA, current smoker, BODE, Pulmonary Artery diameter>30mm
We first confirmed that well recognized survival predictors in COPD patients were also predictors of survival in our population: age, smoking status, MMRC, FEV1%, 6MWD and BODE index. PA diameter as a continuous variable and as a categorical variable using the cut-off associated with PH (≥30mm), was independently associated with all cause survival. Factors usually associated with survival in COPD patients such as BMI and emphysema presence were not associated with survival in our population.
Table 4 Panel B. shows the results of the multivariable Cox regression analysis for those variables statistically significant in the univariable analysis. Being older and with a PA diameter ≥30mm were the most powerful predictors of survival in our cohort, stronger than the BODE index which did not retained in the final model.
Fig 3 shows the Kaplan Meier curves with the cumulative survival for those with and without PAE and for Pulmonary Artery diameter Quartiles.
Fig 3. Kaplan Meier curves showing the cumulative survival for those with and without PAE and for pulmonary artery diameter quartiles.
Discussion
The most important and novel finding from this mainly male COPD cohort, is that having a main PA diameter ≥30mm as measured on chest CT is a powerful and independent predictor of survival, providing greater prognostic information than well-established predictors of survival such as the BODE index.
The Framingham Heart Study provided the largest population based cohort (n = 706) to define normal values for main PA size measurement in non-contrast chest CT [24]. In this “healthy” population based cohort (nonsmokers without hypertension, obesity, COPD, thromboembolic disease, diabetes mellitus, cardiovascular disease or heart surgery) the mean value for main PA was 25.1±2.8mm with a 90th percentile for men at 28.9mm and for women at 26.9mm. A recent meta-analysis of 12 studies [25] including different types of patients, established a cut-off value of 29.5mm has a sensitivity of 87% and specificity of 89% for PH and therefore is usually recommended for PH screening acknowledging that even a normal diameter cannot exclude the presence of PH. The ratio between main PA to ascending Aorta diameters has also been postulated as an indirect measurement for the presence of PH. The same Framingham Heart Study also provided the normal values for this ratio in a population based cohort: 0.77±0.09mm with a 90th percentile cut off value at 0.91mm. The literature suggests that this ratio is a better predictor of PA pressure [24].
The main goal of the present work was to compare the prognostic power of PAE evaluation with existing clinical and physiological tools for survival and not to diagnose PH in COPD patients. Patients´ mean PA diameter was 24.7mm, falling within what is considered normal for a mainly male population, but 22 patients (12%) with a main PA diameter ≥30mm. Only 7 patients (3.7%) have what is considered an abnormal PA/Aorta ratio (>0.91). In our patients, PAE (≥30mm) correlated well with the PA/Aorta, but was a better predictor of survival than PA/Aorta ratio quartiles. Having a main PA diameter≥30mm and an older age were the best predictors of all of the tested variables. Terzikhan et al.[17] from the population based Rotterdam Study has recently provided information regarding the relationship between PAE and all-cause mortality in COPD patients. They studied a large sample of individuals from the general population (n = 2197) and as expected, 10% of them (222 patients) had pre-bronchodilator AL or COPD. They found that PA/Aorta ratio quartiles (largest vs shortest) were predictive of all-cause mortality but only in those with moderate to severe AO. There are several differences between that study and the present one. Firstly, Terzikhan´s is a population based study, where the diagnosis was made with pre bronchodilator spirometry where up to 30% of these patients may not have COPD in post bronchodilation according with previous data [26], while this study was conducted in a well characterized population with clinical COPD. Secondly and most important, Terzikhan et al. did not compare the predictive power of PAE with other well established prognostic tools of the disease. A PA diameter≥30mm was a stronger predictor of survival even than the multimensional BODE index, that has been consistently shown to be the best predictor of all-cause mortality in COPD patients [27]. This implies that independently of the degree of AL of our patients or in which BODE quartile they are, knowing the size of their main PA could further help physicians predict their survival. In clinical practice, most of our COPD patients usually get a LDCT for several reasons: for early detection of lung cancer [28], to determine the presence and distribution of emphysema to guide a potential lung volume reduction procedure [29], to explore the presence of bronchiectasis [11], to determine the presence of coronary calcium [30] and now we are also providing novel information to help in determining their survival.
Shin et al.[22] also explored the relationship between PA diameter and mortality in patients with COPD. In a sample of 65 patients from an Advanced Lung Disease clinic for potential lung transplantation or volume reduction surgery, these investigators found that those with PH proven on right heart catheterization had a larger mean PA diameter than those without PH: 34.4mm vs 29.1mm, p = 0.0003. They also found that those with a PA/Aorta ratio >1 had a reduced mortality although in a highly selected population of severe COPD patients.
As expected, PA diameter significantly correlated with age, pack year history and BMI. As has been shown previously it also correlated (although weakly) with the history of exacerbations the year prior to enrollment [15]. All components of the BODE index and the index itself statistically correlated well with PA diameter. The strongest correlation was found with 6MWD (r = -0.39, p<0.001) implying that even in this middle age mild to moderate COPD population the presence of an enlarged PA negatively impact on exercise capacity.
Potential explanations for an enlarged PA in a COPD are many [13]. Chronic hypoxemia secondary to lung parenchyma destruction due to emphysema is the most frequent one, even more in these patients with up to 30% of them have grade 2–3 (moderate to severe) visual emphysema that could have not only intermittent hypoxemia but also pulmonary vessels destruction. Both emphysema severity and DLCO were not associated with main PA diameter in our cohort. Peinado et al. showed in transplanted lungs from severe COPD patients the association of emphysema and pulmonary vascular remodeling [31]. Co-existence of Obstructive Sleep Apnea (OSA) could be as highly prevalent as 30% in COPD patients [32] and a frequent cause of PH [33]. Vascular remodeling and endothelial dysfunction are a common feature even in patients with mild to moderate disease [13] as a consequence of chronic intermittent hypoxia and smoking.
There are several limitations in the present work. Firstly, these findings come from a relatively small sample of COPD patients usually followed at a pulmonary clinic and therefore could not be extrapolated to other types of COPD patients. Secondly, these findings should be restricted to male COPD patients since most of the participants were men. A similar study should be conducted in female COPD patients to confirm our findings. Thirdly, unfortunately an important and frequent determinant of PH in COPD patients such as OSA has not been explored. Nevertheless, independently of the presence or not of OSA, the detection of an enlarged PA still could predict patient`s survival. Fourthly, although BSA was included in the multivariable analysis to correct PA size for each patient characteristic, this model included PAE as a dichotomous ordinal variable and not the PA size a continuous variable that could be more appropriate. Lastly this is a single centre study and replication is required in a multicenter study.
In conclusion, in a population of mainly male COPD with mild to moderate AL and followed in our pulmonary clinic, the presence of an enlarged (diameter≥30mm) PA was the strongest predictor of all cause survival along with age, even stronger than most of the clinical and physiologic prognostic parameters for the disease, including the well-validated multidimensional BODE index.
Supporting information
(SAV)
Abbreviations
- COPD
Chronic Obstructive Pulmonary Disease
- MRC
modified Medical Research Council scale
- 6MWD
six minute walking distance
- BMI
body mass index
- FFMI
free fat mass index
- PH
pulmonary hypertension
- PAE
Pulmonary Artery Enlargement
- mPAP
Mean Pulmonary Artery Pressure
- AL
airway limitation
- ATS
American Thoracic Society
- ERS
European Respiratory Society
- GOLD
Global Initiative for Chronic Obstructive Lung Disease
- FEV1
Forced expiratory volume in the first second
- AA
ascending aorta
- OSA
Obstructive Sleep Apnea
Data Availability
All relevant data are within the paper and its Supporting Information files. The dataset of the present manuscript can also be found at: https://figshare.com/s/283dcb16f31a98e610c6.
Funding Statement
The authors have reported the following: J. J. Z. is a part-time employee of VisionGate, Inc. None declared (JPDT, A.E., A. B. A., G. B., A. C., J.B., J.G., C.C., B. R. C.). The funder provided support in the form of salaries for author JJZ, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of this author is articulated in the 'author contributions' section.
References
- 1.Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet 2004; 364: 613–620. doi: 10.1016/S0140-6736(04)16855-4 [DOI] [PubMed] [Google Scholar]
- 2.Vogelmeier CF, Criner GJ, Martínez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report: GOLD Executive Summary. Arch Bronconeumol. 2017;53:128–149. doi: 10.1016/j.arbres.2017.02.001 [DOI] [PubMed] [Google Scholar]
- 3.Casanova C, Cote C, de Torres JP, Aguirre-Jaime A, Marin JM, Pinto-Plata V, et al. Inspiratory-to-total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171:591–7. doi: 10.1164/rccm.200407-867OC [DOI] [PubMed] [Google Scholar]
- 4.Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest 2002;121:1434–1440 [DOI] [PubMed] [Google Scholar]
- 5.Casanova C, Cote C, Marin JM, Pinto-Plata V, de Torres JP, Aguirre-Jaíme A, et al. Distance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPD. Chest. 2008;134:746–52 doi: 10.1378/chest.08-0520 [DOI] [PubMed] [Google Scholar]
- 6.Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;157:1791–1797 doi: 10.1164/ajrccm.157.6.9705017 [DOI] [PubMed] [Google Scholar]
- 7.Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60:925–31 doi: 10.1136/thx.2005.040527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:1005–12. doi: 10.1056/NEJMoa021322 [DOI] [PubMed] [Google Scholar]
- 9.Puhan MA, Garcia-Aymerich J, Frey M, ter Riet G, Antó JM, Agustí AG, et al. Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO index. Lancet. 2009;374:704–11. doi: 10.1016/S0140-6736(09)61301-5 [DOI] [PubMed] [Google Scholar]
- 10.Zulueta JJ, Wisnivesky JP, Henschke CI, Yip R, Farooqi AO, McCauley DI, et al. Emphysema scores predict death from COPD and lung cancer. Chest. 2012;141:1216–1223. doi: 10.1378/chest.11-0101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martínez-García MA, de la Rosa Carrillo D, Soler-Cataluña JJ, Donat-Sanz Y, Serra PC, Lerma MA, et al. Prognostic value of bronchiectasis in patients with moderate-to-severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187:823–31. doi: 10.1164/rccm.201208-1518OC [DOI] [PubMed] [Google Scholar]
- 12.Terzikhan N, Bos D, Lahousse L, Wolff L, Verhamme KMC, Leening MJG, et al. Pulmonary artery to aorta ratio and risk of all-cause mortality in the general population: the Rotterdam Study. Eur Respir J. 2017;49(6) [DOI] [PubMed] [Google Scholar]
- 13.Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34–41. [DOI] [PubMed] [Google Scholar]
- 14.Blanco I, Piccari L, Barberà JA. Pulmonary vasculature in COPD: The silent component. Respirology. 2016;21:984–94 doi: 10.1111/resp.12772 [DOI] [PubMed] [Google Scholar]
- 15.Ascha M, Renapurkar RD, Tonelli AR. A review of imaging modalities in pulmonary hypertension. Ann Thorac Med. 2017; 12: 61–73 doi: 10.4103/1817-1737.203742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wells JM, Washko GR, Han MK, Abbas N, Nath H, Mamary AJ, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012;367:913–21. doi: 10.1056/NEJMoa1203830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung KS, Kim YS, Kim SK, Kim HY, Lee SM, Seo JB, et al. Functional and Prognostic Implications of the Main Pulmonary Artery Diameter to Aorta Diameter Ratio from Chest Computed Tomography in Korean COPD Patients. PLoS One. 2016;11:e0154584 doi: 10.1371/journal.pone.0154584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Thoracic Society Statement. Lung function testing; selection of reference values and interpretative strategies (1991) Am Rev Resp Dis. 144: 1202–1218. doi: 10.1164/ajrccm/144.5.1202 [DOI] [PubMed] [Google Scholar]
- 19.ATS Statement: Guidelines for the Six-Minute Walk Test (2002) Am J Respir Crit Care Med. 166: 111–117. doi: 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 20.Mahler D, Weels C (1988) Evaluation of clinical methods for rating dyspnea. Chest. 93: 580–586. [DOI] [PubMed] [Google Scholar]
- 21.National Emphysema Treatment Trial Research Group, Fishman A, Fessler H, Martinez F, McKenna RJ Jr, Naunheim K, Piantadosi S, et al. Patients at High Risk of Death after Lung-Volume–Reduction Surgery. N Engl J Med 2001;345:1075–1083. doi: 10.1056/NEJMoa11798 [DOI] [PubMed] [Google Scholar]
- 22.Shin S, King CS, Brown AW, Albano MC, Atkins M, Sheridan MJ, et al. Pulmonary artery size as a predictor of pulmonary hypertension and outcomes in patients with chronic obstructive pulmonary disease. Respir Med. 2014;108:1626–32 doi: 10.1016/j.rmed.2014.08.009 [DOI] [PubMed] [Google Scholar]
- 23.Monroe S. Multivariate Behav Res. 2018;53:247–266. doi: 10.1080/00273171.2017.1419851 [DOI] [PubMed] [Google Scholar]
- 24.Truong QA, Massaro JM, Rogers IS, Mahabadi AA, Kriegel MF, Fox CS, et al. Reference values for normal pulmonary artery dimensions by noncontrast cardiac computed tomography: The Framingham Heart Study. Circ Cardiovasc Imaging. 2012;5:147–54. doi: 10.1161/CIRCIMAGING.111.968610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tonelli AR, Arelli V, Minai OA, Newman J, Bair N, Heresi GA, et al. Causes and circumstances of death in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2013;188:365–9. doi: 10.1164/rccm.201209-1640OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pérez-Padilla R, Hallal PC, Vázquez-García JC, Muiño A, Máquez M, López MV, et al. ; PLATINO group. Impact of bronchodilator use on the prevalence of COPD in population-based samples. COPD 2007;4:113–120. doi: 10.1080/15412550701341012 [DOI] [PubMed] [Google Scholar]
- 27.de Torres JP, Casanova C, Marín JM, Pinto-Plata V, Divo M, Zulueta JJ, et al. Prognostic evaluation of COPD patients: GOLD 2011 versus BODE and the COPD comorbidity index COTE. Thorax. 2014;69:799–804. doi: 10.1136/thoraxjnl-2014-205770 [DOI] [PubMed] [Google Scholar]
- 28.de-Torres JP, Casanova C, Marín JM, Zagaceta J, Alcaide AB, Seijo LM, et al. Exploring the impact of screening with low-dose CT on lung cancer mortality in mild to moderate COPD patients: a pilot study. Respir Med. 2013;107:702–7 doi: 10.1016/j.rmed.2013.01.013 [DOI] [PubMed] [Google Scholar]
- 29.Shah PL, Herth FJ, van Geffen WH, Deslee G, Slebos DJ. Lung volume reduction for emphysema. Lancet Respir Med. 2017;5:147–156. doi: 10.1016/S2213-2600(16)30221-1 [DOI] [PubMed] [Google Scholar]
- 30.Williams MC, Murchison JT, Edwards LD, Agustí A, Bakke P, Calverley PM, et al. Coronary artery calcification is increased in patients with COPD and associated with increased morbidity and mortality. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) investigators. Thorax. 2014;69:718–23. doi: 10.1136/thoraxjnl-2012-203151 [DOI] [PubMed] [Google Scholar]
- 31.Peinado VI, Gómez FP, Barberà JA, Roman A, Angels Montero M, et al. Pulmonary vascular abnormalities in chronic obstructive pulmonary disease undergoing lung transplant. J Heart Lung Transplant. 2013;32:1262–9. doi: 10.1016/j.healun.2013.09.007 [DOI] [PubMed] [Google Scholar]
- 32.Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182:325–3 doi: 10.1164/rccm.200912-1869OC [DOI] [PubMed] [Google Scholar]
- 33.Chaouat A, Weitzenblum E, Krieger J, Ifoundza T, Oswald M, Kessler R. Association of chronic obstructive pulmonary disease and sleep apnea syndrome. Am J Respir Crit Care Med. 1995;151:82–86. doi: 10.1164/ajrccm.151.1.7812577 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files. The dataset of the present manuscript can also be found at: https://figshare.com/s/283dcb16f31a98e610c6.