Abstract
The aim of the present meta-analysis study was to evaluate the efficacy of low-dose aspirin, commenced at ≤16 weeks of gestation, in preventing preterm and term preeclampsia, as well as associated maternal and neonatal adverse events in women at risk of preeclampsia. The Embase, PubMed, Cochrane Central Register of Controlled Trials and the Web of Science databases were searched for relevant random controlled trials (RCTs) published between January 1979 and October 2017. After quality assessment and data extraction, a meta-analysis was performed using RevMan 5.3 software. Outcomes of interest were preeclampsia with subgroups of preterm preeclampsia (delivery at <37 weeks) and term preeclampsia, as well as maternal adverse outcomes, including gestational hypertension, postpartum hemorrhage and preterm birth, and neonatal adverse outcomes, including intrauterine growth retardation (IUGR) or small for gestation age infant (SGA), stillbirth or death, and newborn weight. A total of 10 RCTs involving 3,168 participants were included. The meta-analysis demonstrated that, compared with placebo or no treatment, low-dose aspirin was associated with a significant reduction in the overall risk ratio (RR) of preeclampsia regardless of the time to delivery [RR=0.67; 95% confidence interval (CI)=0.57–0.80]. This was apparent for preterm preeclampsia (RR=0.35; 95% CI=0.13–0.94) but not for term preeclampsia (RR=1.01; 95% CI=0.60–1.70). Except for postpartum hemorrhage, low-dose aspirin also significantly reduced the risk of maternal and neonatal adverse outcomes. In conclusion, low-dose aspirin in women at risk of preeclampsia, commenced at ≤16 weeks of gestation, was associated with a reduced risk of preterm preeclampsia, and of adverse maternal and neonatal outcomes.
Keywords: preeclampsia, low-dose aspirin, meta-analysis
Introduction
Preeclampsia is characterized by development of hypertension and proteinuria after 20 weeks of gestation, and is considered to be a multisystem disorder associated with pregnancy. Worldwide, >70,000 maternal deaths per annum are associated with hypertensive disorders arising during pregnancy, mainly preeclampsia (1). Preeclampsia is also associated with increased long-term cardiovascular mortality for mother and infant (2).
In 1979, Crandon and Isherwood (3) first reported that patients who had taken aspirin during pregnancy were less likely to suffer from preeclampsia than those who had not. Over subsequent decades, >50 trials and 27 meta-analyses have investigated the use of low-dose aspirin for the prevention of preeclampsia. However, based on the results provided by high-quality, multicenter randomized controlled trials (RCTs) involving a large number of women and of systematic reviews, the efficacy of aspirin in reducing preeclampsia and associated outcomes remains controversial (4–7). Of note, the effectiveness of low-dose aspirin in preventing preeclampsia may be associated with the time-point of treatment initiation. The World Health Organization recommend that administration of low-dose aspirin (75 mg/day) for the prevention of preeclampsia in high-risk females should start during early pregnancy (8).
Recently, a multicenter, double-blinded, placebo-controlled trial including 1,776 women with singleton pregnancies who received low-dose aspirin or placebo from early gestation until 36 weeks of gestation indicated that aspirin decreases the incidence of preterm preeclampsia. However, no significant differences were identified between groups regarding the incidence of neonatal adverse outcomes or other adverse events (7). Therefore, it is possible that early use of aspirin may be more effective in preventing preterm than term preeclampsia, or in preventing other adverse outcomes. It is important to better understand the effects of aspirin associated with this indication, as it is currently the best option for improving outcomes for females at risk of preeclampsia and associated adverse sequelae. The aim of the present study was to evaluate the efficacy of low-dose aspirin administration to females at risk of preeclampsia commenced at ≤16 weeks of gestation in preventing preeclampsia, including preterm and term preeclampsia, as well as the impact on associated maternal and neonatal adverse events.
Materials and methods
Search strategy
In the present study, a systematic review and meta-analysis of RCTs that evaluated the effect of aspirin intake during pregnancy was performed. Relevant citations from January 1979 until October 2017 were extracted from the Embase, PubMed, Cochrane Central Register of Controlled Trials and Web of Science databases. A combination of keywords and MeSH terms was used for the search: ‘aspirin’, ‘antiplatelet’, ‘acetylsalicylic acid’, ‘ASA’, ‘pregnancy-complication’, ‘pregnancy’, ‘eclampsia’, ‘hypertens*’, ‘blood press*’, ‘*eclamp*’, ‘PIH’ and ‘toxemia’. No language restriction was imposed. A first reviewer sorted all articles by citations and abstract for more detailed evaluation. Two independent reviewers then selected relevant abstracts and citations for complete evaluation of the studies. The quality of this review was validated according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (9).
Selection criteria
Only prospective, randomized controlled trials were included. The included population was pregnant females at risk of preeclampsia who were randomized into a low-dose aspirin and a placebo or no treatment group, at ≤16 weeks of gestation. Low-dose aspirin was defined as 50–150 mg daily. The following exclusion criteria were applied: Trials with i) no control group; ii) incomplete data or no data; and iii) repeated studies on the same subjects. Each potentially eligible study was assessed independently by at least two researchers and the risk of bias of the studies was evaluated using the Cochrane Handbook for Systematic Reviews of Interventions (10). Discrepancies were resolved by discussion or by consultation with a third reviewer.
Outcomes
The primary outcome was preeclampsia (hypertension with new-onset proteinuria at ≥20 weeks of gestation regardless of delivery time) and its subcategories: Preterm preeclampsia (delivered at <37 weeks) and term preeclampsia. Secondary outcomes were other maternal adverse events, including gestational hypertension, preterm birth (delivered at <34 weeks) and postpartum hemorrhage, as well as neonatal adverse events, including intrauterine growth retardation (IUGR), infant small for gestational age (SGA), stillbirth or infant death, and newborn weight.
Statistical analysis
The data were analyzed using RevMan 5.3 software (The Cochrane Collaboration, London, UK). The significance threshold for the chi-square test was set at α=0.1, and it was deemed that heterogeneity existed when P<0.1. Heterogeneity between studies was determined by calculating the Higgins I2 value and considered high if it was ≥50%. The individual risk ratio (RR) and 95% confidence intervals (CI) were estimated using a fixed-effects model if no heterogeneity existed; otherwise, the random-effects model was used. Publication bias was tested by visual inspection of funnel plots generated using a Begg's test.
Results
Study selection and evaluation
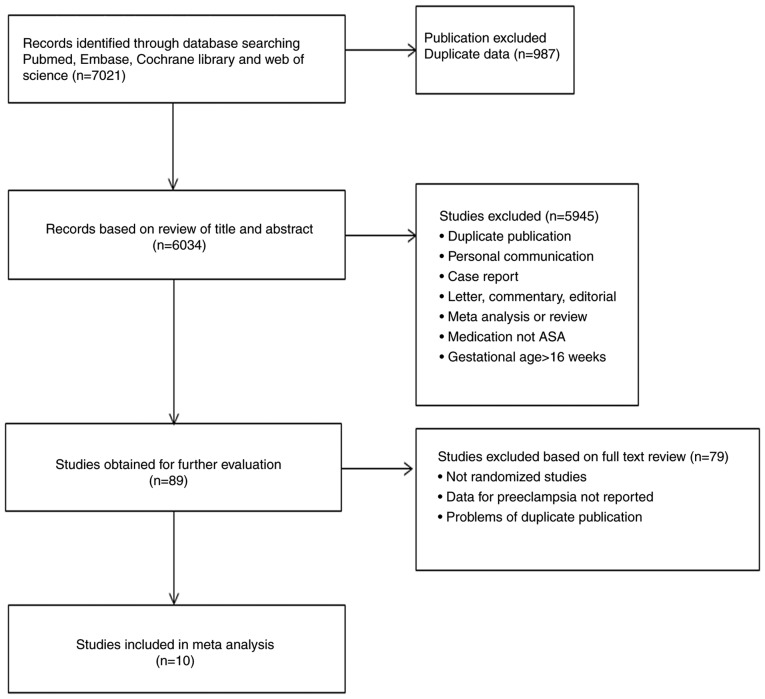
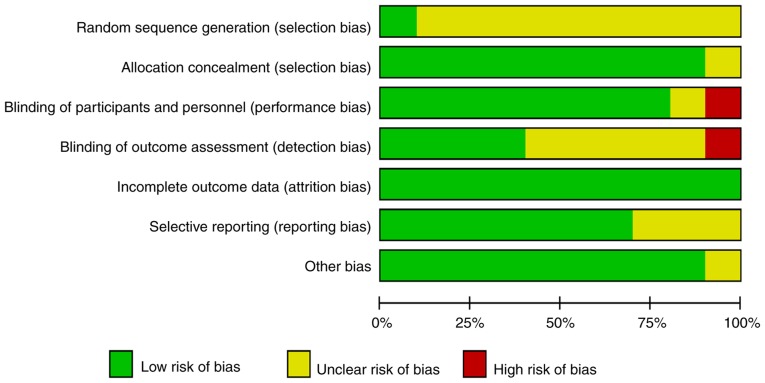
Fig. 1 displays the flowchart of the study selection process. The initial 7,021 identified citations were reduced to 6,932 following review for duplicated publications and of the title and abstract against the inclusion criteria. The full text of the remaining 89 studies was evaluated, resulting in the exclusion of a further 79 studies. The remaining 10 RCTs comprising 3,168 participants were included, including 1,581 patients treated with low-dose aspirin and 1,587 who received placebo or no treatment. The details of the regimens are listed in Table I. No publication bias was identified by the funnel plot method on the basis of data on the total rate of efficacy (Fig. 2). In addition the quality of RCTs was assessed by The Cochrane Collaboration's tool for assessing risk of bias (Fig. 3). The majority of studies used the correct allocation concealment strategies, reported incomplete outcome data and were double-blind. A moderate number of studies were randomized incorrectly in sequence generation and were not blinded to the outcome assessment.
Figure 1.
Flowchart depicting the method of study selection. ASA, acetylsalicylic acid.
Table I.
Characteristics of randomized controlled trials.
| Study (year) | Gestation age (weeks) | N | Inclusion criteria | Intervention | Outcomes | (Refs.) |
|---|---|---|---|---|---|---|
| Ayala et al (2013) | ≤16 | 350 | Pregnant women with higher risk for gestational hypertension or preeclampsia | ASA 100 mg/d vs. placebo | PE; preterm birth; IUGR; stillbirth; newborn weight; Apgar score; gestational hypertension; postpartum hemorrhage | (27) |
| Bakhti and Vaiman (2011) | 8–10 | 164 | Women without previous vasculo-renal pathology | ASA 100 mg/d vs. no treatment | Preterm PE; PE; IUGR; gestation hypertension; postpartum hemorrhage; stillbirth; preterm birth; newborn weight | (28) |
| Benigni et al (1989) | 12 | 33 | Women with hypertension or previous obstetrical history: Fetal death, severe IUGR, early onset of preeclampsia | ASA 60 mg/d vs. placebo | PE; gestational hypertension; preterm birth; IUGR; perinatal death; newborn weight | (29) |
| Caritis et al (1998) | 13–16 | 523 | Women with diabetes mellitus, chronic hypertension or a history of PE | ASA 60 mg/d vs. placebo | PE; IUGR; newborn weight. | (30) |
| Chiaffarino et al (2004) | <14 | 35 | Women with chronic hypertension, history of severe pre-eclampsia or eclampsia or IUGR or intrauterine fetal death | ASA 100 mg/d vs. no treatment | PE; gestational hypertension; abortion; birth weight | (31) |
| Ebrashy et al (2005) | 14–16 | 139 | A high-risk factor for preeclampsia or IUGR, including previous history of the disease, essential hypertension, family history of or underlying vascular disorder, maternal age <20 or >40 years, and gestational diabetes mellitus | ASA 75 mg/d vs. no treatment | Preterm PE; PE; IUGR; preterm birth; apgar score; maternal hemorrhage; newborn weight | (32) |
| Hermida et al (1997) | 12–16 | 100 | Women with risk factors of pre-eclampsia: Family or own history of gestational hypertension or PE, chronic HT, cardiovascular or endocrine problem, bleeding or endocrine disease | ASA 100 mg/d vs. placebo | PE; gestational hypertension; preterm birth; IUGR; perinatal death; birth weight | (33) |
| Rolnik et al (2017) | 11–14 | 1,620 | Women with high risk high risk (>1 in 100) for preterm preeclampsia according to the screening algorithm | ASA 150 mg/d vs. placebo | Preterm PE; PE; gestational hypertension; preterm birth; stillbirth; abruption; SGA | (7) |
| Vainio et al (2002) | 12–14 | 86 | Women considered to be at high risk of preeclampsia or intrauterine growth retardation were screened by transvaginal Doppler ultrasound | ASA 0.5 mg/kg/d vs. placebo | Preterm PE; PE; gestational hypertension; preterm birth; stillbirth; abruption; SGA | (34) |
| Villa et al (2013) | 12–13 | Women with risk factors for pre-eclampsia or abnormal uterine artery Doppler velocimetry | ASA 100 mg/d vs. placebo | Preterm PE; PE; gestational hypertension; newborn birthweight; Apgar score | (35) |
ASA, acetylsalicylic acid; PE, preeclampsia; IUGR, intrauterine growth retardation; SGA, small for gestation age infant; d, day.
Figure 2.
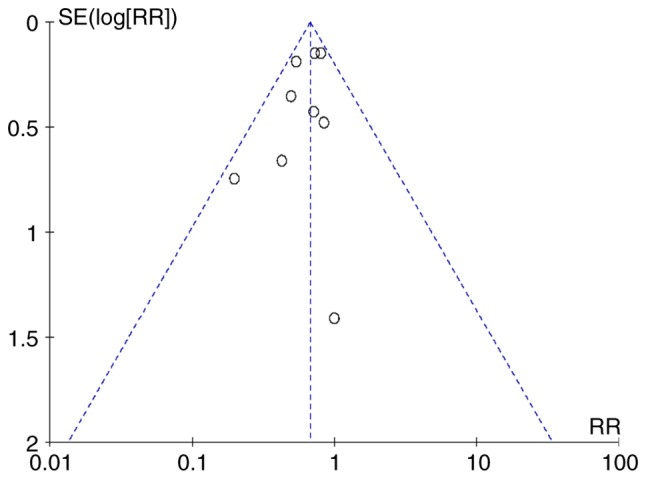
Funnel plot of publication bias. RR, risk ratio. SE, standard error.
Figure 3.
Summary risk of bias assessment according to the Cochrane handbook.
Low-dose aspirin commenced at ≤16 weeks of gestation reduces in the risk of preeclampsia
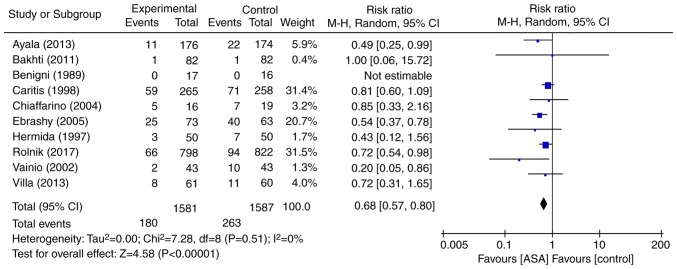
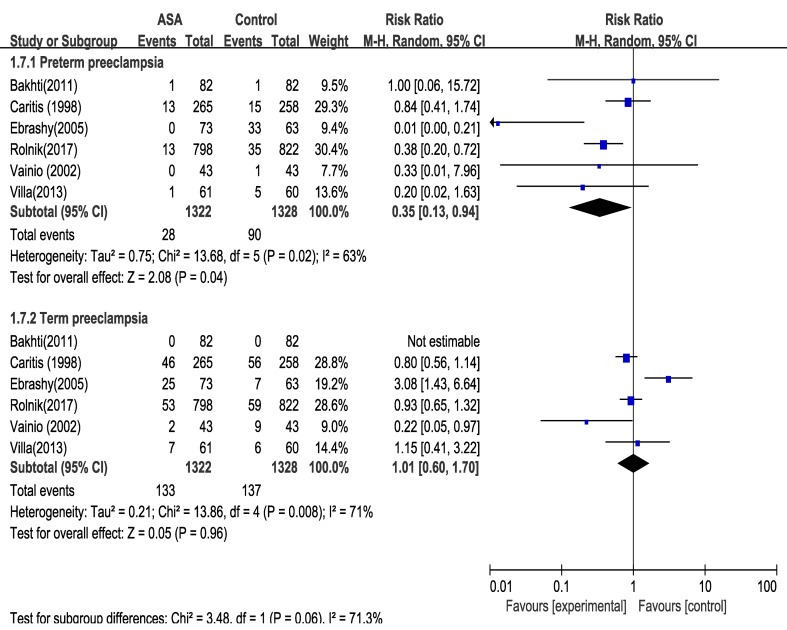
All 10 RCTs evaluated the effect of low-dose aspirin for the prevention of preeclampsia irrespective of the time to delivery (Fig. 4). As no heterogeneity was identified (P=0.51, I2=0%), the fixed-effects model was used for the meta-analysis. The results indicated that, compared with placebo or no treatment, low-dose aspirin was associated with a 33% reduction in the relative risk of preeclampsia regardless of the time to delivery (RR=0.68, 95% CI=0.57–0.80; P<0.0001). Next, the efficacy in the two subgroups of preterm and term preeclampsia was evaluated (Fig. 5). Analysis of the data from 6 RCTs indicated that low-dose aspirin, administered at ≤16 weeks of gestation, was associated with a 65% reduction in the risk of preterm preeclampsia. By contrast, no reduction in the relative risk of term preeclampsia by administration of low-dose aspirin was obtained (RR=1.01; 95% CI=0.60–1.70).
Figure 4.
Forest plot of the effect of low-dose aspirin on the risk of preeclampsia. df, degrees of freedom; M-H, Mantel-Haenszel; CI, confidence interval; ASA, acetylsalicylic acid. Black diamonds indicate the weight of each study; blue squares indicate the overall result; horizontal lines indicate the sample size of the studies.
Figure 5.
Forest plots of the effect of low-dose aspirin on the risk of preterm preeclampsia and term preeclampsia. df, degrees of freedom; M-H, Mantel-Haenszel; CI, confidence interval; ASA, acetylsalicylic acid. Black diamonds indicate the weight of each study; blue squares indicate the overall result; horizontal lines indicate the sample size of the studies.
Low-dose aspirin commenced at ≤16 weeks of gestation reduces in the risk of gestational hypertension and preterm birth
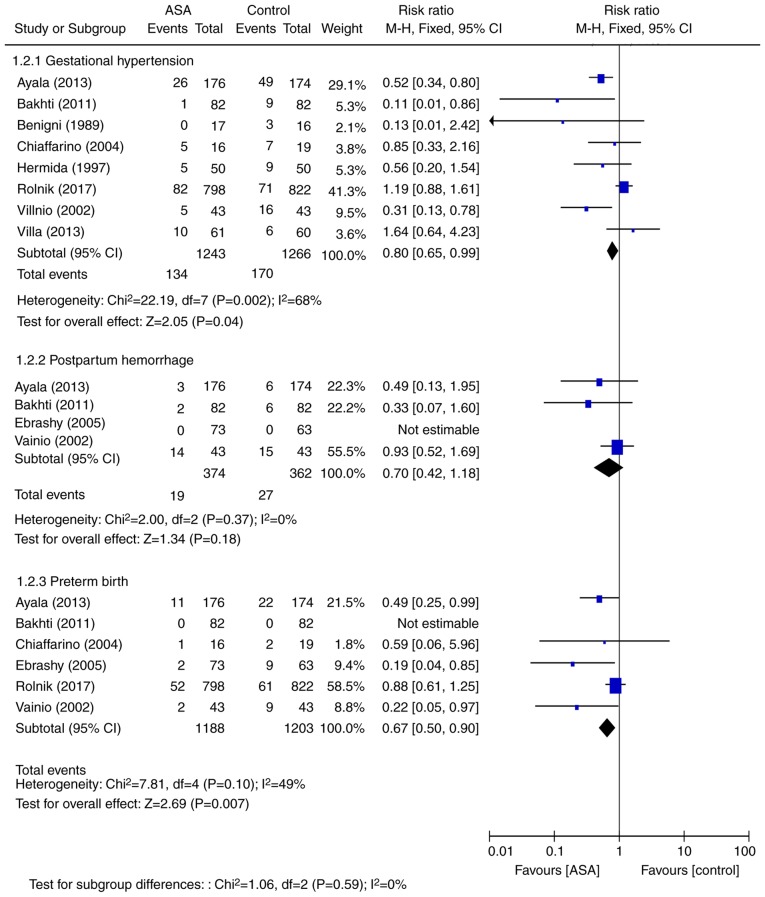
As no heterogeneity was identified (P=0.59, I2=0%), the fixed-effects model was used for the meta-analysis. The results for the other maternal adverse outcomes are presented in Fig. 6. A total of 9 RCTs comprising 2,508 cases reported on gestational hypertension, with results indicating a 20% reduction in the RR of gestational hypertension with aspirin (RR=0.80, 95% CI=0.65–0.99; P=0.0400). Similarly, meta-analysis of the results from 6 RCTs comprising 2,391 cases indicated a 23% reduction in the RR for preterm birth (RR=0.67, 95% CI=0.50–0.90; P=0.0070). The results obtained from 4 RCTs comprising 736 maternal patients suggested a 30% reduction in the likelihood of postpartum hemorrhage (RR=0.70, 95% CI=0.42–1.18; P=0.18), however this was not significant.
Figure 6.
Forest plots of the effect of low-dose aspirin on the risk of maternal adverse outcomes. df, degrees of freedom; M-H, Mantel-Haenszel; CI, confidence interval; ASA, acetylsalicylic acid. Black diamonds indicate the weight of each study; blue squares indicate the overall result; horizontal lines indicate the sample size of the studies.
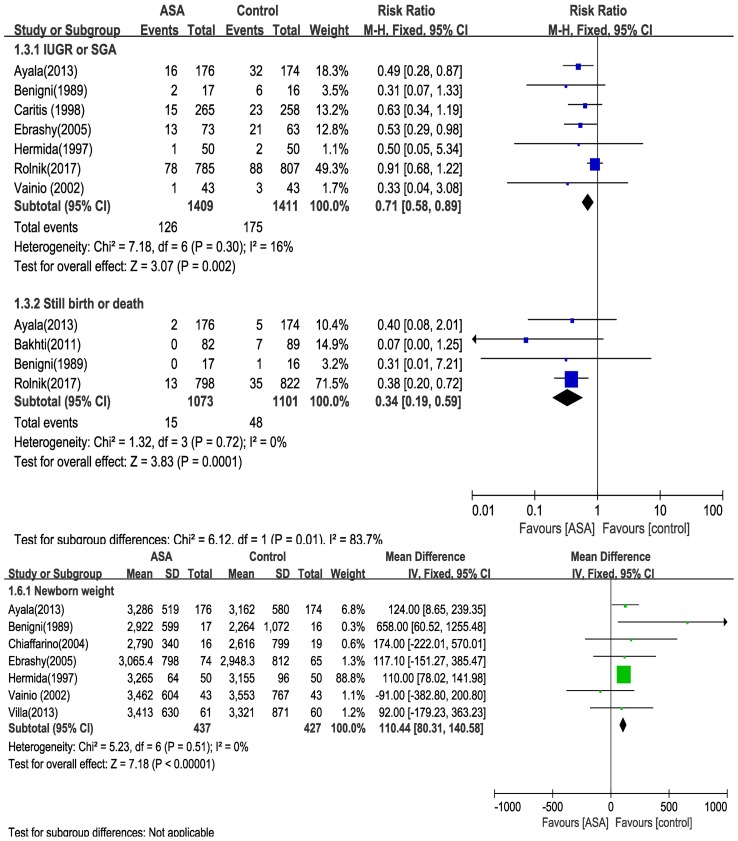
Low-dose aspirin commenced at ≤16 weeks of gestation reduces in the risk of neonatal adverse outcomes
As no heterogeneity was identified (IUGR or SGA, I2=0%; still birth or mortality, I2=0%; newborn weight, I2=0%, respectively), the fixed-effects model was used for the meta-analysis. Neonatal adverse outcomes are presented in Fig. 7. Meta-analysis of the results from 7 RCTs comprising 2,820 maternal patients suggested that aspirin reduced the risk of IUGR or SGA (RR=0.71; 95% CI=0.58–0.89; P=0.0040). Furthermore, analysis of the data of 4 RCTs involving 2,174 maternal patients suggested fewer still births or deaths associated with aspirin intake (RR=0.34, 95% CI=0.19–0.59; P=0.0001). In addition, data on 864 infants suggested that aspirin intake during pregnancy was associated with an increased newborn weight by 110.44 g (95% CI=80.31–140.58 g; P<0.0001) in the setting of maternal risk of preeclampsia.
Figure 7.
Forest plots of the effect of low-dose aspirin initiated on the risk of neonatal adverse outcomes. df, degrees of freedom; M-H, Mantel-Haenszel; CI, confidence interval; ASA, acetylsalicylic acid; IUGR, intrauterine growth retardation; SGA, small for gestation age infant; IV, inverse variance. Black diamonds indicate the weight of each study; blue squares indicate the overall result; horizontal lines indicate the sample size of the studies.
Overall, low-dose aspirin administration at ≤16 weeks of gestation to women at risk of preeclampsia was associated with a reduction in maternal and neonatal adverse outcomes, compared with placebo or no treatment. Aspirin administration was also associated with an improvement of fetal growth.
Discussion
The present systematic review and meta-analysis was restricted to RCTs that assessed outcomes of low-dose aspirin administration commenced at ≤16 weeks of gestation in females at risk of preeclampsia. The outcomes were preeclampsia (including two subgroups of preterm and term preeclampsia), as well as maternal adverse outcomes, including gestational hypertension, postpartum hemorrhage and preterm birth, and neonatal adverse outcomes, including IUGR or SGA, stillbirth or death, and newborn weight. The inclusion criteria were met by 10 RCTs comprising a total of 3,168 female patients. The meta-analysis revealed a major beneficial effect of low-dose aspirin, commenced at ≤16 weeks of gestation, on the risk of preeclampsia regardless of the time to delivery (RR=0.68; 95% CI=0.57–0.80). This appeared mainly due to a reduction in preterm preeclampsia (RR=0.35; 95% CI=0.13–0.94), as low-dose aspirin was not associated with any significant reduction in the risk of term preeclampsia. Furthermore, maternal adverse outcomes, including gestational hypertension and preterm birth, and neonatal adverse outcomes, including IUGR or SGA, stillbirth or infant death, and newborn weight, were improved by maternal aspirin intake.
In recent decades, the ability of antiplatelet agents to prevent or delay preeclampsia and its complications has been widely tested in numerous studies. While various studies have reported significant benefits (11–13), others have not (14–16). In the present study, the efficacy of low-dose aspirin therapy in maternal patients at risk of preeclampsia commenced at ≤16 weeks of gestation was assessed regarding the prevention of preeclampsia and the results of the meta-analysis were similar to those observed in a previous meta-analysis of individual patient data, which indicated a moderate but consistent reduction in the RR for maternal and neonatal adverse events (4). A recent multicenter, double-blind, placebo-controlled trial of 1,776 women with singleton pregnancies at high risk for preterm preeclampsia demonstrated that low dose aspirin significantly reduced the incidence of this diagnosis compared with the placebo (7). In the present study randomized controlled trials were selected that met the indicated inclusion criteria, including this recent study. The results of the present study supported those of previous studies, demonstrating that the use of aspirin commenced at ≤16 weeks of gestation may be particularly effective in preventing preeclampsia.
Although the exact underlying cause of preeclampsia remains to be fully elucidated, it is widely accepted that abnormalities including angiogenesis, oxidative stress and inflammation are involved. To date, numerous attempts at primary and secondary prevention of preeclampsia using various supplements and medications, including anti-hypertensives (17), calcium (18), or the antioxidants vitamins C and E (19), have failed. Pilot studies suggest a promising beneficial effect of pravastatin (20). However, its benefits (and safety in pregnancy) require investigation in a large and well-designed RCT with a sample size that is sufficiently large to achieve high statistical power, prior to its implementation in routine clinical practice.
Normal implantation and placentation are critical for a successful pregnancy. It is thought that the first wave of trophoblast invasion is already complete by around 10 weeks of gestation and continues until the 20th week (21). It is also known that aspirin exerts beneficial effects on endothelial function, as well as early formation and development of the placenta (22,23). Bujold et al (24) reported that administration of low-dose aspirin commenced at ≤16 weeks of gestation significantly decreases the risk of preeclampsia and other adverse maternal and neonatal outcomes, whereas the effect is not present with later commencement of aspirin. However, a recent meta-analysis reported a consistent effect of low-dose aspirin on preeclampsia and its complications regardless of whether it was started prior to or after 16 weeks of gestation (25). These conflicting results may be due to different inclusion criteria, and of note, the latter review included participants who received one or more antiplatelet agents (e.g., dipyridamole or low-molecular-weight heparin). Furthermore, in the latter meta-analysis of individual participant data, studies were selected where antiplatelet agent initiation was not restricted to the first 16 weeks of pregnancy, thereby including more studies.
The present result that low-dose aspirin reduced the risk of maternal and neonatal adverse outcomes is compatible with an earlier meta-analysis, which indicated that antiplatelet agents achieved reductions in preterm birth, SGA and other adverse maternal and fetal outcomes (4). The major limitation of the present meta-analysis was the small number of studies included. In particular, the presence of heterogeneity for maternal and newborn adverse outcome suggests variance between the included studies. The presence of heterogeneity (I2=68%) for gestational hypertension and heterogeneity (I2=83.7%) for subgroup analyses in IUGR or SGA and still birth or death, suggested the presence of a variance between the included studies. Females in the present small trial appeared to have a larger than average reduction in the risk ratio for adverse events. The recognition of bias from small trials is well known and these outcomes should be interpreted with caution (26).
In conclusion, the present meta-analysis indicated that initiation of low-dose aspirin commenced at ≤16 weeks of gestation resulted in a 33% decrease in the occurrence of preeclampsia, mostly due to a 63% reduction of preterm preeclampsia, although this change was not significant. However, low-dose aspirin had no effect on the risk of term preeclampsia. The present study also indicated that aspirin produced significant reductions in maternal and neonatal adverse events. The most likely explanation for these results is that early administration of low-dose aspirin improves early formation and development of the placenta. This should be discussed with women at risk of developing preeclampsia to help them make informed choices regarding their antenatal care. However, the potential benefit of low-dose aspirin regarding the prevention of preeclampsia, as well as associated maternal and neonatal adverse outcomes, remains controversial. Additional clinical trials of higher quality and with a larger sample size are necessary to further verify the effectiveness of aspirin for this indication.
Acknowledgements
The authors thank Dr Zhi Wang and Dr Yifang Zhu in the Department of Health and Human Services, Yiwu Maternity and Children Health Care Hospital for their assistance.
Funding
No funding received.
Availability of data and materials
The analyzed data sets generated during the study are available from the corresponding author on reasonable request.
Authors' contributions
FZ designed the study and checked the results. YC and BZ performed the experiments and analyzed the data. The final version of the manuscript was read and approved by all authors.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376:631–644. doi: 10.1016/S0140-6736(10)60279-6. [DOI] [PubMed] [Google Scholar]
- 2.Tooher J, Thornton C, Makris A, Ogle R, Korda A, Horvath J, Hennessy A. Hypertension in pregnancy and long-term cardiovascular mortality: A retrospective cohort study. Am J Obstet Gynecol. 2016;214:722.e1–6. doi: 10.1016/j.ajog.2015.12.047. [DOI] [PubMed] [Google Scholar]
- 3.Crandon AJ, Isherwood DM. Effect of aspirin on incidence of pre-eclampsia. Lancet. 1979;1:1356. doi: 10.1016/S0140-6736(79)91996-2. [DOI] [PubMed] [Google Scholar]
- 4.Askie LM, Duley L, Hendersonsmart DJ, Stewart LA. PARIS Collaborative Group: Antiplatelet agents for prevention of pre-eclampsia: A meta-analysis of individual patient data. Lancet. 2007;369:1791–1798. doi: 10.1016/S0140-6736(07)60712-0. [DOI] [PubMed] [Google Scholar]
- 5.Groeneveld E, Lambers MJ, Lambalk CB, Broeze KA, Haapsamo M, de Sutter P, Schoot BC, Schats R, Mol BW, Hompes PG. Preconceptional low-dose aspirin for the prevention of hypertensive pregnancy complications and preterm delivery after IVF: A meta-analysis with individual patient data. Hum Reprod. 2013;28:1480–1488. doi: 10.1093/humrep/det022. [DOI] [PubMed] [Google Scholar]
- 6.CLASP: A randomized trial of low-dose aspirin for the prevention and treatment of pre eclampsia among 9364 pregnant-women. CLASP (Collaborative Low-dose Aspirin Study in Pregnancy) Collaborative Group. Lancet. 1994;343:619–629. doi: 10.1016/S0140-6736(94)92633-6. [DOI] [PubMed] [Google Scholar]
- 7.Rolnik DL, Wright D, Poon LC, O'Gorman N, Syngelaki A, de Paco Matallana C, Akolekar R, Cicero S, Janga D, Singh M, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377:613–622. doi: 10.1056/NEJMoa1704559. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization (WHO): WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia. WHO; Geneva: 2011. [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group: Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green S, editor. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series. Wiley-Blackwell; 2008. [DOI] [Google Scholar]
- 11.Roberge S, Nicolaides K, Demers S, Hyett J, Chaillet N, Bujold E. The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: Systematic review and meta-analysis. Am J Obstet Gynecol. 2017;216:110–120.e6. doi: 10.1016/j.ajog.2016.09.076. [DOI] [PubMed] [Google Scholar]
- 12.Roberge S, Nicolaides KH, Demers S, Villa P, Bujold E. Prevention of perinatal death and adverse perinatal outcome using low-dose aspirin: A meta-analysis. Ultrasound Obstet Gynecol. 2013;41:491–499. doi: 10.1002/uog.12421. [DOI] [PubMed] [Google Scholar]
- 13.Henderson JT, Whitlock EP, O'Conner E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: A systematic evidence review for the U.S. preventive services task force. Ann Intern Med. 2014;160:695–703. doi: 10.7326/M13-2844. [DOI] [PubMed] [Google Scholar]
- 14.Roberge S, Sibai B, McCaw-Binns A, Bujold E. Low-dose aspirin in early gestation for prevention of preeclampsia and small-for-gestational-age neonates: Meta-analysis of large randomized trials. Am J Perinatol. 2016;33:781–785. doi: 10.1055/s-0036-1572495. [DOI] [PubMed] [Google Scholar]
- 15.Bergeron TS, Roberge S, Carpentier C, Sibai B, Mccaw-Binns A, Bujold E. Prevention of preeclampsia with aspirin in multiple gestations: A systematic review and meta-analysis. Am J Perinatol. 2016;33:605–610. doi: 10.1055/s-0035-1570381. [DOI] [PubMed] [Google Scholar]
- 16.Meher S, Alfirevic Z. Aspirin for pre-eclampsia: Beware of subgroup meta-analysis. Ultrasound Obstet Gynecol. 2013;41:479–485. doi: 10.1002/uog.12470. [DOI] [PubMed] [Google Scholar]
- 17.Abalos E, Duley L, Steyn DW, Henderson-Smart DJ. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev: Cd002252. 2007 doi: 10.1002/14651858.CD002252.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Levine RJ, Hauth JC, Curet LB, Sibai BM, Catalano PM, Morris CD, DerSimonian R, Esterlitz JR, Raymond EG, Bild DE, et al. Trial of calcium to prevent preeclampsia. N Engl J Med. 1997;337:69–76. doi: 10.1056/NEJM199707103370201. [DOI] [PubMed] [Google Scholar]
- 19.Conde-Agudelo A, Romero R, Kusanovic JP, Hassan SS. Supplementation with vitamins C and E during pregnancy for the prevention of preeclampsia and other adverse maternal and perinatal outcomes: a systematic review and metaanalysis. Am J Obstet Gynecol. 2011;204:503.e1–12. doi: 10.1016/j.ajog.2011.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Costantine MM, Cleary K, Hebert MF, Ahmed MS, Brown LM, Ren Z, Easterling TR, Haas DM, Haneline LS, Caritis SN, et al. Safety and pharmacokinetics of pravastatin used for the prevention of preeclampsia in high-risk pregnant women: a pilot randomized controlled trial. Am J Obstet Gynecol. 2016;214:720.e1–720.e17. doi: 10.1016/j.ajog.2015.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Knöfler M, Pollheimer J. IFPA award in placentology lecture: Molecular regulation of human trophoblast invasion. Placenta. 2012;33(Suppl):S55–S62. doi: 10.1016/j.placenta.2011.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quyyumi AA. Effects of aspirin on endothelial dysfunction in atherosclerosis. Am J Cardiol. 1998;82:31S–33S. doi: 10.1016/S0002-9149(98)00673-0. [DOI] [PubMed] [Google Scholar]
- 23.Tarim E, Bal N, Kilicdag E, Kayaselcuk F, Bağiş T, Kuscu E. Effects of aspirin on placenta and perinatal outcomes in patients with poor obstetric history. Arch Gynecol Obstet. 2006;274:209–214. doi: 10.1007/s00404-006-0162-y. [DOI] [PubMed] [Google Scholar]
- 24.Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, Forest JC, Giguère Y. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: A meta-analysis. Obstet Gynecol. 2010;116:402–414. doi: 10.1097/AOG.0b013e3181e9322a. [DOI] [PubMed] [Google Scholar]
- 25.Meher S, Duley L, Hunter K, Askie L. Antiplatelet therapy before or after 16 weeks' gestation for preventing preeclampsia: an individual participant data meta-analysis. Am J Obstet Gynecol. 2017;216:121–128.e2. doi: 10.1016/j.ajog.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 26.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. John Wiley & Sons; Hoboken, NJ: 2009. [DOI] [Google Scholar]
- 27.Ayala DE, Ucieda R, Hermida RC. Chronotherapy with low-dose aspirin for prevention of complications in pregnancy. Chronobiol Int. 2013;30:260–279. doi: 10.3109/07420528.2012.717455. [DOI] [PubMed] [Google Scholar]
- 28.Bakhti A, Vaiman D. Prevention of gravidic endothelial hypertension by aspirin treatment administered from the 8th week of gestation. Hypertens Res. 2011;34:1116–1120. doi: 10.1038/hr.2011.111. [DOI] [PubMed] [Google Scholar]
- 29.Benigni A, Gregorini G, Frusca T, Chiabrando C, Ballerini S, Valcamonico A, Orisio S, Piccinelli A, Pinciroli V, Fanelli R, et al. Effect of low-dose aspirin on fetal and maternal generation of thromboxane by platelets in women at risk for pregnancy-induced hypertension. N Engl J Med. 1989;321:357–362. doi: 10.1056/NEJM198908103210604. [DOI] [PubMed] [Google Scholar]
- 30.Caritis S, Sibai B, Hauth J, Lindheimer MD, Klebanoff M, Thom E, VanDorsten P, Landon M, Paul R, Miodovnik M, et al. Low-dose aspirin to prevent preeclampsia in women at high risk National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;338:701–705. doi: 10.1056/NEJM199803123381101. [DOI] [PubMed] [Google Scholar]
- 31.Chiaffarino F, Parazzini F, Paladini D, Acaia B, Ossola W, Marozio L, Facchinetti F, Del Giudice A. A small randomised trial of low-dose aspirin in women at high risk of pre-eclampsia. Eur J Obstet Gynecol Reprod Biol. 2004;112:142–144. doi: 10.1016/S0301-2115(03)00269-0. [DOI] [PubMed] [Google Scholar]
- 32.Ebrashy A, Ibrahim M, Marzook A, Yousef D. Usefulness of aspirin therapy in high-risk pregnant women with abnormal uterine artery Doppler ultrasound at 14–16 weeks pregnancy: Randomized controlled clinical trial. Croat Med J. 2005;46:826–831. [PubMed] [Google Scholar]
- 33.Hermida RC, Ayala DE, Iglesias M, Mojón A, Silva I, Ucieda R, Fernández JR. Time-dependent effects of low-dose aspirin administration on blood pressure in pregnant women. Hypertension. 1997;30:589–595. doi: 10.1161/01.HYP.30.3.589. [DOI] [PubMed] [Google Scholar]
- 34.Vainio M, Kujansuu E, Iso-Mustajärvi M, Mäenpää J. Low dose acetylsalicylic acid in prevention of pregnancy-induced hypertension and intrauterine growth retardation in women with bilateral uterine artery notches. BJOG. 2002;109:161–167. doi: 10.1111/j.1471-0528.2002.01046.x. [DOI] [PubMed] [Google Scholar]
- 35.Villa PM, Kajantie E, Räikkönen K, Pesonen AK, Hämäläinen E, Vainio M, Taipale P, Laivuori H. PREDO Study group: Aspirin in the prevention of pre-eclampsia in high-risk women: A randomised placebo-controlled PREDO Trial and a meta-analysis of randomised trials. BJOG. 2013;120:64–74. doi: 10.1111/j.1471-0528.2012.03493.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The analyzed data sets generated during the study are available from the corresponding author on reasonable request.