Abstract
This study examined the frequency and type of CAM therapy, as well as characteristics associated with CAM usage. A survey about parental preferences and beliefs regarding CAM usage was distributed to 5 schools with predominantly low socioeconomic (SES) Vietnamese children. For the 360 Vietnamese children previously diagnosed with asthma whose families responded, most preferred conventional therapy as prescribed by the physician. The prevalence of CAM usage was 38.1%. Common CAM therapies were steam inhalation, creams/topical oils, foods, prayer, oil inhalation, massage, herbal medication, coining and cupping. Significant predictors of CAM usage were older age (11–12 years) (P=.038), English language of survey response of (p=.001), environmental tobacco smoke (ETS) exposure (P=.001), fear of long term medication usage, and perception of asthma as a condition related to genetics (p=.023). These findings suggest that assessing CAM therapy will provide a more holistic approach to asthma therapy.
Keywords: Vietnamese children, asthma, Asians, minority, low socioeconomic status, Complimentary and Alternative Medicine, holistic
Introduction
Asian Americans are one of the fastest growing groups in the United States (US), with Vietnamese being the fourth largest group among Asians (1, 2). Out of the more than 1.5 million Vietnamese living in the US, more than 1/3 live in Orange County California, serving as home to the largest Vietnamese community in America (1). However, few studies have characterized specific health related preferences and cultural beliefs as well as the use of Complementary and Alternative Medicine (CAM) in these Vietnamese families (3, 4) who often experience low socioeconomic status (SES) (1). These factors are obviously of great importance to health care providers who treat these patients. Among the chronic illnesses in the pediatric population, asthma is of great concern particularly in minority, low SES children. (5, 6) Previous surveys in Orange County have shown asthma to be a major health issue in Vietnamese children with a prevalence approaching 30%.(7, 8)
The high asthma burden in low SES minority populations may be a result of several potential barriers to good asthma management including economic and educational disadvantages, low English proficiency, lack of health insurance, and poor access to consistent medical care.(9, 10) For asthma these factors may play a role in the poor adherence to conventional therapy seen in this population.(11, 12) Another consideration for poor adherence in asthmatic children is the use of CAM, which is frequently undisclosed to the provider (3,12,13). For example, among Chinese and Vietnamese Americans only 7.6% of these patients had discussed their CAM usage with their clinician.(3) This is particularly important because CAM usage has been increasing, especially in children with respiratory disease. (14) In addition, CAM therapy has shown both promise in treating allergic disease (15) and has been reported to have potential serious side effects (16), information critical to the provider.
CAM therapy is defined by the National Center for Complementary and Alternative Medicine “as a group of diverse medical and healthcare systems, practices, and products that are not currently consistent with conventional medicine.” (14) The exact prevalence of CAM in asthmatic children is not known, as estimates vary between 33% to 89% (17). Although it has been suggested that the prevalence of CAM appears to be similar in different ethnic groups with some variation in specific CAM practices, (12) more recent reports indicate important ethnic differences in the prevalence and type of CAM therapy among Asian populations (3, 4). The purpose of this study was to characterize CAM usage and predictions of CAM therapy for Vietnamese asthmatic children living in Orange County, CA.
METHODS
Study Setting
The study took place in Orange County, California in a community known as “Little Saigon”, where Vietnamese Americans represent approximately 30% of the population in this area. Little Saigon encompasses the cities of Garden Grove and Westminster and is accepted as the largest population of Vietnamese residents outside of Vietnam. Five elementary schools were selected on the basis of the largest Vietnamese population and also the highest number of children eligible to receive free or reduced cost meals which was consistent with low SES. Children, ages 3–12 years, were surveyed between June 2011 and April 2012.
The study was part of the Vietnamese Children’s Asthma Project (VCAP), a partnership comprised of the American Academy of Pediatrics (local chapter), CalOptima, Children’s Hospital of Orange County (CHOC) Children’s Breathmobile, Orange County Asian and Pacific Islander Community Alliance, the Orange County Department of Education, Project Vietnamese Foundation, and the University of California, Irvine Department of Family Medicine. This group was developed in 2010 to address and understand the burden of asthma in Vietnamese children in Orange County.
Survey Tool
The study’s survey tool was initially based on a report by Ries et al., regarding the use of CAM in a largely immigrant Vietnamese population (18). Our survey was available in English and Vietnamese based on the diversity of students in the participating schools and the language preferences of their parents. The survey contained nine questions. The questions focused on what parents would choose given the option of using traditional Vietnamese providers and medication compared to conventional Western Medicine, and their comfort level with the choices for care. There were also questions about the use of CAM therapy. The survey for asthmatic children was further developed after we conducted focus group interviews with parents, teachers and health providers (19). Once developed and translated into Vietnamese by a certified translator, respectively, members of each community were consulted for wording and for back translation. Once the survey wording was validated, the survey was distributed to parents in English and Vietnamese. Parents were given the option to complete the survey in the language in which they were most comfortable.
Procedure
Study surveys were introduced to the schools during a “lunch and learn” session for teachers and staff. At these sessions teachers were educated about asthma and the details of the study. Teachers were informed that the surveys were to be sent home with students, and then returned to the classroom after the parents completed them. The survey with a cover letter was sent home with each child through the schools. An incentive of a $25 gift card was given to classrooms with greater than an 80% return rate, as a way of increasing survey return. Survey data were then entered into an Excel spreadsheet and analyzed using SPSS version 18.0. A random number generator distinguished surveys with identifying information removed from the database prior to analysis. The CHOC Children’s Hospital Institutional Review Board approved this study.
Statistical Analyses
Chi-square tests assessed significance of distributional differences in patient characteristics, treatment preferences for asthma, and related knowledge for Vietnamese children. An independent t-test assessed significance of difference in average age. Multivariable logistic regression analyses using stepwise selection of significant factors determined the combination of demographic characteristics, treatment preferences for asthma, and related knowledge items most predictive of CAM usage in Vietnamese children. A Forest plot was created to present adjusted odds ratios and corresponding 95% confidence intervals based on the final model. Analyses were performed using SPSS v18.0 (Chicago: SPSS Inc) on de-identified data.
RESULTS
Across the five schools, a total of 2,735 survey packets were distributed to enrolled students, and 2338 were returned for an overall return rate of 85.5%. Surveys returned reflected the overall student population of predominately Asian (68.7%) children. The majority of Asian children attending the five schools were of Vietnamese descent (97%). Demographics for Vietnamese children with a previous physician diagnosis of asthma are shown in Table 1. There were 360 Vietnamese children with a previous diagnosis of asthma and characteristics that included a mean age of 8.2 years, male gender 61.2%, parents living in the United States > 10 years 85%, and public health insurance 75.0%. In addition, environmental tobacco smoke (ETS) exposure was reported in 40.6% of Vietnamese homes, and English language proficiency was seen at 35.3%.
Table I.
Characteristics of 360 Vietnamese Students Previously Diagnosed With Asthma.
| Characteristics | Percentage |
|---|---|
| Age, years, mean (SD) | 8.2 (2.1) |
| Male | 61.2 |
| Parent time in the United States ≥10 years | 85.8 |
| Public health insurance coveragea | 75.0 |
| Smoker in household | 40.6 |
| English language of survey completion | 35.3 |
Specification of insurance categories: Public—Healthy families (n = 105), Medical (n = 163), no insurance (n = 2); Private—Private insurance (n = 5), work insurance (n = 79), not specified/multiple (n = 6).
Treatment preferences, asthma knowledge, and CAM use are shown in Table 2. In terms of treating chronic conditions such as asthma, a small number of parents (20.4%) used a combination of traditional and conventional therapy indicating that most families use only conventional therapy and give the medication as prescribed by the physicians (71.7%). However, 41.2% of families felt very uncomfortable giving daily medication for a chronic condition prescribed by their doctor, presumably because of concern about possible side effects of long term medication, (23.4%). In terms of route of administering asthma medication, the inhalation route was preferred, by meter dose inhaler or nebulizer (80.6%), rather than the oral route. For asthma knowledge, most indicated that asthma was caused by genetics (36.9%) and environmental factors (58.9%), with only 3.7% who thought hot and cold foods were related to asthma. Less than 50% of Vietnamese parents felt asthma should be treated only for symptoms rather than regularly. CAM usage (ever) was reported in38.1% of Vietnamese families. The percentage who reported use of only one type of CAM was 23.8% whereas 14.3% of Vietnamese families used two or more types of CAM.
Table 2.
Treatment Preference for Asthma and Related Knowledge Among Parents Whose Child Has Asthma Based on Prior Diagnosis (Vietnamese N = 360).
| Percentage | |
|---|---|
| Treatment preferences | |
| Preference for treating chronic conditions: | |
| Prefer traditional therapy combined with doctor recommendationa | 20.4 |
| Parent feels “very uncomfortable” about giving their child daily medication for a chronic condition prescribed by a doctor | 26.9 |
| Reason(s) that could keep parent from giving their child medications exactly the way a doctor prescribed it? | |
| 1. I always give medications exactly as instructed | 71.7 |
| 2. I’m afraid of the side effects or long-term effects | 23.4 |
| 3. My child feels better then I give less medication | 19.7 |
| 4. Costs of medication | 3.4 |
| 5. I give less because the medication is too strong | 2.9 |
| 6. I don’t understand the instructions | 1.4 |
| 7. My child feels worse then I give more medication | 0.9 |
| 8. I don’t understand why it was prescribed | 0.3 |
| Asthma medications come in many different forms, for treating your child’s asthma, which do you prefer? | |
| Inhalers—examples, Flovent, Albuterol, Ventolin | 64.2 |
| Nebulizers | 16.4 |
| Pills or tablets to take by mouth | 5.4 |
| Liquids to take by mouth | 14.0 |
| Asthma knowledge | |
| To the best of your knowledge, asthma is | |
| 1. A condition that only requires medication if there are symptoms (cough, trouble breathing, wheezing, etc) | 48.9 |
| 2. Genetic or inherited family condition | 36.9 |
| 3. Related to environment (dirt, dust, smoke, pollution) | 58.9 |
| 4. Related to cool and hot foods | 3.7 |
| Parent has used complementary and alternative (CAM) medicine | 38.1 |
Further specification of treatment preference categories: To use traditional home therapies (n = 5), to go to traditional healer (n = 4), combination with doctor recommendation (n = 62).
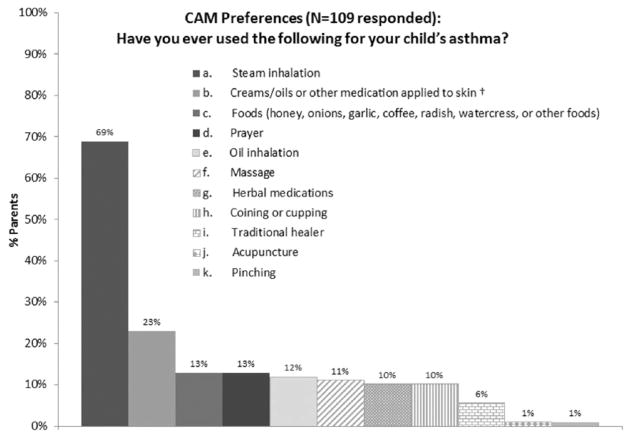
The type of CAM used is shown in rank order for those who reported the use of at least one CAM (Figure 1). The prevalence ranged from 69% for hot steam inhalation to 1% for pinching. The common CAM therapies also included creams/topical oils, foods, prayer, oil inhalation, massage, herbal medication, and coining/cupping. Less frequent (<10%) CAM therapies included traditional healing, acupuncture and pinching.
Figure 1.
Complementary and alternative medicine (CAM) preferences in response to “Have you ever used the following for your child’s asthma” (N = 109 reponses).
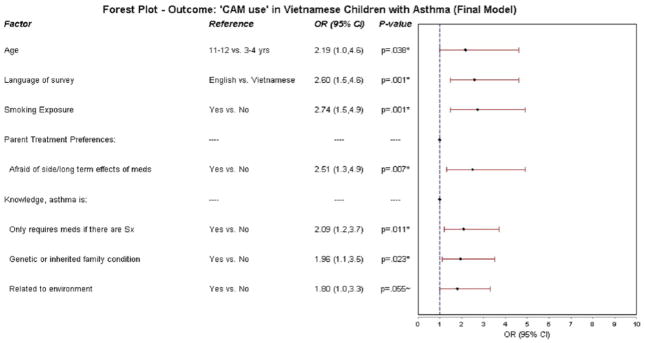
A Forest plot presents results from the multivariate analysis determining factors most predictive of CAM usage in Vietnamese children (Figure 2). Key factors included age 11–12 vs. 3–4 years with an odds ratio (OR) of 2.19 (1.0, 4.6) P=.038, language of survey response (English vs. Vietnamese, with an OR of 2.60 (1.6, 4.6) P=.001, ETS exposure with an OR of 2.74 (1.5, 1.9) P=.001, concerns about side effects/long term effects of medication with an OR of 2.51 (1.3, 1.9) P=.007, and asthma knowledge consisting of requiring medication when it is needed, and genetic or environmental factors with an OR ranging from 1.80 to 2.09, and P values ranging from 0.011 to 0.055.
Figure 2.
Forest plot outcome: “CAM use” in Vietnamese children with asthma (final model). CAM, complementary and alternative medicine.
DISCUSSION
We have examined the prevalence and characteristics of CAM usage in a community of predominately low SES asthmatic Vietnamese children residing in Orange County, California. A review of the current literature suggests that assessment of CAM therapy in Vietnamese asthmatic children has not been previously reported. We found that CAM usage was common in Vietnamese families with asthmatic children at 38.1%. The most common biologically-based CAMs were inhalation of steam and oil, topical applications of creams/oils, and herbal therapy; mind/body therapy-prayer; and body-based massage and coining/cupping. Less common were energy-based therapies such as acupuncture and therapeutic pinching (Figure 1).
Significant predictors of CAM seen in the multivariate analysis for the Vietnamese population included older children 11–12 years vs. 3–4 years, English response to the survey, ETS exposure, fear of medication side effects with long term use, and perception of asthma as requiring medication only as needed, as well as asthma being a genetic condition related to the environment. Asthma being related to hot and cold foods, a traditional concept of “upsetting the internal balance” (20) was not predictive.
CAM usage has increased particularly in children with respiratory illnesses, including asthma (21, 22). Although the exact prevalence in children has not been established, a meta- analysis by Slater and colleagues using selected studies with a more robust design suggested prevalence of 50 to 60% in asthmatic children (17). Their analysis suggests the factors which could influence prevalence include asthma severity, ethnicity, SES, gender, definition of CAM, sample size, response rate, and survey technique such as telephone, face to face interview, email survey and language used. In addition, others have suggested that those asthmatics using CAM are uninsured and have concerns about cost of asthma medication and potential adverse effects of long term asthma medication as seen in our study, and dissatisfaction with health care. (3, 23) CAM users also have increased healthcare utilization and generally poor asthma control (23, 24) the latter association not seen in our study. English proficiency can also be associated with CAM use (3, 4). Regarding ethnicity, although Adams suggested no major differences among ethnic groups, although the type of CAM can differ (12), several studies have shown significant differences in both the prevalence of CAM and specific CAM therapy. In Asian Americans there are differences reported along racial/ethnic lines for Vietnamese, Mandarin, and Cantonese Chinese (3, 4). For example, Vietnamese families have the highest usage among these three populations at 72%, while those speaking Mandarin Chinese were the lowest at 55%. The type of CAM usage can also differ although many similarities were seen in these Asian groups. Thus, although both Vietnamese and Chinese used acupuncture, and herbal medications, Vietnamese were more likely to use coining/cupping and massage (3) as seen in our study. In addition, CAM therapy in our study of Vietnamese asthmatic children included inhalation of both steam and oils, as well as topical oils/creams, food and prayer.
Comparison of our study with previous reports in terms of predictive characteristics is difficult since there is a paucity of data on CAM usage in Vietnamese asthmatic children. However, several comparisons are available in terms of predicting CAM. In terms of the English proficiency, we found in Vietnamese families that those responding in English had increased use of CAM. In previous reports Ahn found that English proficiency had no effect in predicting use of CAM (3), while Hsiao reported that those with decreased English proficiency were more likely to use CAM in several Asian cultures (4). Although at first glance our findings seem counter intuitive, since CAM use is generally greater in new immigrants (18), however, in recent years CAM has become more mainstream and popular among higher educated groups and Caucasian individuals (12). The other common finding in our study regarding prediction of CAM was the observation that concern about possible adverse effects of long term medication use increased the use of CAM, a finding shared by other investigators (23, 24). Unique predictive factors in our study included age (older vs. younger children), ETS exposure, and perception of asthma as a genetic and environmental disease. Another interesting finding was that the preferred route of administering asthma medication was by inhalation, the current conventional therapeutic approach (25), rather than the oral route as previously reported in an Asian population because of fear of dependency or addiction (26).
Several studies have expressed concern regarding safety of CAM. Most relevant is the concern that use of CAM may decrease adherence to conventional asthma therapy. Although some reports have shown decreased adherence related to CAM therapy (11, 12), a recent study by Philip and colleagues has shown that over a 3 year follow up period, the initiation of CAM was not associated with subsequent decreased adherence with conventional asthma therapy (14). Their explanation was that they encouraged the child and parent to view CAM as “complementary” rather than an alternative, thus creating an integrative approach. These authors stress that physicians should routinely ask about CAM in a non-judgmental fashion in order to manage their asthmatic patient in a more holistic manner. This would be a big step as illustrated by the fact that many patients do not disclose the use of CAM to their physician (3, 12, 13). Disclosure could be beneficial in the overall management of asthma. Thus, CAM therapy has actually been shown to be effective for asthma in acute placebo controlled randomized studies (15, 27). For example, Li reported that recent randomized control trials using traditional Chinese medicine (TCM) was both safe and effective compared to placebo for both allergic asthma and allergic rhinitis, in addition to showing an immunomodulatory effect (15). As a result, several clinical trials have recently been initiated in the United States for treating asthma and food allergy in children. Another important value of inquiring into CAM use was described by George et al (16). They called attention to potential dangers of natural products and over the counter medication for pediatric asthma patients. They point out that in addition to the concern that CAM use might affect adherence to conventional therapy, that these products could have serious side effects. For example, Echinacea and Chamomile, both products in the ragweed family, could make asthma worse in the ragweed sensitive patient. In addition, natural ephedra, used in traditional Chinese medication (TCM), could potentiate the albuterol effect and licorice containing products could prolong the half life of cortisone potentially increasing steroid adverse effects. Thus, there are multiple reasons for the provider to inquire about CAM usage when evaluating the asthmatic child including both potential benefit and safety reasons.
Limitations
Several limitations need to be mentioned. We only asked about CAM in the asthmatic cohort since this would be relevant to treating a chronic disease which would not necessarily be applicable in the non asthma cohort. Although the cultural beliefs and preferences in the asthmatics were similar to those in the non asthmatics (data not shown), we cannot assume CAM usage would be the same in the two populations. Potential for selection bias is minimal as we had a strong survey response rate, 85.5%, and feel that this represents a vast majority of diversity within the parent population at the five schools we surveyed. We did not have a control group by which to compare SES and are not aware whether individuals of a different socio-economic background may share the same beliefs and practices. If the study were applied to a more general population of Vietnamese children in O.C., it would have given us a better overview of cultural and health beliefs and practices for this group as a whole in Orange County, California.
Finally, we didn’t determine whether Vietnamese parents of asthmatic children disclosed CAM to their physicians, or whether the use of CAM interfered with adherence to their controller asthma medication. However in the latter case there were no statistically significant differences in persistent asthma in those using or not using CAM (data not shown), suggesting no significant differences in adherence with CAM in this population. These issues should be addressed in future studies, but this report could encourage the beginning of the dialogue which should help adherence.
Conclusions
We found that CAM therapy is common in Vietnamese asthmatic children and have identified use of specific CAM therapies in this population which should be helpful to the clinician. In Vietnamese children, factors which appeared to predict CAM usage included age, English proficiency, ETS exposure, fear of long term medication with the potential of long term effects, and perception of asthma as a product of genetics and the environment. Our report should hopefully provide a strong rationale for encouraging providers to consider CAM as complementary to conventional therapy and to ask about CAM as part of the routine asthma evaluation for a more holistic approach to management.
Acknowledgments
Funding Source:
ICTS Incubator Grant: The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR000153. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Also, South Coast Air Quality Management District (SCAQMD). The content is solely the responsibility of the authors and does not necessarily represent the official views of SCAQMD.
Abbreviations
- ETS
environmental tobacco exposure
- SES
socioeconomic status
- CAM
complementary and alternative medicine
Footnotes
Financial Disclosure Statement: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest Statement: The authors have no conflicts of interest to disclose.
Clinical Trial Registration: NA
CONTRIBUTORS’ STATEMENT PAGE
Jill Berg PhD, RN, David Kilgore MD, Jackie Tran MPH contributed to the conception and design, acquisition of data, drafted and revised the manuscript, and approved the final manuscript as submitted.
Tricia Morphew MS contributed to the conception and design, analysis and interpretation of data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Stanley Galant MD conceptualized and designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
References
- 1.Orange County Health Needs Assessment Special report 2010: A look at Health in OC’s Vietnamese Community. Orange County California; 2010 Print. [Google Scholar]
- 2.U.S. Census Bureau. American FactFinder. 2013 Jul 15; http://factfinder2.census.gov.
- 3.Ahn AC, Ngo-Metzger Q, Legedza ATR, Massagli MP, Clarridge BR. Complementary and alternative medical therapy use among Chinese and Vietnamese Americans; prevalence associated factors, and effects of patient-clinical communication. Am J Public Health. 2006;96:647–653. doi: 10.2105/AJPH.2004.048496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsiao AF, Wong MD, Goldstein MS, Becerra LS, Cheng EM, Wenger NS. Complementary and alternative medicine use among Asian-American subgroups: Prevalence, predictors and lack of relationship to acculturation and access to conventional health care. The Journal of Alternative and Complementary Medicine. 2006;10:1003–1010. doi: 10.1089/acm.2006.12.1003. [DOI] [PubMed] [Google Scholar]
- 5.Liao O, Morphew T, Amaro S, Galant SP. The Breathmobile™: A novel comprehensive school-based mobile asthma care clinic for urban underprivileged children. J Sch Health. 2006;76:313–319. doi: 10.1111/j.1746-1561.2006.00119.x. [DOI] [PubMed] [Google Scholar]
- 6.Weiss KB, Gergen PJ, Crain EF. Inner city asthma: the epidemiology of an emerging US Public health concern. Chest. 1992;101:362s–367s. doi: 10.1378/chest.101.6.362s. [DOI] [PubMed] [Google Scholar]
- 7.Galant SP, Crawford LJR, Morphew T, Jones CA, Bassin SL. Predictive value of a cross-cultural asthma case-detection tool in an elementary school population. Pediatrics. 2004;114:e307–e316. doi: 10.1542/peds.2003-0575-F. [DOI] [PubMed] [Google Scholar]
- 8. [Accessed in October 18, 2013];California Health Interview Survey, 2011–2012. Available at www.chis.ucla.edu.
- 9.Rosser FJ, Forno E, Cooper PJ, Celedon TC. Asthma in Hispanics. Amer J Respir Crit Care Med. 2014;189:1316–1327. doi: 10.1164/rccm.201401-0186PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gellert GA, Maxwell RM, Higgins V, Mai KK, Lowery R. Barriers to health care access and utilization among Vietnamese Americans in Southern California. Health and Place. 1995;1:91–99. [Google Scholar]
- 11.McQuaid EL, Fede DA, Adams SK, Koinis-Mitchell D, Mitchell J, Kopel S, et al. Complementary and alternative medicine use and adherence to asthma medication among Latino and non-Latino White families. Academic Pediatrics. 2014:192–199. doi: 10.1016/j.acap.2013.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adams JK, Murdock KK, McQuaid EL. Complementary and alternative medicine use and asthma outcomes in children: an urban perspective. J Asthma. 2007;44:775–782. doi: 10.1080/02770900701645835. [DOI] [PubMed] [Google Scholar]
- 13.Chao MT, Wade C, Kronenberg F. Disclosure of complementary and alternative medicine to conventional medical provides: variation by race/ethnicity and type of CAM. J Natl Med Ass. 2008;100:1341–1349. doi: 10.1016/s0027-9684(15)31514-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Philip JC, Maselli J, Pachter LM, Cabana MD. Complementary and alternative medicine use and adherence with pediatric asthma treatment. Pediatrics. 2012;41:994–1004. doi: 10.1542/peds.2011-2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y-M. Complementary and alternative medicine in pediatrics allergic disorders. Curr Opin Allergy Clin Immunol. 2009;9:161–216. doi: 10.1097/ACI.0b013e328329226f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.George M, Topaz M. A systemic review of complementary and alternative medicine for asthma self management. Nurs Clin North Am. 2013;48:1–47. doi: 10.1016/j.cnur.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Slader CA, Reddel HK, Jenkins CR, Armour CL, Bosnic-Anticevich SZ. Complementary and Alternative medicine use in asthma: who is using what? Respirology. 2006;11:373–387. doi: 10.1111/j.1440-1843.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- 18.Ries AW, Picchi MA, Nguyen LHT, Moser RJ, Molgaard LA, Wassermant SI. Asthma in Vietnamese refugee population. Am J Respir Crit Care Med. 1997;155:1895–1901. doi: 10.1164/ajrccm.155.6.9196092. [DOI] [PubMed] [Google Scholar]
- 19.Ngo G, Kilgore DB, Tran JH, Galant SP. Using Community-Based Participatory Research to assess the asthma Needs of Vietnamese American Children. Progress in Community Health Partnership. 2014 doi: 10.1353/cpr.2014.0057. In press. [DOI] [PubMed] [Google Scholar]
- 20.Jenkins CNH, Thao LE, McPhee SJ, Stewart S, Ha NT. Health care access and preventative care among Vietnamese immigrants: Do traditional beliefs and practices pose barriers? Soc Sci Med. 1996;43:1049–1056. doi: 10.1016/0277-9536(95)00368-1. [DOI] [PubMed] [Google Scholar]
- 21.Ernst E. Prevalence of complementary/alternative medicine for children: a systematic review. Eur J Pediatr. 1999;158:7–13. doi: 10.1007/s004310051000. [DOI] [PubMed] [Google Scholar]
- 22.Pitetti R, Singh S, Hornyak D, Garcia SE, Herr S. Complementary and alternative medicine use in children. Pediatr Emergency Care. 2001;17:165–169. doi: 10.1097/00006565-200106000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Morgan W, Center H, Arms-Chavez C, Lobello SG. Complementary and alternative medicine use and asthma: relation to asthma severity and comorbid chronic disease. J Asthma. 2014;51:333–338. doi: 10.3109/02770903.2013.871559. [DOI] [PubMed] [Google Scholar]
- 24.Shen J, Oraka E. Complementary and alternative medicine (CAM) use among children with current asthma. Preventative Medicine. 2012;54:27–31. doi: 10.1016/j.ypmed.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 25.Expert Panel Report 3 (EPR3) Guidelines for the diagnosis and management of asthma. NIH Summary Report 2007. J Allergy Clin Immunol. 2007;120:s93–s138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 26.Chan PWK, DeBrun YE. Parental concerns towards the use of inhaled therapy in children with chronic asthma. Pediatrics International. 2000;42:547–551. doi: 10.1046/j.1442-200x.2000.01278.x. [DOI] [PubMed] [Google Scholar]
- 27.Kealoha MK. What’s new in alternative therapies for asthmatic children? Journal of Community Health Nursing. 2009;26:198–205. doi: 10.1080/07370010903259329. [DOI] [PubMed] [Google Scholar]