Abstract
Metacarpal fractures constitute 7.8% of the upper extremity fractures. The common treatments remain nonsurgical procedure, but high-demanding patients or unstable fractures require fixation with Kirschner wire (K-wires), plate, and screws. However, these approaches may cause scarring and adhesion with poor functional results. From 2014 to 2015, the authors used an intramedullary headless screw to treat 25 patients (24 men, 1 woman) with metacarpal bones fractures (20 V, 3 IV, 1 III, and 1 II). The fractures patterns were 23 fractures of distal third of metacarpal bone (16 oblique, 5 comminute configurations, and 2 transverse), 1 fracture of the base of the II metacarpal bone. One case presented a multiple metacarpal and phalangeal facture associated. The authors used wide-awake anesthesia (bupivacaine-epinephrine 1:100,000) and intramedullary titanium headless screw fixation percutaneously inserted (CCS Medartis and HCS Synthes 3 mm of diameter). No open reduction was needed. Early active mobilization started with a buddy strapping soon after surgery (0–3 days). The authors followed all patients until satisfactory function was achieved (4–6 weeks) and recorded the time till return to work. All fracture healed with less than 5 degrees of rotational or axial deformities. All patients return to work within 2.38 weeks after surgery (0.5–6 weeks). No cases of complex regional pain syndrome (CRPS), tendon lesions, nerve injuries, infection, hardware protruding, or mobilization were reported. Intramedullary screw fixation with wide-awake anesthesia for transverse, oblique, and select comminuted fractures treatment metacarpal fractures represent a reliable option to early active mobilization recovery and a quick return to the work and ordinary activities.
Keywords: metacarpal factures, intramedullary fixation, headless screws, wide-awake anesthesia
Introduction
The most common treatments of metacarpal fractures remain nonsurgical procedures, but high-demanding patients or unstable fractures require fixation with Kirschner wires (K-wires), plate, and screws. All these procedures may cause scarring and adhesion arising from the implant itself or from the insufficient restoration of skeletal stability.
Studies showed good clinical results with retrograde intramedullary fixation of metacarpal and proximal phalanx fractures, using cannulated headless screws. 1 2 This technique may be performed by percutaneous procedure or, if necessary, with minimal exposure and provides primary stability for early active mobilization, minimizing the risk of adhesions.
The aim of this study was to report the outcomes of 25 patients treated with intramedullary headless compression screw and wide-awake anesthesia for unstable or secondary displaced fractures of the metacarpals bones.
Patients and Methods
From March 2014 to December 2015, 25 consecutive extra-articular unstable fractures of the metacarpal in 24 adult patients were treated and reviewed retrospectively (level of evidence IV). Fourteen fractures were initially treated conservatively, but displacement took place after first radiologic control (1 week later). The other 10 fractures were judged to be unstable from the morphology of the fracture. The patients included 24 men and 1 woman with a mean age of 32.8 years (range: 19–59). Nineteen fractures were to the dominant hand and six to the nondominant hand. There were no open or pathologic fractures. A total of 24 patients had an isolated fracture in a single ray. One patient had concomitant fractures in multiple digits (metacarpal and phalanx). There were 20 fractures at the distal third of fifth, 3 of the fourth, 1 of the second, and 1 of the third metacarpals. The mean time from injury to surgical intervention was 5.6 days (range: 1–13). Eight patients (five white-collars and three soldiers) had a health care daily benefit, whereas the others were not covered for medical expenses, as freelancer and student had a high functional demand (cyclists, musician, etc).
The procedure was performed using wide-awake anesthesia without tourniquet in all cases except one (polytrauma). The patients were anesthetized using an infiltration with 0.5% bupivacaine and epinephrine (1:100,000) (20 mL), injected 30 minutes before surgery around the dorsal aspect of the ray, from the metacarpal head to metacarpal base 3 ( Fig. 1 ). In all patients, the diameter of the intramedullary canal, measured on the lateral radiograph, was bigger than 30 mm. Only one patient with the fractures of second metacarpal bone was operated upon with anterograde screw insertion.
Fig. 1.
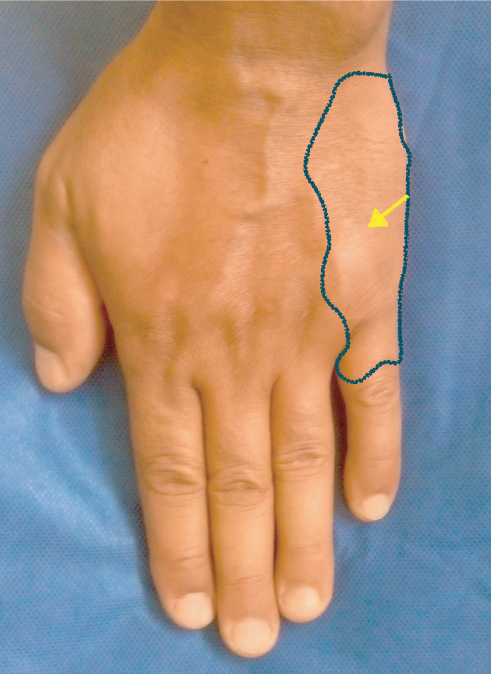
The dorsal metacarpal area involved by anesthesia.
Fractures were reduced using Jahss’ maneuver under fluoroscopy, and if there was a rotational deformity (using a full active finger flexion after K-wire temporary fixation to the cortical of the metacarpal base), it was corrected by handling of the finger ( Fig. 2 ).
Fig. 2.

The unstable multifrag mentary fracture of the meta carpal neck.
All fingers were operated upon using an intrarticular retrograde technique, inserting the K-guidewire and screw through the dorsoradial/ulnar aspect of the head of the metacarpal, dependent on the configuration of the fractures with the metacarpophalangeal (MCP) joint in approximately 80 to 90 degrees of flexion. Once the guidewire was in the appropriate position and a satisfactory reduction was obtained, a 2-mm skin incision was performed and the screw was inserted over the guide without predrilling ( Fig. 3 ). After, a 3-mm diameter, self-tapping cannulated headless screw was used (CCS Medartis [Basel, Switzerland] in 8 cases and HCS Synthes [Oberdorf, Switzerland] in 17 patients).
Fig. 3.

The percutaneous introduction of cannulated screw, after close reduction.
In cases of comminute fracture pattern, to decrease the risk collapse of the fragments during screw insertion, the guidewire was put bedside another K-wire. The screw used was as long as possible to avoid excessive forces and secondary displacement of the fractures. The length of the screw was calculated preoperatively and verified under fluoroscopy before insertion. Care was taken to avoid the proximally protrusion of the base of screw. After the fixation, alignment and rotation were controlled asking an immediate patients’ active motion. Later, the metacarpal and digit were dressed with buddy strapping to the adjacent fingers. All patients were encouraged to actively mobilize the involved finger immediately after surgery and before starting hand therapy ( Fig. 4 ). All patients were checked within 8 days (range: 7–15) of surgery. The second follow-up was planned at 1 month after surgery (range: 28–45 days) with radiographs. The patients were followed-up for an average of 16.8 weeks (range: 8–24) ( Fig. 5 ).
Fig. 4.

After osteosynthesis, the metacarpal and the adjacent digit were dressed with buddy strapping. The patients were encouraged to actively mobilize finger immediately after surgery.
Fig. 5.

The TAM recovered at the end of follow-up.
Patients were addressed to surgical treatment by three hand surgeons. The surgeon who performed the operative fixation and the physician who registered the postoperative data were not the same who enrolled the patients. This was to reduce the possible bias into the medical record.
Manchester-modified or M2 DASH (Disabilities of the Arm, Shoulder and Hand questionnaire) Score Test and Total Active Motion (TAM) of the fingers were measured at each follow-up, and at the final follow-up, grip strength was measured in both the hands using a Jamar dynamometer (Patterson Medical Holding, Warrenville, Illinois, United States). 4 Hand therapist (included in the study team) performed the tests.
Results
Fractures were radiologically healed within 4.36 weeks (range: 4–6). The functional recovery was checked with M2 DASH Score, mean 0.6 (range: 0–5); TAM, mean 250.8 degrees (range: 220–260); and Jamar grip strength, mean 42.24 kg (range: 33–52). At the final follow-up, the average extension lag for the MCP joint was 4 degrees (range: 0–16), for the proximal interphalangeal (PIP) joint it was 7 degrees (range: 0–18), and no extension lag for the distal interphalangeal (DIP) joint was evaluated ( Table 1 ). No inadequate fixation, intra-articular protruding screws, loss of reduction, malrotation, infection, screw migration, or complex regional pain syndrome (CRPS) was revealed. No implant was removed, and at the final follow-up, no signs of early osteoarthritis was revealed.
Table 1. Functional results at the final follow-up.
| No. | Occupation | Age (y) | DASH score pre | DASH Score post | Return to work (w) | Union Rx (w) | Grip Injured hand (Kg) | Grip Uninjured hand (Kg) | Follow-up (w) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Abbreviations: DASH, Disabilities of the Arm, Shoulder and Hand questionnaire; Rx, treatment; TAM, Total Active Motion. | ||||||||||
| TAM (deg) | 1 | Student | 19 | 35 | 0 | 0.5 | 4 | 56 | 58 | 24 |
| 260 | 2 | Engineer | 40 | 49 | 0 | 3 | 5 | 51 | 57 | 18 |
| 255 | 3 | White-collar | 27 | 30 | 0 | 4 | 4 | 58 | 60 | 15 |
| 245 | 4 | Doctor | 54 | 47 | 0 | 1 | 5 | 45 | 44 | 10 |
| 260 | 5 | Musician | 28 | 43 | 0.7 | 0.5 | 5 | 48 | 50 | 24 |
| 260 | 6 | Soldier | 35 | 35 | 5 | 6 | 5 | 53 | 54 | 24 |
| 245 | 7 | White-collar | 37 | 40 | 2 | 3 | 4 | 33 | 28 | 9 |
| 230 | 8 | Cyclist | 25 | 50 | 0 | 0.5 | 4 | 48 | 50 | 8 |
| 260 | 9 | Cyclist | 22 | 35 | 0 | 0.5 | 4 | 40 | 49 | 6 |
| 260 | 10 | Student | 26 | 43 | 0 | 2 | 4 | 28 | 46 | 12 |
| 255 | 11 | White-collar | 40 | 55 | 0 | 4 | 5 | 33 | 38 | 18 |
| 250 | 12 | Lawyer | 59 | 40 | 0 | 0.5 | 4 | 48 | 45 | 24 |
| 255 | 13 | White-collar | 45 | 35 | 0.7 | 4 | 4 | 33 | 36 | 21 |
| 220 | 14 | Soldier | 39 | 49 | 5 | 6 | 4 | 56 | 41 | 24 |
| 235 | 15 | White-collar | 31 | 40 | 1 | 4 | 4 | 41 | 38 | 19 |
| 250 | 16 | Musician | 27 | 45 | 0 | 0.5 | 4 | 33 | 30 | 17 |
| 265 | 17 | Freelancer | 22 | 55 | 0 | 1 | 5 | 40 | 41 | 16 |
| 240 | 18 | Cyclist | 21 | 60 | 0 | 0.5 | 6 | 33 | 42 | 24 |
| 240 | 19 | Surgeon | 34 | 30 | 0 | 0.5 | 4 | 41 | 38 | 10 |
| 245 | 20 | Freelancer | 37 | 50 | 0.7 | 2 | 4 | 33 | 45 | 12 |
| 260 | 21 | Soldier | 21 | 49 | 5 | 8 | 4 | 46 | 37 | 11 |
| 245 | 22 | Cyclist | 19 | 60 | 0 | 0.5 | 4 | 38 | 40 | 18 |
| 260 | 23 | Cyclist | 20 | 45 | 0 | 1 | 4 | 35 | 30 | 16 |
| 250 | 24 | White-collar | 56 | 35 | 0 | 4 | 4 | 41 | 48 | 18 |
| 260 | 25 | Freelancer | 35 | 40 | 0 | 2 | 5 | 45 | 39 | 24 |
| 265 | TOTAL | 32.8 | 43.8 | 0.6 | 2.38 | 4.36 | 42.24 | 43.36 | 16.8 | |
Although the results achieved are overall very good, the authors stress the different recovery time between the patients who benefit of a public insurance found (white-collar, soldier, etc.) with a return to work in mean 5 weeks versus the patients without health insurance assistance (freelancer, student, etc.) or with high functional demands (cyclist, musician, etc.) that have a very fast return to daily activities (mean 2.38 weeks). 4 5 6 7 8
Discussion
This case series showed that intramedullary headless screws combined with wide-awake anesthesia is a safe, quick, and reliable alternative to fix unstable metacarpal fractures. This procedure is even more suitable in patients who require a short period to recovery before return to work or daily life (athletes, white-collar, freelancer, or high demand worker). 9 10
To achieve good results and reduce disadvantages, a strict adherence to the surgical technique is mandatory. In practice, it is important to understand the fracture pattern and try to fix it, achieving good primary stability and avoiding shortening, rotation, and kneeling of the metacarpal head. These critical issues can be preventing with a careful preoperative planning, choosing the correct diameter and length of the screw.
Another key point remains the insertion area on the metacarpal head, where the loading area of the articular surface should be respected. 1 2 7 9 11 12 13
The technique is even more handy using a wide-awake local anesthesia with bupivacaine + epinephrine (1:100,000). In fact, this procedure reduces perioperative time with a concrete cost and time saving. 3 4
Furthermore, the wide-awake procedure allows to achieve: (1) surgery without tourniquet, (2) reduction in the volume needed to obtain a painless surgery (20 mL rather 40 mL), taking advantage from one single injection dorsal block, (3) immediate malrotation check, (4) a very cost-efficient procedure, reliable in the outpatient setting rather in the main operating room, and (5) prolonged pain control effect. Indeed, bupivacaine is slowly released after injection into the surgical area. This effect is due to a liposomal activity, and it provides prolonged pain analgesia up to 72 hours, clearly longer than bupivacaine alone. 3 11
The two main limits of this procedure include the difficult screw management during percutaneous insertion, in particular when the screw base get in the soft tissue, and the difficult removal that probably implies a more difficult surgery than insertion. 1 2 9 11
On the other hand, very good results achieved, especially in term of fast return to work and daily actions, should be a stimulus to return to daily and productive life, primarily for patients who benefit of a public insurance found. These data could be deepen and analyzed with further studies with the aim of improving the public spending review.
Note
The level of evidence is IV.
Acknowledgments
The authors would like to thank Giulia Ghelarducci, Hand Therapist of the University Hospital of Pisa and Fisiolife Upper limb Team Therapy for dedication and professionalism.
Footnotes
Conflict of Interest None.
References
- 1.Giesen T, Gazzola R, Poggetti A, Giovanoli P, Calcagni M. Intramedullary headless screw fixation for fractures of the proximal and middle phalanges in the digits of the hand: a review of 31 consecutive fractures. J Hand Surg Eur Vol. 2016;41(07):688–694. doi: 10.1177/1753193416641330. [DOI] [PubMed] [Google Scholar]
- 2.Borbas P, Dreu M, Poggetti A, Calcagni M, Giesen T. Treatment of proximal phalangeal fractures with an antegrade intramedullary screw: a cadaver study. J Hand Surg Eur Vol. 2016;41(07):683–687. doi: 10.1177/1753193416641319. [DOI] [PubMed] [Google Scholar]
- 3.Thomson C J, Lalonde D H. Randomized double-blind comparison of duration of anesthesia among three commonly used agents in digital nerve block. Plast Reconstr Surg. 2006;118(02):429–432. doi: 10.1097/01.prs.0000227632.43606.12. [DOI] [PubMed] [Google Scholar]
- 4.Fess E E, Moran C A. Clinical assessment recommendation. American Society of Hand Therapists. 1981.
- 5.Ozturk I, Erturer E, Sahin F et al. Effects of fusion angle on functional results following non-operative treatment for fracture of the neck of the fifth metacarpal. Injury. 2008;39(12):1464–1466. doi: 10.1016/j.injury.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 6.Cepni S K, Aykut S, Bekmezci T, Kilic A. A minimally invasive fixation technique for selected patients with fifth metacarpal neck fracture. Injury. 2016;47(06):1270–1275. doi: 10.1016/j.injury.2016.01.034. [DOI] [PubMed] [Google Scholar]
- 7.Ruchelsman D E, Puri S, Feinberg-Zadek N, Leibman M I, Belsky M R. Clinical outcomes of limited-open retrograde intramedullary headless screw fixation of metacarpal fractures. J Hand Surg Am. 2014;39(12):2390–2395. doi: 10.1016/j.jhsa.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 8.Page S M, Stern P J. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23(05):827–832. doi: 10.1016/S0363-5023(98)80157-3. [DOI] [PubMed] [Google Scholar]
- 9.Malasitt P, Owen J R, Tremblay M A, Wayne J S, Isaacs J E. Fixation for metacarpal neck fracture: a biomechanical study. Hand (NY) 2015;10(03):438–443. doi: 10.1007/s11552-015-9744-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boulton C L, Salzler M, Mudgal C S. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg Am. 2010;35(08):1260–1263. doi: 10.1016/j.jhsa.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 11.del Piñal F, Moraleda E, Rúas J S, de Piero G H, Cerezal L. Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg Am. 2015;40(04):692–700. doi: 10.1016/j.jhsa.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 12.Doarn M C, Nydick J A, Williams B D, Garcia M J. Retrograde headless intramedullary screw fixation for displaced fifth metacarpal neck and shaft fractures: short term results. Hand (NY) 2015;10(02):314–318. doi: 10.1007/s11552-014-9620-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ten Berg P W, Mudgal C S, Leibman M I, Belsky M R, Ruchelsman D E. Quantitative 3-dimensional CT analyses of intramedullary headless screw fixation for metacarpal neck fractures. J Hand Surg Am. 2013;38(02):322–330. doi: 10.1016/j.jhsa.2012.09.029. [DOI] [PubMed] [Google Scholar]


