Abstract
Background
As length of stay decreases for total joint arthroplasty, much of the patient preparation and teaching previously done in the hospital must be performed before surgery. However, the most effective form of preparation is unknown. This randomized trial evaluated the effect of a one-time, one-on-one preoperative physical therapy education session coupled with a web-based microsite (preopPTEd) on patients’ readiness to discharge from physical therapy (PT), length of hospital stay, and patient-reported functional outcomes after total joint arthroplasty.
Questions/purposes
Was this one-on-one preoperative PT education session coupled with a web- based microsite associated with (1) earlier achievement of readiness to discharge from PT; (2) a reduced hospital length of stay; and (3) improved WOMAC scores 4 to 6 weeks after surgery?
Methods
Between February and June 2015, 126 typical arthroplasty patients underwent unilateral TKA or THA. As per our institution’s current guidelines, all patients attended a preoperative group education class taught by a multidisciplinary team comprising a nurse educator, social worker, and physical therapist. Patients were then randomized into two groups. One group (control; n = 63) received no further education after the group education class, whereas the intervention group (experimental; n = 63) received preopPTEd. The preopPTEd consisted of a one-time, one-on-one session with a physical therapist to learn and practice postoperative precautions, exercises, bed mobility, and ambulation with and negotiation of stairs. After this session, all patients in the preopPTEd group were given access to a lateralized, joint-specific microsite that provided detailed information regarding exercises, transfers, ambulation, and activities of daily living through videos, pictures, and text. Outcome measures assessed included readiness to discharge from PT, which was calculated by adding the number of postoperative inpatient PT visits patients had to meet PT milestones. Hospital length of stay (LOS) was assessed for hospital discharge criteria and 6-week WOMAC scores were gathered by study personnel. At our institution, to meet PT milestones for hospital discharge criteria, patients have to be able to (1) independently transfer in and out of bed, a chair, and a toilet seat; (2) independently ambulate approximately 150 feet; (3) independently negotiate stairs; and (4) be independent with a home exercise program and activities of daily living. Complete followup was available on 100% of control group patients and 100% patients in the intervention group for all three outcome measures (control and intervention of 63, respectively).
Results
The preopPTEd group had fewer postoperative inpatient PT visits (mean, 3.3; 95% confidence interval [CI], 3.0-3.6 versus 4.4; 95% CI, 4.1-4.7; p < 0.001) and achieved readiness to discharge from PT faster (mean, 1.6 days; 95% CI, 1.2-1.9 days versus 2.7 days; 95% CI, 2.4-3.0; p < 0.001) than the control group. There was no difference in hospital LOS between the preopPTEd group and the control group (2.4 days; 95% CI, 2.1-2.6; p = 0.082 versus 2.6 days; 95% CI, 2.4-2.8; p = 0.082). There were no clinically relevant differences in 6-week WOMAC scores between the two groups.
Conclusions
Although this protocol resulted in improved readiness to discharge from PT, there was no effect on LOS or WOMAC scores at 6 weeks. Preoperative PT was successful in improving one of the contributors to LOS and by itself is insufficient to make a difference in LOS. This study highlights the need for improvement in other aspects of care to improve LOS.
Level of Evidence
Level II, therapeutic study.
Introduction
Over the past 20 years, hospital length of stay (LOS) after total joint arthroplasty (TJA) has steadily decreased to an average of 2 to 4 days [5, 10, 11, 13, 27]. Today, some investigators even advocate for outpatient TJA [1, 12]. The decrease in LOS has largely been made possible by improved surgical techniques, better pain management, early mobilization, modifications to rehabilitation protocols, and pathway-directed care [1]. Many ambulatory or short-term LOS pathways rely on preoperative education and multidisciplinary care as crucial components to prepare patients for surgery [1, 13, 23].
Several authors have reported that preoperative education reduces preoperative anxiety and improves postoperative satisfaction and outcomes [2, 3, 18, 23]. However, a recent Cochrane review [16] noted only low-quality evidence in support of preoperative education. Despite this, many providers still utilize preoperative education as a result of the relative absence of associated adverse effects [16-18].
Various methods have been used for preoperative education including booklets, videotapes, webinars, and, most commonly, group classes. Although group classes may reduce LOS [22, 23], others have reported that up to 77% of patients can have unfulfilled knowledge expectations with respect to their postoperative function with similar protocols [8]. To make patients’ expectations more realistic and improve preoperative fitness, some institutions have encouraged patients to meet with a physical therapist before surgery for “prehabilitation” [4, 6, 20, 24, 25]. Although the majority of studies have found insufficient evidence to support preoperative physical therapy (PT) from a strength building perspective [7, 26], little is known regarding the effectiveness of a one-time educational PT session on postoperative recovery. Because physical therapists often provide teaching to patients undergoing arthroplasty postoperatively, we hypothesized that a preoperative education session may lead to improved postoperative recovery.
Therefore, we asked: Was this one-on-one preoperative PT education session coupled with a web-based microsite associated with (1) earlier achievement of readiness to discharge from PT; (2) a reduced hospital LOS; and (3) improved WOMAC scores 4 to 6 weeks after surgery?
Patients and Methods
Between February and October 2015, a randomized controlled trial was designed to evaluate the efficacy of a one-on-one preoperative PT education protocol on postoperative function and hospital LOS. This study was approved by our institutional review board (IRB# 2015-306) and was also posted on ClinicalTrials.gov (#NCT02872337). A priori, it was determined that patients would be eligible for participation if they represented a typical patient undergoing unilateral arthroplasty at our specialized orthopaedic institution. Therefore, we included patients who were scheduled for unilateral TJA (THA or TKA), between 18 and 85 years old, able to independently ambulate a half a block or more with or without an assistive device, able to independently perform nonreciprocal stairs with or without assistive devices, and planned to be discharged home after surgery. Overall, 141 patients were approached and consented to participate in the study. A priori, it was determined that patients who did not undergo scheduled surgery, underwent a procedure other than primary TJA, or were discharged to inpatient rehabilitation centers would be eliminated from subsequent analyses (Fig. 1). This determination was based on an effort to eliminate bias associated with LOS requirements, especially those associated with inpatient rehabilitation centers [21]. Based on these a priori criteria, 126 patients (n = 63 TKA; n = 63 THA) were included in subsequent analyses. The mean age for all patients in the study was 61 ± 9 years (range, 37-85 years) with a mean body mass index (BMI) of 29 ± 6 kg/m2 (range, 17-48 kg/m2) (Table 1). Eighty (64%) patients were women and 46 (37%) were men.
Fig. 1.
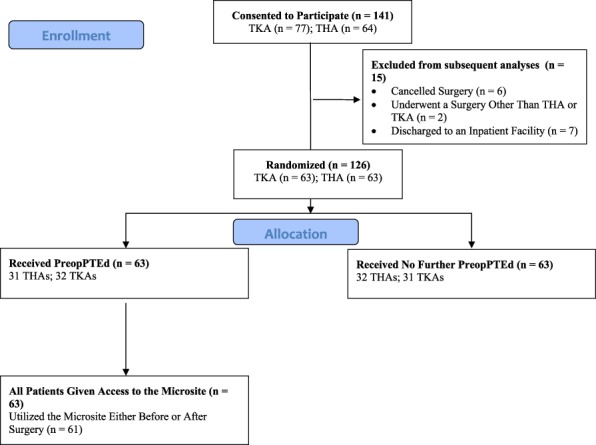
A patient flowchart shows study inclusion and exclusion criteria.
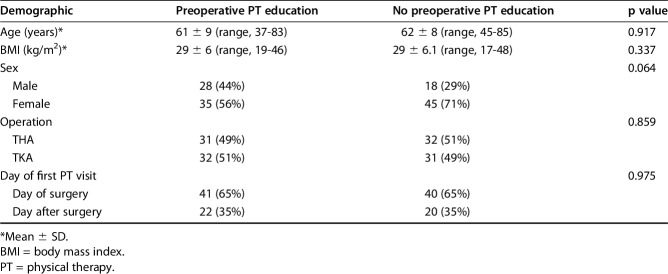
Table 1.
Demographics
There were no differences between the preoperative PT education (preopPTEd) group and the control group with respect to operation type, age, BMI, sex, or day on which postoperative PT was started (Table 1). When stratified based on operation type, there were no differences in age, BMI, sex distribution, or day on which postoperative PT was started for those who underwent TKA. In the THA group, there were no differences in age, BMI, surgical approach, or day on which postoperative PT was initiated. More men (15 of 31 [48%]) were randomized into the preoperative education group than into the control group (six of 32 [19%]; p = 0.013). Regardless of cohort, all patients in the study attended the preoperative group education class and received a surgery-specific information booklet as per the institution’s current guidelines for patient care. Patients were approached to participate in the study either at the time of their presurgical office consultation or after the group education class. Patients were randomly assigned to two groups through a predetermined blocked randomization schedule, which was generated by a blinded statistician (JCBK) using SAS 9.3 (Cary, NC, USA). The schedule was determined based on the number of participating surgeons (n = 14) based on anticipated patient volume. One cohort (control group) received no further preoperative education besides the group education class as per our institution’s current guidelines for patient care. The other cohort (experimental) underwent the preoperative education class and preopPTEd session with a physical therapist. There was no difference between participating surgeons regarding patient expectations or use of other educational modalities besides the preoperative group education class (control) and preopPTEd (intervention).
The preopPTEd session took place before surgery (approximately 2 weeks) on a predetermined day that consisted of a preoperative medical evaluation and the all-inclusive preoperative group class. The preopPTEd session typically lasted approximately 20 to 30 minutes. All patients were seen by the same physical therapist. The focus of the preopPTEd session was attention to topics such as preoperative preparation, function during the acute inpatient hospital stay, discharge instructions, negotiating activities of daily living after surgery, goal setting, and aligning patients’ expectations regarding upcoming surgery and postsurgical recovery. Patients had an opportunity to learn postsurgical precautions; practice transfers in and out of bed, a chair, a toilet seat, or car; ambulation with and without assistive devices; and negotiation of stairs before surgery, which they would otherwise learn postoperatively. Patient specific surgical and postsurgical rehabilitation-related recovery concerns were addressed. The main difference between a group class and the preopPTEd was that the session gave the patient an opportunity to practice mobility and assistive devices before the surgery, prepare and modify the home environment if needed, discuss concerns and questions in a private environment, and set goals with the therapist. The group class is for general didactics and does not allow the opportunity to practice mobility and personalized care based on and within boundaries of standard institutional patient care guidelines.
After the session, all patients in the preopPTEd (intervention) group were given access to a rehabilitation focused microsite (www.hss.edu/rpthr, www.hss.edu/lpthr, www.hss.edu/rathr, www.hss.edu/lathr, www.hss.edu/rtkr, www.hss.edu/ltkr) that consists of educational information in the form of videos and pictures (see Appendix, Supplemental Digital Content 1). Unlike educational booklets given at the group preoperative education class (control group), microsite access was limited to specific surgery (ie, TKA versus THA), surgical approach (ie, direct anterior versus posterior THA), and lateralization (ie, right versus left). Content of the microsites included pertinent information regarding the rehabilitation recovery process in various formats including photographs and videos. Microsites have the ability to be scaled to mobile phone screens. Thus, microsites reinforced information presented during the one-on-one session with the physical therapist and gave the patient an opportunity to view it as many times before and after surgery as needed at his or her own convenience. All patients reported utilizing the microsite at one point in the study period with 96% reportedly utilizing it preoperatively and 76% reportedly using it postoperatively.
The operating surgeon and inpatient therapists were blinded to the assigned group unless otherwise alerted by the patient. Postoperatively all patients received a uniform PT protocol with one-on-one PT two times a day and a third session with a mobility technician for the duration of the inpatient stay. Inpatient PT was started either on the day of or the day after surgery.
Function during the inpatient stay was measured utilizing hospital metrics based on the institution’s current guidelines for patient care including readiness to discharge from PT and hospital LOS. At our institution, readiness to discharge from PT is defined as the ability to (1) independently transfer in and out of bed, a chair, and a toilet seat; (2) independently ambulate approximately 150 feet; (3) independently negotiate stairs; and (4) be independent with a home exercise program and activities of daily living. Readiness to discharge from PT and hospital LOS were obtained from hospital records by a research assistant (PBW).
Postoperative pain, stiffness, and function were assessed using WOMAC scores administered both before and after surgery (approximately 4-6 weeks). WOMAC pain (0-20, where 0 is no pain), WOMAC stiffness (0-8, where 0 is no stiffness), and WOMAC function (0-68, where 0 is no difficulty in function) subscores as well as the total WOMAC score (0-96, where 0 is best and 96 is worst) were recorded. WOMAC scores were collected by the principal investigator (RS) before surgery and by a research assistant (PBW) and physical therapy assistant (PP) after surgery. Preoperatively, there were no differences in WOMAC subscores or total WOMAC scores (Table 2). In addition to WOMAC, patients answered a single question regarding utilization of the microsites (yes or no) after surgery (approximately 4-6 weeks). In the group randomized to the preopPTEd session (n = 63), 61 (97%) reported utilizing the microsite. Of those, 44 (72%) utilized the microsite both before and after surgery, 15 (25%) only before surgery, and two (3%) only after surgery.
Table 2.
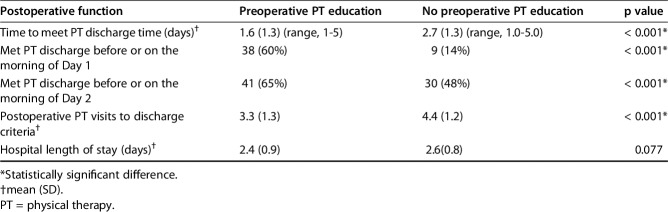
Postoperative function during the inpatient stay
Statistical Analysis
An a priori power analysis was performed to determine the number of patients necessary for the study. A previous study at our institution utilizing a similar postoperative protocol revealed that patients undergoing joint arthroplasty require five inpatient postoperative PT visits to meet PT discharge criteria [9]. Using a minimally clinically important difference of one inpatient postoperative PT visit, we hypothesized that there would be no difference in the number of PT visits patients had to meet PT discharge between our two groups. At a level of significance of 0.05, a total of 126 patients undergoing joint arthroplasty was required to achieve a power of 0.8. Accounting for a 20% dropout rate, we aimed to enroll 141 patients in this study.
Descriptive statistics are presented as means and 95% confidence intervals (additional statistics are also provided) for continuous variables and frequencies and percentages for categorical variables. Overall differences in categorical variables were assessed with chi-square and Fisher's exact tests, whereas differences in continuous variables between groups were assessed with independent-sample t-tests and Mann-Whitney U tests. Additionally, subgroup analyses were performed to analyze the effects of preopPTEd on patients undergoing THA and TKA separately. All analyses were performed with SAS 9.3 with a level of significance of 0.05.
Results
Readiness to Discharge From PT
Patients who received preopPTEd had a mean of 3.3 inpatient postoperative PT visits (95% confidence interval [CI], 3.0-3.6; p < 0.001) and a mean of 1.6 days (95% CI, 1.2-1.9 days) (Table 3). Thirty-eight (60%) patients met the readiness to discharge from PT criteria on the first postoperative day and 41 (65%) met readiness to discharge by the second postoperative day. Patients in the control group required 4.4 inpatient postoperative PT visits (95% CI, 4.1-4.7; p < 0.001) and 2.7 days (95% CI, 2.4-3.0) to meet the readiness to discharge from PT criteria. Nine (14%) patients were able to meet the readiness to discharge from PT criteria on the first postoperative day and 30 (48%) patients were able to meet readiness to discharge from PT criteria by the second postoperative day. More patients in the intervention group were able to meet PT discharge criteria on the first postoperative day and by the second postoperative day (p < 0.001 and p < 0.001, respectively).
Table 3.
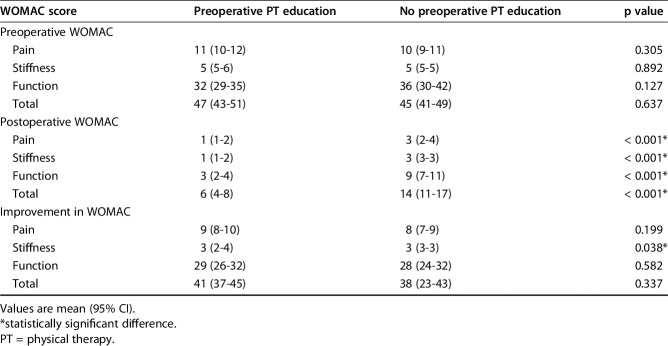
Pain, stiffness, and function WOMAC scores
When stratified based on procedure, the preopPTEd TKA group had a mean of 3.4 (95% CI, 3.0-3.9) PT visits and met PT discharge criteria at a mean of 1.8 days (95% CI, 1.4-2.3). The control group had a mean of 4.6 (95% CI, 4.2-5.0) PT visits and met PT discharge criteria in 2.9 (95% CI, 2.5-3.4) days. The preopPTEd TKA group had fewer PT visits and met PT readiness to discharge faster than the control group (p < 0.001 and p < 0.001, respectively). The preopPTEd THA group had a mean of 3.1 (95% CI, 2.6-3.6) PT visits and 1.3 (95% CI, 0.8-1.8) days to meet the readiness to discharge criteria. The control group had 4.1 PT visits (95% CI, 3.6-4.6) and 2.3 (95% CI, 2.0-2.9) days to meet the PT readiness to discharge criteria. The preopPTEd group had fewer PT visits and time to meet readiness to discharge (p = 0.001 and p < 0.001, respectively).
Hospital Length of Stay
The mean hospital LOS was 2.6 days (95% CI, 2.4-2.8) and 2.4 days (95% CI, 2.1-2.6; p = 0.077) for the control and preopPTEd groups, respectively. There were no differences between the groups in terms of length of hospital stay (p = 0.077). When stratified based on procedure, the preopPTEd TKA group had a hospital LOS of 2.7 days (95% CI, 2.4-3.0) and the control group had a LOS of 3.0 days (95% CI, 2.7-3.3). There was no difference in the mean hospital LOS for patients undergoing TKA (p = 0.161). With respect to the THA cohort, the preopPTEd group had a LOS of 2.0 (95% CI, 1.7-2.3) and the control group had a LOS of 2.3 days (95% CI, 2.1-2.6). There was no difference in hospital LOS for patients undergoing THA (p = 0.150).
WOMAC Scores
By 6 weeks after surgery, the preopPTEd group had a mean postoperative WOMAC pain score of 1 (95% CI, 1-2), stiffness score of 1 (95% CI, 1-2), function score of 3 (95% CI, 3-4), and total score of 6 (95% CI, 4-8) (Table 2). The control group had a mean postoperative pain score of 3 (95% CI, 2-4), stiffness score of 3 (95% CI, 3-3), function score of 9 (95% CI, 7-11), and total score of 14 (95% CI, 11-17). The preopPTEd group had significantly improved postoperative pain (p < 0.001), stiffness (p < 0.001), and function (p < 0.001) subscores as well as total scores (p < 0.001). With regard to 6-week improvements in WOMAC scores, the preopPTEd group had improvements in a mean WOMAC pain score of 9 (95% CI, 8-10), stiffness score of 3 (95% CI, 2-4), function score of 29 (95% CI, 26-32), and total score of 41 (95% CI, 37-45). The control group had a 6-week improvement in mean WOMAC pain score of 8 (95% CI, 7-9), stiffness score of 3 (95% CI, 3-3), function score of 28 (95% CI, 24-32), and total score of 38 (95% CI, 23-43). The preopPTEd group had significantly better improvement scores (p = 0.038); however, there were no differences in pain, function, or total scores (p = 0.199, p = 0.582, and p = 0.337, respectively).
Discussion
Rapid early mobilization and short inpatient hospitalization have become increasingly common in the care of patients undergoing TJA [1, 12]. As a result, numerous multidisciplinary protocols and pathways are currently used to improve patient function and reduce LOS associated with TJA [5, 10, 13, 27] including preoperative patient education classes. Although many institutions utilize group classes for preoperative education, it has been reported that up to 77% of patients have unfulfilled knowledge expectations with respect to their postoperative function [8]. There is limited literature to support or oppose these measures. Therefore, we asked whether a structured preoperative PT education session would result in more rapid attainment of therapy goals, shorter LOS, and better early function. We found that patients achieved PT goals for home discharge faster with somewhat better early function, but found no effect on LOS or 4- to 6-week function.
This study is not without limitations. First, this study took place at one institution, and therefore the results should be generalized to other institutions with caution. Furthermore, institutions with limited resources may have difficulty adopting a similar protocol despite the negligible associated costs. Second, as a result of the sample size, there was limited power for subgroup analyses within the THA and TKA subgroups. However, we did discover that the findings with respect to inpatient postoperative function were the same in the subgroups. We did find a greater distribution of males who received preopPTEd in the THA subgroup than those who did not. The authors believe this was the result of random chance during the consenting process. Third, the results are limited to a study population that represented the typical patient undergoing arthroplasty at our institution, but may not represent patients undergoing arthroplasty at other institutions. This included English-speaking patients scheduled for either unilateral primary TKA or THA who were able to independently ambulate a New York city block (264 feet x 900 feet) and planned to go home after surgery and were approached to participate in the study. Thus, results of this study may not apply to non-English-speaking patients, patients undergoing revision or bilateral TJA, or patients with severe mobility limitations. Fourth, the use of the microsites is highly dependent on the ability of the user to utilize and have access to the technology. However, we found that all patients given access to the microsites (100%) utilized the platform at some point throughout the process. Fifth, in an effort to eliminate the bias associated with discharge disposition and the 3-day rule for inpatient rehabilitation facilities, patients discharged to inpatient rehabilitation facilities were not analyzed [21]. A followup study is warranted to determine the effectiveness of this protocol on this population.
In this study, we found that meeting with a physical therapist preoperatively effectively reduced the number of PT visits a patient received to meet our institution’s readiness to discharge from PT criteria. We believe that this protocol effectively shifted the postoperative learning curve to earlier in the recovery process ultimately allowing patients to recover functionality approximately 1 day earlier than otherwise. This PT discharge timing was not only faster than our control group (2.7 days), but also was faster than a previous study at our institution (approximately 2.2-2.5 days) [9]. This protocol was intended to improve readiness to PT discharge timing and align patients’ expectations regarding rehabilitation recovery. Despite all the limitations, there is meaningful clinical importance of preopPTEd as it resulted in one or two postoperative PT visits in the hospital. Although there was an improvement in the readiness to meet PT discharge criteria (approximately 1 day), we found that hospital LOS did not significantly improve with the use of preopPTEd.
With regard to the 4- to 6-week WOMAC scores, we found no clinically relevant differences in WOMAC subscores (pain, function, and stiffness) or total scores. This is similar to what was found in a previous study at our institution that used a similar postoperative PT protocol [9]. Recent meta-analyses appear to also agree that the literature is inconsistent with regard to the use of “prehab” on WOMAC scores [20, 23]. Silkman Baker and McKeon [20] evaluated four studies and found inconsistent findings with respect to “prehab” and WOMAC scores. Peer et al. [17] found a moderate correlation between resistance training and WOMAC scores, but their meta-analysis only included two studies on that topic. Although likely not clinically relevant, we did find that all of the postoperative scores were significantly improved compared with our control group. This finding and the slight correlations found in the meta-analyses may demonstrate that “prehab” muscle strengthening or “prehab” as an educational tool may better align patient and physician expectations.
To complement the one-on-one preopPTEd session, we also gave patients access to a rehabilitation-focused microsite. The purpose of the microsites was to supplement written material and improve memory retention [19]. In recent times, there have been few studies that have documented the usefulness of the Internet as a means of tracking patients for followup [14, 15] and only one study that has shown a beneficial effect of the use of telecommunications technology in providing patient preoperative health education [24]. To our knowledge, there have been no studies documenting the usefulness of a rehabilitation-specific web-based microsite as a means of preoperative education. Therefore, it is difficult to determine which benefits in this study are attributable to the preopPTEd session or the microsites. However, we found that every patient with access to the microsite used the platform at least once through the surgical process. Also, all patients said they would recommend the microsites for all patients undergoing TJA. The authors believe this may highlight how associative, complementary technologies can be used to aid patient education. Further studies should be performed to determine the effectiveness of different technologies (mobile versus web) in this setting.
In conclusion, we found that the use of a one-time, one-on-one preoperative PT session protocol with a supplemental microsite was effective at reducing the number of postoperative PT visits and time for readiness to discharge from PT. However, we found that it did not reduce LOS and had no effect on outcomes at 4 to 6 weeks. Allocating an educational PT visit preoperatively may be effective in organizations that incorporate postoperative rehabilitation milestones for their discharge criteria as described in this study. PreopPTEd might also be useful in reducing LOS when combined with a multipronged effort among surgeons, medical physicians, and case managers to facilitate hospital discharge. That said, because this study was tested in a well-funded specialty hospital, we recommend caution when implementing this protocol at smaller, nonspecialized hospitals with limited resources. Further studies should be performed to determine the efficacy of similar PT protocols on other procedures.
Supplementary Material
Acknowledgments
We thank Peter Panagos for helping with data collection; and JeMeCioppa-Mosca, Carol Page, Charles Fisher, Dana Gallagher, Mathew Titmuss, Julie Pelaez, Danielle Edwards, Julia Doty, Ometa Borne-Forde, and Stephen Bartalini for assisting with microsite development.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Hip and Knee Surgeons Writing Committee: Michael M. Alexiades MD, Friedrich Boettner MD, Mathias P. Bostrom MD, Michael B. Cross MD, Mark P. Figgie MD, Steven B. Haas MD, Seth A. Jerabek MD, David J. Mayman MD, Danyal Nawabi MD, Douglas E. Padgett MD, Amar S. Ranawat MD, Thomas P. Sculco MD, Edwin P. Su MD, Geoffrey H. Westrich MD, Russell E. Windsor MD.
References
- 1.Argensen JN, Husted H, Lombardi A, Jr, Booth RE, Thienpont E. Global Forum: an international perspective on outpatient surgical procedures for adult hip and knee reconstruction. J Bone Joint Surg Am. 2016;98:e55. [DOI] [PubMed] [Google Scholar]
- 2.Baker PN, van der Meulen JH, Lewsey J, Gregg PJ. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br. 2007;89:893–900. [DOI] [PubMed] [Google Scholar]
- 3.Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247. [DOI] [PubMed] [Google Scholar]
- 4.Carli F, Zavorsky GS. Optimizing functional exercise capacity in the elderly surgical population. Curr Opin Clin Nutr Metab Care. 2005;8:23–32. [DOI] [PubMed] [Google Scholar]
- 5.denHartog YM, Mathijssen NM, Hannink G, Vehmeijer SB. Which patient characteristics influence length of hospital stay after primary total hip arthroplasty in a ‘fast-track’ setting? Bone Joint J. 2015;97:19–23. [DOI] [PubMed] [Google Scholar]
- 6.Ditmyer MM, Topp R, Pifer M. Prehabilitation in preparation for orthopaedic surgery. Orthop Nurs. 2002;21:43–51. [DOI] [PubMed] [Google Scholar]
- 7.Hoogeboom TJ, Oosting E, Vriezekolk JE, Veenhof C, Siemonsma PC, de Bie RA, van den Ende1 CHM, van Meeteren NLU. Therapeutic validity and effectiveness of preoperative exercise on functional recovery after joint replacement: a systematic review and meta-analysis. PLoS One. 2012;7:e38031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johansson Stark A, Ingadottir B, Salanterä S, Sigurdardottir AK, Valkeapää K, Bachrach-Lindström M, Unosson M. Fulfillment of knowledge expectations and emotional state among people undergoing hip replacement: a multi-national survey. Int J Nurs Stud. 2014;51:1491–1499. [DOI] [PubMed] [Google Scholar]
- 9.Joshi R, White PB, Murray-Weir M, Alexiades MM, Sculco TP, Ranawat AS. Prospective randomized trial of the efficacy of continuous passive motion post total knee arthroplasty: experience of the Hospital for Special Surgery. J Arthroplasty. 2015;30:2364–2369. [DOI] [PubMed] [Google Scholar]
- 10.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630–641. [DOI] [PubMed] [Google Scholar]
- 11.Keswani A, Beck C, Meier KM, Fields A, Bronson MJ, Moucha CS. Day of surgery and surgical start time affect hospital length of stay after total hip arthroplasty. J Arthroplasty. 2016;31:2426–2431. [DOI] [PubMed] [Google Scholar]
- 12.Lombardi AV, Jr, Barrington JW, Berend KR, Berend ME, Dorr LD, Hamilton W, Hurst JM, Morris MJ, Scuderi GR. Outpatient arthroplasty is here now. Instr Course Lect. 2016;65:531–546. [PubMed] [Google Scholar]
- 13.Maempel JF, Clement ND, Ballantyne JA, Dunstan E. Enhanced recovery programs after total hip arthroplasty can result in reduced length of hospital stay without compromising functional outcome. Bone Joint J. 2016;98:475–482. [DOI] [PubMed] [Google Scholar]
- 14.Marsh J, Bryant D, MacDonald SJ, Naudie D, Remtulla A, McCalden R, Howard J, Bourne R, McAuley J. Are patients satisfied with web-based follow-up after total joint arthroplasty. Clin Orthop Relat Res. 2014;472:1972–1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marsh J, Hoch JS, Bryant D, MacDonald SJ, Naudie D, McCalden R, Howard J, Bourne R, McAuley J. Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J Bone Joint Surg Am. 2014;96:1910–1916. [DOI] [PubMed] [Google Scholar]
- 16.McDonald S, Page MJ, Beringer K, Wasiak J, Sprowson A. Preoperative education for hip or knee replacement. Cochrane Database Syst Rev. 2014. May 13. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peer MA, Rush R, Gallacher PD, Gleeson N. Pre-surgery exercise and post-operative physical function of people undergoing knee replacement surgery: a systematic review and meta-analysis of randomized controlled trials. J Rehabil Med. 2017;49:304–315. [DOI] [PubMed] [Google Scholar]
- 18.Rooks DS, Huang J, Bierbaum BE, Bolus S, Rubano J, Connolly CE, Alpert S, Iversen MD, Katz JN. Effect of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis Rheum. 2006;55:700–708. [DOI] [PubMed] [Google Scholar]
- 19.Sandberg EH, Sharma R, Sandberg WS. Deficits in retention for verbally presented medical information. Anesthesiology. 2012;117:772–779. [DOI] [PubMed] [Google Scholar]
- 20.Silkman Baker C, McKeon JM. Does preoperative rehabilitation improve patient-based outcomes in persons who have undergone total knee arthroplasty? A systematic review. PM R. 2012;4:756–767. [DOI] [PubMed] [Google Scholar]
- 21.Sisko ZW, Lu M, Puri L. The 72-hour Medicare mandate after total joint arthroplasty: is this medically necessary? J Arthroplasty. 2016;31:947–951. [DOI] [PubMed] [Google Scholar]
- 22.Soever LJ, Mackay C, Saryeddine T, Davis AM, Flannery JF, Jaglal SB, Levy C, Mahomed N. Educational needs of patients undergoing total joint arthroplasty. Physiother Can. 2010;62:206–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tait MA, Dredge C, Barnes CL. Preoperative patient education for hip and knee arthroplasty: financial benefit? J Surg Orthop Adv. 2015;24:246–251. [PubMed] [Google Scholar]
- 24.Thomas K, Buron D, Withrow L, Adkisson B. Impact of a preoperative education program via interactive telehealth network for rural patients having total joint replacement. Orthop Nurs. 2004;23:39–44. [DOI] [PubMed] [Google Scholar]
- 25.Topp R, Ditmyer M, King K, Doherty K, Hornyak J., III The effect of bed rest and potential of prehabilitation on patients in the intensive care unit. AACN Clin Issues. 2002;13:263–276. [DOI] [PubMed] [Google Scholar]
- 26.Valkenet K, van de Port IG, Dronkers JJ, de Vries WR, Lindeman E, Backx FJ. The effects of preoperative exercise therapy on postoperative outcome: a systematic review. Clin Rehabil. 2011;25:99–111. [DOI] [PubMed] [Google Scholar]
- 27.Weingarten S, Riedinger MS, Sandhu M, Bowers C, Ellrodt AG, Nunn C, Hobson P, Greengold N. Can practice guidelines safely reduce hospital length of stay? Results from a multi-center interventional study. Am J Med. 1998;105:33–40. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.