Abstract
Bilateral sagittal split osteotomy (BSSO) is a widely-performed procedure in orthognathic surgery for the correction of dentofacial deformity. Condylar positioning is a critical step during BSSO to maximize functional and morphological results. The unsuitable positioning of condyles represents one of the causative mechanisms that may induce temporomandibular joint noxious effects after BSSO. Repositioning devices can assist surgeons in maintaining the preoperative condylar position; however, empirical repositioning methods based on experience gained are still commonly used. Trainee learning curves are difficult to assess. The aim of this study was to evaluate the relevance of computer-assisted surgery in the acquisition of condylar positioning skills. Forty-eight patients underwent BSSO performed by six maxillofacial trainees (four junior residents and two senior experienced residents). A condyle positioning system (CPS) was used by a senior surgeon to record a condylar position score during the procedure. Firstly, scores were recorded when the trainee manually positioned the condyle without access to the CPS score (phase 1) and then when the trainee positioned the condyle and performed osteosynthesis with visual access to the CPS score (phase 2). Six parameters describing condylar three-dimensional motions were assessed: translational motion from top to bottom (TB), back to front (BF), and left to right (LR), axial rotation (AR), sagittal rotation (SR), frontal rotation (FR), and a total score (TS). There were no significant differences between junior and senior residents in condyle positioning without access to the CPS. Condyles were significantly better positioned during phase 2 with access to the CPS (p<0.001). Over time, use of the CPS (phase 2) produced significantly quicker improvements in scores (p = 0.042). For those teaching surgeries to trainees, computer-assisted devices can potentially result in more rapid learning curves than traditional “observations-imitation” models. Use of a CPS by trainees facilitated condylar repositioning that resulted in an accurate occlusal result and avoidance of adverse effects on the temporomandibular joint.
Introduction
Bilateral sagittal split osteotomy (BSSO) is a widely-performed orthognathic procedure for the correction of dentofacial deformity. Maintaining the condylar position during BSSO remains technically difficult and is related to the surgeon’s experience. Most maxillofacial surgeons use an intuitive repositioning technique consisting of manual placement of the condylar process in the superior and posterior glenoid fossa [1,2]. Centric condyle relation is considered as a reference positioning and used for reproducibility. Acquisition of condyle repositioning skills is critical in achieving BSSO competency to avoid adverse effects on the temporomandibular joint. The unsuitable positioning of condyles represents one of the causative mechanism that may induce temporomandibular joint noxious effects among many factors [3]. The relationship between intraoperative malpositioning of the condyle and the occurrence of condylar resorption with relapse resulting in high levels of strain is well-known. Condylar resorption is a complication with a reported frequency of between 1.4% and 31% [3,4]. Relapse of the occlusal result can occur because of unduly posterior positioning of the condyle during mandibular advancement [5,6] or a high degree of rotation of the condyle during mandibular setback [7]. Plastic and maxillofacial surgery supervisors have an obligation to provide a training environment that includes evaluation mechanisms to certify acceptable acquisition of surgical skills [8,9]. Trainee learning curves for condylar positioning during BSSO are difficult to assess, especially using a manual empirical method. Traditional “observations-imitation” models based on the action of a supervisor require repeated practice and have steep learning curves. Dissection training is constrained and cannot offer condylar repositioning training because it may introduce damage to tissues which influences their anatomical position [10]. Despite of none scientific evidence supported the routine use of condyle positioning devices to prevent TMJ disorders [11–14], computer-assisted navigation could be considered as an educational tool to control the learning curve for condylar positioning among condylar positioning devices available to help surgeons in condylar repositioning [12]. Bettega et al. [15,16] have developed a condylar positioning system (CPS) based on navigation and underlined the benefits of using CPS routinely for clinical and educational purposes. The aim of this study was to evaluate the relevance of this computer-assisted surgery in acquiring condylar positioning competence.
Materials and methods
Forty-eight patients without temporomandibular joint disorder (TMD) underwent BSSO with osteosynthesis performed by six maxillofacial trainees. Two senior residents (trainees 1 and 6) had already undergone a period of supervised training with an experienced surgeon and the remaining four junior trainees had no experience (trainees 2, 3, 4, and 5). Patients with non-syndromic dentofacial deformity requiring isolated BSSO with or without bimaxillary osteotomy were included for analysis. One ramus was assessed regardless of the side and the opposite side was handled by an instructor. The condyle positioning system (CPS) developed by Bettega et al. [15,16] (and improved with technological progress) was used by a senior surgeon to record a condylar position score during the procedure. The system consisted of a 3D optical localizer, Orthopilot® (B. Braun-Aesculap, Tuttlingen, Germany), including a double camera (Polaris; NDI, Waterloo, Canada) (Fig 1) and infrared reflectors fixed on the coronoid process (Fig 2) and orbital ridge (Fig 3). The device fixed on the coronoid process was equipped with a connection that could hold a removable intermediary part to support infrared reflectors. Surgery began with the recording of the condyle reference position and identification of predetermined anatomic landmarks. The reference position corresponded to the centric relation that was established during the preoperative assessment and could be reproduced using a sterile centric relation splint. The patient’s centric relation bite was recorded using Dawson’s bilateral manipulation method [17] the day before the surgery in order to obtain the most posterior and superior location of the condyle in glenoid fossa. Reflectors fixed on the coronoid process were then removed and only the osseous anchorage remained, which completely freed the operation field.
Fig 1. System with a 3D optical localizer including a double camera.
Fig 2. Infrared reflectors fixed on the coronoid process.
Fig 3. Infrared reflectors fixed on the orbital rim.
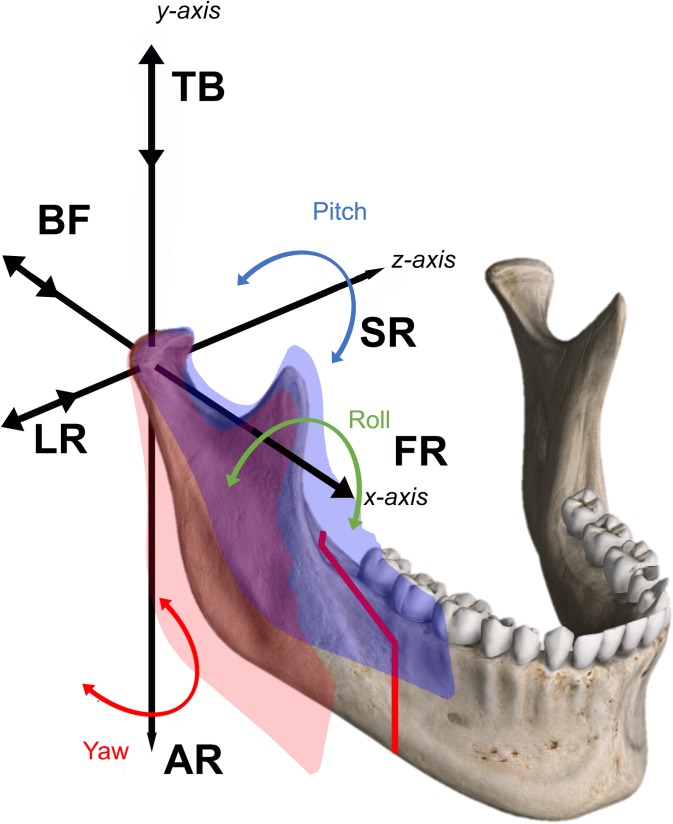
Each BSSO procedure was performed according to Obwegeser-Dal Pont [18,19]. Maxillomandibular fixation was then secured and the reflectors were reinserted on their respective anchorage to permit positional condyle assessment. The system provided control of the condylar fragment in a three-dimensional position and tracking of condylar displacement on the computer screen (Fig 4) during attempts to overlap the reference position (multimedia file). First, data were recorded by the supervisor as the trainee manually positioned the proximal segment without access to the CPS score (phase 1). Then, when the trainee positioned the proximal segment and performed osteosynthesis, they were given visual access to the CPS score (phase 2). The condyle position records during phase 2 were obtain before the osteosynthesis and then the osteosynthesis were performed in keeping the control of the condylar position on the screen. Osteosynthesis was performed by fixing three bicortical positional bone screws (2 mm diameter) placed using a transbuccal approach (S1 Video). Each trainee performed eight consecutive procedures. Six parameters describing condylar three-dimensional motions were assessed in phase 1 and phase 2 (Fig 5). First, the translational displacements were assessed: from top to bottom (TB), back to front (BF), and left to right (LR). Second, rotational displacements were assessed: axial rotation (AR), sagittal rotation (SR), frontal rotation (FR), and total score (TS), which was the sum of the scores in absolute values (). Translational and rotational parameters were defined in millimeters and degrees, respectively. Positive and negative signs indicated the direction of displacement. Quantitative variables were expressed as means and standard deviations (SD).
Fig 4. Tracking of condylar displacement (rotational and translational motions) on the computer screen.
green: condylar fixed reference position, blue: mobilized bone segment by trainee (trainee position).
Fig 5. Translational and rotational displacements.
Top to bottom (TB), back to front (BF), left to right (LR) and axial rotation (AR), sagittal rotation (SR), frontal rotation (FR), and total score (TS).
Qualitative variables were expressed as counts and percentages. Differences between groups were evaluated using the chi-square test or Fisher’s exact test for categorical variables and the t test for continuous variables. Linear mixed effect models were used to analyze the evolution of the measured value with increases in the number of interventions. Statistical analyses were performed using R.3.2.3 software.
A positive IRB n°5921 (Ethic committee, CECIC Rhône-Alpes-Auvergne) expeditive review was obtained (S1 Text) and all patients were informed orally of the protocol with writing consent, risks and use of the data for biomedical research.
Results
The mean age of patients who underwent BSSO was 21.98 years, and 27 (56.25%) were female and 21 (43.75%) were male. Twenty-four patients received an isolated mandibular osteotomy (± genioplasty) and the other 24 cases underwent bimaxillary procedures (± genioplasty) (Table 1). One ramus for each patient was used to assess the condylar positioning of trainees. No specific complications related to the use of the system were noted. There was no significant difference in the positioning of condyles for the junior and senior residents in phase 1 and phase 2 (Table 2). Condyles were positioned with better control during phase 2 using the CPS for all trainees. The mean (SD) of absolute values was 2.56 (2.36) during phase 1 and 1.37 (1.25) during phase 2 (p<0.001) (Table 3). Results showed that rotational movements in the axial axis (AR) with a mean of 4° (p<0.001) and translational movements in the left to right (LR) dimension with a mean of 2.48 mm (p = 0.013) were more difficult and less accurate to handle during phase 1 for all trainees (Table 3).
Table 1. Summary of the population and the surgical procedures.
| Patient (N°) | Gender | Age (year) | Indication | Surgical procedure | Trainee-Intervention (n°-n°) | Side |
|---|---|---|---|---|---|---|
| 1 | M | 22 | Mandibular Class II | BSSO advancement of 6 mm, genioplasty | 1–1 | L |
| 2 | F | 16 | Mandibular Class II | BSSO advancement of 9 mm | 1–2 | L |
| 3 | F | 20 | Open bite Class III | Le Fort I advancement, BSSO asymmetric set back 2 mm | 1–3 | L |
| 4 | M | 24 | Open bite Class II | Le Fort I advancement, BSSO advancement 9 mm, genioplasty | 2–1 | R |
| 5 | F | 21 | Class III | Le Fort I advancement, BSSO setback 3 mm | 1–4 | L |
| 6 | F | 17 | Mandibular Class II | BSSO advancement of 7 mm | 2–2 | L |
| 7 | F | 15 | Mandibular Class II | BSSO advancement of 5 mm | 1–5 | R |
| 8 | F | 16 | Mandibular Class II | Le Fort I advancement, BSSO asymmetric advancement 4 mm | 2–3 | R |
| 9 | F | 22 | Mandibular Class II | BSSO advancement of 10 mm | 2–4 | R |
| 10 | M | 22 | Open bite Class II | Le Fort I advancement, BSSO advancement 10 mm, genioplasty | 2–5 | L |
| 11 | M | 24 | Mandibular Class II | Le Fort I advancement, BSSO asymmetric advancement 7 mm, genioplasty | 1–6 | L |
| 12 | M | 16 | Open bite Class III | Le Fort I advancement, BSSO asymmetric set back 2 mm | 2–6 | L |
| 13 | F | 16 | Mandibular Class II | BSSO advancement of 7 mm | 1–7 | R |
| 14 | M | 18 | Open bite Class II | Le Fort I advancement, BSSO advancement 8 mm | 1–8 | L |
| 15 | M | 22 | Mandibular Class II | Le Fort I reposition, BSSO asymmetric advancement 4 mm, genioplasty | 2–7 | R |
| 16 | M | 19 | Mandibular Class II | BSSO asymmetric advancement of 7 mm | 2–8 | L |
| 17 | F | 17 | Mandibular Class II | BSSO advancement of 7 mm, genioplasty | 3–1 | R |
| 18 | M | 21 | Mandibular Class II | BSSO advancement of 6 mm | 3–2 | R |
| 19 | M | 37 | Mandibular Class II | BSSO advancement of 6 mm, genioplasty | 3–3 | R |
| 20 | F | 16 | Mandibular Class II | BSSO advancement of 9 mm, genioplasty | 3–4 | L |
| 21 | M | 16 | Class III | Le Fort I advancement, BSSO set back 3 mm | 3–5 | L |
| 22 | M | 23 | Class III | Le Fort I advancement, BSSO set back 3 mm, genioplasty | 3–6 | L |
| 23 | F | 21 | Open bite Class III | Le Fort I advancement, BSSO asymmetric set back 3 mm | 3–7 | L |
| 24 | M | 18 | Mandibular Class II | Le Fort I reposition, BSSO advancement of 10 mm | 3–8 | L |
| 25 | F | 19 | Asymmetrical Class II | Le Fort I frontal rotation for midline correction, BSSO asymmetrical advancement 9 mm | 4–1 | L |
| 26 | M | 24 | Mandibular Class II | BSSO advancement of 9 mm | 4–2 | L |
| 27 | F | 20 | Asymmetric Class I | Le Fort I frontal rotation for midline correction, BSSO | 4–3 | L |
| 28 | M | 17 | Open bite Class II | Le Fort I advancement, BSSO advancement 9 mm, genioplasty | 5–1 | R |
| 29 | M | 17 | Mandibular Class II | BSSO advancement of 8 mm | 6–1 | L |
| 30 | F | 16 | Mandibular Class II | BSSO advancement of 9 mm | 5–2 | L |
| 31 | F | 56 | OSAS | Le Fort I + BSSO advancement of 12 mm | 5–3 | L |
| 32 | F | 19 | Open bite Class III | Le Fort I advancement, BSSO asymmetric set back 2 mm | 4–4 | L |
| 33 | F | 20 | Mandibular Class II | BSSO advancement of 8 mm | 6–2 | R |
| 34 | F | 24 | Mandibular Class II | BSSO advancement of 7 mm | 4–5 | L |
| 35 | M | 16 | Mandibular Class II | BSSO advancement of 7 mm | 4–6 | R |
| 36 | F | 32 | Open bite Class II | Le Fort I advancement, BSSO advancement 11 mm, genioplasty | 4–7 | R |
| 37 | M | 29 | Mandibular Class II | BSSO advancement of 6 mm | 5–4 | R |
| 38 | F | 30 | Open bite Class II | Le Fort I advancement, BSSO advancement 14 mm, genioplasty | 4–8 | R |
| 39 | M | 17 | Mandibular Class II | BSSO advancement of 6 mm | 5–5 | L |
| 40 | M | 20 | Mandibular Class II | BSSO advancement of 5 mm, genioplasty | 6–3 | R |
| 41 | F | 22 | Class III | Le Fort I advancement, BSSO set back 3 mm | 5–6 | R |
| 42 | F | 30 | Open bite Class II | Le Fort I advancement, BSSO advancement 9 mm, genioplasty | 5–7 | L |
| 43 | F | 24 | Mandibular Class II | BSSO asymmetric advancement of 7 mm | 6–4 | L |
| 44 | F | 42 | OSAS | Le Fort I + BSSO advancement of 12 mm | 5–8 | L |
| 45 | F | 16 | Mandibular Class II | BSSO advancement of 9 mm | 6–5 | R |
| 46 | M | 18 | Open bite Class III | Le Fort I advancement, BSSO asymmetric set back 2 mm | 6–6 | L |
| 47 | F | 25 | Mandibular Class II | BSSO advancement of 6 mm | 6–7 | R |
| 48 | F | 23 | Mandibular Class II | BSSO advancement of 10 mm, genioplasty | 6–8 | R |
M, male; F, female; L, left; R, right; BSSO, bilateral sagittal split osteotomy; OSAS, obstructive sleep apnea syndrome.
Table 2. Difference in the positioning of condyle between the junior and senior residents in phase 1 and phase 2.
| Phase 1 | Phase 2 | |||||
|---|---|---|---|---|---|---|
| Junior trainees Score (SD) | Senior trainees Score (SD) | p (t-test) | Junior trainees Score (SD) | Senior trainees Score (SD) | p (t-test) | |
| TB (mm) | 1.95(1.61) | 1.7(1.16) | 0.652 | 1.16(0.95) | 1.1(0.88) | 0.862 |
| BF (mm) | 1.08(1.08) | 1.5(1.18) | 0.285 | 0.97(0.75) | 1.1(0.74) | 0.638 |
| LR (mm) | 2.45(2.04) | 2.6(1.71) | 0.829 | 1.47(1.11) | 2.3(2.11) | 0.095 |
| FR (°) | 2.24(2.12) | 3(1.94) | 0.31 | 1.61(1.22) | 2.7(2.36) | 0.047 |
| AR (°) | 4.26(2.8) | 3(2.05) | 0.189 | 1.68(1.68) | 1.2(0.63) | 0.378 |
| SR (°) | 3.74(3.25) | 2.1(2.23) | 0.142 | 1.13(0.88) | 0.6(0.7) | 0.083 |
| TS | 15.71(7.01) | 13.9(4.41) | 0.132 | 8.03(3.28) | 9(3.13) | 0.403 |
TB, top to bottom translation; BF, back to front translation; LR, left to right translation; FR, frontal rotation; AR, axial rotation; SR, sagittal rotation; TS, total score; mm, millimeters; °, degrees; SD, standard deviation. Scores in absolute values.
Table 3. Difference in the positioning of condyle between phase 1 and phase 2 for all trainees.
| Junior and senior trainees | |||
|---|---|---|---|
| Phase 1 Score (SD) | Phase 2 Score (SD) | p (student test) | |
| TB (mm) | 1.9 (1.52) | 1.15 (0.92) | 0.003 |
| BF (mm) | 1.17 (1.1) | 1 (0.74) | 0.364 |
| LR (mm) | 2.48 (1.96) | 1.65 (1.39) | 0.013 |
| FR (°) | 2.4 (2.09) | 1.83 (1.56) | 0.104 |
| AR (°) | 4 (2.69) | 1.58 (1.53) | <0.001 |
| SR (°) | 3.4 (3.12) | 1.02 (0.86) | <0.001 |
| TS | 15 (6.55) | 8.23 (3.24) | <0.001 |
| Mean | 2.56 (2.36) | 1.37 (1.25) | <0.001 |
TB, top to bottom translation; BF, back to front translation; LR, left to right translation; FR, frontal rotation; AR, axial rotation; SR, sagittal rotation; TS, total score; mm, millimeters; °, degrees; SD, standard deviation. Score (mean of absolute values).
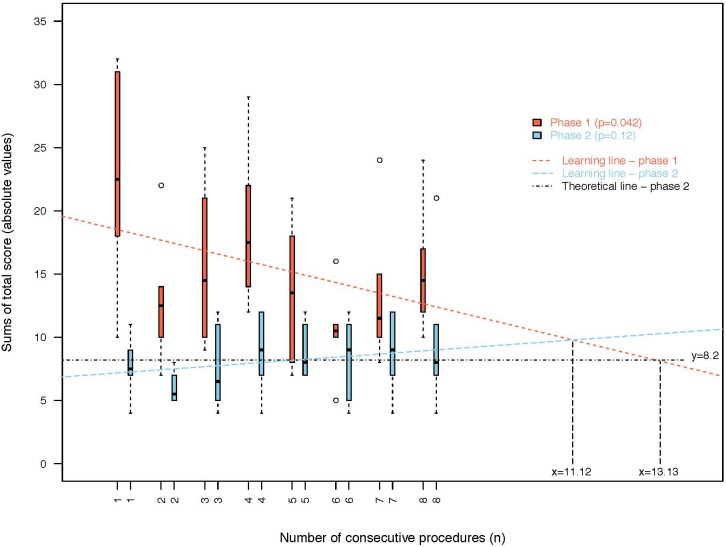
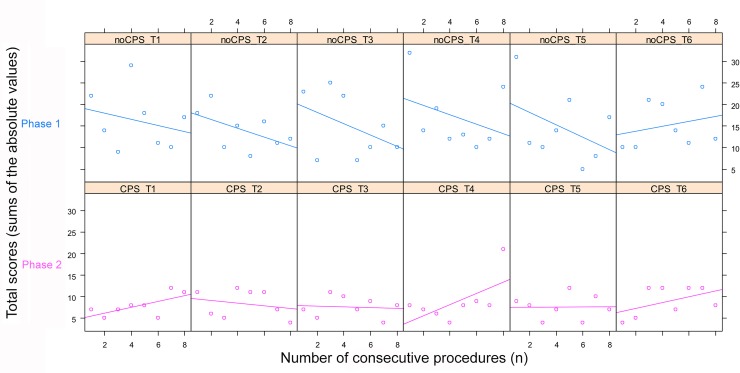
Over eight consecutive procedures, significant global improvements in total scores (TS) (sums of the absolute values) were seen in phase 1 (p = 0.042) for trainees (Fig 6), and there was a non-significant deterioration in scores in phase 2 (p = 0.12). Fig 7 shows the total score (TS) of each trainee, and only results for trainee 6 did not improve in phase 1.
Fig 6. Total scores (TS) evolution according to the number of procedures.
Fig 7. Total score (TS) of each trainee with consecutive procedures.
CPS: condyle positioning system.
The evolution of the score lines for phase 1 and phase 2 showed a crossing after 11 procedures. The theoretical line of no-deterioration in phase 2 should have crossed the phase 1 line after 13 procedures (Fig 6).
Discussion
Most maxillofacial surgeons use an intuitive empirical method for repositioning the condylar fragment during BSSO [2,12]. The condyle centric position used as a reference is not a physiological position but rather a border position that is used for reproducibility. Surgeons rely on manual repositioning after BSSO in order to obtain the best mandibular proximal segment relationship with the condylar fossa [13]. Acquisition of this “intuitive” technical skill using the traditional ‘‘apprentice–mentor” education model produces a lengthy learning curve in which performance tends to improve after a long period of experience [20,21]. Acquisition of condylar repositioning skills mastered using observation, followed by imitation of the mentor’s actions can be difficult for trainees and this can result in adverse functional implications following this technically demanding step. Condyle repositioning devices are usually used by clinicians who do not wish to intuitively reposition the condylar fragment during BSSO [12]. Among many condyle repositioning techniques, the navigation technique developed by Bettega et al. [15,16] can improve condyle position within a precision of 1 mm in translational movements and 1° in rotational movements. Elfring et al. [22] assessed the accuracy of the optical localizer system used in our study and showed equal precision.
Bettega et al. [15,16] compared groups of patients which underwent BSSO with standard technique (empirical group) and BSSO with CPS (active group) and assessed postoperative occlusion, stability of skeletal position, the preservation of mandibular motion and the occurrence of temporomandibular dysfunction with 12 months follow up. Forty five percent of empirical group showed worsened temporomandibular joint status and only one in the active group. Despite of the previous results we do not overestimate the usefulness of CPS because our study did not provide any results on the occurrence of the temporomandibular joint disorders and we emphasize the educational interest of CPD more than its clinical importance.
Computer-aided innovations have become routine practice in oral and maxillofacial surgery teaching [23,24]. To the best of our knowledge, no study has evaluated the contribution of navigation devices for skill development. In a recent review, Azermehr et al. [25] described the most common indications for navigation devices in all fields of oral and maxillofacial surgery; however, this has not raised interest. Therefore, the aim of this study was to evaluate the relevance of a CPS device that provides graphical results of performance against experience as a learning tool to facilitate a short learning curve.
In our orthognathic center, we use navigation systems and computer-aided BSSO surgery to help surgeons in replacing the condylar process, and therefore, the implementation of this device for our research was simple to establish. This study assessed clinical practice and was not a clinical research study. The navigational device used in this study removed the need for preoperative CT imaging, and therefore, unnecessary patient irradiation that occurs with other navigational techniques [26]. Furthermore, it prevents registration of data problems by the computer algorithm, which could affect the precision and accuracy of the navigation system [27].
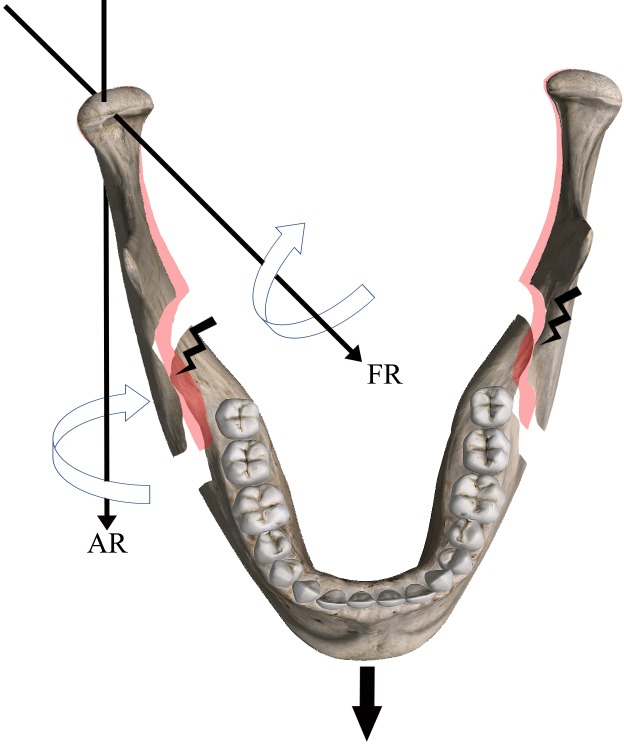
Our study showed a significant improvement in condyle placement over consecutive procedures with a crossing of the phase 1 and phase 2 lines after 10 procedures. Theoretically, the phase 2 line should have been “flat” without any increase or decrease in slope but there was a non-significant deterioration in the overall score. This was due to the bad replacement performed in patient n° 38 by trainee 4 during the last procedure (Table 1), with a total score of 24 in phase 1 and 21 in phase 2 (Fig 7). This procedure was a crucial mandibular advancement resulting in an internal segment and proximal condylar segment conflict [28]. This might have led to the interference of unidentified posterocaudal bony segments with the final positioning of the condylar segment, showing that placement in a similar preoperative position is still challenging after excessive mandibular movement [29] (Fig 8). Indeed, it is commonly accepted that advancements greater than 10 mm expose condyles to condylar resorption due to an increasing of tension of the surrounding soft tissues producing an inferior-posteriorly directed force [3,30]. Condyle rotation induces excessive mechanical stress and the adaptive capacities of the host are diminished, the remodeling becomes dysfunctional, and this leads to condylar resorption. This demonstrates, once again, to the importance of leaving the condyle in a position as close as possible to the preoperative position. Trainee 4 could not correctly relocate the condyle axial rotation movement, which is often the case in large advancements. Therefore, we drew a theoretical line of optimal placement of the condyle. The phase 1 line crossed this theoretical line after about 13 procedures. We can assume that regardless of the type of BSSO, the learning curve plateau after 13 procedures, which is supposedly a shorter period compared to traditional learning. On the other hand, the experienced trainee 6 was the only trainee to not improve during phase 1, perhaps due to prior experience in condylar repositioning.
Fig 8. Interference of posterocaudal bony segments with axial and frontal condylar segment rotation after excessive mandibular advancement.
To the best of our knowledge, no study has assessed the learning curves for condylar positioning in trainees to determine the number required procedures without (and with) CPS. Future studies should assess the effectiveness of non-tutored practice of condylar positioning during phase 1 of BSSO to clarify this point. The highly individual learning curves suggest a predefined number of practice sessions before a mean plateau is reached, highlighting the maximum possible benefit. However, achieving this level is dependent on defining such a standard first, and ideally using a validated performance assessment tool. Most reported instruments for condylar segment repositioning performance assessment, such as cephalometric analysis [31], CT [5], cone beam CT (CBCT) [32,33], and finite element analysis [34], can capture position aspects, but only in post-operative conditions. The CPS appears to be an efficient intra-operative learning tool that is completely safe. Nonetheless, all of these methods are dependent on the time-consuming rating of performance using trained experts’ context of deliberate practice and training towards a standard set of proficiency levels.
Our study assessed the learning curve of condyle repositioning regardless of the side of the BSSO. However, it seems essential to pay attention to the effect of the dominant hand and side on the ability and confidence in using powered instruments. Abdel-Galil et al. [35] assessed trainers and trainees during BSSO, and confirmed that most operators were right-handed and most trainees surveyed reported that they operated predominantly from the left side when doing a BSSO, whereas their trainers operated predominantly from the right side. It is our practice that trainers and trainees alternate operating sides for consecutive cases, allowing the trainee to experience performing the same procedure using different approaches, as well as learning the motor skills required to use the non-dominant hand, thereby improving confidence and safety.
The length of time taken for the procedure was not included as a study parameter and the “learning curve” was also defined as improving performance over time or increasing experience or training. In retrospect, we should have undertaken a “learning curve cumulative sum analysis (LC-CUSUM)”, which is a sequential analysis tool originally developed for quality control purposes according the duration of the procedure and can be used to judge when an individual’s performance has reached a predefined level of competence [36]. This statistical tool would allow evaluation of the specific influence of the CPS in the learning of repositioning skills during phase 1 after consecutive procedures, and not only in phase 2.
Learning and skills acquisition is dependent on memory consolidation, and the spacing of practice allows this to occur [37]. The optimal intertraining interval for skills practice and consolidation (distributed practice) is still debated in the literature, but has been demonstrated to benefit complex psychomotor skills acquisition in virtual reality simulated laparoscopy training [38]. Our study was based on consecutive practice and did not assess the effects of intertraining intervals which ranged from 1 day to many days. However, this parameter is more suitable for the learning of virtual reality simulation surgery [37]. The optimal intertraining interval for skills practice and consolidation is still debated in the literature [39]. Learning and skills acquisition is dependent on memory consolidation, and spacing of practice allows this to occur [40]. A minimal of three intertraining days is considered as sufficient for improving novice performance [40]. In our study this intertraining delay was respected.
Various virtual reality simulators and haptic devices have been proposed and implemented in past years [23,41]. Surgical simulation offers a near-realistic training environment, with the possibility for unlimited training over a wide variety of procedures. However, simulation is not suitable for condylar positioning skill development as the simulation of realistic force feedback is not possible. Furthermore, positioning guides and pre-bended osteosynthesis plates are being increasingly used in orthognathic surgery owing to their accuracy. These guides are manufactured using computer-aided design/computer-aided manufacturing (CAD/CAM) technologies after digital surgery planning rather than conventional planning to provide better accuracy [42][43]. Condyle positioning is predetermined during the digital planning and this offers facilitation of better intraoperative condyle positioning, but this cannot be considered as a learning tool.
In our study, all BSSO osteosynthesis procedures involved rigid fixation and the fixation of three bicortical positional bone screws. Rigid and non-rigid fixation in BSSO are important considerations in the condylar segment positioning learning curve. Indeed, the technical management is different for the two procedures, and clinicians are concerned that rigid internal fixation can induce great changes in the position of the condyle compared to non-rigid fixation [33,44,45]. The use of condylar positioning devices seems reasonable for practice and learning [12], but there are still controversies. In a future study, we will assess the condylar positioning with non-rigid fixation learning curve using the same procedures and will compare results to the results of this study.
We have emphasized in this study the importance of the condyle position during BSSO but we highlight the influence of the closing and opening muscle groups of the jaw on the stress distribution in the condyles with changing jaw position after BSSO with condylar resorption consequence [34,46–48].
We must remember that the condylar positioning step of BSSO is critical to learn, but the acquisition of osteotomy skills is also crucial and cannot be assessed with the CPS. The development of a simulator that provides training for all stages of BSSO would be ideal.
Conclusion
Our results show that condylar repositioning skill development based on navigational computer-assisted surgery is effective for trainees, and the acquired skills are qualitatively and quantitatively measurable. CPS provides for trainees to obtain a condyle position reference positioning during bilateral sagittal split osteotomy and limits the excessive movement of the condyles. The use of a CPS is an effective aid in condylar repositioning and can be consider as a tool for acquiring condylar positioning skills, particularly taking into account the reduced working hours and increased number of residents in hospitals, which may result in less exposure to surgery. Our study showed only this educational interest, however further studies need to carry out to assess the relationship between the use of CPS and less occurring of temporomandibular joint disorders.
Constant innovations in treatment modalities means there are always new surgical procedures to be learnt by supervisors and mentors and this reduces the number of surgical procedures available for the teaching and learning of apprentices. Furthermore, the continuous pressure to reduce operation times in order to be more cost effective, and the ethical aspects to limit patient morbidity, reduce complications, and maximize patient safety drive public awareness and demand professional responsibility.
Supporting information
(MP4)
(PDF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Oh S-M, Lee C-Y, Kim J-W, Jang C-S, Kim J-Y, Yang B-E. Condylar repositioning in bilateral sagittal split ramus osteotomy with centric relation bite. J Craniofac Surg. 2013;24: 1535–8. doi: 10.1097/SCS.0b013e31829028be [DOI] [PubMed] [Google Scholar]
- 2.Lee CY, Yang BE, Kim JY, Oh SM, Park KN. Centric-relation bite as a condylar positioning device in bimaxillary surgery. J Oral Maxillofac Surg. 2013;71: e65–e66. [Google Scholar]
- 3.Mousoulea S, Kloukos D, Sampaziotis D, Vogiatzi T, Eliades T. Condylar resorption in orthognathic patients after mandibular bilateral sagittal split osteotomy: A systematic review. Eur J Orthod. 2017;39: 294–309. doi: 10.1093/ejo/cjw045 [DOI] [PubMed] [Google Scholar]
- 4.Wolford LM, Reiche-Fischel O, Mehra P. Changes in temporomandibular joint dysfunction after orthognathic surgery. J Oral Maxillofac Surg. 2003;61: 655–60; discussion 661. doi: 10.1053/joms.2003.50131 [DOI] [PubMed] [Google Scholar]
- 5.Kobayashi T, Izumi N, Kojima T, Sakagami N, Saito I, Saito C. Progressive condylar resorption after mandibular advancement. Br J Oral Maxillofac Surg. 2012;50: 176–180. doi: 10.1016/j.bjoms.2011.02.006 [DOI] [PubMed] [Google Scholar]
- 6.Hwang SJ, Haers PE, Sailer HF. The role of a posteriorly inclined condylar neck in condylar resorption after orthognathic surgery. J Craniomaxillofac Surg. 2000;28: 85–90. doi: 10.1054/jcms.2000.0129 [DOI] [PubMed] [Google Scholar]
- 7.Roh YC, Shin SH, Kim SS, Sandor GK, Kim YD. Skeletal stability and condylar position related to fixation method following mandibular setback with bilateral sagittal split ramus osteotomy. J Cranio-Maxillofacial Surg. 2014;42: 1958–1963. doi: 10.1016/j.jcms.2014.08.008 [DOI] [PubMed] [Google Scholar]
- 8.Nestel D, Harlim J, Bryant M, Rampersad R, Hunter-Smith D, Spychal B. Surgical education and training in an outer metropolitan hospital: a qualitative study of surgical trainers and trainees. Adv Heal Sci Educ. 2017;22: 639–651. doi: 10.1007/s10459-016-9697-2 [DOI] [PubMed] [Google Scholar]
- 9.Weber RA, Cable CT, Wehbe-Janek H. Learner Perspectives of a Surgical Educators Faculty Development Program Regarding Value and Effectiveness: A Qualitative Study. Plast Reconstr Surg. 2016;137: 1057–1061. doi: 10.1097/01.prs.0000475825.09531.68 [DOI] [PubMed] [Google Scholar]
- 10.Kienle M. Cadaver training in the education of orthognathic surgery. J Oral Maxillofac Surg. 2012;70: e59–e60. [Google Scholar]
- 11.Bénateau H, Chatellier A, Leprovost N, Ghezal S, Compère JF, Veyssière A. Positionnement condylien lors de la chirurgie orthognathique mandibulaire. Revue de Stomatologie, de Chirurgie Maxillo-faciale et de Chirurgie Orale. 2014. pp. 245–249. doi: 10.1016/j.revsto.2014.06.003 [DOI] [PubMed] [Google Scholar]
- 12.Costa F, Robiony M, Toro C, Sembronio S, Polini F, Politi M. Condylar positioning devices for orthognathic surgery: a literature review. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology. 2008. pp. 179–190. doi: 10.1016/j.tripleo.2007.11.027 [DOI] [PubMed] [Google Scholar]
- 13.Ueki K, Moroi A, Sotobori M, Ishihara Y, Marukawa K, Takatsuka S, et al. A hypothesis on the desired postoperative position of the condyle in orthognathic surgery: A review. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2012. pp. 567–576. doi: 10.1016/j.oooo.2011.12.026 [DOI] [PubMed] [Google Scholar]
- 14.Ellis E 3rd. Condylar positioning devices for orthognathic surgery: are they necessary? J Oral Maxillofac Surg. 1994;52: 536–52. doi: 10.1016/B978-1-4557-2698-1.00030–7 [DOI] [PubMed] [Google Scholar]
- 15.Bettega G, Leitner F. Chirurgie orthognathique assistée par ordinateur: Le repositionnement condylien. Revue de Stomatologie, de Chirurgie Maxillo-faciale et de Chirurgie Orale. 2013. pp. 205–210. doi: 10.1016/j.revsto.2013.06.001 [DOI] [PubMed] [Google Scholar]
- 16.Bettega G, Cinquin P, Lebeau J, Raphal B. Computer-assisted orthognathic surgery: Clinical evaluation of a mandibular condyle repositioning system. J Oral Maxillofac Surg. 2002;60: 27–34. doi: 10.1053/joms.2002.29069 [DOI] [PubMed] [Google Scholar]
- 17.Dawson PE. Temporomandibular joint pain-dysfunction problems can be solved. J Prosthet Dent. 1973;29: 100–112. doi: 10.1016/0022-3913(73)90148-0 [DOI] [PubMed] [Google Scholar]
- 18.Surgical THE, Of C, Prognathism M, With R, Of C. Operative Oral Surgery. JAMA J Am Med Assoc. 1948;138: 929–930. doi: 10.1001/jama.1948.02900120071035 [Google Scholar]
- 19.Dal Pont G. Retro-molar osteotomy for correction of prognathism. Minerva Chir. 1959;14: 1138–1141. [PubMed] [Google Scholar]
- 20.Bays RA, Bouloux GF. Complications of orthognathic surgery. Oral and Maxillofacial Surgery Clinics of North America. 2003. pp. 229–242. doi: 10.1016/S1042-3699(02)00098-5 [DOI] [PubMed] [Google Scholar]
- 21.Berlin NL, Tuggle CT, Steinbacher DM. Improved Short-Term Outcomes following Orthognathic Surgery Are Associated with High-Volume Centers. Plast Reconstr Surg. 2016;138: 273e–281e. doi: 10.1097/PRS.0000000000002384 [DOI] [PubMed] [Google Scholar]
- 22.Elfring R, De La Fuente M, Radermacher K. Assessment of optical localizer accuracy for computer aided surgery systems. Comput Aided Surg. 2010;15: 1–12. doi: 10.3109/10929081003647239 [DOI] [PubMed] [Google Scholar]
- 23.Chen X, Xu L, Sun Y, Politis C. A review of computer-aided oral and maxillofacial surgery: planning, simulation and navigation. Expert Rev Med Devices. 2016;13: 1043–1051. doi: 10.1080/17434440.2016.1243054 [DOI] [PubMed] [Google Scholar]
- 24.Lund B, Fors U, Sejersen R, Sallnas E-L, Rosen A. Student perception of two different simulation techniques in oral and maxillofacial surgery undergraduate training. BMC Med Educ. 2011;11: 82 doi: 10.1186/1472-6920-11-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Azarmehr I, Stokbro K, Bell RB, Thygesen T. Surgical Navigation: A Systematic Review of Indications, Treatments, and Outcomes in Oral and Maxillofacial Surgery. Journal of Oral and Maxillofacial Surgery. 2017. pp. 1987–2005. doi: 10.1016/j.joms.2017.01.004 [DOI] [PubMed] [Google Scholar]
- 26.Collyer J. Stereotactic navigation in oral and maxillofacial surgery. Br J Oral Maxillofac Surg. 2010;48: 79–83. doi: 10.1016/j.bjoms.2009.04.037 [DOI] [PubMed] [Google Scholar]
- 27.Mezger U, Jendrewski C, Bartels M. Navigation in surgery. Langenbeck’s Archives of Surgery. 2013. pp. 501–514. doi: 10.1007/s00423-013-1059-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolford LM. Influence of osteotomy design on bilateral mandibular ramus sagittal split osteotomy. J Oral Maxillofac Surg. 2015;73: 1994–2004. doi: 10.1016/j.joms.2015.03.023 [DOI] [PubMed] [Google Scholar]
- 29.Suojanen J, Leikola J, Stoor P. The use of patient-specific implants in orthognathic surgery: A series of 30 mandible sagittal split osteotomy patients. J Cranio-Maxillofacial Surg. 2017;45: 990–994. doi: 10.1016/j.jcms.2017.02.021 [DOI] [PubMed] [Google Scholar]
- 30.Hwang SJ, Haers PE, Seifert B, Sailer HF. Non-surgical risk factors for condylar resorption after orthognathic surgery. J Cranio-Maxillofacial Surg. 2004;32: 103–111. doi: 10.1016/j.jcms.2003.09.007 [DOI] [PubMed] [Google Scholar]
- 31.Chen S, Lei J, Fu KY, Wang X, Yi B. Cephalometric analysis of the facial skeletal morphology of female patients exhibiting skeletal class II deformity with and without temporomandibular joint osteoarthrosis. PLoS One. 2015;10 doi: 10.1371/journal.pone.0139743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ha MH, Kim Y Il, Park SB, Kim SS, Son WS. Cone-beam computed tomographic evaluation of the condylar remodeling occurring after mandibular set-back by bilateral sagittal split ramus osteotomy and rigid fixation. Korean J Orthod. 2013;43: 263–270. doi: 10.4041/kjod.2013.43.6.263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim YI, Jung YH, Cho BH, Kim JR, Kim SS, Son WS, et al. The assessment of the short- and long-term changes in the condylar position following sagittal split ramus osteotomy (SSRO) with rigid fixation. J Oral Rehabil. 2010;37: 262–270. doi: 10.1111/j.1365-2842.2009.02056.x [DOI] [PubMed] [Google Scholar]
- 34.Xiangdong QI, Limin MA, Shizhen Z. The influence of the closing and opening muscle groups of jaw condyle biomechanics after mandible bilateral sagittal split ramus osteotomy. J Cranio-Maxillofacial Surg. 2012;40 doi: 10.1016/j.jcms.2011.07.024 [DOI] [PubMed] [Google Scholar]
- 35.Abdel-Galil K, Ganesan K, Russell J. Bilateral procedures in maxillofacial surgery in the United Kingdom: survey of higher trainees’ performance and experience. Br J Oral Maxillofac Surg. 2009;47: 140–142. doi: 10.1016/j.bjoms.2008.07.189 [DOI] [PubMed] [Google Scholar]
- 36.Biau DJ, Williams SM, Schlup MM, Nizard RS, Porcher R. Quantitative and individualized assessment of the learning curve using LC-CUSUM. Br J Surg. 2008;95: 925–929. doi: 10.1002/bjs.6056 [DOI] [PubMed] [Google Scholar]
- 37.Andersen SAW, Konge L, Cayé-Thomasen P, Sørensen MS. Learning Curves of Virtual Mastoidectomy in Distributed and Massed Practice. JAMA Otolaryngol Neck Surg. 2015; 1 doi: 10.1001/jamaoto.2015.1563 [DOI] [PubMed] [Google Scholar]
- 38.Brunner WC, Korndorffer JR, Sierra R, Massarweh NN, Dunne JB, Yau CL, et al. Laparoscopic virtual reality training: Are 30 repetitions enough? Journal of Surgical Research. 2004. pp. 150–156. doi: 10.1016/j.jss.2004.08.006 [DOI] [PubMed] [Google Scholar]
- 39.Moulton C-AE, Dubrowski A, MacRae H, Graham B, Grober E, Reznick R. Teaching Surgical Skills: What Kind of Practice Makes Perfect? Trans. Meet Am Surg Assoc. 2006;124: 66–75. doi: 10.1097/01.sla.0000234808.85789.6a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shea CH, Lai Q, Black C, Park JH. Spacing practice sessions across days benefits the learning of motor skills. Hum Mov Sci. 2000;19: 737–760. doi: 10.1016/S0167-9457(00)00021-X [Google Scholar]
- 41.Yu H, Cheng J, Cheng AH, Shen SG. Preliminary study of virtual orthognathic surgical simulation and training. J Craniofac Surg. 2011;22: 648–51. doi: 10.1097/SCS.0b013e318207f2e8 [DOI] [PubMed] [Google Scholar]
- 42.Stokbro K, Aagaard E, Torkov P, Bell RB, Thygesen T. Virtual planning in orthognathic surgery. Int J Oral Maxillofac Surg. 2014;43: 957–965. doi: 10.1016/j.ijom.2014.03.011 [DOI] [PubMed] [Google Scholar]
- 43.Zhang N, Liu S, Hu Z, Hu J, Zhu S, Li Y. Accuracy of virtual surgical planning in two-jaw orthognathic surgery: comparison of planned and actual results. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122: 143–151. doi: 10.1016/j.oooo.2016.03.004 [DOI] [PubMed] [Google Scholar]
- 44.Harris MD, Van Sickels JE, Alder M. Factors influencing condylar position after the bilateral sagittal split osteotomy fixed with bicortical screws. J Oral Maxillofac Surg. 1999;57: 650–655. doi: 10.1016/S0278-2391(99)90422-6 [DOI] [PubMed] [Google Scholar]
- 45.Han JJ, Hwang SJ. Three-dimensional analysis of postoperative returning movement of perioperative condylar displacement after bilateral sagittal split ramus osteotomy for mandibular setback with different fixation methods. J Cranio-Maxillofacial Surg. 2015;43: 1918–1925. doi: 10.1016/j.jcms.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 46.Ellis E, Throckmorton GS, Sinn DP. Bite forces before and after surgical correction of mandibular prognathism. J Oral Maxillofac Surg. 1996;54: 176–181. doi: 10.1016/S0278-2391(96)90443-7 [DOI] [PubMed] [Google Scholar]
- 47.Dicker GJ, Tuijt M, Koolstra JH, Van Schijndel RA, Castelijns JA, Tuinzing DB. Static and dynamic loading of mandibular condyles and their positional changes after bilateral sagittal split advancement osteotomies. Int J Oral Maxillofac Surg. 2012;41: 1131–1136. doi: 10.1016/j.ijom.2012.03.013 [DOI] [PubMed] [Google Scholar]
- 48.Dicker GJ, Castelijns JA, Tuinzing DB, Stoelinga PJW. Do the changes in muscle mass, muscle direction, and rotations of the condyles that occur after sagittal split advancement osteotomies play a role in the aetiology of progressive condylar resorption? Int J Oral Maxillofac Surg. 2015;44: 627–631. doi: 10.1016/j.ijom.2015.01.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(MP4)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.