Abstract
We tested the hypothesis that social integration, measured as number of social roles, is associated with less age-related loss of lung function, an important marker of health and longevity. We also investigated possible psychological factors through which social integration might influence lung health. Data were analyzed from the Health and Retirement Study (ages 52-94, n = 4,224). Each additional social role reported at baseline was associated with less of a decline in lung function between baseline and the follow-up assessment four years later. The association withstood controls for demographics, weight, and height and was mediated by more positive and less negative affect and lower rates of cigarette smoking and more physical activity. Roles were mostly substitutable, with both high (spouse, parent, friends, relatives) and low (employee, religious service attendee, volunteer, members of other groups) intimacy roles independently contributing to less age related decline in lung function.
Keywords: Lung Function, Social Integration, Social Roles, Aging
There is considerable evidence that the social environment influences our health (e.g., reviews by Cohen, 2004; Kiecolt-Glaser & Newton, 2001; Uchino, 2004). Social integration (SI), the extent to which an individual participates in a diverse range of social relationships (Brissette, Cohen, & Seeman, 2000), has proven to be a particularly reliable predictor of both morbidity (e.g., Chang et al., 2017; Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997) and mortality (reviewed by Holt-Lunstad, Smith, & Layton, 2010), with greater network diversity associated with lower risks for disease and death.
Although measures of SI vary, it is often assessed as the number of social roles (e.g., spouse, friend, close relative, volunteer) one reports actively participating in (e.g., Cheng, Leung, & Chan, 2014; Cohen et al., 1997). A key implication of engagement in multiple roles is that most roles generate motivation to take care of oneself so that one can care for others (Umberson, 1987), as well as direct social pressures to engage in health promoting behaviors (e.g., physical activity, good diets, not smoking, and adhering to medical regimens; Berkman & Breslow, 1983; Cohen, 1988). Social roles also instill a sense of predictability in people’s lives by providing information about how they ought to act (Thoits, 1983). They additionally offer the opportunity to enhance feelings of self-worth, control, purpose, and positive affect by meeting role expectations (Cohen, 1988; Thoits, 1983; Wills, 1985). These cognitive and affective responses to enacting social roles are in turn thought to positively influence health by encouraging better health practices and aiding in the regulation of physiological systems (Cohen, 1988).
Lung function is an important indicator of health that decreases as we age (Schünemann, Dorn, Grant, Winkelstein, & Trevisan, 2000). The efficiency by which the lungs can inhale and exhale is not only a marker of respiratory health, it is also an indicator of general health, particularly in older adults. Poor lung function is an independent risk factor for mortality (Cook et al., 1991) as well as for a wide range of diseases, including diabetes, cardiovascular disease and dementia (Emery, Finkel, & Pedersen, 2012; Engström et al., 2003; Sin, Wu, & Man, 2005).
The hypothesized pathways linking SI to disease risk listed earlier emphasize the roles of external social pressures and diverse social participation in generating motivation to care for oneself. This seems particularly relevant to understanding a potential relation between SI and lung function, since refraining from smoking and engaging in physical activities are behaviors closely linked to maintaining lung function as we age (Dement, Welch, Ringen, Cranford, & Quinn, 2017; Pelkonen et al., 2003).
To date, two cross-sectional studies have examined the association between SI and lung function. Crittenden et al. (2014) used data collected from a sample of highly functioning 70-79 year old men and women in the United States. They found that greater numbers of social roles were associated with better peak expiratory flow rate (PEFR), a measure of lung function. Similarly, in a sample of Hong Kong Chinese 60 years old and over, Cheng et al. (2014) found that those in networks with more social roles had better PEFR. Of course, the cross-sectional design of these studies cloud causal inference, since the participants’ poorer lung function might have influenced their ability to build and maintain their social networks.
An enduring issue in the SI literature has been identifying the form of the relationship between SI and health. A common interpretation is that the association is attributable to a threshold effect, where those acting in a very few social domains (the “socially isolated”), would experience high levels of stress, and consequently have poorer health than those above the threshold (e.g., House, 2001). An alternative explanation is that there is a graded (possibly linear) relationship between SI and health, with each additional social role contributing to a decrease in risks for morbidity and mortality (e.g., Cohen, 2004; Seeman et al., 1993; Yang et al., 2016). As noted earlier, a graded relation could be due to increased social pressures to reduce behavioral risks such as smoking and inactivity, or to psychological changes associated with increasing SI such as increased positive affect, feelings of personal control, and purpose in life (Cohen, 1988). Interestingly, it is possible for both models to apply where there is a graded association but the socially isolated (those with very few roles) are worse off than one would expect if the relation was linear.
Finally, few SI studies address the relative impact of individual social roles. An analysis of participants aged 18-69 years from the Alameda County Study (Berkman & Breslow, 1983) found that both an aggregate measure based on number of social roles, as well as each of the five roles they assessed (marriage, friendship, relatives, church, and social group members) were associated with lower risk for mortality. These data are generally interpreted as suggesting that social roles are interchangeable in their contribution to total SI. Other work with older adults suggests that the contribution of individual roles varies with role intimacy. For example, in one mortality study (Seeman, Kaplan, Knudsen, Cohen, & Guralnik, 1987), the oldest participants at baseline (60+ years) benefited only from close friends and relatives. Similarly, a cross-sectional study of persons 70-79 years found that better lung function was associated with marriage, family, and friends but not with less intimate roles (Crittenden et al., 2014). Here we evaluate the association of an SI index in a larger, younger, mostly employed sample based on eight social roles with changes in lung function over four years. We also examine the independent contributions of each of the individual social roles, as well as two 4-item SI subscales representing high-intimate and low-intimate roles in the prediction of changes in lung function.
We present evidence from a prospective analysis of data from the Health and Retirement Study (HRS). We test whether there is a relationship between SI at study baseline and the rate of decline in lung function with aging. This is a 4-year follow-up controlling for lung function at baseline as well as age, sex, education, race/ethnicity, weight, and height. Where an association between SI and lung function is found, we further examine whether it is accounted for by those with few social roles (socially isolated) having a steep decline in lung function, or whether it is a more graded relationship with each additional social role associated with a lesser decline. We also test whether roles need to be intimate in order to provide health benefits. Finally, we examine whether the association between SI at baseline and changes in lung function over time are mediated by cognitive (greater purpose and controllability), affective (more positive and less negative affect) and behavioral (not smoking and physical activity) factors.
Methods
Study Designs and Participants
HRS is a longitudinal cohort study of the population of the United States over the age of 50. It is sponsored by the National Institute of Aging and is conducted via the Institute for Social Research at the University of Michigan. Data collection began in 1992, targeting community-dwelling adults who were between 51 and 61 years old. Blacks, Hispanics, and residents of Florida were oversampled in an attempt to overcome unequal selection probabilities in other US geographical areas. Follow-up interviews were conducted every 2 years thereafter with additional participants added at each follow-up. HRS was approved by the Behavioral Sciences Committee institutional review board at the University of Michigan. See Heeringa and Connor (1995) and Juster and Suzman (1995) for further details on HRS sampling and study design.
In the 2006 wave, 50% of the sample were randomly chosen to participate in a face-to-face interview that included the assessment of lung function. After the face-to-face interview, they were also given a “leave behind” questionnaire which was a self-administered series of questions assessing various psychological domains.
The current analysis is limited to HRS participants who agreed to the 2006 face-to-face interview, filled out the 2006 questionnaire, and had lung function data at both 2006 and 2010. We excluded participants who reported having any lung disease, shortness of breath, coughing, phlegm, or congestion at baseline. This left a sample size of 4,224. Demographics for the sample are reported in Table 1. When compared to all participants who took part in the 2006 face-to-face interview, the sample we selected for lung health was younger, more educated, more likely to be employed and less likely to be married. The samples were similar in race/ethnicity.
Table 1.
Descriptive information for the full HRS sample (N = 4224)
| Variable | Available N (%) | N (%) | Mean (SD) |
|---|---|---|---|
| Age (years) | 4224 (100) | 67.37 (9.15) | |
| Current Smokers at Time 1 | 4224 (100) | 442 (10.5) | |
| Education (years) | 4224 (100) | 13.15 (4.33) | |
| Ethnicity | 4224 (100) | ||
| White | 3370 (79.8) | ||
| Black | 480 (11.4) | ||
| Hispanic | 69 (1.6) | ||
| Other | 305 (7.2) | ||
| Gender | 4224 (100) | ||
| Males | 1772 (42.0) | ||
| Females | 2452 (58.0) | ||
| Height (inches) | 4176 (98.9) | 66.45 (29.04) | |
| PEFR at Time 1 (L/min) | 4224 (100) | 384.23 (130.81) | |
| PEFR at Time 2 (L/min) | 4224 (100) | 371.49 (135.47) | |
| Physical Activity (0 – 4) | 3364 (79.6) | 2.32 (1.42) | |
| Social Integration at Time 1 (1 – 8) | 4224 (100) | 5.42 (1.33) | |
| Social Roles Endorsed at Time 1 | 4224 (100) | ||
| Club/Organization | 2094 (49.6) | ||
| Employee | 1601 (37.9) | ||
| Family | 4043 (95.7) | ||
| Friends | 3984 (94.3) | ||
| Parent | 3958 (93.7) | ||
| Religious Service | 2504 (59.3) | ||
| Spouse | 2930 (69.4) | ||
| Volunteer | 1783 (42.2) | ||
| Weight (pounds) | 4043 (95.7) | 180.13 (49.39) |
Note: HRS = Health and Retirement Study; PEFR = peak expiratory flow rate; Time 1 = 2006; Time 2 = 2010
Measures
Lung Function
Lung function was measured via peak expiratory flow rate (PEFR). PEFR is the maximum speed of respiration produced by an individual when they are exerting maximal effort, after they have maximally inhaled. All tests were performed by trained technicians. The higher the PEFR, the less airway constriction and the better the lung function. PEFR is measured in liters per minute (L/min). PEFR consisted of 3 measurements taken 30 seconds apart using a Mini-Wright peak flow meter (Clement Clarke International, LTD, Harlow, United Kingdom). The best PEFR out of the three attempts was used.
Social Integration
SI scores were constructed from a series of questions about social relationships included in HRS. The scores represent the number of social roles reported by an individual. There were eight possible roles including being a spouse, parent, other family member, friend, employee, religious service attendee, volunteer, and member of other groups clubs and organization (cf. Cohen et al., 1997). To be counted as a role, the participants must have had at least a minimal amount of interaction (for most roles at least once per month) in that role. The exceptions are married couples, who we assumed met this criterion and volunteers, since the available data only provided information about participation during the last year. Table 2 presents the description of the role questions and of the criterion used for defining participation in each role. Because the questions used to assess individual roles were not originally meant to be used in a single scale, the response alternatives for frequency of interaction vary, and in turn the criterion to define participation across roles varies slightly.
Table 2.
Information regarding how social roles were coded
| Social Role | Code | Question | Responses a |
|---|---|---|---|
| Spouse | 0 = not married 1 = married |
A series of questions were used to identify each participant’s marital status. | Married Annulled Separated Divorced Widowed Never Married Other |
| Parent | 0 = did not interact with children
more than every few months or no children 1 = interacted with children more than every few months |
On average, how often do you do each of the following [e.g., meeting, speaking on the phone, writing or emailing] with any of your children, not counting any who live with you? | Three or more times per week Once or twice a week Once or twice a month Every few months Once or twice a year Less than once a year or never |
| Family | 0 = did not interact with other
family members more than every few months or no family members 1 = interacted with other family members more than every few months |
On average, how often do you do each of the following [e.g., meeting, speaking on the phone, writing or emailing] with any of your family members, not counting any who live with you? | Three or more times per week Once or twice a week Once or twice a month Every few months Once or twice a year Less than once a year or never |
| Friends | 0 = did not interact with friends
more than every few months or no friends 1 = interacted with friends more than every few months |
On average, how often do you do each of the following [e.g., meeting, speaking on the phone, writing or emailing] with any of your friends, not counting any who live with you? | Three or more times per week Once or twice a week Once or twice a month Every few months Once or twice a year Less than once a year or never |
| Employee | 0 = not currently working 1 = currently working |
Are you working now, temporarily laid off, unemployed and looking for work, disabled and unable to work, retired, a homemaker, or what? | Working now Unemployed, looking for work Temporary leave Disabled Retired Homemaker Other |
| Religious Service Attendee | 0 = did not attend religious
services at least two or three times a month 1 = attended religious services at least two or three times a month |
About how often have you attended religious services during the past year? | More than once a week Once a week Two or three times a month One or more times a year Not at all |
| Volunteer | 0 = did not engage in volunteer
work in past year 1 = engaged in volunteer work in past year |
Have you spent any time in the past 12 months doing volunteer work for religious, educational, health-related or other charitable organizations? | Yes No |
| Club | 0 = did not attend event in past
month 1 = attended event in past month |
How often do you (1) go to a sport, social, or other club, or (2) attend meetings of non-religious organizations, such as political, community, or other interest groups? | Daily Several times a week Once a week Several times a month At least once a month Not in the last month Never/not relevant |
Underlined Responses Indicate Answers Coded as “1”
Standard Control Variables
Information was collected on six variables that might account for both more roles and better lung function. These were assessed at baseline (2006) and included self-reports of age (years), sex (male, female), education (years) and racial/ethnic status (White, Black, Hispanic, other). We used objective measures of height (inches) and weight (pounds) as indicated for use in models testing PEFR (Mishra et al., 2013).
Potential Mediating Variables
Mediational analyses tested for the potential roles of cognitive (purpose in life and perceived control), affective (positive and negative affect), and behavioral (cigarette smoking status and level of physical activity) factors. Purpose in life was assessed using a seven-item questionnaire adapted from the Purpose Scale of the Ryff Psychological Well-Being scales (Ryff & Keyes, 1995). Positive and negative affect were assessed using the 12-item subscale from the Midlife Developmental Inventory (Mroczek & Kolarz, 1998) and perceived control was assessed using the 5-item Sense of Control Scale from the Midlife in the United States study (Lachman & Weaver, 1998). Current cigarette smoking status (yes/no) was assessed using self-report. Physical activity was assessed using a self-report of frequency of vigorous (e.g. running, swimming, working out) and moderate (e. g. gardening, walking) activity. Answers were summarized using a calculated variable previously used in the English Longitudinal Study of Aging (McMunn, Hyde, Janevic, & Kumari, 2003). This categorized physical activity into five categories ranging from 0 (sedentary) to 4 (active).
Data Analytic Approach
Analyses were conducted using SPSS (IBM Corporation, 2016) except where otherwise noted and were based on all available data. We first tested for mean changes in PEFR from Time 1 (T1) to Time 2 (T2). For this, we present the individual means (M) and standard deviations (SD) for the two time points as well as the mean difference (MD), paired sample t-test, two-tailed p-value, 95% confidence interval (CI95), and effect size (d).
Then, to examine whether SI assessed at T1 (in 2006) predicted lung function at T2 (4 years later, in 2010), we evaluated a series of three multiple linear regressions. For Model 1, raw PEFR values at T2 were regressed on the total number of social roles reported at baseline. For Model 2, Model 1 was adjusted for T1 PEFR. Finally, for Model 3, Model 2 was further adjusted for the six standard control variables. Given average declines in lung function between T1 and T2, these regression analyses reflect residual differences in rate of lung function decline. For these analyses, we report standardized regression coefficients (β), unstandardized regression coefficients (b), two-tailed p-values, and 95% CIs for the unstandardized regression coefficients.
We replicated the analysis of the raw data using a transformation often used by pulmonologists. Here PEFR was transformed into the percent of the expected norm for individuals based on their sex, age, height, and ethnicity using equations previously developed for HRS (Roberts & Mapel, 2012). For details, see Supplemental Table 1.
We also evaluated whether cognitive, affective, and behavioral factors mediated the association between T1 total SI and T2 lung function. All models were adjusted for T1 PEFR, and the six standard control variables. For cognitive factors, we examined T1 purpose in life and T1 perceived control. For affective factors, we examined T1 positive affect and T1 negative affect (reverse scored such that higher values indicate less negative affect). We also report an analysis from a composite of the T1 positive and negative affect variables due to the relatively large correlation between the two variables (r = -0.603, p < .001). To create this composite, we computed z-scores for both positive and reverse-scored negative affect and averaged them. For behavioral factors, we separately considered T1 physical activity (continuous) and smoking status (binary; details on smoking status analyses are presented below). We report regression coefficients, two-tailed p-values, and 95% CIs for the analyses (1) predicting the given mediator from total social roles at T1 (ba); (2) predicting lung function at T2 from the given mediator, controlling for total social roles at T1 (bb); and (3) predicting the direct effect of total social roles at T1 on lung function at Time 2 (bc′). We then used the PROCESS macro for SPSS (Hayes, 2013) to obtain estimates of the indirect effects for purpose in life, perceived control, positive affect, negative affect, composite affect, and physical activity, along with 95% CIs. These CIs were constructed using the percentile bootstrap based on 50,000 resamples. We considered mediation models examining each potential mediator individually as well simultaneously. In a model considering the continuous mediators simultaneously (purpose in life, perceived control, the composite affect variable, and physical activity), we report the proportion of the total effect accounted for by each of the four tested indirect effects. We also considered mediation models evaluating the indirect effect of changes in the various mediators from T1 to T2 (for details, see the online supplemental material). We use the terms “indirect effect,” “direct effect,” and “total effect” to be consistent with common terminology used to describe mediational analyses. We are not suggesting that our analyses demonstrate causation.
We also evaluated the binary variable for smoking status at T1 as a potential mediator of the association between T1 total SI and T2 lung function, adjusting for T1 PEFR and the six standard control variables. Because smoking status was expressed as a binary variable, this model could not be estimated using the methods employed by the PROCESS macro. Instead, we used the package mediation for R (R Core Team, 2016; Tingley, Yamamoto, Hirose, Keele, & Imai, 2014) to compute the average causal mediation effect (ACME) of smoking, along with a percentile bootstrap 95% CI. This technique is based on the counterfactual framework for assessing mediation and requires discrete data, thus in order to perform this analysis and for ease of interpretability, the variable for SI at T1 was median split (SI ≤ 5 = 0, SI > 5 = 1). Smoking was coded as 0 = “current smoker,” and 1 = “not a current smoker.” The portion of this model predicting smoking status at T1 was evaluated via logistic regression using the maximum likelihood estimator and logit link function. The portion of this model predicting lung function at T2 was evaluated via linear regression. We use the term “ACME” to be consistent with the terminology used in this type of mediational analysis, not to suggest we demonstrate causation.
We next examined individual associations between each of the eight social roles measured at T1 and lung function at T2 in separate multiple linear regression models. We also evaluated a model with all eight social roles entered simultaneously. These models were all adjusted for T1 PEFR and the six standard control variables.
We additionally used multiple linear regression to predict lung function at T2 from the number of social domains endorsed at T1 divided into high (family, friends, parent, spouse) and low (club, employee, religious service attendee, volunteer) intimacy categories. We examined high and low intimacy social roles in separate models as well as simultaneously in a single model. These analyses were adjusted for T1 PEFR and the six standard covariates.
Finally, to evaluate the possibility that associations between intimate or non-intimate social roles and lung function might vary as a function of age, in separate models we evaluated the interaction between age and (1) total social roles, (2) intimate and non-intimate social roles in separate models, and (3) intimate and non-intimate social roles in the same model. These models were all adjusted for Time 1 PEFR and the six standard covariates.
Results
Total Number of Social Roles and Lung Function
For descriptive information about the sample and the study variables, see Table 1. The sample consisted of 4,224 participants from 3,203 households. Since there were fewer households than participants, this means that other household members were included in households with more than one participant. To make sure no household factors were driving the reported associations, we ran analyses using the full dataset as well as a dataset with one person per household chosen randomly from the larger sample (referred to as the “restricted” dataset).
As expected, PEFR decreased on average from T1 (M = 384.233, SD = 130.806) to T2 (M = 371.491, SD = 135.474), MD = 12.742, t(4223) = 9.549, p < .001, CI95 = [10.126, 15.358], d = 0.147. Full results for the models predicting PEFR are presented in Table 3. Findings indicated a positive linear association between T1 SI and T2 lung function in both the full HRS dataset and the restricted dataset. This association remained when adjusting for T1 PEFR in Model 2 as well as when further adjusting for the standard covariates in Model 3 (see Figure 1).
Table 3.
Regression results for predicting Time 2 PEFR from total number of Time 1 social roles
| HRS: Full Sample | HRS: Restricted to One Person Per Household | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | β | b | p-value | CI95 for b | N | β | b | p-value | CI95 for b | |
| Model 1 a | 4224 | 0.216 | 21.933 | < .001 | [18.939, 24.927] | 3203 | 0.198 | 19.21 | < .001 | [15.921, 22.500] |
| Model 2 b | 4224 | 0.066 | 6.66 | < .001 | [4.748, 8.573] | 3203 | 0.070 | 6.733 | < .001 | [4.587, 8.880] |
| Model 3 c | 4028 d | 0.050 | 5.144 | < .001 | [3.187, 7.101] | 3047 d | 0.050 | 4.853 | < .001 | [2.670, 7.036] |
Note: HRS = Health and Retirement Study; PEFR = peak expiratory flow rate
Model 1 not adjusted for any covariates
Model 2 adjusted for PEFR at Time 1
Model 3 adjusted for PEFR at Time 1, age, gender, ethnicity, education, height, and weight
Sample sizes for Model 3 are reduced due to missing values for height and weight
Figure 1.
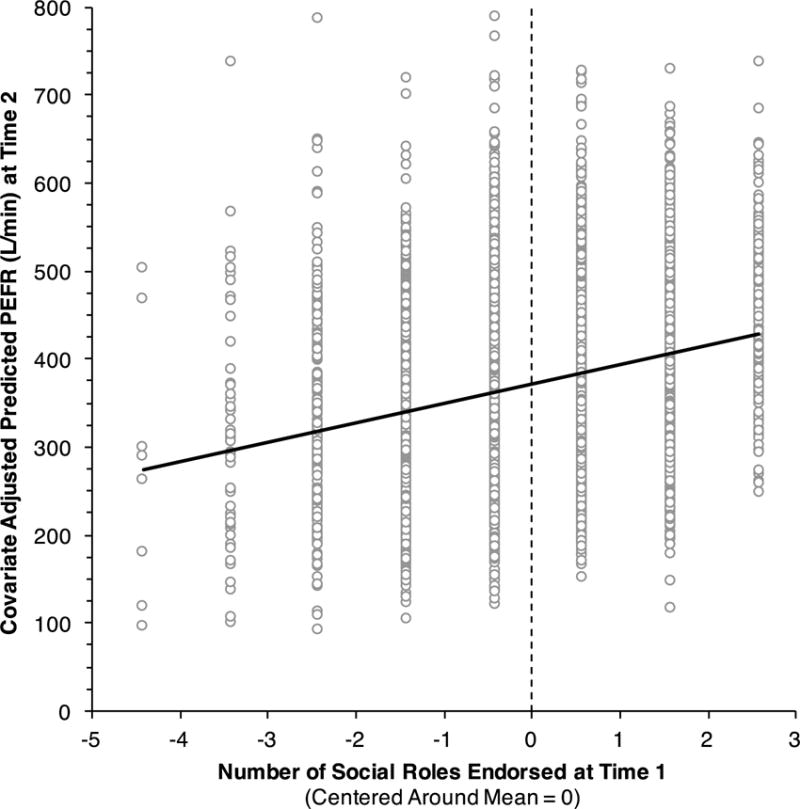
Regression results predicting Time 2 PEFR values (L/min) from total social roles at Time 1, adjusting for individual differences in Time 1 PEFR, age, gender, ethnicity, education, height, and weight (N = 4028). The total number of social roles variable was centered around a mean of 0. The total number of social roles at Time 1 was positively and linearly associated with PEFR at Time 2, β = 0.050, b = 5.144, p < .001, CI95 = [3.187, 7.101].
Analyzing the data using each individuals’ percent of their expected PEFR value based on height, age, sex, and race/ethnicity yielded the same results as those reported above that were based on the raw PEFR values (statistics presented in Supplemental Table 1). Given the consistency in findings regardless of whether raw or percent of expected PEFR values were used, or whether the full or restricted HRS dataset was used, for all remaining analyses we only present models predicting the raw PEFR values based on the full HRS dataset.
Mediators of the Association between Total Number of Social Roles and Lung Function
Cognitive
T1 SI was associated with T1 purpose in life, ba = 0.138, p < .001, CI95 = [0.116, 0.159]. T1 purpose in life was associated with T2 lung function, bb = 5.486, p < .001, CI95 = [2.605, 8.367]. The CI95 for the indirect effect (ba × bb = 0.754) did not contain 0, providing support for mediation, CI95 = [0.380, 1.1377]. There was evidence for a direct effect of T1 SI on T2 lung function, bc′ = 4.502, p < .001, CI95 = [2.498, 6.506].
T1 SI was associated with T1 perceived control, ba = 0.108, p < .001, CI95 = [0.081, 0.134]. T1 perceived control was weakly associated with T2 lung function, bb = 2.216, p = .057, CI95 = [−0.070, 4.501]. The CI95 for the indirect effect (ba × bb = 0.239) contained 0, failing to provide support for mediation, CI95 = [−0.021, 0.510]. There was evidence for a direct effect of T1 SI on T2 lung function, bc′ = 4.873, p < .001, CI95 = [2.894, 6.851].
Affect
T1 SI was associated with T1 positive affect, ba = 0.083, p < .001, CI95 = [0.067, 0.099]. T1 positive affect was associated with T2 lung function, bb = 7.072, p < .001, CI95 = [3.256, 10.889]. The CI95 for the indirect effect (ba × bb− = 0.588) did not contain 0, providing support for mediation, CI95 = [0.256, 0.958]. There was evidence for a direct effect of T1 SI on T2 lung function, bc′ = 4.668, p < .001, CI95 = [2.681, 6.654].
T1 SI was also associated with reverse scored T1 negative affect, ba = 0.079, p < .001, CI95 = [0.064, 0.093]. T1 negative affect was associated with T2 lung function, bb = 7.590, p < .001, CI95 = [3.412, 11.768]. The CI95 for the indirect effect (ba × bb− = 0.598) did not contain 0, providing support for mediation, CI95 = [0.258, 0.950]. There was evidence for a direct effect of T1 SI on T2 lung function, bc′ = 4.617, p < .001, CI95 = [2.625, 6.609].
Finally, T1 SI was associated with the T1 composite affect variable, ba = 0.126, p < .001, CI95 = [0.104, 0.147]. The T1 composite affect variable was associated with T2 lung function, bb = 5.784, p < .001, CI95 = [2.957, 8.611]. The CI95 for the indirect effect (ba × bb− = 0.727) did not contain 0, providing support for mediation, CI95 = [0.354, 1.120]. There was evidence for a direct effect of Time 1 SI on Time 2 lung function, bc′ = 4.520, p < .001, CI95 = [2.529, 6.512].
Behavioral
T1 SI was associated with T1 physical activity, ba = 0.171, p < .001, CI95 = [0.134, 0.208]. T1 physical activity was associated with T2 lung function, bb = 3.285, p = .002, CI95 = [1.187, 5.383]. The CI95 for the indirect effect (ba × bb− = 0.561) did not contain 0, providing support for mediation, CI95 = [0.169, 0.973]. There was also evidence for a direct effect of T1 SI on T2 lung function, bc′ = 5.252, p < .001, CI95 = [3.005, 7.498].
We also tested whether the binary variable for current smoking status at T1 mediated the association between T1 SI and T2 lung function. In this analysis, we found that higher SI at T1 was associated with a lower likelihood of smoking at T1, b = 0.684, p < .001, CI95 = [0.456, 0.912], which, in turn, was associated with better lung function at T2, b = 29.464, p < .001, CI95 = [21.147, 37.782]. The CI95 for the indirect effect (ACME = 1.412) did not contain 0, providing support for mediation, CI95 = [0.882, 2.641].
Combined Cognitive, Affective, and Behavioral Factors
Due to differences in the analytic framework of methods of evaluating mediation by continuous versus binary variables, the binary variable smoking status could not be included in this model as a parallel mediator, however we included it as a covariate. The 95% CIs for the indirect effects of purpose in life (ba × bb− = 0.243) and perceived control (ba × bb− = -0.144) both contained 0, suggesting that these variable were not mediators when also considering affect, physical activity, and smoking status, CI95 for purpose in life = [−0.207, 0.703], CI95 for perceived control = [−0.495, 0.182].
Conversely, the CI95 for the indirect effect of the composite affect variable (ba × bb− = 0.631) did not contain 0, providing support for mediation, CI95 = [0.078, 1.224]. Likewise, the CI95 for the indirect effect of physical activity (ba × bb− = 0.420) also did not contain 0, providing support for mediation, CI95 = [0.057, 0.804]. In this analysis, the composite affect variable, physical activity, purpose in life, and perceived control accounted for 12.9%, 8.6%, 5.0%, and 2.9% respectively of the total effect of T1 SI on T2 lung function.
We also re-ran the analysis considering the binary variable for currents smoking status at T1 as a mediator of the association between T1 SI and T2 lung function controlling for purpose in life, perceived control, composite affect, and physical activity. The CI95 for the indirect effect (ACME = 1.480) did not contain 0, providing support for mediation, CI95 = [0.578, 2.514].
Individual Social Roles and Lung Function
Full numerical results for these models are available in Table 4. In separate models, belonging to a club, being an employee, interacting with friends, having a spouse, and being a volunteer at T1 were all individually associated with better lung function at T2. Moreover, when all eight of the T1 SI variables were entered simultaneously into a single model, again, belonging to a club, being an employee, interacting with friends, having a spouse, and being a volunteer were each independently associated with better lung function at T2.
Table 4.
Regression results for predicting Time 2 PEFR from total number of Time 1 social roles in full HRS sample (N = 4028)
| Social Role Type | Variables Evaluated Individually in Separate Models a | Variables Evaluated Simultaneously in Single Model a | ||||||
|---|---|---|---|---|---|---|---|---|
| β | b | p-value | CI95 for b | β | b | p-value | CI95 for b | |
| Club | 0.034 | 9.163 | < .001 | [4.137, 14.189] | 0.023 | 6.210 | .030 | [0.599, 11.822] |
| Employee | 0.023 | 6.490 | .033 | [0.516, 12.464] | 0.030 | 8.304 | .010 | [1.964, 14.644] |
| Family | 0.004 | 2.377 | .706 | [−9.969, 14.723] | 0.003 | 1.994 | .766 | [−11.116, 15.104] |
| Friends | 0.025 | 15.06 | .006 | [4.252, 25.868] | 0.022 | 12.736 | .031 | [1.148, 24.325] |
| Parent | -0.008 | -4.576 | .380 | [−14.786, 5.634] | -0.017 | -9.661 | .106 | [−21.363, 2.041] |
| Religious Service Attendee | 0.005 | 1.274 | .624 | [−3.826, 6.374] | 0.010 | 2.689 | .357 | [−3.037, 8.415] |
| Spouse | 0.027 | 7.875 | .006 | [2.258, 13.491] | 0.030 | 8.848 | .005 | [2.738, 14.958] |
| Volunteer | 0.037 | 10.166 | < .001 | [5.084, 15.248] | 0.035 | 9.578 | .001 | [3.898, 15.259] |
| Addition of SI variables: ΔR2 = 0.004, p < .001 | ||||||||
Note: HRS = Health and Retirement Study; PEFR = peak expiratory flow rate
All models adjusted for Time 1 PEFR, age, gender, ethnicity, education, height, and weight
Low versus High Intimacy Social Roles and Lung Function
Full numerical results for these models are available in Table 5. In separate models, both the high and low intimate social role subscales at T1 were positively associated with lung function at T2. Likewise, when entered simultaneously into a single model, more high and low intimate social roles were both independently associated with better lung function at T2.
Table 5.
Regression results for predicting Time 2 PEFR from intimate and non-intimate Time 1 social roles in full HRS sample (N = 4028)
| Variables Evaluated Individually in Separate Models a | Variables Evaluated Simultaneously in Single Model | |||||||
|---|---|---|---|---|---|---|---|---|
| β | b | p-value | CI95 for b | β | b | p-value | CI95 for b | |
| Intimate Social Roles b | 0.025 | 5.304 | < .001 | [1.412, 9.196] | 0.020 | 4.225 | .034 | [0.313, 8.138] |
| Non-Intimate Social Roles c | 0.046 | 5.868 | < .001 | [3.433, 8.302] | 0.044 | 5.545 | < .001 | [3.093, 7.996] |
| Addition of SI variables: ΔR2 = 0.002, p < .001 | ||||||||
Note: HRS = Health and Retirement Study; PEFR = peak expiratory flow rate
All models adjusted for Time 1 PEFR, age, gender, ethnicity, education, height, and weight
Intimate social roles included family, friends, parent, and spouse
Non-intimate social roles included club, employee, religious service attendee, and volunteer
Age and the Association between Social Roles and Lung Function
In separate models, there were no interactions between age and total social roles, b = -0.075, p = .471, CI95 = [−0.280, 0.130], intimate roles, b = -0.238, p = .242, CI95 = [−0.638, 0.161], or non-intimate roles, b = -0.071, p = .594, CI95 = [−0.334, 0.191], at T1 in predicting lung function at Time 2. Likewise, when considering both intimate and non-intimate social roles simultaneously in a single model, there was no evidence for an interaction between age and the number of intimate, b = -0.143, p = .490, CI95 = [−0.549, 0.263], or non-intimate, b = -0.041, p = .764, CI95 = [−0.307, 0.226], roles endorsed at T1 in predicting lung function at T2.
Discussion
This study is the first to find a prospective relationship between SI and lung function, an important risk factor for morbidity and mortality. Specifically, as the number of social roles one engages in at baseline increases, age-related decline in lung function decreases. The prospective HRS analysis found no support for a threshold effect, where the association is attributable primarily to a drop in function among those with very few roles (the socially isolated). Rather, the relationship was linear with each additional social role associated with a lesser decline at 4-year follow-up. This association withstood controls for age, sex, education, ethnicity, height, and weight. Recent mortality data suggest that graded effects are limited to white participants (Barger & Uchino, 2017). Because the majority of HRS participants in the current sample were White, we lacked sufficient numbers of other ethnic groups to test this possibility here.
We also found evidence that it is the number of roles one occupies that counts, not having specific roles. When examined individually, five of the eight roles independently predicted lung function. The three roles that did not predict were family, parent, and church attendee. That family and parent did not predict is likely attributable to the percentage of the sample who held those roles, 96% for family and 94% for parent, resulting in reduced variability. Less clear is why church did not predict. Church attendance has been found to predict less morbidity in other studies (reviewed by Powell, Shahabi, & Thoresen, 2003), but this role may be more important for subsamples of the population (e.g., Black women; Dupre, Franzese, & Parrado, 2006).
Unlike some previous studies of older adults (Crittenden et al., 2014; Seeman et al., 1987), we did not find that intimate roles were more important predictors. In fact, both low and high intimacy roles predicted independently when entered into the equation at the same time. Overall, these analyses provide evidence for independent effects of the roles used here and in turn support for substitutability, even across intimacy levels and age. This suggests that functions like the diffusion of influence and information (including information about health care) usually associated with less intimate roles (weak ties; Granovetter, 1973) may operate as separate mechanisms linking SI to health, or that participation in less intimate roles contribute to the affective and behavioral factors that we found acted like mediators.
Having more social roles is thought to proportionally increase one’s sense of identity, predictability and stability, purpose, meaning, belonging, security, and self-worth (Cohen, 1988; Thoits, 1983; Wills, 1985). More roles are also thought to aid in emotional regulation, increasing positive affect and helping limit the intensity and duration of negative affective states (Cohen, 1988). These positive cognitions and emotions are presumed to be beneficial because they reduce psychological despair (Thoits, 1983), or result in greater motivation to care for oneself (e.g., Cohen, 1988). Here we found that these cognitive (purpose in life, perceived control), affective (positive and negative affect), and behavioral (physical activity and smoking) responses may mediate the association between SI and lung function. All three categories contributed to the association. However, when we entered purpose in life, perceived control, composite affect, and physical activity simultaneously in the same analysis, only affect and physical activity acted like mediators, accounting for 21.5% of the total effect. The remaining total effect may be due to inadequate measurement of the factors we assessed, and/or other factors not identified here, including direct physiological mechanisms (Uchino, 2006). The evidence for mediation we report is generally consistent with evidence from cross-sectional studies reporting positive affect (Crittenden et al., 2014) and physical activity (Cheng et al., 2014) as mediators of the association between SI and lung function. Like these studies, the mediators were assessed at the same time as SI and thus do not demonstrate temporal ordering.
The graded association of SI and lung function suggests implications for planning interventions. Specifically, the data suggest that not only would socially isolated individuals see a health benefit from adding social roles, but also those who are already engaged in several roles can benefit from adding more social roles. Moreover, the evidence for substitutability suggests that both high intimate and low intimate roles should work.
The study we report has a number of strengths including a large representative sample, and longitudinal data. The prospective analyses eliminate the possibility of reverse causation (poor lung function influencing number of roles) and the multiple covariates control for many third factor explanations. One weakness is the inability to establish temporal ordering of the mediators. Another possible weakness is the use of PEFR to assess lung function. This is a reasonable and predictive measure (e.g., it predicts mortality; Cook et al., 1991), but is not as sensitive as the state of the science use of spirometry.
That SI is linked to change in lung function with aging is important in itself. Although not tested here, our data are also consistent with the possibility that, at least for older adults, lung function may act as a pathway through which SI is associated with other illnesses and death.
Supplementary Material
Acknowledgments
Preparation of this manuscript was supported by grants from the National Center for Complementary and Integrative Health (AT006694). The data reported were from the Health and Retirement Study (HRS 2006 Core, Final V2.0; HRS 2010 Core, Final V1.0) sponsored by the National Institute on Aging (Grant NIA U01AG009740) and conducted by the University of Michigan.
Footnotes
The authors declare that they have no conflicts of interest with respect to their authorship or the publication of this article.
Contributor Information
Crista N. Crittenden, Department of Biobehavioral Health, The Pennsylvania State University
Michael L. M. Murphy, Department of Psychology, Carnegie Mellon University
Sheldon Cohen, Department of Psychology, Carnegie Mellon University.
References
- Barger SD, Uchino BN. Racial and ethnic variation in the association of social integration with mortality: Ten-year prospective population-based US Study. Scientific Reports. 2017;7:43874. doi: 10.1038/srep43874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman LF, Breslow L. Health and ways of living: The Alameda County Study. New York: Oxford University Press; 1983. [Google Scholar]
- Brissette I, Cohen S, Seeman T. Measuring social integration and social networks. In: Cohen S, Underwood LG, Gottlieb BH, editors. Social support measurement and intervention: A guide for health and social scientists. Oxford University Press; 2000. [Google Scholar]
- Chang SC, Glymour M, Cornelis M, Walter S, Rimm EB, Tchetgen ET, Kubzansky LD. Social integration and reduced risk of coronary heart disease in women: The role of lifestyle behaviors. Circulation Research. 2017;120:1927–1937. doi: 10.1161/CIRCRESAHA.116.309443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng ST, Leung EMF, Chan TWS. Physical and social activities mediate the associations between social network types and ventilatory function in Chinese older adults. Health Psychology. 2014;33:524–534. doi: 10.1037/hea0000026. [DOI] [PubMed] [Google Scholar]
- Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychology. 1988;7:269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59:676–684. doi: 10.1037/0003-066x.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Social ties and susceptibility to the common cold. Journal of the American Medical Association. 1997;277:1940–1944. doi: 10.1001/jama.1997.03540480040036. [DOI] [PubMed] [Google Scholar]
- Cook NR, Evans DA, Scherr PA, Speizer FE, Taylor JO, Hennekens CH. Peak expiratory flow rate and 5-year mortality in an elderly population. American Journal of Epidemiology. 1991;133:784–794. doi: 10.1093/oxfordjournals.aje.a115957. [DOI] [PubMed] [Google Scholar]
- Crittenden CN, Pressman SD, Cohen S, Janicki-Deverts D, Smith BW, Seeman TE. Social integration and pulmonary function in the elderly. Health Psychology. 2014;33:535–543. doi: 10.1037/hea0000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dement JM, Welch LS, Ringen K, Cranford K, Quinn P. Longitudinal decline in lung function among older construction workers. Occupational & Environmental Medicine. 2017 doi: 10.1136/oemed-2016-104205. [DOI] [PubMed] [Google Scholar]
- Dupre ME, Franzese AT, Parrado EA. Religious attendance and mortality: Implications for the black-white mortality crossover. Demography. 2006;43:141–164. doi: 10.1353/dem.2006.0004. [DOI] [PubMed] [Google Scholar]
- Emery CF, Finkel D, Pedersen NL. Pulmonary function as a cause of cognitive aging. Psychological Science. 2012;23:1024–1032. doi: 10.1177/0956797612439422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engström G, Hedblad B, Nilsson P, Wollmer P, Berglund G, Janzon L. Lung function, insulin resistance and incidence of cardiovascular disease: a longitudinal cohort study. Journal of Internal Medicine. 2003;253:574–581. doi: 10.1046/j.1365-2796.2003.01138.x. [DOI] [PubMed] [Google Scholar]
- Granovetter MS. The strength of weak ties. American Journal of Sociology. 1973;78:1360–1380. doi: 10.1086/225469. [DOI] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: The Guilford Press; 2013. [Google Scholar]
- Heeringa SG, Connor JH. Technical description of the Health and Retirement Study sample design. 1995 Retrieved from http://hrsonline.isr.umich.edu/
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLOS Medicine. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS. Social isolation kills, but how and why? Psychosomatic Medicine. 2001;63:273–274. doi: 10.1097/00006842-200103000-00011. [DOI] [PubMed] [Google Scholar]
- IBM Corporation. IBM SPSS Statistics, Version 24. Armonk, NY: IBM Corporation; 2016. [Google Scholar]
- Juster FT, Suzman R. An overview of the health and retirement study. Journal of Human Resources. 1995;30:S7–S56. doi: 10.2307/146277. [DOI] [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037//0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology. 1998;74:763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- McMunn A, Hyde M, Janevic M, Kumari M. Health. In: Marmot M, Banks J, Blundell R, Lessof C, Nazroo J, editors. Health, wealth and lifestyles of the older population: The 2002 English Longitudinal Study of Ageing. London: IFS; 2003. pp. 207–230. [Google Scholar]
- Mishra J, Mishra S, Satpathy S, Manjareeka M, Nayak PK, Mohanty P. Variations in PEFR among males and females with respect to anthropometric parameters. IOSR Journal of Dental and Medical Sciences. 2013;5:47–50. doi: 10.9790/0853-0514750. [DOI] [Google Scholar]
- Mroczek DK, Kolarz CM. The effect of age on positive and negative affect: A developmental perspective on happiness. Journal of Personality and Social Psychology. 1998;75:1333–1349. doi: 10.1037/0022-3514.75.5.1333. [DOI] [PubMed] [Google Scholar]
- Pelkonen M, Notkola IL, Lakka T, Tukiainen HO, Kivinen P, Nissinen A. Delaying decline in pulmonary function with physical activity: A 25-year follow-up. American Journal of Respiratory and Critical Care Medicine. 2003;168:494–499. doi: 10.1164/rccm.200208-954OC. [DOI] [PubMed] [Google Scholar]
- Powell LH, Shahabi L, Thoresen CE. Religion and spirituality: Linkages to physical health. American Psychologist. 2003;58:36–52. doi: 10.1037/0003-066X.58.1.36. [DOI] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing (Version 3.3.1) Vienna, Austria: R Foundation for Statistical Computing; 2016. [Google Scholar]
- Roberts MH, Mapel DW. Limited lung function: Impact of reduced peak expiratory flow on health status, health-care utilization, and expected survival in older adults. American Journal of Epidemiology. 2012;176:127–134. doi: 10.1093/aje/kwr503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD, Keyes CLM. The structure of psychological well-being revisited. Journal of Personality and Social Psychology. 1995;69:719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Schünemann HJ, Dorn J, Grant BJB, Winkelstein W, Trevisan M. Pulmonary function is a long-term predictor of mortality in the general population: 29-year follow-up of the Buffalo Health Study. Chest. 2000;118:656–664. doi: 10.1378/chest.118.3.656. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Berkman LF, Kohout F, Lacroix A, Glynn R, Blazer D. Intercommunity variations in the association between social ties and mortality in the elderly: A comparative analysis of three communities. Annals of Epidemiology. 1993;3:325–335. doi: 10.1016/1047-2797(93)90058-C. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Kaplan GA, Knudsen L, Cohen R, Guralnik J. Social network ties and mortality among the elderly in the Alameda County Study. American Journal of Epidemiology. 1987;126:714–723. doi: 10.1093/oxfordjournals.aje.a114711. [DOI] [PubMed] [Google Scholar]
- Sin DD, Wu LL, Man SFP. The relationship between reduced lung function and cardiovascular mortality: A population-based study and a systematic review of the literature. Chest. 2005;127:1952–1959. doi: 10.1378/chest.127.6.1952. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Multiple identities and psychological well-being: A reformation and test of the social isolation hypothesis. American Sociological Review. 1983;48:174–187. [PubMed] [Google Scholar]
- Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. mediation: R Package for Causal Mediation Analysis. Journal of Statistical Software. 2014;59 doi: 10.18637/jss.v059.i05. [DOI] [Google Scholar]
- Uchino BN. Social support and physical health: Understanding the health consequences of relationships. New Haven: Yale University Press; 2004. [Google Scholar]
- Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Umberson D. Family status and health behaviors: Social control as a dimension of social integration. Journal of Health and Social Behavior. 1987;28:306–319. doi: 10.2307/2136848. [DOI] [PubMed] [Google Scholar]
- Wills TA. Supportive functions of interpersonal relationships. In: Cohen S, Syme SL, editors. Social support and health. New York, NY: Academic Press; 1985. pp. 61–82. [Google Scholar]
- Yang YC, Boen C, Gerken K, Li T, Schorpp K, Harris KM. Social relationships and physiological determinants of longevity across the human life span. Proceedings of the National Academy of Sciences of the United States of America. 2016;113:578–583. doi: 10.1073/pnas.1511085112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


