Abstract
PURPOSE
Preemptive pharmacogenetic testing aims to optimize medication use by having genetic information at the point of prescribing. Payers’ decisions influence implementation of this technology. We investigated U.S. payers’ knowledge, awareness, and perspectives on preemptive pharmacogenetic testing.
METHODS
A qualitative study was conducted using semi-structured interviews. Participants were screened for eligibility through an online survey. A blended inductive and deductive approach was used to analyze the transcripts. Two authors conducted an iterative reading process to code and categorize the data.
RESULTS
Medical or pharmacy directors from 14 payer organizations covering 122 million U.S. lives were interviewed. Three concept domains and ten dimensions were developed. Key findings include: clinical utility concerns and limited exposure to preemptive germline testing, continued preference for outcomes from randomized controlled trials, interest in guideline development, importance of demonstrating an impact on clinical decision making, concerns of downstream costs and benefit predictability, and the impact of public stakeholders such as the FDA and CMS.
CONCLUSION
Both barriers and potential facilitators exist to developing cohesive reimbursement policy for pharmacogenetics, and there are unique challenges for the preemptive testing model. Prospective outcome studies, more precisely defining target populations, and predictive economic models are important considerations for future research.
Keywords: Pharmacogenetics, Pharmacogenomics, Preemptive, Reimbursement, Insurance, Payers
INTRODUCTION
Pharmacogenetics remains at the forefront of precision medicine, and preemptive testing is emerging as a best practice.1–3 Preemptive pharmacogenetic testing translates germline genotypes into actionable phenotypes that are then integrated into the electronic health record (EHR) and made available to clinicians at the point-of-prescribing.4,5 Compared to reactive testing, where the patient’s genotype is obtained in anticipation of a high-risk drug prescription or in response to unexplained adverse effects, the preemptive approach aims to optimize drug therapy by screening patients for multiple pharmacogenetic variants prior to an indication for pharmacotherapy.6,7
Recent efforts to implement preemptive pharmacogenetics have overcome challenges and illustrate its feasibility. Implementation projects have targeted populations, developed infrastructure for use of results, and assessed the benefits of preemptive pharmacogenetics.5,8–11 Patients with likely actionable phenotypes have been quantified and the incidence of patient exposure to high-risk drugs that are affected by pharmacogenetic variations has been determined.7,12 The Clinical Pharmacogenetics Implementation Consortium (CPIC) provides clinical practice guidelines to enable the use of genetic information to guide medication prescribing. To date, 19 guidelines have been published to guide therapy for over 30 drugs (corresponding to 14 genes).13,14 Among 5,000 clinical subjects, approximately 96% of them had at least 1 CPIC level A actionable variant.15 In 2013, 738 million prescriptions for pharmacogenetically high-risk drugs were written in the U.S., and about 18% of all prescriptions dispensed corresponded to either CPIC level A or B.15,4,7 Despite the fact that preemptive pharmacogenetics is being adopted by more health systems and becoming more actionable to clinicians, reimbursement for this testing approach is absent, and payer perspectives on this approach are not well understood.
Reimbursement for germline pharmacogenetic testing has experienced some success under the reactive ordering approach, using single gene–drug pair tests.10 An analysis of beneficiaries showed that single-gene tests are often billed to Medicare: from 2012 to 2013, a total of 519,340 tests were billed for the genes CYP2D6, CYP2C19, and CYP2C9. Total expenditures for these 3 genes were $117,845,531 among 454,575 beneficiaries. This equates to approximately $260 per individual gene test.16 These 3 genes and 2 others that were listed, VKORC1 and UGT1A1, are frequently included in multi-gene panels used in practice. Some Medicare Administrative Contractors have narrowed the covered indications for several tests and now classify these gene-drug combinations as investigational, citing insufficient evidence to support clinical utility or lack of impact from adverse drug events (www.cms.gov/medicare-coverage-database).
Coverage policies and payers’ decision-making in pharmacogenetics has been mainly focused on somatic variants that guide the selection of cancer therapies and on a limited number of germline variants.17–20 Payers’ policy development for new health technologies is described as a data-driven hierarchical approach that has historically valued certain types of evidence more than others (e.g. randomized control trial [RCT] data ahead of retrospective study data).21 A formal health technology assessment (HTA) protocol is established in some organizations to use evidence and evaluate new products and technologies according to safety, efficacy, cost-effectiveness, ethics, legality, and politics.22,23 Limited research aimed at understanding the views of the U.S. payer has been performed in the diffusion of pharmacogenetics.17,19,23,24 The purpose of this study was to investigate U.S. payer’s knowledge, awareness, and perspectives on preemptive pharmacogenetic testing.
MATERIALS AND METHODS
Study design
Semi-structured, in-depth interviews were used to obtain a rich and detailed understanding of payers’ perspectives. Identifying individual preferences, decision-making, behaviors, values, and beliefs are areas in which qualitative data are particularly useful.25 The study was approved by the University of Mississippi institutional review board.
Study population and sampling strategy
U.S. payers from a variety of organization types were recruited to participate in the study. The payers were recruited through a panel made available by Medical Marketing Economics, LLC [MME], (www.m2econ.com), a healthcare consulting and research firm with both clinician and payer relationships. This established panel includes Pharmacy and Medical Directors with decision-making roles at their organization who serve on the Pharmacy and Therapeutics (P&T) committee, medical technology committee, or both.
Interview guide development
Interview guide development was informed by discussions with healthcare professionals with payer or pharmacogenetics expertise. Questions were framed by 3 concept domains: 1) the clinical utility and applicability of preemptive pharmacogenetics, 2) the economic utility and cost considerations of preemptive pharmacogenetics and, 3) other factors influencing policy development regarding preemptive pharmacogenetics (Table S1).25 A screening survey was administered to identify participants with a basic knowledge of pharmacogenetic testing before sending a formal interview invitation. The survey also focused on the payer’s professional role in their institution, plan size, covered lives, and plan type (e.g. commercial, Medicare, Medicaid). To structure each interview, background material on pharmacogenetics was provided prior to the interview, including a brief summary of CPIC processes and recommendations, examples of clinical decision support, and representative implementations of preemptive pharmacogenetics (Table S2).5,8,9
Data collection
Members of the MME panel were invited and provided a link to the screening survey (Qualtrics, Provo, UT). Those who responded “not at all familiar” to a question on general familiarity with pharmacogenetic testing were excluded from further participation. The initial survey noted responses would remain confidential and obtained consent from participants. Eligible participants who consented to participate were interviewed via telephone to facilitate the inclusion of a diverse group of payers unrestricted by geography.
Data analysis
The screening questionnaire results were analyzed using descriptive statistics. The interviews were coded and analyzed manually by two authors (NK and MR) using content analysis in the style of the constant comparative method. This analysis blended both inductive and deductive strategies. The inductive approach, a majority of the analysis, uses open and iterative coding of the transcripts that lead to the refinement of the essential dimensions within the concept domains. Deductive analysis begins with a strong theoretical foundation or retesting of existing data in a new context, and in many cases, uses predefined coding schemes based on this theory or a particular interest within a topic.26 The framing of questions into the concept domains mentioned previously reflects the deductive approach to the current analysis. Though theoretical development was not the goal of the project, these techniques reflect the approach of a grounded theory study and constant comparative method of analysis.27
RESULTS
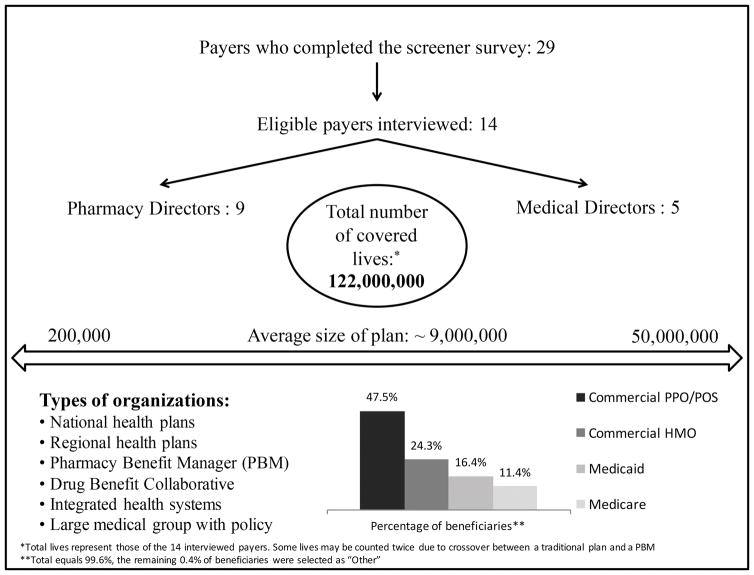
Of a 75-member payer panel, 35 responded to the screener survey and 29 met eligibility criteria. The six respondents ineligible for the interview failed to respond to a qualifying question in the screener survey. A total of 14 payers agreed to be interviewed, each from a unique organization, with plans that ranged greatly in size (Figure 1). A visual comparison of the data showed no outstanding difference between those respondents who agreed to participate in the interview and the 15 who did not. Figure 1 provides further detail on the characteristics of the interviewed payers. Interview analysis yielded a number of dimensions under each of the aforementioned concept domains. Table 1 summarizes all domains and dimensions.
Figure.
Payer Respondent Characteristics
Table 1.
Summary of dimensions from each domain of the analysis
| Domain | |||
|---|---|---|---|
| Clinical utility and applicability | Economic utility and cost considerations | Policy development influences | |
| Dimensions | The value message of preemptive pharmacogenetics | Recognition of potential downstream benefits…but concerns of sustainability | Preventive population health |
| CPIC guidelines and actionability | Stratifying beneficiaries | The role of CMS and the FDA | |
| The appropriate demonstration of evidence for payers | The number needed to test (NNT) | Impact of current implementation projects | |
| Testing compared to standard practice of medication use | |||
Clinical utility and applicability of domain dimensions
The value message of preemptive pharmacogenetics
Payers believe there is potential value in pharmacogenetic data, but they remained skeptical that pharmacogenetics improves clinical outcomes. As one payer said:
“[Pharmacogenetic data have] tremendous potential to help us much better refine who we give drugs that often have to be targeted for large populations .…But that being said, at the present time, they are relatively low on the value scale.” (Medical Director #2 - Regional PBM with medical policy)
To reap the future benefits of pharmacogenetic testing, payers find value in a test that allows clinicians to choose therapies for specific populations. One payer said, “Is it going to have an impact on how prescribers manage patients or what they prescribe?’” (Pharmacy Director #2 - Regional Health Plan) In fact, several payers made it clear that they desired a test that would provide them with an ability to build coverage criteria around the results:
“…it often [means] that we can use a treatment in a more precise way: avoid treating people who won’t respond, focus on treating people who will respond. When it clearly allows us to focus, it can be built into the criteria…for a certain drug. That’s fairly rare at this point…” (Pharmacy Director #5 - Regional Health Plan)
Guidelines and actionability of preemptive pharmacogenetics
Almost all payers were initially unfamiliar with CPIC but were unanimously positive about this work once they were introduced to it. This reaction was somewhat tempered by a concern about a “gray area” for using pharmacogenetic information:
“I think the biggest issue in thinking about this is that some of the tests that we have may not be definitive for rule-in, rule-out. There’s always going to be a gray area. In other words, you may have the probability that the patient will respond or will not respond however the test is set up.…” (Pharmacy Director #6 - Large National Plan)
Payers communicated that expanding the breadth of CPIC guidelines beyond prescription and dose changes could increase their usability. The National Comprehensive Cancer Network guidelines were cited as a potential model if such changes were pursued. However, payers stopped short of saying that they would reimburse based on these guidelines.
“I think the consortium should really —and again, I don’t know if that is the intent of what they are trying to do—but I think the consortium should come together and say who should be eligible. At least not just the level of the test itself, but what type of patient, what level of risk, age, and things like that.” (Pharmacy Director #7 - Large Regional Health Plan)
The appropriate demonstration of evidence for payers
For many payers, the randomized controlled trial (RCT) remains the “gold standard” in evidence for this area. As one payer stated, “I quite frankly do think you need the randomized controlled trials. Those clinical reports may be helpful. If you’re going to do this, it really depends on the disease process in terms of that. You have to establish an outcome.” (Medical Director #1 – Large National Plan) However, several others maintained flexibility and suggested different types of study designs that might be useful in their evaluation:
“You almost wonder if the best way to do this is in some kind of real-world type of population-based study where you test a large group of people and then look retrospectively…for maybe a drug problem or a failure to respond….” (Medical Director #4 - Drug benefit collaborative)
Preemptive pharmacogenetic testing compared to standard practice of medication use
Preemptive pharmacogenetics aims to change the paradigm of clinician prescribing towards one of testing then treating and away from the current standard practice of treating and monitoring. Payers responded to this subject with references to the large number of cheap, generic alternatives available. As one payer stated, “But frankly, if it’s a very low-cost drug, you know, you try one and then maybe try another. Because one of the concerns with some of the testing is that it’s going to lead you to maybe pick first line.” (Pharmacy Director #6 - Large National Plan) Again, the tests that payers were most familiar with, and generally covered, were the companion diagnostics for high-priced cancer drugs for which no generic or low-cost alternative exists. As such, it was difficult for them to imagine paying for comparatively expensive preemptive pharmacogenetic testing when several cheap generic drugs could be tried first.
Comparisons to the reactive model of pharmacogenetic testing were also made by some respondents. “If we have a patient already diagnosed with a condition and we’re going to do testing to understand which drug might be best, sure that’s intuitive. It depends on the place in which we’re saying that we’re testing.” (Pharmacy Director #6 – Large National Plan) There was similar sentiment from others, including beliefs that there is a linear relationship between the genes tested and costs, and concerns of insufficient clinical relevance for numerous genes on the panels.
See Table 2 for additional verbatim quotes from this domain.
Table 2.
Additional verbatim quotes from the dimensions of the clinical utility and applicability domain
| The value message of preemptive pharmacogenetics | Now what needs to be tied to that is products A and C work better with this patient than product B and D for patient two based on the genetic profile as far as outcomes improvement; survival, lower exacerbation, delay in correction, higher level of control. Pharmacy Director #1 - Large National Plan | I can see where this makes sense in terms of the results of the test can potentially change the prescription and change the drug. Quite frankly, what’s concerning here is I don’t think there’s a consensus…I think the overall clinical utilization of these tests is unclear. Medical Director #1 - Large National Plan | I think the promise of screening large populations for pharmacogenomic variability in response to drugs has not lived up yet. I say yet because I think it will, but it has not lived up to yet to fairly broad application. Pharmacy Director #3 - Mid-sized Integrated Network | The question really is what is the expectation that they’re ever going to use that information? I think our desire is that we make this as patient specific as possible and as drug specific as possible so that we’re not wasting dollars. Pharmacy Director #4 - Regional Pharmacy Benefit Manager |
| Guidelines and actionability of preemptive pharmacogenetics | They [NCCN] started creating interest as far as should you cover this, should you not cover that…they have different ratings for the drugs. That really hadn’t happened in a long period of time at all. I think that model could be used in something like this. Medical Director #5 - Medical Group with Insurance Policy | If you have a particular drug where a test said [drug dosing] needs to be reduced – I would speculate to say that this is compelling data. Those things can be built in as alerts. The electronic record, dysfunctional as it is, can be useful for that. Medical Director #5 - Medical Group with Insurance Policy | ||
| The appropriate demonstration of evidence for payers | Again, we realize there are some situations where randomized control trials are not practical, are not possible. We wouldn’t have a closed mind about other well done studies. The randomized control trials are usually preferred but won’t always be the appropriate affair. Medical Director #5 - Medical group with Insurance policy | Do something prospective. Go out and maybe partner with a couple of - whether it is an integrated delivery system, some HPOs, maybe some small regional plan that can get the membership and the physician and the plan all onboard piloted. Pharmacy Director #3 - Mid-sized integrated network | ||
| Preemptive testing compared to standard practice of medication use | The question is…is that test going to delay intervention? We are waiting for the results. How long does waiting two or three days or a week for test results really going to impact outcome? Pharmacy Director #2 - Regional Health Plan | Okay, maybe we need to do this test to see whether they are a rapid metabolizer or not. As far as to necessarily identify a specific gene, and that’s a gene over one drug. As opposed to a drug that is very cheap because it’s generic. And the fact that there are multiple competitors out there, that may be just as effective. Medical Director #1 - Large National Plan | How many different markers and what is the use of it? How many of them will potentially would be useful to a physician in making decisions as opposed to paying for one test? At one point they were fixed genes. Now, there are 20. Others are coming out with 150 genes with obviously matching prices. What is the clinical utility of this information? I think it very well may become a standard of care but not until it’s supported by additional research. Medical Director #3 – Large National Plan | |
Economic utility domain dimensions
Recognition of potential downstream benefits and the concerns of sustainability
All payers were apprehensive of the large initial costs and the unpredictability of benefits downstream for coverage of preemptive pharmacogenetics. One payer stated, “…let’s say it’s even a ridiculously low, low price of 100 bucks. If I got a million members that I got to test, I just spent a (hundred) million dollars and I don’t know what my return on that investment is going to be.” (Medical Director #4 - Drug benefit collaborative) However, many payers speculated on potential benefits:
“If you are going to identify a responder knowing full well that six weeks down the road they may switch to something else, but now they are not because you know they are going to respond…I could see some cost savings associated with that. (It’s) the same thing with the adverse event. Again, I see that more as a cost benefit, but downstream though.” (Pharmacy Director #2 - Regional Health Plan)
Payer’s sensitivity to price was explored through a hypothetical scenario comparing a $250 single-gene test to a $500 multi-gene. There was agreement that this price difference was not concerning for the individual patient, but large-scale testing was likely untenable. “Do we need to manage it? A one off test that costs $500, are we going to be concerned about it? No. If we start getting thousands of them, then yes.” (Pharmacy Director #5 – Regional Health Plan)
Stratifying beneficiaries for coverage
Given difficulties with widespread upfront adoption, payers were asked to speculate about whether they would consider the stratification of beneficiaries for coverage based on potential actionability. This suggestion was met with variable response, but several payers were willing to consider it. One payer stated:
“Maybe if you were 22 to 30, or maybe 40, you wouldn’t really have to do that testing for those patients because usually they’re relatively healthy.…Then you look at it, maybe you relegate it to 50 and above, I guess, if you wanted to do that type of testing. You might relegate it to specific disease states, too.… (Pharmacy Director #5 - Regional Health Plan)
Number needed to test (NNT)
NNT calculations were frequently mentioned by payers when discussing the economic utility of these tests. As one payer asked, “… how many do you have to test I guess, like how many (tests) to prevent that one adverse event or to prevent that one hospitalization?” (Pharmacy Director #7 - Large Regional Health Plan) Payers stated that this was something that they and physicians used frequently when evaluating utility of a new treatment or technology. As one payer described, “Maybe you can come up with something like that for this type of testing and specific diseases. A lot of docs really hang their hat on that stuff. It might also be indicative to whether a payer pays for it or not.” (Medical Director #5 - Medical group with insurance policy)
See Table 3 for additional verbatim quotes from this domain.
Table 3.
Additional verbatim quotes from the dimensions of the economic utility and cost considerations domain
| Recognition of potential downstream benefits and the concerns of sustainability | We’re obviously very interested in hospitalizations and preventing re-hospitalizations and expense of adverse events. If these tests do show robust predictive value, then we would be interested in using them. Again, this is probably going to be on a case-by-case basis. Medical Director #5 - Medical group with insurance policy | The cost savings would be not having to re-stent the patient that didn’t have the enzyme. I think that there’s a lot of application for it. I think that it’s just a little bit premature I guess because of the way the design is currently in the marketplace for pharmaceuticals. Pharmacy Director #7 - Regional Health Plan | Would we focus it on where we had potential risks either in preventable admissions or hospital readmissions and have offsets? Yes. I think when it trickles down through all that triage, to what’s good for society and good for the patient to get an earlier experience, I’m gonna suggest probably funding and resources run out before we get to that level of compassion and empathy. Pharmacy Director #8 - Large National Plan | You’re committing yourself to doing a fairly substantial expense on a large number of patients. The problem you’re going to run into there is, again, a big upfront cost for unknown value down the road. Medical Director #4 - Drug Benefit Collaborative |
| Stratifying beneficiaries for coverage | I’d even consider in high-risk populations, the possibility you have here of the preemptive testing. If there’s evidence that every childhood asthmatic should get preemptive testing or evidence that every patient post-myocardial infarction should get preemptive testing, I’m willing to consider that also. Pharmacy Director #9 - Integrated Health System Plan | I think that if you have a patient that’s 60 years old and they’re relatively healthy, you may have already done this; but you may decide that at that age 60, it’s time that he or she has this information in his file, so the $500 gets spent. I think that’s going to be really up to the physician on how they view the patient. But I don’t think we are going to go out and promote a multi-gene testing for everybody over 65 or everybody over 60 just because the consortium or the guidelines say that is the right patient for these. Pharmacy Director #5 - Regional Health Plan | ||
| Number needed to test | Maybe you can come up with something like that for this type of testing and specific diseases. If you could come up with NNT. A lot of docs really hang their hat on that stuff. It might also be indicative to whether a payer pays for it or not to. Medical Director #5 - Medical Group with Insurance Policy | I guess my question is if you test 100 people how many do you have to test I guess, like how many (tests) to prevent that one adverse event or to prevent that one hospitalization? Again the assumption is that we are being told that if you test everybody you are going to reap benefits from everybody you test. Pharmacy Director #7 - Large Regional Health Plan | ||
Policy development influence domain dimensions
Preventive population health
Discussions of population and preventive health resulted in payers suggesting that preemptive pharmacogenetics might be suitable for a recommendation from the U.S. Preventive Services Task Force (USPSTF) as one way to overcome concerns about downstream returns on testing. As one payer stated, “…If it ever became a part of an annualized preventative health guideline, published and adopted and/or became a quality metric…we would pay for it.” (Pharmacy Director #5 - Regional Health Plan) Another payer added that achieving the necessary evidence threshold of the USPSTF at the present time might be a challenge.
There was evident frustration from a few payers about the willingness of the pharmaceutical industry to support pharmacogenetic testing in a broader population. As one payer stated, “You would think that the pharmaceutical company would come out with it but they don’t because they want it to be used in everybody and not just specific patients.” (Pharmacy Director #2 - Regional Health Plan)
The role of the CMS and the FDA
The influence of the Centers for Medicare and Medicaid Services (CMS) was undeniable for wider adoption. One payer stated, “Outside of CMS or somebody…that’s probably where it’s going to have to start, is to have somebody start doing these things and publish data for the rest of us to see that it’s worth it or changes things.” (Medical Director #2 - Regional PBM with medical policy) The CMS “coverage with evidence development” (CED) program was used to probe payers’ interest in pursuing something similar. Some spoke highly of it and indicated interest in developing their own pilot-type studies. Other payers would find the results of such studies from CMS valuable and instinctively follow their lead:
“I think the learnings from that kind of a (CED) program translate probably more into the potential that, at some point down the road, the tests become part of the things like system pathways or guidelines that insurers start to point… I think we could certainly adapt our coverage criteria too, if it becomes a standard of care.…” (Pharmacy Director #4 - Regional PBM
Payers also stressed the importance of the Food and Drug Administration (FDA) approving and including pharmacogenetic testing on a product label. Some indicated that it would be an absolute necessity to have FDA labeling, “I think it’s still going to have to be approved by the FDA. It has to be part of the product labeling. You don’t see too many other ways around that. (Medical Director #2 - Regional PBM with medical policy) Another payer believed that the FDA should apply pressure to the pharmaceutical industry, although this would not apply to post-marketed drugs:
“What we’re hoping to see down the road as part of the drug approval process…before the drug even is allowed to come to market, (is the FDA) requiring that manufacturers have some sort of companion diagnostic or predictive test that’s going to show whether the drug will work on a given patient. (Pharmacy Director #4 - Regional PBM)
Impact of current implementation projects
Payers were pleased that academic centers were implementing preemptive pharmacogenetic testing. Some suggested these initiatives provided the framework for similar implementations in other settings, especially for those in smaller or integrated networks. Others await the resulting outcome-based clinical studies:
“I’d also like to see their (implementation projects) data and how it’s made a difference, and what specific entity, what diseases they treated, and what were the outcomes based on the choices that they’ve made… Did they actually change the medication, did they alter the dose of the medication…was the patient discharged sooner…?” (Medical Director #1 - Large National Plan)
See Table 4 for additional verbatim quotes from this domain.
Table 4.
Additional verbatim quotes from the dimensions of the coverage and policy development domain
| Preventive population health | I think to the extent that a mapping can become part of the preventive health guideline that goes with your annual well visit and it’s as simple as just when we do a CBC as [part of] an annual well visit…at a price point and convenience point…add to that, if it became commoditized and the price drops even further…I think that’s a great benefit for society. Preventive health guidelines for an annual well visit as the third companion lab diagnostic would be great. Pharmacy Director #5 - Regional Health Plan | We believe in population health management, so if that information which could proactively screen – like any other screening tests, there are fairly rigid criteria to justify a screening test. My reading it at this point is that it’s not reached that level where the evidence that an organization such as the National Preventers Services Task Force would advocate for it. Medical Director #5 - Medical Group with Insurance Policy | I think they’re going to be very cognizant of it as a concern we all have of drugs that are targeted. Having drugs available for small target populations notoriously meant much more expensive so that the cost savings by targeting the drugs may disappear because the drug prices will go up. Medical Director #5 - Medical Group with Insurance Policy |
| The role of CMS and the FDA | CMS would probably have to set something like this if there was a requirement for genetic testing. It would be a nightmare if a health plan decided that they were going to do it, and then somebody else did it, and then somebody else did it. Pharmacy Director #7 - Regional Health Plan | The FDA is the biggest standard. The second-biggest one is the societal guidelines. Really, behind those two, the secondary level is –again, it’s a subjective opportunity for a plan. Pharmacy Director #2 - Regional Health Plan | |
| Impact of current implementation projects | I think that we will all look at them and kind of learn from what they’ve done. I’m pretty bullish. I think a lot of good stuff’s going to come out of it and it’s going to help some smaller systems like ours be more comfortable to take that next step. Pharmacy Director #9 - Integrated Health System Plan | I think that, that cuts to what we were just talking about, which is that I think that when those organizations implement those programs and then they’re able to show results, that’s likely to eventually start to siphon over into things like treatment pathways and treatment guidelines that, “Hey look, these guys have found a test which is reliable whether you’re checking risk or treatment success.” Pharmacy Director #4 - Regional Pharmacy Benefit Manager | |
DISCUSSION
Preemptive germline pharmacogenetic testing does not appear to fit most payer’s mental model for genetic testing coverage decisions. Driven by familiarity with tumor mutation and companion diagnostics, payers desire the ability to make clear yes or no coverage decisions from a pharmacogenetic test. However, multi-gene pharmacogenetic testing provides a broad range of data with which to optimize drug therapy over time. Some germline pharmacogenetic testing is focused on drug selection, which could influence coverage decisions; but in other instances, the value is proactively selecting the correct dose, which does not involve drug coverage.
Payers valued the role of guidelines in both their decision making and in setting best practices for clinicians. CPIC was noted as a positive and enabling resource for preemptive pharmacogenetics. CPIC specifically focuses on how to use pharmacogenetic data once available.13 However, multiple payers were interested in CPIC moving beyond its current scope. Future work should explore the expanded use of guidelines for preemptive pharmacogenetics beyond CPIC and the potential impact on payer decision making.
Payers were open to evidence besides traditional RCTs, especially trials with a prospective component. A recent commentary from the payer community, citing the size and expense of clinical trials, opened the door for “positive influence on medical decision-making” as being “desirable” and “sufficient” evidence.28 However, minimal out-of-pocket costs was recognized as one of the top two reasons a clinician would order a pharmacogenetic test.29 Without broader reimbursement policies, real-world studies aimed at evaluating the influence of pharmacogenetics on medical decision-making will be difficult to conduct. A method to consider comes from a recent study in a polypharmacy elderly population that showed significant decreases in cost and resource utilization in a prospective pharmacogenetic tested cohort propensity score matched to a retrospective non-tested cohort.30 Real-world prospective studies could address questions on the incremental benefit of the testing and treating strategy over treating and monitoring. Some payers were willing to accept trial and error for commoditized medications, and placed less value on enabling clinicians to quickly select a more precise drug.
Seen as a valuable tool to both payers and clinicians, the NNT becomes more complex when applied to preemptive pharmacogenetics. The wide range of benefits to the patient must be considered: from selecting the right dose to avoiding a hospitalization or adverse event. As implementation of pharmacogenetics matures, clearly documenting these outcomes will enable calculations of meaningful NNTs. Recent work describes appropriate methods for evaluating population health impacts from pharmacogenetic tests including the NNT, as well as the population attributable fraction.31
Payers quickly identified that the value of testing will differ greatly across subsets of the population they cover. Recognizing preemptive pharmacogenetics provides value over a lifetime, traditional fee-for-service reimbursement models, in which payers are incentivized to meet an annual budget target, do not encourage preemptive testing. Although payers were concerned about adverse events, they were not confident that preemptive pharmacogenetic testing would provide a return within the common one-year cost-benefit timeframe. Further research should pursue models of the economic and clinical benefits potential realized from multi-gene preemptive testing in smaller subsets of populations based on age, co-morbidities, polypharmacy, and other risk factors. The RIGHT project may address this gap by estimating average clinical efficacy and cost-effectiveness of preemptive pharmacogenetic testing across diverse patient populations (rightsim.org).
Recommendations from the USPSTF for using preemptive pharmacogenetics as a preventive health service would be a paradigm shift that would pull influence away from the payer population. Preemptive pharmacogenetics will continue to struggle in a traditional reimbursement environment where decisions are made based on medical necessity. The concept of preemptively ordering a multi-gene panel before a diagnosis directly contradicts this approach, and thus, traditional payer decision making. Unlike other USPSTF endorsements, germline pharmacogenetic testing provides lifetime results, requiring updates only as additional gene-drug relationships are discovered.
With payer price sensitivity being quite inelastic for single patients, and the cost of several multi-gene panels approaching or less than the aforementioned $250 mark, clinicians and institutions may consider selecting a primary gene and drug of interest that payers currently reimburse, then ordering a multi-gene test that allows the remaining genes to be available preemptively over time. Blending single-gene associations currently deemed medically necessary with the low marginal cost of a multi-gene preemptive test may be a tractable scenario that fits payer interest in reimbursing specific genes and drugs while opening the benefits of preemptive testing to patients and clinicians, as well as to researchers following health outcomes.
Our study reveals barriers and facilitators for reimbursing preemptive pharmacogenetic testing. Although payers understand the potential benefits for patients and the health system from a preemptive approach, limited knowledge and narrow preference for acceptable study designs delay new reimbursement policies. Fundamentally, the preemptive testing model was a challenging economic construct. Concerns included large upfront costs with unpredictable downstream benefits and uncertainty of the use of test results within a timeframe of interest to the payer. The influence of the FDA, CMS, and NIH-funded implementation projects serve unique, parallel roles in facilitating widespread implementation. A cultural and regulatory shift of preemptive pharmacogenetics to a preventive health service would have broad implications on coverage and population health. Although the study sample cast a wide geographic net, it may be limited in scope by the high percentage of commercial payers. An increased focus on patients with high medication use, such as Medicare beneficiaries, should be considered to address this limitation.32 Prospective outcome studies, more precise definitions of target populations, and predictive economic models are also important considerations for future research in this area. As genetic technologies continue to development, the pharmacogenetics community must collaborate with policy-makers to establish precedents to responsibly evaluate and communicate the value of preemptive pharmacogenetics.
Supplementary Material
Acknowledgments
We thank Medical Marketing Economics, LLC for providing access to their payer panel, and the individuals who provided face-validity assessments of the interview guide: Samuel Johnson, Pharm.D., Julie Field, Ph.D., Sarah Bland, MBA, MPH, and members of the St. Jude Children’s Research Hospital PG4KDS protocol team.
Footnotes
Conflicts of interest
This work was funded, in part, by the National Institutes of Health (R24GM115264) and ALSAC; the Center for Pharmaceutical Marketing and Management at the University of Mississippi provided funding for professional transcription of the interviews.
References
- 1.Shuldiner AR, Relling MV, Peterson JF, et al. The Pharmacogenomics Research Network Translational Pharmacogenetics Program: Overcoming Challenges of Real-World Implementation. Clin Pharmacol Ther. 2013;94(2):207–210. doi: 10.1038/clpt.2013.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bielinski SJ, Olson JE, Pathak J, et al. Preemptive genotyping for personalized medicine: design of the right drug, right dose, right time—using genomic data to individualize treatment protocol. Paper presented at: Mayo Clin Pro; 2014. pp. 25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weitzel KW, Cavallari LH, Lesko LJ. Preemptive Panel-Based Pharmacogenetic Testing: The Time is Now. Pharm Res. 2017;34(8):1551–1555. doi: 10.1007/s11095-017-2163-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Relling MV, Evans WE. Pharmacogenomics in the clinic. Nature. 2015;526(7573):343–350. doi: 10.1038/nature15817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoffman JM, Haidar CE, Wilkinson MR, et al. PG4KDS: A model for the clinical implementation of pre-emptive pharmacogenetics. Am J Med Genet C Semin Med Genet. 2014;166C(1):45–55. doi: 10.1002/ajmg.c.31391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Society of Health-System Pharmacists. ASHP statement of the pharmacist’s role in clinical pharmacogenomics. Am J Health-Syst Pharm. 2015;72:579–81. doi: 10.2146/sp150003. [DOI] [PubMed] [Google Scholar]
- 7.Dunnenberger HM, Crews KR, Hoffman JM, et al. Preemptive Clinical Pharmacogenetics Implementation: Current programs in five United States medical centers. Annu Rev Pharmacol Toxicol. 2015;55:89. doi: 10.1146/annurev-pharmtox-010814-124835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schildcrout JS, Denny JC, Bowton E, et al. Optimizing drug outcomes through pharmacogenetics: a case for preemptive genotyping. Clin Pharmacol Ther. 2012;92(2):235–242. doi: 10.1038/clpt.2012.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’donnell PH, Danahey K, Jacobs M, et al. Adoption of a clinical pharmacogenomics implementation program during outpatient care–initial results of the University of Chicago “1,200 Patients Project”. Am J Med Genet C Semin Med Genet. 2014;166C(1):68–75. doi: 10.1002/ajmg.c.31385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weitzel KW, Elsey AR, Langaee TY, et al. Clinical pharmacogenetics implementation: approaches, successes, and challenges. Am J Med Genet C Semin Med Genet. 2014;166C(1):56–67. doi: 10.1002/ajmg.c.31390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Driest SL, Shi Y, Bowton EA, et al. Clinically actionable genotypes among 10,000 patients with preemptive pharmacogenomic testing. Clin Pharmacol Ther. 2014;95(4):423–431. doi: 10.1038/clpt.2013.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samwald M, Xu H, Blagec K, et al. Incidence of Exposure of Patients in the United States to Multiple Drugs for Which Pharmacogenomic Guidelines Are Available. PloS One. 2016;11(10):e0164972. doi: 10.1371/journal.pone.0164972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caudle KE, Klein TE, Hoffman JM, et al. Incorporation of pharmacogenomics into routine clinical practice: the Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline development process. Curr Drug Metab. 2014;15(2):209–217. doi: 10.2174/1389200215666140130124910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caudle KE, Gammal RS, Whirl-Carrillo M, Hoffman JM, Relling MV, Klein TE. Evidence and resources to implement pharmacogenetic knowledge for precision medicine. Am J Health Syst Pharm. 2016;73(23):1977–1985. doi: 10.2146/ajhp150977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bush WS, Crosslin DR, Owusu-Obeng A, et al. Genetic variation among 82 pharmacogenes: The PGRNseq data from the eMERGE network. Clin Pharmacol Ther. 2016;100(2):160–169. doi: 10.1002/cpt.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lynch JA, Berse B, Dotson WD, Khoury MJ, Coomer N, Kautter J. Utilization of genetic tests: analysis of gene-specific billing in Medicare claims data. Genet Med. 2017 doi: 10.1038/gim.2016.209. e-pub ahead of print 26 Jan 2017. [DOI] [PubMed] [Google Scholar]
- 17.Cohen J, Wilson A, Manzolillo K. Clinical and economic challenges facing pharmacogenomics. Pharmacogenomics J. 2013;13(4):378–388. doi: 10.1038/tpj.2011.63. [DOI] [PubMed] [Google Scholar]
- 18.Meckley LM, Neumann PJ. Personalized medicine: factors influencing reimbursement. Health Policy. 2010;94(2):91–100. doi: 10.1016/j.healthpol.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Trosman JR, Van Bebber SL, Phillips KA. Coverage policy development for personalized medicine: private payer perspectives on developing policy for the 21-gene assay. Journal Oncol Pract. 2010;6(5):238–242. doi: 10.1200/JOP.000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hresko A, Haga SB. Insurance coverage policies for personalized medince. J Pers Med. 2012;2:201–216. doi: 10.3390/jpm2040201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leung MY, Halpern MT, West ND. Pharmaceutical technology assessment: perspectives from payers. J Manag Care Pharm. 2012;18(3):256–265. doi: 10.18553/jmcp.2012.18.3.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lam Y. Scientific challenges and implementation barriers to translation of pharmacogenomics in clinical practice. ISRN Pharmacol. 2013;2013 doi: 10.1155/2013/641089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deverka P. Pharmacogenomics, evidence, and the role of payers. Public Health Genomics. 2009;12(3):149–157. doi: 10.1159/000189627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Faulkner E, Annemans L, Garrison L, et al. Challenges in the development and reimbursement of personalized medicine—payer and manufacturer perspectives and implications for health economics and outcomes research: a report of the ISPOR Personalized Medicine Special Interest Group. Value Health. 2012;15(8):1162–1171. doi: 10.1016/j.jval.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 25.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elo S, Kyngäs H. The qualitative content analysis process. Journal Adv Nurs. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 27.Foley G, Timonen V. Using grounded theory method to capture and analyze health care experiences. Health Serv Res. 2015;50(4):1195–1210. doi: 10.1111/1475-6773.12275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pezalla EJ. Payer view of personalized medicine. Am J Health Syst Pharm. 2016;73(23):2007–2012. doi: 10.2146/ajhp160038. [DOI] [PubMed] [Google Scholar]
- 29.Peterson JF, Field JR, Shi Y, et al. Attitudes of clinicians following large-scale pharmacogenomics implementation. Pharmacogenomics J. 2016;16(4):393–398. doi: 10.1038/tpj.2015.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brixner D, Biltaji E, Bress A, et al. The effect of pharmacogenetic profiling with a clinical decision support tool on healthcare resource utilization and estimated costs in the elderly exposed to polypharmacy. J Med Econ. 2016;19(3):213–228. doi: 10.3111/13696998.2015.1110160. [DOI] [PubMed] [Google Scholar]
- 31.Tonk E, Gurwitz D, Maitland-van der Zee A, Janssens A. Assessment of pharmacogenetic tests: presenting measures of clinical validity and potential population impact in association studies. Pharmacogenomics J. 2016 doi: 10.1038/tpj.2016.34. e-pub ahead of print 10 May 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert OpinDrug Saf. 2014;13(1):57–65. doi: 10.1517/14740338.2013.827660. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.