Abstract
Pisiform dislocation is a rare wrist injury. The limited literature available describes this pathology in the form of case reports. An immediate closed reduction and immobilization is indicated for acute injury while there is a debate in the management of cases with delayed diagnosis or failed closed reduction. In this case, a 32-year-old, right-handed man visited the emergency department with pain at the ulnar side of his left wrist after a fall. The initial management involved immobilization, and the patient was referred to the authors’ specialized clinic 10 days later because of persistence of important ulnar wrist pain. The choice of treatment was pisiform excision without ligament reconstruction with excellent functional results.
Keywords: dislocation, luxation, pisiform, wrist injury
Introduction
The pisiform bone is situated in the proximal row of the carpal bones where it forms a diarthrodial synovial joint by articulating dorsally with the triquetrum. Though it is considered as a sesamoid bone, it provides stability to the wrist. During development, its center of ossification appears between 7, 5, and 10 years of age, and it is fully developed by the age of 12 years. It is the last carpal bone to ossify. 1
Various anatomical studies have reported complex connections with a variety of ligaments. On the volar surface, the pisiform bone is hooded by the flexor carpi ulnaris (FCU) tendon. The other connections include the pisohamate ligament, origin of the abductor digiti minimi, anterior annular ligament, pisometacarpal ligament, and extensor retinaculum ( Fig. 1 ).
Fig. 1.
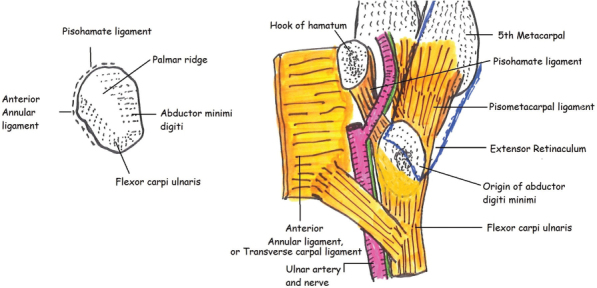
Pisiform anatomical connections.
Traumatic dislocation of the pisiform bone is a rare injury with very few cases described in the literature. In the event of acute injury, closed reduction and immobilization can be performed. However, there is a debate in the management on cases with delayed diagnosis. Some authors suggest an open or closed reduction with pinning of the unstable pisiform in its anatomical location whereas others prefer its excision. In this article, the authors present a case report and a comprehensive review of the literature.
Case Report
In November 2014, a 32 year-old, right-handed man visited the emergency department with pain at the ulnar side of his left wrist after a fall from a height of approximately 1 m. The initial management involved immobilization and oral painkillers. Because of the persistence of the pain and limited wrist mobility, the patient was referred to the authors’ specialized clinic 10 days after the initial injury. The clinical examination revealed a painful mass on the distal ulnar side of the triquetrum and severely diminished wrist motion.
Radiologic imaging by plain X-rays confirmed the diagnosis of pisiform dislocation associated with a small avulsion of the distal extremity of the triquetrum regarding the pisotriquetral ligament ( Fig. 2 ).
Fig. 2.

Radiologic imaging confirming the diagnosis of pisiform dislocation.
An additional imaging, by magnetic resonance imaging (MRI), was decided to investigate any ligamentous or tendon injury. There was no lesion of the FCU tendon or a hematoma ( Fig. 3 ).
Fig. 3.

MRI image showing no FCU tendon lesion.
Because the authors were already at day 10 post injury, pisiform excision was decided as the choice of treatment. During the operation, the pisiform bone was identified through a hypothenar incision and detached meticulously from its ligamentous attachments ( Fig. 4 ).
Fig. 4.

Surgical approach identifying dislocated pisiform in hypothenar region.
No FCU ligamentoplasty was performed. The operation site was closed with Donati-type sutures using Prolene 4–0 (Ethicon Inc., Somerville, New Jersey, United States). The wrist was immobilized in an antebrachial plaster cast for 2 weeks followed by 2 weeks in a removable prefabricated wrist brace. Sutures were removed at 2 weeks while physiotherapy was initiated at 3 weeks postoperatively. At 2-month follow-up, the patient had a full range of motion with no pain to his left wrist, and at 6 months, full restoration of grip power was noted ( Fig. 5 ).
Fig. 5.

At 2-month follow-up: with full range of motion.
The patient regained all his professional and leisure activities at 2.5 months and was extremely satisfied with the aesthetic and functional result ( Fig. 6 ).
Fig. 6.

At 6-month follow-up: minimal scarring with extremely satisfying aesthetic result for the patient.
Discussion
The authors performed a search in the most frequented medical databases. Pisiform, dislocation, and luxation were used as keywords. In the Ovid database, 14 results were identified of which 6 directly described a pisiform dislocation. In PubMed and Embase databases, the total results were 47 and 62, respectively. However, from these, 22 in PubMed and 26 in Embase were eligible. Only articles that directly described cases of pisiform luxation that could be found were included. Consequently total 19 articles were identified. 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20
Of these 19, 14 cases involved adults whereas 5 were of children or adolescents. Fourteen reported isolated dislocations, 1 dislocation fracture, whereas 2 cases were associated with distal radius fractures and 3 had concomitant hamate dislocation. The mechanism of injury was predominantly direct impact to the pisiform region with 16 reports. Other mechanisms included two crush injuries and one after a cartwheel maneuver. Of these cases, 6 were treated conservatively and 13, surgically. As operative procedures, there were 1 open reduction and pining and 12 pisiform excisions.
Traumatic dislocation of the pisiform bone is a rare injury with no consensus for the treatment of choice. The limited literature suggests that closed reduction and immobilization could have good outcomes in acute injuries with correct immediate diagnosis. However, several cases are misdiagnosed in an emergency setting and are identified when the patient is referred to a specialist. In most cases, this happens after several days because of the persistence of wrist pain and disability.
Open or closed reduction and fixation of the pisiform seems to have poor results with high incidence of pisiform instability and recurrent dislocation. In some cases initially treated by reduction and pining, a secondary excision was required.
Direct excision of the pisiform seems to be the best option for cases with delayed diagnosis. While most reports describe a technique with a longitudinal incision, in this case the authors used an incision along the hypothenar crease with a good aesthetic result ( Fig. 6 ). Some authors suggest that a careful ligamentoplasty should be performed after the excision to stabilize the FCU tendon and prevent loss of grip power. 1 15 18 21 The authors showed that careful detachment of the pisiform bone alone could have excellent functional results with rapid restoration of stability and strength.
Footnotes
Conflict of Interest None.
References
- 1.Pevny T, Rayan G M, Egle D. Ligamentous and tendinous support of the pisiform, anatomic and biomechanical study. J Hand Surg Am. 1995;20(02):299–304. doi: 10.1016/S0363-5023(05)80030-9. [DOI] [PubMed] [Google Scholar]
- 2.Cohen I. Dislocation of the Pisiform. Ann Surg. 1922;75(02):238–239. doi: 10.1097/00000658-192202000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Immermann E W. Dislocation of the pisiform. J Bone Joint Surg Am. 1948;30A(02):489–22. [PubMed] [Google Scholar]
- 4.Sundaram M, Shively R, Patel B, Tayob A. Isolated dislocation of the pisiform. Br J Radiol. 1980;53(633):911–912. doi: 10.1259/0007-1285-53-633-911. [DOI] [PubMed] [Google Scholar]
- 5.Korovessis P. [Traumatic luxation of the pisiform bone] Handchir Mikrochir Plast Chir. 1983;15(03):196–197. [PubMed] [Google Scholar]
- 6.Minami M, Yamazaki J, Ishii S. Isolated dislocation of the pisiform: a case report and review of the literature. J Hand Surg Am. 1984;9A(01):125–127. doi: 10.1016/s0363-5023(84)80200-2. [DOI] [PubMed] [Google Scholar]
- 7.Gainor B J. Simultaneous dislocation of the hamate and pisiform: a case report. J Hand Surg Am. 1985;10(01):88–90. doi: 10.1016/s0363-5023(85)80255-0. [DOI] [PubMed] [Google Scholar]
- 8.García-Elias M.Simultaneous dislocation of the hamate and pisiform bone J Hand Surg Am 19851006Pt01908–909. [DOI] [PubMed] [Google Scholar]
- 9.McCarron R F, Coleman W. Dislocation of the pisiform treated by primary resection. A case report. Clin Orthop Relat Res. 1989;(241):231–233. [PubMed] [Google Scholar]
- 10.Ishizuki M, Nakagawa T, Itoh S, Furuya K. Positional dislocation of the pisiform. J Hand Surg Am. 1991;16(03):533–535. doi: 10.1016/0363-5023(91)90027-9. [DOI] [PubMed] [Google Scholar]
- 11.Sharara K H, Farrar M. Isolated dislocation of the pisiform bone. J Hand Surg [Br] 1993;18(02):195–196. doi: 10.1016/0266-7681(93)90108-r. [DOI] [PubMed] [Google Scholar]
- 12.Ashkan K, O'Connor D, Lambert S. Dislocation of the pisiform in a 9-year-old child. J Hand Surg [Br] 1998;23(02):269–270. doi: 10.1016/s0266-7681(98)80195-2. [DOI] [PubMed] [Google Scholar]
- 13.Kubiak R, Slongo T, Tschäppeler H. Isolated dislocation of the pisiform: an unusual injury during a cartwheel maneuver. J Trauma. 2001;51(04):788–789. doi: 10.1097/00005373-200110000-00029. [DOI] [PubMed] [Google Scholar]
- 14.Levante S, Ebelin M. [Traumatic dislocation of the pisiform bone: a case report and review of the literature] Chir Main. 2002;21(04):264–268. doi: 10.1016/s1297-3203(02)00122-1. [DOI] [PubMed] [Google Scholar]
- 15.Schädel-Höpfner M, Böhringer G, Junge A. Dislocation of the pisiform bone after severe crush injury to the hand. Scand J Plast Reconstr Surg Hand Surg. 2003;37(04):252–255. doi: 10.1080/02844310310016758. [DOI] [PubMed] [Google Scholar]
- 16.Mancini F, De Maio F, Ippolito E. Pisiform bone fracture-dislocation and distal radius physeal fracture in two children. J Pediatr Orthop B. 2005;14(04):303–306. doi: 10.1097/01202412-200507000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto T, Tsunoda M, Yamaguchi S et al. Traumatic dislocation of the hamate and pisiform: a case report and review of the literature. J Orthop Trauma. 2005;19(04):282–285. doi: 10.1097/01.bot.0000135839.17363.93. [DOI] [PubMed] [Google Scholar]
- 18.Goriainov V, Bayne G, Warwick D J. Traumatic dislocation of the pisiform: a case report. J Orthop Surg (Hong Kong) 2010;18(03):389–390. doi: 10.1177/230949901001800329. [DOI] [PubMed] [Google Scholar]
- 19.Saleh W R, Yajima H, Nakanishi A. Conservative treatment of the isolated dislocation of the pisiform bone. J Plast Surg Hand Surg. 2014;48(04):283–284. doi: 10.3109/2000656X.2013.779799. [DOI] [PubMed] [Google Scholar]
- 20.Hurni Y, Fusetti C, de Rosa V. Fracture dislocation of the pisiform bone in children: a case report and review of the literature. J Pediatr Orthop B. 2015;24(06):556–560. doi: 10.1097/BPB.0000000000000210. [DOI] [PubMed] [Google Scholar]
- 21.Pevny T, Rayan G M. Recurrent dislocation of the pisiform bone. Am J Orthop. 1996;25(02):155–156. [PubMed] [Google Scholar]


