Abstract
Spermatogenesis is regulated by the 2 pituitary gonadotropins, luteinizing hormone (LH) and follicle-stimulating hormone (FSH). This process is considered impossible without the absolute requirement of LH-stimulated testicular testosterone (T) production. The role of FSH remains unclear because men and mice with inactivating FSH receptor (FSHR) mutations are fertile. We revisited the role of FSH in spermatogenesis using transgenic mice expressing a constitutively strongly active FSHR mutant in a LH receptor–null (LHR-null) background. The mutant FSHR reversed the azoospermia and partially restored fertility of Lhr–/– mice. The finding was initially ascribed to the residual Leydig cell T production. However, when T action was completely blocked with the potent antiandrogen flutamide, spermatogenesis persisted. Hence, completely T-independent spermatogenesis is possible through strong FSHR activation, and the dogma of T being a sine qua non for spermatogenesis may need modification. The mechanism for the finding appeared to be that FSHR activation maintained the expression of Sertoli cell genes considered androgen dependent. The translational message of our findings is the possibility of developing a new strategy of high-dose FSH treatment for spermatogenic failure. Our findings also provide an explanation of molecular pathogenesis for Pasqualini syndrome (fertile eunuchs; LH/T deficiency with persistent spermatogenesis) and explain how the hormonal regulation of spermatogenesis has shifted from FSH to T dominance during evolution.
Keywords: Endocrinology, Reproductive Biology
Keywords: Fertility, Reproductive biochemistry
Introduction
It is textbook knowledge that spermatogenesis is impossible without luteinizing hormone–stimulated (LH-stimulated) testicular testosterone (T) production (1, 2). Human mutations and genetically modified mice provide further proof for this, as men harboring inactivating LHB and LHCGR mutations are hypogonadal and azoospermic, with knockout mice for the same genes exhibiting a similar phenotype (2). Surprisingly, the role of follicle-stimulating hormone (FSH), the other endocrine stimulus of spermatogenesis, has remained elusive. Although a long-held notion ascribes the pubertal initiation and maintenance of normal spermatogenesis to FSH (1), phenotypes of inactivating FSHB (3) and FSH receptor (FSHR) (4) mutations in men and knockout mice for the cognate genes (5, 6) prompt a different conclusion. With the exception of men with FSHB mutations (3), all others preserve spermatogenesis and fertility. Hence, the current view is that FSH improves spermatogenesis qualitatively and quantitatively in additive fashion with T, but is not necessary for male fertility per se. While T can maintain spermatogenesis without FSH, the reverse has never been demonstrated (7). Despite the crucial role of T, the specific phase of spermatogenesis that is absolutely androgen dependent and the distinct functions of T and FSH have not been completely delineated. Because of their entirely different mechanisms of action, FSH acting through a GPCR with cAMP as second messenger and T activating the androgen receptor (AR), a nuclear transcription factor, it is justified to hypothesize that each hormone has distinct and irreplaceable effects.
To delineate the cryptic role of FSH in spermatogenesis, we used the transgenic mouse model expressing a constitutively strongly activating Fshr point mutation (Fshr-CAM; D580H) in Sertoli cells (SC) under the human anti-Müllerian hormone promoter (8). These mice were crossed with female heterozygous Lhr–/– mice (9) with the expectation that the role of FSH could in this way be amplified and studied in isolation from the LH/T effects. The unexpected findings during the experiments challenge the dogma of T dependence of spermatogenesis because missing T action was completely compensated for by strong FSH stimulation. Our findings therefore herald potentially novel strategies into the treatment of human spermatogenic failure and suggest mechanisms for some unexplained aberrations of human spermatogenesis and the evolution of its hormonal regulation.
Results and Discussion
Our transgenic mouse model expressed a constitutively strongly activating (cAMP response >10-fold above basal) Fshr point mutation (Fshr-CAM; D580H) under the human anti-Müllerian hormone promoter (8), providing strict SC-specific expression of the transgene (10) and almost a 20-fold Fshr expression at mRNA level in comparison with WT mice. Unlike females with a robust ovarian and reproductive phenotype (8), the male littermates had no apparent abnormalities. Their testicular architecture (Figure 1B) and hormonal parameters (Supplemental Table 1; supplemental material available online with this article; https://doi.org/10.1172/JCI96794DS1) were as in WT (Figure 1A and Supplemental Table 1). Immunohistochemical localization of the FSH protein and RNAscope in situ hybridization of Fshr mRNA were confined to SC (Supplemental Figure 1), indicating that functionally meaningful leakage of the Fshr-CAM transgene to Leydig cells (LC) is highly unlikely. In the absence of any phenotype of the Fshr-CAM males, it is apparent that physiological FSH concentrations provide maximal SC stimulation. This may explain why only 2 activating FSHR mutations, detected serendipitously, have been described. One was a hypophysectomized man with persistent spermatogenesis (11) and the other a man with normal spermatogenesis in the absence of circulating FSH (12). Furthermore, testicular function appears normal in men with pituitary adenomas secreting excessive FSH (13, 14). Hence, there may be no phenotypic effect of enhanced FSH action in otherwise healthy men.
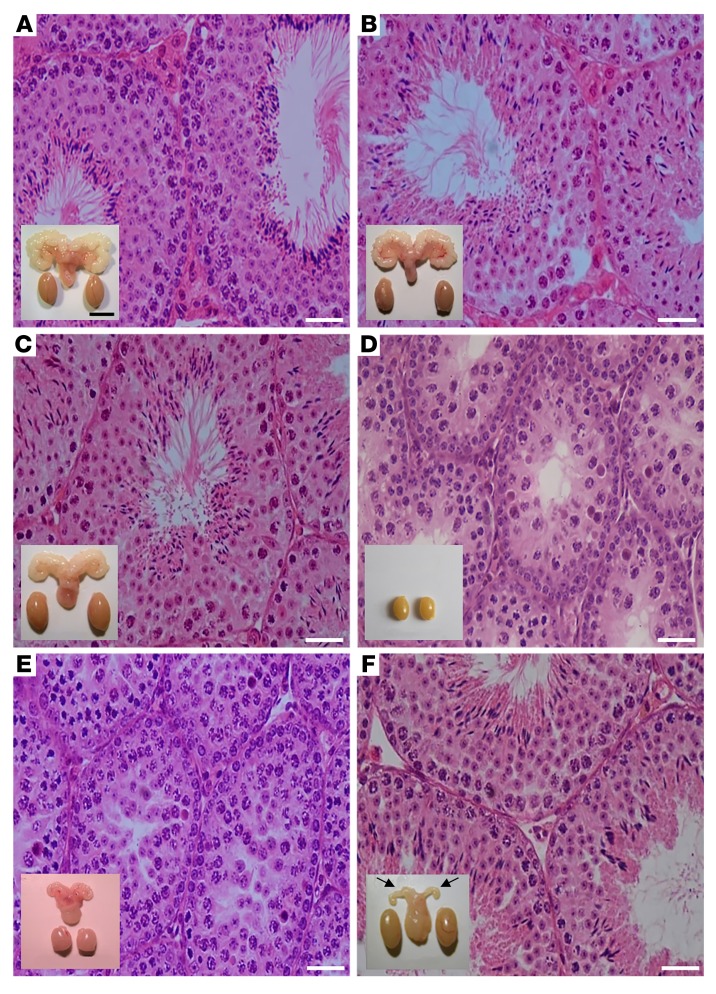
Figure 1. Testicular histology and macroscopic views of testes and urogenital blocks from different mouse genotypes and from flutamide-treated animals.
Representative views of (A) WT, (B) Fshr-CAM, (C) Fshr-CAM/Lhr–/–, and (D) Lhr–/– mice (n = 5–8/group). A–C show normal spermatogenesis and testis and SV sizes. In D, spermatogenesis is shown as arrested at the RS stage, with small testes and rudimentary SV (not shown). (E) Treatment of WT mice (n = 5/group) with antiandrogen flutamide arrested spermatogenesis at RS stage, with reduced testis and SV sizes. (F) Identical treatment of Fshr-CAM/Lhr–/– mice (n = 5/group) had no apparent effect on spermatogenesis and testis size, but reduced SV sizes (arrows in F). Scale bars: 50 μm; 10 mm (insets).
Strong Fshr activation in the double-mutant Fshr-CAM/Lhr–/– mice surprisingly reversed the hypogonadism and infertility of the Lhr–/– mice, with development of a near-normal male phenotype with increased testicular size and spermatogenesis (Figure 1C), comparable to that in WT and Fshr-CAM littermates (Figure 1, A and B). These mice, however, presented with delayed puberty (Supplemental Figure 2A). The anogenital distance, another androgen-dependent developmental parameter, was similar in the Fshr-CAM/Lhr–/– mice and control littermates at weaning (P20), but at puberty and thereafter, it was approximately 10% and 40% shorter in the Fshr-CAM/Lhr–/– and Lhr–/– mice, respectively (Supplemental Figure 2B). Mating tests showed similar mounting behavior in Fshr-CAM/Lhr–/– mice and WT littermates, with evidence for copulatory plugs in females. However, the Fshr-CAM/Lhr–/– breeding pairs had lower frequencies of pregnancies and smaller litter sizes (Supplemental Table 2), with no evidence for embryonic lethality in offspring.
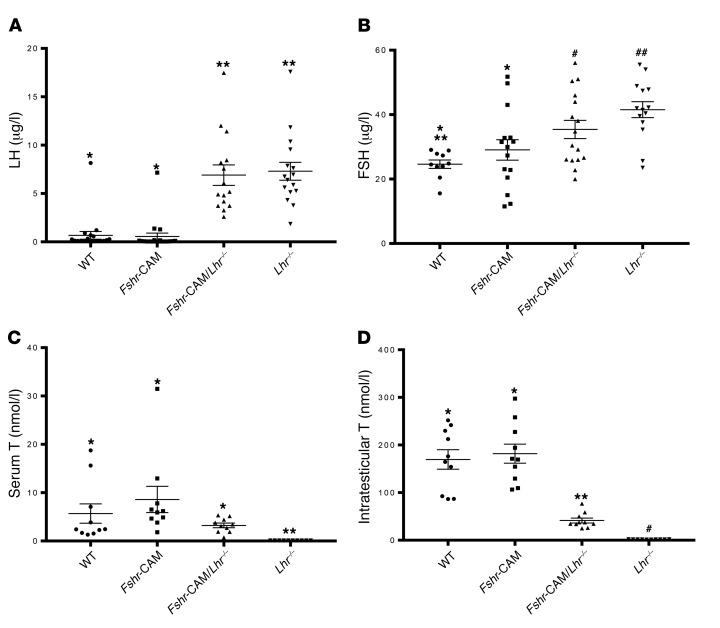
LH concentrations were markedly (10-fold) and FSH marginally (1.5-fold) elevated in the mice with Lhr–/– genotypes (Figure 2, A and B). Serum T in the Lhr–/– mice was very low (<0.01 nmol/l), while in Fshr-CAM/Lhr–/– mice, it recovered to about 40% of WT levels (Figure 2C). Similar trends, though with greater differences between genotypes, were observed in intratesticular T (iTT) concentrations (Figure 2D). The increased seminal vesicle (SV), epididymis, and testis weights (Supplemental Figure 2, C–E) and the observed testicular descent in Fshr-CAM/Lhr–/– mice demonstrated biological action of the partially recovered T production. However, the lack of LH suppression indicated that the recovered T production was insufficient to evoke negative feedback.
Figure 2. Hormone analyses.
(A) Serum LH, (B) serum FSH, (C) serum T, and (D) iTT. Data represent mean ± SEM. n = 10–15 individual samples/group. Groups with different symbols differ significantly from each other (P < 0.05; ANOVA/Newman-Keuls).
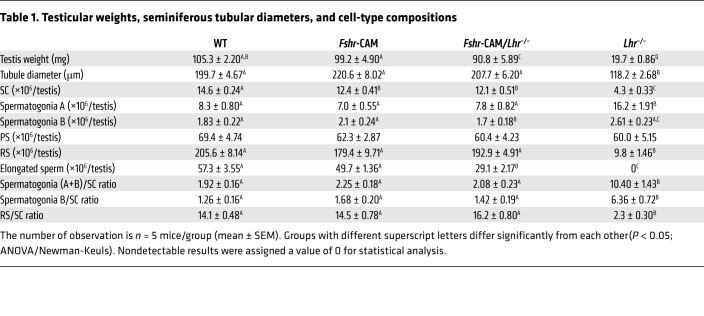
Sizes of the double-mutant mouse testes were indistinguishable from those of WT (Table 1 and Supplemental Figure 2E) and reflected on the appearance of fully developed seminiferous tubules, with typical stages of the seminiferous epithelial cycle and presence of elongated and mature spermatids (Figure 1C). A noticeable difference common to both Lhr–/– genotypes was the apparent lack of mature LC (Figure 1, C and D). Stereological assessment per testis (Table 1) and per mg testis (Supplemental Table 3) indicated approximately 15% less SC per testis of the Fshr-CAM/Lhr–/– mice, with no difference in tubular diameter or the number of spermatogonia A and B, when compared with WT. The round spermatid (RS) number and RS/SC and spermatogonia/SC ratios were also similar; however, the number of elongated spermatids per testis was about half that in WT. This observation was different in the Lhr–/– testes, where tubular diameter was approximately half of WT, the number of spermatogonia A was doubled, RS and RS/SC ratios were drastically reduced, the spermatogonia/SC ratio was increased, and elongated spermatids were completely absent (Figure 1D).
Table 1. Testicular weights, seminiferous tubular diameters, and cell-type compositions.
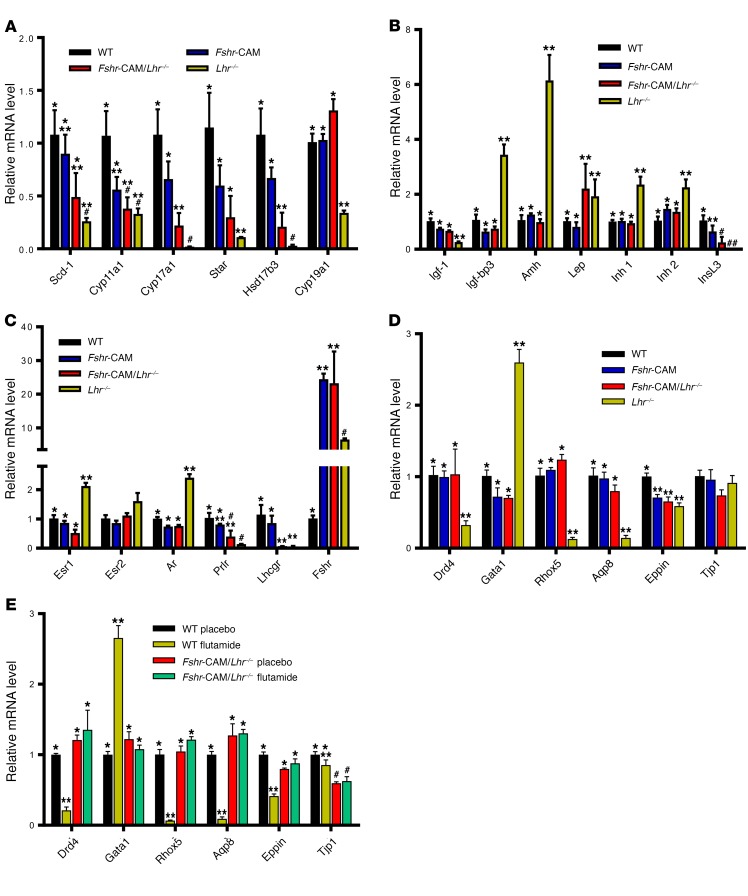
At this stage, we hypothesized that the recovery of spermatogenesis in the Fshr-CAM/Lhr–/– mice was due to the partially recovered T production by rudimentary LC, stimulated by the well-documented FSH-responsive paracrine signaling from SC (2, 15–17). Accordingly, the expression of LC-specific genes Scd1, Star, Cyp11a1, Cyp17a1, and Hsd17b3 was slightly increased in the double-mutant mice over Lhr–/– mice (Figure 3A), while the expression levels of SC genes roughly paralleled the proportion of SC in the testes (Figure 3, B and C). Immunohistochemistry of StAR, HSD17B3, CYP17A1, and HSD3B1 demonstrated that the steroidogenic transport protein and enzymes were solely confined to LC in all genotypes (Supplemental Figure 3), excluding ectopic SC T production. The observed iTT concentration of approximately 40 nmol/l in the Fshr-CAM/Lhr–/– mice is in fact sufficient to initiate spermatogenesis in T-treated Lhr–/– mice (18).
Figure 3. Relative mRNA expression in testes.
(A) Steroidogenic genes. (B) Hormones and growth factors. (C) Hormone receptors. (D) Androgen-regulated (Drd5, Rhox5, Eppin, and Tjp1), postmeiotic germ cell–specific (Aqp8), and germ cell–regulated (Gata1) genes in WT, Fshr-CAM, Fshr-CAM/Lhr–/–, and Lhr–/– testes. In contrast with the LC genes downregulated in Lhr–/– testes (A), we identified several upregulated SC-specific genes (B and C). Expression of 3 steroid receptor genes with mixed localization, namely, Esr1, Esr2, and Ar, also resembled that of the SC-specific genes (C). The increased proportion of SC per unit weight in Lhr–/– testes (Table 1 and Supplemental Table 3) apparently explains, at least partly, the enrichment of the SC genes. Expression of these genes became normalized in the Fshr-CAM/Lhr–/– mice, in accordance with the normalization of testis size and proportions of the different cell types. (E) Effect of flutamide treatment on expression of androgen-regulated genes in WT and Fshr-CAM/Lhr–/– mice. Data represent mean ± SEM. n = 3 samples/group. Bars with different symbols differ significantly from each other (P < 0.05; ANOVA/Newman-Keuls).
We next addressed the role of the residual T levels in the unexpected activation of spermatogenesis in the Fshr-CAM/Lhr–/– mice by eliminating the effect of this androgen through treatment with the potent antiandrogen flutamide. As anticipated, in WT control mice, flutamide induced shrinkage of SVs and testes along with complete cessation of spermatogenesis at the RS stage (Figure 1E). Stereological assessment of the testes after treatment (Supplemental Table 4) confirmed the efficacy of flutamide treatment. Previously, the same antiandrogen treatment in 12-month-old Lhr–/– mice completely blocked spermatogenesis at the RS stage; however, spermatogenesis was qualitatively complete in control Lhr–/– mice and driven by the residual low iTT level (2% of normal) (19). Surprisingly, identical antiandrogen treatment of Fshr-CAM/Lhr–/– mice brought about only shrinkage of the SVs, without affecting testicular size, cell-type composition, and sperm maturation (Figure 1F and Supplemental Table 4). Hence, upon complete blockage of androgen action, the constitutively active FSHR maintained spermatogenesis in these mice.
Previously, a study on the role of FSH in mouse spermatogenesis compared Lhr–/– and hypogonadal gonadotropin–deficient hpg mice, expressing through transgenesis either human FSH or a mildly constitutively active form of human FSHR (20). Both presented with normal to high-normal FSH action and low T levels, which, relative to hpg controls, led to increased SC numbers, enhanced spermatogonial proliferation, and some meiotic development, but no mature spermatids. FSH stimulation alone in these models was unable to evoke complete spermatogenesis without the critical involvement of LH-stimulated T production. In contrast, our findings demonstrate that stimulation of spermatogenesis with strong FSH effect alone is possible.
Quantification of selected androgen-dependent SC genes Drd4, Rhox 5, and Eppin (2) demonstrated their clearly decreased expression in the flutamide-treated WT testes in agreement with their low expression in the androgen-deprived Lhr–/– testes (Figure 3, D and E). In contrast, no reduction in the high expression of these androgen-dependent genes was found in flutamide-treated Fshr-CAM/Lhr–/– testes (Figure 3E), indicating that the strong Fshr-CAM signaling was able to maintain the expression of genes considered strictly androgen regulated. A similar expression pattern was found with the indirectly androgen-dependent postmeiotic germ cell–specific gene Aqp8 (21), apparently reflecting the persistence of testicular postmeiotic germ cells, normally present in the testis only through androgen action, but maintained by Fshr activation in the flutamide-treated Fshr-CAM/Lhr–/– testes. Another SC-specific gene, Gata-1, is resistant to androgen action, but downregulated by paracrine effects from postmeiotic germ cells (22). Hence, it was upregulated in the flutamide-treated WT testes, consequent to postmeiotic germ cell depletion, but not in the Fshr-CAM/Lhr–/– testes with full spermatogenesis. Expression of Tjp1, a loosely androgen-regulated SC gene (23), was largely unaffected by the genetic and hormonal manipulations. Hence, Fshr-CAM expression could substitute for missing androgen action in the maintenance of testicular androgen–dependent gene expression, providing a mechanism for the unexpected androgen-independent spermatogenesis.
T and FSH are assumed to regulate spermatogenesis through distinct and nonoverlapping signaling mechanisms (24, 25). Closer evaluation of T- and FSH-driven signaling, however, reveals that the actions of these hormones affect overlapping pathways, as both FSH and T activate the MAP/ERK and CREB signaling cascades (25), recently shown to be crucial for murine spermatogenesis through a rapid T signaling mechanism (26). FSH and T also have nonadditive effects on SC intracellular levels of free Ca2+, possibly mediated by the same Ca2+ channels (27, 28). Consequently, T and FSH signaling pathways are partly overlapping, but strong FSH stimulation in the absence of T is required to observe the FSH effect on classical androgen-regulated genes. The incomplete recovery of quantitative spermatogenesis and fertility in the Fshr-CAM/Lhr–/– mice emphasizes that qualitatively and quantitatively full spermatogenesis requires T.
Our finding of strong FSH stimulation maintaining spermatogenesis in the absence of T in mice is in all probability similar to what occurs in humans and could explain the equivocal effects of FSH therapy in the treatment of idiopathic oligozoospermia (29, 30). We believe that strong FSH action can boost spermatogenesis beyond that achieved at physiological levels and may even compensate for missing or insufficient T action, e.g., in oligozoospermia due to partial androgen resistance. Indeed, a study using 3- to 6-fold higher than the standard dose of FSH (75 IU, 2 to 3 times weekly) showed significant stimulation of spermatogenesis in idiopathic oligozoospermia (31). Besides increased FSH doses, the recently developed small molecule allosteric agonists of glycoprotein hormones (32) could offer a future alternative to boost FSHR activation. These findings may also explain the mechanism of persistent spermatogenesis in a hypophysectomized male with activating FSHR mutation (11) and suggest a role for FSH in the LH/T-deficient Pasqualini syndrome (fertile eunuch) (33). Clearly, spermatogenesis is possible without T, and the potential of strong FSH stimulation in the treatment of spermatogenic failure needs further attention. Finally, our findings provide insight into the perplexing shift in the hormonal regulation of spermatogenesis during evolution from FSH in teleost fishes to LH/T dominance in mammals (34).
Methods
Statistics.
Single comparisons were performed with unpaired 2-tailed Student’s t tests and multiple comparisons using ANOVA and Newman-Keuls post hoc test. All data sets are presented as mean ± SEM, unless otherwise stated. P < 0.05 was considered statistically significant.
Study approval.
All procedures conformed to the Imperial College London Animal Welfare Protocol and were approved in accordance with the regulations and standards of the UK Home Office Animal Scientific Procedures Act (ASPA) 1986 and the European Union Directive (2010).
For additional information, see Supplemental Methods.
Author contributions
OOO, HP, and ITH designed the study. OOO, HP, AP, LV, MC, MD, LS, LO, and BK performed experiments and collected data. OOO, HP, AP, LV, MC, MD, LS, NAR, and ITH analyzed the data. OOO and ITH drafted the manuscript, with final editing from all authors.
Supplementary Material
Acknowledgments
This work was supported by Wellcome Trust Programme grant 082101/Z07/Z and MRC Project grant 0600002 (to ITH); Polish National Science Center grant 2015/17/B/NZ5/00636, and the Moikoinen Cancer Research Foundation (to NR). We thank Tuula Hämäläinen and Taina Kirjonen (Department of Physiology, University of Turku), Jennifer H. Steel, Nicholas Wood, and Anthony Okolo (IRDB, Imperial College London) for their kind help. The FSHR323 antibody was a gift from Nicolae Ghinea (Institut Curie, Paris, France).
Version 1. 03/26/2018
Electronic publication
Version 2. 05/01/2018
Print issue publication
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
License: This work is licensed under the Creative Commons Attribution 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
Reference information: J Clin Invest. 2018;128(5):1787–1792.https://doi.org/10.1172/JCI96794.
Contributor Information
Hellevi Peltoketo, Email: Hellevi.Peltoketo@oulu.fi.
Ariel Poliandri, Email: apoliand@sgul.ac.uk.
Laura Vengadabady, Email: laura.vengadabady@gmail.com.
Marcin Chrusciel, Email: marchr@utu.fi.
Milena Doroszko, Email: milena.doroszko@utu.fi.
Luna Samanta, Email: luna_samanta@rediffmail.com.
Laura Owen, Email: laura.owen@uhsm.nhs.uk.
Brian Keevil, Email: Brian.Keevil@UHSM.NHS.UK.
References
- 1.McLachlan RI, et al. Identification of specific sites of hormonal regulation in spermatogenesis in rats, monkeys, and man. Recent Prog Horm Res. 2002;57:149–179. doi: 10.1210/rp.57.1.149. [DOI] [PubMed] [Google Scholar]
- 2. Smith LB, Walker WH. Hormonal signaling in the testis. In: Plant TM, Zeleznik AJ, eds. Knobil and Neill’s Physiology of Reproduction. Vol. 1. Waltham, Massachusetts, USA: Academic Press; 2015;637–675. [Google Scholar]
- 3.Zheng J, et al. Novel FSHβ mutation in a male patient with isolated FSH deficiency and infertility. Eur J Med Genet. 2017;60(6):335–339. doi: 10.1016/j.ejmg.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Tapanainen JS, Aittomäki K, Min J, Vaskivuo T, Huhtaniemi IT. Men homozygous for an inactivating mutation of the follicle-stimulating hormone (FSH) receptor gene present variable suppression of spermatogenesis and fertility. Nat Genet. 1997;15(2):205–206. doi: 10.1038/ng0297-205. [DOI] [PubMed] [Google Scholar]
- 5.Kumar TR, Wang Y, Lu N, Matzuk MM. Follicle stimulating hormone is required for ovarian follicle maturation but not male fertility. Nat Genet. 1997;15(2):201–204. doi: 10.1038/ng0297-201. [DOI] [PubMed] [Google Scholar]
- 6.Abel MH, Wootton AN, Wilkins V, Huhtaniemi I, Knight PG, Charlton HM. The effect of a null mutation in the follicle-stimulating hormone receptor gene on mouse reproduction. Endocrinology. 2000;141(5):1795–1803. doi: 10.1210/endo.141.5.7456. [DOI] [PubMed] [Google Scholar]
- 7.Schaison G, Young J, Pholsena M, Nahoul K, Couzinet B. Failure of combined follicle-stimulating hormone-testosterone administration to initiate and/or maintain spermatogenesis in men with hypogonadotropic hypogonadism. J Clin Endocrinol Metab. 1993;77(6):1545–1549. doi: 10.1210/jcem.77.6.8263139. [DOI] [PubMed] [Google Scholar]
- 8.Peltoketo H, et al. Female mice expressing constitutively active mutants of FSH receptor present with a phenotype of premature follicle depletion and estrogen excess. Endocrinology. 2010;151(4):1872–1883. doi: 10.1210/en.2009-0966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang FP, Poutanen M, Wilbertz J, Huhtaniemi I. Normal prenatal but arrested postnatal sexual development of luteinizing hormone receptor knockout (LuRKO) mice. Mol Endocrinol. 2001;15(1):172–183. doi: 10.1210/mend.15.1.0582. [DOI] [PubMed] [Google Scholar]
- 10.Lécureuil C, Fontaine I, Crepieux P, Guillou F. Sertoli and granulosa cell-specific Cre recombinase activity in transgenic mice. Genesis. 2002;33(3):114–118. doi: 10.1002/gene.10100. [DOI] [PubMed] [Google Scholar]
- 11.Gromoll J, Simoni M, Nieschlag E. An activating mutation of the follicle-stimulating hormone receptor autonomously sustains spermatogenesis in a hypophysectomized man. J Clin Endocrinol Metab. 1996;81(4):1367–1370. doi: 10.1210/jcem.81.4.8636335. [DOI] [PubMed] [Google Scholar]
- 12.Casas-González P, et al. Normal testicular function without detectable follicle-stimulating hormone. A novel mutation in the follicle-stimulating hormone receptor gene leading to apparent constitutive activity and impaired agonist-induced desensitization and internalization. Mol Cell Endocrinol. 2012;364(1–2):71–82. doi: 10.1016/j.mce.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 13.Snyder PJ. Gonadotroph cell pituitary adenomas. Endocrinol Metab Clin North Am. 1987;16(3):755–764. [PubMed] [Google Scholar]
- 14.Galway AB, Hsueh AJ, Daneshdoost L, Zhou MH, Pavlou SN, Snyder PJ. Gonadotroph adenomas in men produce biologically active follicle-stimulating hormone. J Clin Endocrinol Metab. 1990;71(4):907–912. doi: 10.1210/jcem-71-4-907. [DOI] [PubMed] [Google Scholar]
- 15.Benahmed M, Tabone E, Grenot C, Sanchez P, Chauvin MA, Morera AM. Paracrine control of Leydig cell activity by FSH dependent proteins from Sertoli cells: an in vitro study. J Steroid Biochem. 1986;24(1):311–315. doi: 10.1016/0022-4731(86)90071-3. [DOI] [PubMed] [Google Scholar]
- 16.Verhoeven G, Cailleau J. Specificity and partial purification of a factor in spent media from Sertoli cell-enriched cultures that stimulates steroidogenesis in Leydig cells. J Steroid Biochem. 1986;25(3):393–402. doi: 10.1016/0022-4731(86)90252-9. [DOI] [PubMed] [Google Scholar]
- 17.Matikainen T, Toppari J, Vihko KK, Huhtaniemi I. Effects of recombinant human FSH in immature hypophysectomized male rats: evidence for Leydig cell-mediated action on spermatogenesis. J Endocrinol. 1994;141(3):449–457. doi: 10.1677/joe.0.1410449. [DOI] [PubMed] [Google Scholar]
- 18.Oduwole OO, et al. Overlapping dose responses of spermatogenic and extragonadal testosterone actions jeopardize the principle of hormonal male contraception. FASEB J. 2014;28(6):2566–2576. doi: 10.1096/fj.13-249219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang FP, Pakarainen T, Poutanen M, Toppari J, Huhtaniemi I. The low gonadotropin-independent constitutive production of testicular testosterone is sufficient to maintain spermatogenesis. Proc Natl Acad Sci U S A. 2003;100(23):13692–13697. doi: 10.1073/pnas.2232815100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Allan CM, et al. Complete Sertoli cell proliferation induced by follicle-stimulating hormone (FSH) independently of luteinizing hormone activity: evidence from genetic models of isolated FSH action. Endocrinology. 2004;145(4):1587–1593. doi: 10.1210/en.2003-1164. [DOI] [PubMed] [Google Scholar]
- 21.Yeung CH, Callies C, Tüttelmann F, Kliesch S, Cooper TG. Aquaporins in the human testis and spermatozoa - identification, involvement in sperm volume regulation and clinical relevance. Int J Androl. 2010;33(4):629–641. doi: 10.1111/j.1365-2605.2009.00998.x. [DOI] [PubMed] [Google Scholar]
- 22.Wakabayashi J, et al. GATA-1 testis activation region is essential for Sertoli cell-specific expression of GATA-1 gene in transgenic mouse. Genes Cells. 2003;8(7):619–630. doi: 10.1046/j.1365-2443.2003.00658.x. [DOI] [PubMed] [Google Scholar]
- 23.Hazra R, et al. Temporal role of Sertoli cell androgen receptor expression in spermatogenic development. Mol Endocrinol. 2013;27(1):12–24. doi: 10.1210/me.2012-1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Plant TM, Marshall GR. The functional significance of FSH in spermatogenesis and the control of its secretion in male primates. Endocr Rev. 2001;22(6):764–786. doi: 10.1210/edrv.22.6.0446. [DOI] [PubMed] [Google Scholar]
- 25.Walker WH, Cheng J. FSH and testosterone signaling in Sertoli cells. Reproduction. 2005;130(1):15–28. doi: 10.1530/rep.1.00358. [DOI] [PubMed] [Google Scholar]
- 26.Toocheck C, et al. Mouse spermatogenesis requires classical and nonclassical testosterone signaling. Biol Reprod. 2016;94(1):11. doi: 10.1095/biolreprod.115.132068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gorczynska E, Handelsman DJ. Androgens rapidly increase the cytosolic calcium concentration in Sertoli cells. Endocrinology. 1995;136(5):2052–2059. doi: 10.1210/endo.136.5.7720654. [DOI] [PubMed] [Google Scholar]
- 28.Lyng FM, Jones GR, Rommerts FF. Rapid androgen actions on calcium signaling in rat sertoli cells and two human prostatic cell lines: similar biphasic responses between 1 picomolar and 100 nanomolar concentrations. Biol Reprod. 2000;63(3):736–747. doi: 10.1095/biolreprod63.3.736. [DOI] [PubMed] [Google Scholar]
- 29.Attia AM, Abou-Setta AM, Al-Inany HG. Gonadotrophins for idiopathic male factor subfertility. Cochrane Database Syst Rev. 2013;23(8):CD005071. doi: 10.1002/14651858.CD005071.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rastrelli G, Corona G, Mannucci E, Maggi M. Factors affecting spermatogenesis upon gonadotropin-replacement therapy: a meta-analytic study. Andrology. 2014;2(6):794–808. doi: 10.1111/andr.262. [DOI] [PubMed] [Google Scholar]
- 31.Ding YM, et al. Treatment of idiopathic oligozoospermia with recombinant human follicle-stimulating hormone: a prospective, randomized, double-blind, placebo-controlled clinical study in Chinese population. Clin Endocrinol (Oxf) 2015;83(6):866–871. doi: 10.1111/cen.12770. [DOI] [PubMed] [Google Scholar]
- 32.Nataraja SG, Yu HN, Palmer SS. Discovery and development of small molecule allosteric modulators of glycoprotein hormone receptors. Front Endocrinol (Lausanne) 2015;6:142. doi: 10.3389/fendo.2015.00142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Valdes-Socin H, Rubio Almanza M, Tomé Fernández-Ladreda M, Debray FG, Bours V, Beckers A. Reproduction, smell, and neurodevelopmental disorders: genetic defects in different hypogonadotropic hypogonadal syndromes. Front Endocrinol (Lausanne) 2014;5:109. doi: 10.3389/fendo.2014.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huhtaniemi I. A short evolutionary history of FSH-stimulated spermatogenesis. Hormones (Athens) 2015;14(4):468–478. doi: 10.14310/horm.2002.1632. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.