Abstract
Hepcidin and ferroportin, which are known as key iron regulators, may be used in future treatments of pancreatic ductal adenocarcinoma. Iron is essential for life support; it helps oxygen molecules bind to hemoglobin and acts as an important catalytic enzyme center. However, iron overload is a risk factor for cancer, possibly through the generation of reactive oxygen species (ROS). Hepcidin, which is a peptide hormone mainly generated by the liver, inhibits iron absorption via enterocytes and iron release from macrophages. Notably, hepcidin regulates iron homeostasis in the body by regulating the iron transporter ferroportin. In the present study, it was assumed that high hepcidin expression and low ferroportin expression result in malignancy. Therefore, it was examined whether hepcidin and ferroportin expression levels were correlated with the prognosis of pancreatic cancer in patients. Results revealed that high hepcidin expression levels and low ferroportin expression levels in pancreatic cancer tissue were significantly associated with poor prognosis in the analyses of overall survival (P=0.0140 and 0.0478, respectively). Additionally, there was no significant difference in disease-free survival in the hepcidin- and ferroportin-staining groups. Hepcidin expression correlated with the pathological stage and vascular invasion (P=0.0493 and 0.0400, respectively), and ferroportin expression was correlated with age (P=0.0372). Multivariate analysis of overall survival in the hepcidin-staining group revealed that pathological N factor (pN), adjuvant chemotherapy, and hepcidin expression were independent prognostic factors (P=0.0450, 0.0002, and 0.0049, respectively). Similarly, multivariate analysis of overall survival in the ferroportin-staining group revealed that vascular invasion, and ferroportin expression were independent prognostic factors (P=0.0028, P<0.0001, and P=0.0056, respectively). Thus, hepcidin and ferroportin expressions might be novel prognostic indicators for pancreatic cancer.
Keywords: pancreatic cancer, hepcidin, ferroportin, immunohistochemistry, iron, reactive oxygen species
Introduction
Pancreatic ductal adenocarcinoma (PDAC) is a lethal neoplasm due to its potential for distant metastasis in early stages of the disease, and it has a five-year survival rate of approximately 6% (1). PDAC has poor prognosis because it is difficult to detect in the early stages and exhibits rapid progression (2). Although surgery is the only treatment option that improves survival, it is curative in only 10–20% of cases (3). Therefore, to improve the prognosis of patients with pancreatic cancer, novel therapeutic agents need to be developed.
Recently, iron metabolism has been targeted for the development of new cancer therapeutic agents. Iron is associated with many vital reactions such as respiration and is essential for life support; it helps oxygen molecules bind to hemoglobin and acts as an important catalytic center for many enzymes, e.g., cytochromes (4). Iron is incorporated into the enzymes and proteins required for important cellular processes, such as oxygen transport, proliferation and energy production (5). Iron absorption in the duodenum and upper jejunum is highly regulated to maintain iron levels in the body (6). However, iron works as a double-edged sword; iron overload is a risk factor for cancer, presumably through the generation of reactive oxygen species (ROS). ROS include superoxide (O2•-), peroxides (H2O2 and ROOH), and free radicals (HO• and RO•), which are generated through the Fenton reaction. This persistent oxidative stress has been shown to induce carcinogenesis (7–9).
Cancer cells also depend on iron for proliferation; JARID1B, a well-known example, is an epigenetic factor that works as an H3K4 demethylase and activates cell growth in melanoma, esophageal cancer, colon cancer, breast cancer, and prostate cancer (10–14). Iron is required as a cofactor to upregulate JARID1B activity (13). Conversely, several studies have shown that iron deprivation inhibits in vitro tumor growth (15).
Hepcidin is a key peptide hormone that regulates iron homeostasis in chordates and is produced by the liver in response to inflammatory stimuli and iron overload (16,17). Hepcidin is a small antimicrobial peptide that inhibits iron absorption by enterocytes, iron release from macrophages, and iron transport across the placenta. The role of hepcidin is shown to be related to its regulation of the iron transporter ferroportin (18). Ferroportin is an important regulator of iron metabolism in the body and is a membrane transport protein that transfers intracellular iron to the extracellular environment. Reduced ferroportin expression on the cell surface leads to an increase in intracellular free iron, making the tumor cells more aggressive (19). Hepcidin binds to ferroportin on the cell surface and induces ferroportin internalization and degradation, which elevates the intracellular iron levels (20). In breast tumors, it has been suggested that tumor hepcidin expression is marginally increased relative to adjacent tissues. By contrast, tumor ferroportin concentration is greatly reduced in breast tumors, particularly in malignant tumors, compared with concentration in adjacent tissues (21).
Therefore, we hypothesized that high hepcidin expression levels contribute to a decrease in the expression of its downstream receptor ferroportin and an increase in intracellular iron retention, which accelerates tumor malignancy (tumor cell growth and disease progression) in patients with pancreatic cancer and finally leads to poor outcomes of the disease. In the present study, we examined whether hepcidin and ferroportin expressions are associated with prognosis of patients with pancreatic cancer.
Materials and methods
Patients and paraffin-embedded tissue samples
Ninety-two pancreatic tissue samples in total were obtained from patients with pancreatic cancer who received curative surgery between March 2007 and September 2013 at the Department of Gastroenterological Surgery, Osaka University Hospital. These samples were fixed in 10% formaldehyde and embedded in paraffin. We diagnosed the clinicopathological stage according to the Union for International Cancer Control TNM Classification of Malignant Tumors, 7th edition. The use of paraffin blocks in this study was approved by the Institutional Review Board. We obtained written consent from all patients at the beginning of the study. The present study was performed as a retrospective study on samples.
Immunohistochemical staining
Immunohistochemical staining was performed using the previously described method (22). Briefly, paraffin blocks were cut into 4-µm sections. Next, the sections were deparaffinized in xylene and treated with a boiled antigen retrieval solution; endogenous peroxidase activity was blocked using 0.3% hydrogen peroxide for 20 min at room temperature, and the sections were incubated overnight at 4°C with a specific antibody [anti-hepcidin antibody: Mouse monoclonal, 1:100 dilution (Abcam, Cambridge, MA, USA); anti-SLC40A1: Rabbit polyclonal, 1:200 dilution (Abcam)]. As a positive control for hepcidin antibodies, a liver sample was used, and as a positive control for ferroportin antibodies, a colon sample was used. Thereafter, the sections were incubated with a secondary antibody for 1 h at room temperature and assessed using avidin-biotin complex reagents (Vector Laboratories, Inc., Burlingame, CA, USA). The sections stained for hepcidin and ferroportin were incubated in 3,3′-diaminobenzidine for 1.5 and 2.5 min, respectively. Subsequently, all sections were counterstained with hematoxylin.
Evaluation of hepcidin and ferroportin expression in pancreatic cancer tissues
Expressions of hepcidin and ferroportin were evaluated according to the staining intensity of pancreatic duct epithelial cells in cancer tissues. Pancreatic duct epithelial cells exhibiting the same or higher staining intensity as that of the positive control were classified as the strongly-stained group, whereas those exhibiting weaker staining intensity than that of the control and the cells that were not stained at all were classified as the weakly-stained group. The evaluation of immunostaining intensity was performed by two observers (R.T and M.M.).
Statistical analysis
Continuous variables were expressed as mean ± standard deviation. The associations between categorical variables and hepcidin or ferroportin expression were assessed using the Pearson chi-squared test. Overall survival (OS) was defined as the time elapsed from the date of surgery until the date of tumor-induced death or the last follow-up, and was assessed using the Kaplan-Meier method; the log-rank test was used for comparisons. Recurrence-free survival (RFS) was defined as the time elapsed from the date of surgery until the date of tumor-recurrence or the last follow-up.
Univariate and multivariable Cox proportional hazard models were used to explore the association between age, sex, tumor size, location, histopathological type, pathological T factor (pT), pN, pathological stage (pStage), vascular invasion, neural invasion and adjuvant chemotherapy, and hepcidin expression. These models were used in evaluating the OS and RFS. Ferroportin expression was also evaluated in the same manner. P<0.05 was considered to indicate a statistically significant difference. All statistical analyses were performed using JMP Pro® 12 software (SAS Institute Inc., Cary, NC, USA).
Results
Immunohistochemistry for hepcidin in pancreatic cancer tissues
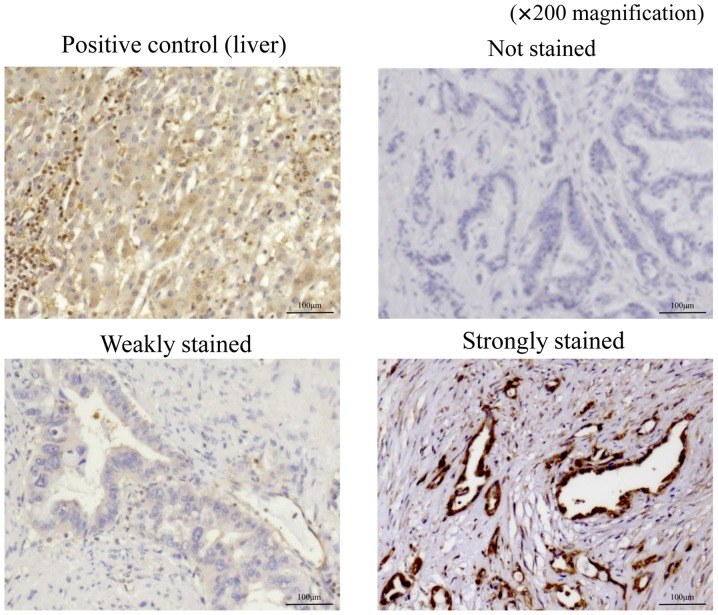
Table I shows the clinicopathological features of 92 patients with pancreatic cancer who underwent curative resection. Stained sections were classified into three categories based on staining intensity: Not stained; weakly stained (stained weaker than positive control); and strongly stained (stained equal to or stronger than positive control; Fig. 1). The sections that were weakly stained or not stained were included in the weakly-stained group, which comprised 26 patients, and those that were strongly stained were included in the strongly-stained group, which comprised 66 patients.
Table I.
Clinicopathological features in 92 patients with pancreatic cancer.
| Variables | Value |
|---|---|
| Age (years) | 67.3±9.99 |
| Sex (M/F) | 57/35 |
| Tumor size (mm) | 24.8±12.0 |
| Location (Ph/Pb/Pt) | 60/23/9 |
| Histopathological type (tub/por/muc) | 87/4/1 |
| pT (1/2/3/4) | 17/9/65/1 |
| pN (0/1) | 61/31 |
| pStage (IA/IB/IIA/IIB/III/IV) | 15/7/38/30/1/1 |
| Vascular invasion (0/1 or 2 or 3) | 22/70 |
| Neural invasion (0/1 or 2 or 3) | 16/76 |
| Adjuvant chemotherapy (complete/failure) | 58/34 |
M, male; F, female; Ph, pancreas head; Pb, pancreas body; Pt, pancreas tail; tub, tubular adenocarcinoma; Por, poorly differentiated adenocarcinoma; muc, mucinous adenocarcinoma.
Figure 1.
Immunohistochemistry findings for hepcidin staining are shown at ×200 magnification. Liver sections were used as positive control for hepcidin staining. Stained sections of pancreatic cancer tissues were classified into three categories according to staining intensity: Not stained; weakly stained (stained weaker than positive control); and strongly stained (stained equal to or stronger than positive control).
The clinicopathological features based on hepcidin expression are summarized in Table II. Among the examined pathological features, we detected a significant difference in pStage and vascular invasion.
Table II.
Clinicopathological features based on hepcidin expression.
| Variables | Weakly or not stained (n=26) | Strongly stained (n=66) | P-value |
|---|---|---|---|
| Age (≥65/<65 years) | 15:11 | 43:23 | 0.5045 |
| Sex (M/F) | 15:11 | 42:24 | 0.5970 |
| Tumor size (≥20/<20 mm) | 12:14 | 45:21 | 0.0500 |
| Location (Ph/Pb or Pt) | 19:7 | 41:25 | 0.3205 |
| Histopathological type (por or muc/tub) | 2:24 | 3:63 | 0.5488 |
| pT (1 or 2/3 or 4) | 10:16 | 15:51 | 0.1266 |
| pN (0/1) | 21:5 | 39:27 | 0.0654 |
| pStage (IIB or III or IV/IA or IB or IIA) | 5:21 | 39:27 | 0.0493a |
| Vascular invasion (0/1 or 2 or 3) | 10:16 | 12:54 | 0.0400a |
| Neural invasion (0/1 or 2 or 3) | 7:19 | 10:56 | 0.1902 |
| Adjuvant chemotherapy (failure/complete) | 9:17 | 25:41 | 0.7703 |
P-values were calculated using the Pearson chi-squared test.
P<0.05. M, male; F, female; Ph, pancreas head; Pb, pancreas body; Pt, pancreas tail; tub, tubular adenocarcinoma; Por, poorly differentiated adenocarcinoma; muc, mucinous adenocarcinoma.
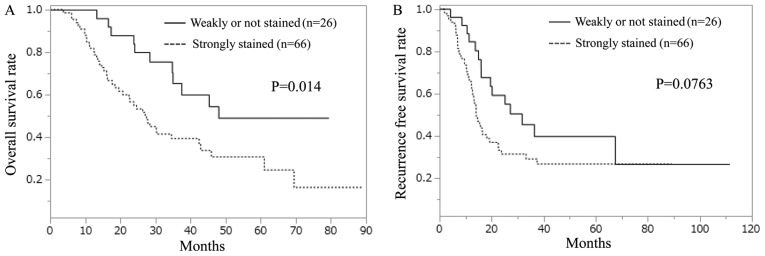
The strongly-stained hepcidin group exhibited a significantly shorter OS than did the weakly-stained hepcidin group (Fig. 2A). In terms of RFS, no significant difference was observed between the strongly- and weakly-stained hepcidin groups; however, the strongly-stained group displayed a tendency toward worse RFS compared with the weakly-stained group (Fig. 2B).
Figure 2.
Kaplan-Meier survival curves in relation to hepcidin staining. (A) Overall survival curve. (B) Recurrence-free survival (RFS) curve. P-values were calculated using the log-rank test.
Univariate analysis revealed significant differences in pN, pStage, vascular invasion, adjuvant chemotherapy, and hepcidin expression (Table III). pStage and vascular invasion were excluded from multivariate analysis because they were associated with hepcidin expression, as described in Table II. Multivariate analysis indicated significant differences in pN, adjuvant chemotherapy, and hepcidin expression; therefore, these items were found to be independent prognostic factors.
Table III.
Univariate and multivariate analysis for overall survival in relation to hepcidin staining.
| Univariate analysis | Multivariate analysis | ||
|---|---|---|---|
| Variables | P-value | HR (95% CI) | P-value |
| Age (≥65/<65 years) | 0.1945 | ||
| Sex (M/F) | 0.9873 | ||
| Tumor size (≥20/<20 mm) | 0.0513 | ||
| Location (Ph/Pb or Pt) | 0.9346 | ||
| Histopathological type (por or muc/tub) | 0.4726 | ||
| pT (3 or 4/1 or 2) | 0.2014 | ||
| pN (1/0) | 0.0203a | 1.83 (1.07–3.10) | 0.0450a |
| pStage (IIB or III or IV/IA or IB or IIA) | 0.0106a | ||
| Vascular invasion (+/−) | 0.0060a | ||
| Neural invasion (1 or 2 or 3/0) | 0.0880 | ||
| Adjuvant chemotherapy (failure/complete) | 0.0006a | 2.64 (1.55–4.47) | 0.0002a |
| Hepcidin (Strongly stained/Weakly or no stained) | 0.0104a | 2.20 (1.19–4.38) | 0.0049a |
P-values from univariate analysis were calculated using log-rank test.
P<0.05. P-values from multivariate analysis were calculated using Cox proportional hazards regression analysis. HR, hazard ratio; CI, confidence interval; M, male; F, female; Ph, pancreas head; Pb, pancreas body; Pt, pancreas tail; tub, tubular adenocarcinoma; Por, poorly differentiated adenocarcinoma; muc, mucinous adenocarcinoma.
Univariate analysis of RFS was performed in a similar manner to that of OS (Table IV). pStage and vascular invasion significantly differed in the univariate analysis; however, there were no significant differences in the multivariate analysis.
Table IV.
Univariate and multivariate analysis for recurrence-free survival in relation to hepcidin staining.
| Univariate analysis | Multivariate analysis | ||
|---|---|---|---|
| Variables | P-value | HR (95% CI) | P-value |
| Age (≥65/<65 years) | 0.7707 | ||
| Sex (M/F) | 0.9452 | ||
| Tumor size (≥20/<20 mm) | 0.2565 | ||
| Location (Ph/Pb or Pt) | 0.9453 | ||
| Histopathological type (por or muc/tub) | 0.3270 | ||
| pT (3 or 4/1 or 2) | 0.3038 | ||
| pN (1/0) | 0.0679 | ||
| pStage (IIB or III or IV/IA or IB or IIA) | 0.0408a | 1.63 (0.91–2.91) | 0.0983 |
| Vascular invasion (+/−) | 0.0358a | 2.19 (0.99–5.52) | 0.0521 |
| Neural invasion (1 or 2 or 3/0) | 0.4832 | ||
| Adjuvant chemotherapy (failure/complete) | 0.0581 | ||
| Hepcidin (Strongly stained/Weakly or no stained) | 0.0684 | ||
P-values from univariate analysis were calculated using log-rank test.
P<0.05. P-values from multivariate analysis were calculated using Cox proportional hazards regression analysis. HR, hazard ratio; CI, confidence interval; M, male; F, female; Ph, pancreas head; Pb, pancreas body; Pt, pancreas tail; tub, tubular adenocarcinoma; Por, poorly differentiated adenocarcinoma; muc, mucinous adenocarcinoma.
Immunohistochemistry for ferroportin in pancreatic cancer tissues
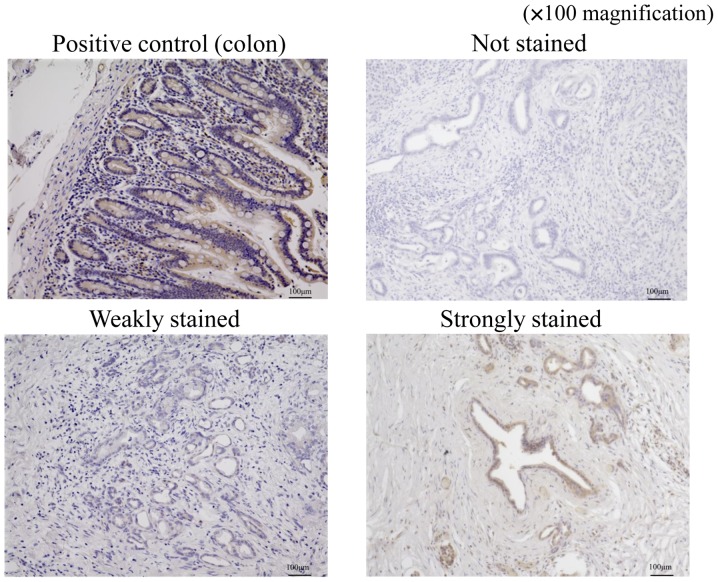
We evaluated immunostaining for ferroportin using a method similar to that used for hepcidin. Stained sections were classified into three categories based on staining intensity: Not stained; weakly stained (stained weaker than positive control); and strongly stained (stained equal to or stronger than positive control; Fig. 3). The sections that were weakly stained or not stained were included in the weakly-stained group and those that were strongly stained were included in the strongly-stained group.
Figure 3.
Immunohistchemistry findings for ferroportin staining are shown at ×100 magnification. Colon sections were used as positive control for ferroportin staining. Stained sections of pancreatic cancer tissues were classified into three categories according to staining intensity: Not stained; weakly stained (stained weaker than positive control); and strongly stained (stained equal to or stronger than positive control).
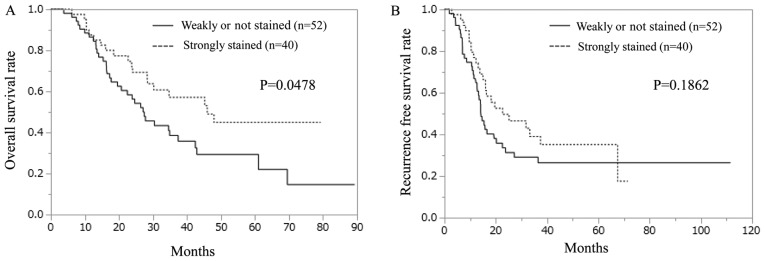
The clinicopathological features based on ferroportin expression are summarized in Table V. Among the examined pathological features, we detected a significant difference only in age. Unlike the hepcidin samples, the weakly-stained ferroportin group exhibited significantly shorter OS than did the strongly-stained ferroportin group (Fig. 4A). In terms of RFS, no significant difference was observed between the strongly- and weakly-stained ferroportin groups (Fig. 4B).
Table V.
Clinicopathological features based on ferroportin expression.
| Variables | Weakly or not stained (n=52) | Strongly stained (n=40) | P-value |
|---|---|---|---|
| Age (≥65/<65 years) | 28:24 | 30:10 | 0.0372a |
| Sex (M/F) | 32:20 | 25:15 | 0.9250 |
| Tumor size (≥20/<20 mm) | 33:19 | 24:16 | 0.7346 |
| Location (Ph/Pb or Pt) | 37:15 | 23:17 | 0.1728 |
| Histopathological type (por or muc/tub) | 4:48 | 1:39 | 0.2761 |
| pT (1 or 2/3 or 4) | 12:40 | 13:27 | 0.4099 |
| pN (0/1) | 33:19 | 28:12 | 0.5107 |
| pStage (IIB or III or IV/IA or IB or IIA) | 19:33 | 13:27 | 0.6868 |
| Vascular invasion (0/1 or 2 or 3) | 11:41 | 11:29 | 0.4793 |
| Neural invasion (0/1 or 2 or 3) | 7:45 | 10:30 | 0.1575 |
| Adjuvant chemotherapy (failure/complete) | 17:35 | 17:23 | 0.3340 |
P-values were calculated using the Pearson chi-squared test.
P<0.05. M, male; F, female; Ph, pancreas head; Pb, pancreas body; Pt, pancreas tail; tub, tubular adenocarcinoma; Por, poorly differentiated adenocarcinoma; muc, mucinous adenocarcinoma.
Figure 4.
Kaplan-Meier survival curves in relation to ferroportin staining. (A) Overall survival curve. (B) Recurrence-free survival (RFS) curve. P-values were calculated using the log-rank test.
Univariate and multivariate analyses for OS with respect to ferroportin staining are shown in Table VI. As described in Table III, in addition to pN, pStage, vascular invasion, and adjuvant chemotherapy, there was a significant difference in ferroportin expression. pStage was excluded from the multivariate analysis because it seemed to be associated with pN. Multivariate analysis revealed significant differences in vascular invasion, adjuvant chemotherapy, and ferroportin expression; therefore, these were considered to be independent prognostic factors.
Table VI.
Univariate and multivariate analysis for overall survival in relation to ferroportin staining.
| Univariate analysis | Multivariate analysis | ||
|---|---|---|---|
| Variables | P-value | HR (95% CI) | P-value |
| Age (≥65/<65 years) | 0.1945 | ||
| Sex (M/F) | 0.9873 | ||
| Tumor size (≥20/<20 mm) | 0.0513 | ||
| Location (Ph/Pb or Pt) | 0.9346 | ||
| Histopathological type (por or muc/tub) | 0.4726 | ||
| pT (3 or 4/1 or 2) | 0.2014 | ||
| pN (1/0) | 0.0203a | 1.17 (0.64–2.11) | 0.6060 |
| pStage (IIB or III or IV/IA or IB or IIA) | 0.0106a | ||
| Vascular invasion (+/−) | 0.0060a | 3.43 (1.50–8.90) | 0.0028a |
| Neural invasion (1 or 2 or 3/0) | 0.0880 | ||
| Adjuvant chemotherapy (failure/complete) | 0.0006a | 4.37 (2.35–8.20) | <.0001a |
| Ferroportin (Weakly or no stained/strongly stained) | 0.0459a | 2.25 (1.26–4.14) | 0.0056a |
P-values from univariate analysis were calculated using log-rank test.
P<0.05. P-values from multivariate analysis were calculated using Cox proportional hazards regression analysis. HR, hazard ratio; CI, confidence interval; M, male; F, female; Ph, pancreas head; Pb, pancreas body; Pt, pancreas tail; tub, tubular adenocarcinoma; Por, poorly differentiated adenocarcinoma; muc, mucinous adenocarcinoma.
Univariate analysis of RFS was performed in a manner similar to that of OS. Significant differences were noted in pStage and vascular invasion in the univariate analysis but not in the multivariate analysis (Table VII).
Table VII.
Univariate and multivariate analysis for recurrence-free survival in relation to ferroportin staining.
| Univariate analysis | Multivariate analysis | ||
|---|---|---|---|
| Variables | P-value | HR (95% CI) | P-value |
| Age (≥65/<65 years) | 0.7707 | ||
| Sex (M/F) | 0.9452 | ||
| Tumor size (≥20/<20 mm) | 0.2565 | ||
| Location (Ph/Pb or Pt) | 0.9453 | ||
| Histopathological type (por or muc/tub) | 0.3270 | ||
| pT (3 or 4/1 or 2) | 0.3038 | ||
| pN (1/0) | 0.0679 | ||
| pStage (IIB or III or IV/IA or IB or IIA) | 0.0408a | 1.48 (0.83–2.61) | 0.1582 |
| Vascular invasion (+/−) | 0.0358a | 1.62 (0.83–3.33) | 0.1835 |
| Neural invasion (1 or 2 or 3/0) | 0.4832 | ||
| Adjuvant chemotherapy (failure/complete) | 0.0581 | ||
| Ferroportin (Weakly or not stained/Strongly | 0.1846 | ||
P-values from univariate analysis were calculated using log-rank test.
P<0.05. P-values from multivariate analysis were calculated using Cox proportional hazards regression analysis. HR, hazard ratio; CI, confidence interval; M, male; F, female; Ph, pancreas head; Pb, pancreas body; Pt, pancreas tail; tub, tubular adenocarcinoma; Por, poorly differentiated adenocarcinoma; muc, mucinous adenocarcinoma.
Discussion
In recent years, iron metabolism has attracted attention as a mechanism in the carcinogenetic process. Above all, hepcidin and ferroportin are thought to play important roles. Hepcidin is a peptide hormone that regulates iron homeostasis by regulating the iron transporter ferroportin and is produced mainly by the liver. Hepcidin expression is increased by the inflammatory cytokine interleukin 6 (IL-6) and iron overload (23). IL-6 is a multifunctional cytokine that is produced by many different cell types and plays an important role in the regulation of inflammation and immune response (20,21). Hepcidin overexpression decreases iron absorption by inhibiting the iron transporter ferroportin in enterocytes and causes hypoferric anemia (24). Conversely, the dysfunction or genetic defect of hepcidin leads to hyperferremia, as observed in hemochromatosis (25). Similarly, mutations in FPN1, the gene that encodes ferroportin, result in iron overload disease that shows dominant inheritance and variations in phenotype (26).
Some reports have indicated that hepcidin and ferroportin expressions are involved in carcinogenesis and tumor malignancy, e.g., according to a report on breast cancer, high hepcidin expression was observed in cells with a high degree of malignancy (27). In colorectal cancer, hepcidin expression in urine is associated with Tstage, and it is detected to measure hepcidin levels in urine using mass spectrometry (28). The serum hepcidin level was significantly higher in patients with non-small cell lung cancer compared with noncancerous individuals (29). In a report on ferroportin, ferroportin overexpression was shown to inhibit lung and liver metastases by altering metastasis-relevant properties, including epithelial-mesenchymal transition (30).
Based on these findings, hepcidin and ferroportin were found to affect the malignancy of various cancers. Hepcidin expression occurs in the pancreas, although the expression level is much lower than that in the liver. Hence, we attempted to examine hepcidin expression in pancreatic cancer tissue. Similar to hepcidin expression, ferroportin expression also occurs in the pancreas (23). Therefore, we expected that hepcidin and ferroportin were possibly involved in patients' prognosis of pancreatic cancer and we decided to examine this involvement.
As clarified in our study, hepcidin expression was correlated with pStage and vascular invasion in patients with pancreatic cancer, and high expression in the hepcidin group indicated shorter OS. pN, adjuvant chemotherapy, and hepcidin expression were found to be independent prognostic factors for OS. Ferroportin expression was correlated with age, and low expression in the ferroportin group indicated shorter OS. Vascular invasion, adjuvant chemotherapy, and ferroportin expression were found to be independent prognostic factors for OS. There was no significant difference in disease-free survival in both the hepcidin- and ferroportin-staining groups.
As previously mentioned, it can be inferred that increases intracellular iron levels through hepcidin-ferroportin signaling might contribute to the malignancy of cancer. However, the detail of the mechanism is not known. One of the mechanisms that may be involved is associated with histone lysine demethylases (KDMs), including Jarid1B, as described in Background. Jarid1B was reported to be well expressed in breast cancers and breast cancer cell lines, but Jarid1B expression was not observed in almost all normal organs except for the testis and ovary (14). Moreover, the TCGA dataset indicated that Jarid1B RNA is expressed in various cancer tissues, including pancreatic cancer. In a prostate cancer cell line, the enzymatic activity of Jarid1B was significantly diminished in the absence of ascorbic acid, α-ketoglutarate, or Fe (II), or in the presence of an iron chelator (13). The data of our previous experiment also shows similar results (data not shown), supporting the notion that JARID1B is an iron-dependent dioxygenase.
To summarize what has been discussed in this paper, although the correlation between Jarid1B and hepcidin-ferroportin signaling has not yet been elucidated, hepcidin-ferroportin signaling promotes iron retention in cells; furthermore, the increase in iron retention activates Jarid1B enzyme activity as a silencer of the tumor suppressor gene. It could be inferred that this is a mechanism of malignant transformation.
Our findings provide new insight into the mechanisms underlying the important role of deregulated hepcidin-ferroportin signaling in cancer, and these findings might contribute to the development of an anticancer therapeutic target.
Acknowledgements
The authors would like to thank Dr Sakai at Osaka University (Osaka, Japan) for providing support in our data analysis and the members of our laboratories for their helpful discussions.
Funding
The present work was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology (grant nos. 17H04282, 17K19698; 16K15615 and 15H05791), a grant from P-DIRECT (grant no. 15cm0106105h0002; AMED-Japan Cancer Research Project).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
RT, MK and HI collaborated in the conception and design. RT, MK and HI were involved in the development of methodology. RT, MK, AA, JK, KA, TO, KM and HI were involved in the acquisition of data (provided the animals, acquired and managed patients, and provided the facilities). RT, MK, HE, TN, YI, DY, TA, HW, KK, KG, TK, TS, YD, MM and HI contributed to the analysis and interpretation of data (statistical analysis, biostatistics and computational analysis). RT, MK, HE, TN, HI wrote and revised the manuscript. MM and HI supervised the study.
Ethics approval and consent to participate
This study has been approved by the research Ethics Committee of Osaka University (ID of the approval: 15149-2) and written informed consent was obtained from all patients.
Consent for publication
Written informed consents were obtained from the patients for publication.
Competing interests
Institutional endowments were received partially from Taiho Pharmaceutical Co., Ltd., Evidence Based Medical Research Center, IDEA Consultants, Inc. (Tokyo, Japan), Unitech Co. Ltd. (Chiba, Japan), and Kinshu-kai Medical Corporation (Osaka, Japan) (Y.D., M.M., and H.I.); Chugai Co., Ltd., Yakult Honsha Co., Ltd., and Merck Co., Ltd (D.S., T.K., T.S., Y.D., and M.M.). These funders had no role in providing the primary experimental equipment, supply expenses, study design, data collection and analysis, decision to publish, or manuscript preparation for this work.
References
- 1.Tomihara H, Eguchi H, Yamada D, Gotoh K, Kawamoto K, Wada H, Asaoka T, Noda T, Takeda Y, Tanemura M, et al. Preoperative chemoradiotherapy does not compromise the feasibility of adjuvant chemotherapy for patients with pancreatic ductal adenocarcinoma. Surg Today. 2017;47:218–226. doi: 10.1007/s00595-016-1405-6. [DOI] [PubMed] [Google Scholar]
- 2.Hirayama K, Kono H, Nakata Y, Akazawa Y, Wakana H, Fukushima H, Fujii H. Expression of podoplanin in stromal fibroblasts plays a pivotal role in the prognosis of patients with pancreatic cancer. Surg Today. 2018;48:110–118. doi: 10.1007/s00595-017-1559-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamada D, Eguchi H, Asaoka T, Tomihara H, Noda T, Wada H, Kawamoto K, Gotoh K, Takeda Y, Tanemura M, et al. The basal nutritional state of PDAC patients is the dominant factor for completing adjuvant chemotherapy. Surg Today. 2017 Apr 18; doi: 10.1007/s00595-017-1522-x. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 4.Sharp P, Srai SK. Molecular mechanisms involved in intestinal iron absorption. World J Gastroenterol. 2007;13:4716–4724. doi: 10.3748/wjg.v13.i35.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oates PS. The role of hepcidin and ferroportin in iron absorption. Histol Histopathol. 2007;22:791–804. doi: 10.14670/HH-22.791. [DOI] [PubMed] [Google Scholar]
- 6.Franchini M, Montagnana M, Lippi G. Hepcidin and iron metabolism: From laboratory to clinical implications. Clin Chim Acta. 2010;411:1565–1569. doi: 10.1016/j.cca.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Dixon SJ, Stockwell BR. The role of iron and reactive oxygen species in cell death. Nat Chem Biol. 2014;10:9–17. doi: 10.1038/nchembio.1416. [DOI] [PubMed] [Google Scholar]
- 8.Yamada Y, Miyamoto T, Kashima H, Kobara H, Asaka R, Ando H, Higuchi S, Ida K, Shiozawa T. Lipocalin 2 attenuates iron-related oxidative stress and prolongs the survival of ovarian clear cell carcinoma cells by up-regulating the CD44 variant. Free Radic Res. 2016;50:414–425. doi: 10.3109/10715762.2015.1134795. [DOI] [PubMed] [Google Scholar]
- 9.Toyokuni S. Role of iron in carcinogenesis: Cancer as a ferrotoxic disease. Cancer Sci. 2009;100:9–16. doi: 10.1111/j.1349-7006.2008.01001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kano Y, Konno M, Ohta K, Haraguchi N, Nishikawa S, Kagawa Y, Hamabe A, Hasegawa S, Ogawa H, Fukusumi T, et al. Jumonji/Arid1b (Jarid1b) protein modulates human esophageal cancer cell growth. Mol Clin Oncol. 2013;1:753–757. doi: 10.3892/mco.2013.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohta K, Haraguchi N, Kano Y, Kagawa Y, Konno M, Nishikawa S, Hamabe A, Hasegawa S, Ogawa H, Fukusumi T, et al. Depletion of JARID1B induces cellular senescence in human colorectal cancer. Int J Oncol. 2013;42:1212–1218. doi: 10.3892/ijo.2013.1799. [DOI] [PubMed] [Google Scholar]
- 12.Roesch A, Fukunaga-Kalabis M, Schmidt EC, Zabierowski SE, Brafford PA, Vultur A, Basu D, Gimotty P, Vogt T, Herlyn M. A temporarily distinct subpopulation of slow-cycling melanoma cells is required for continuous tumor growth. Cell. 2010;141:583–594. doi: 10.1016/j.cell.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xiang Y, Zhu Z, Han G, Ye X, Xu B, Peng Z, Ma Y, Yu Y, Lin H, Chen AP, Chen CD. JARID1B is a histone H3 lysine 4 demethylase up-regulated in prostate cancer. Proc Natl Acad Sci USA. 2007;104:19226–19231. doi: 10.1073/pnas.0700735104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barrett A, Madsen B, Copier J, Lu PJ, Cooper L, Scibetta AG, Burchell J, Taylor-Papadimitriou J. PLU-1 nuclear protein, which is upregulated in breast cancer, shows restricted expression in normal human adult tissues: A new cancer/testis antigen? Int J Cancer. 2002;101:581–588. doi: 10.1002/ijc.10644. [DOI] [PubMed] [Google Scholar]
- 15.Weizer-Stern O, Adamsky K, Margalit O, Ashur-Fabian O, Givol D, Amariglio N, Rechavi G. Hepcidin, a key regulator of iron metabolism, is transcriptionally activated by p53. Br J Haematol. 2007;138:253–262. doi: 10.1111/j.1365-2141.2007.06638.x. [DOI] [PubMed] [Google Scholar]
- 16.Singh B, Arora S, Agrawal P, Gupta SK. Hepcidin: A novel peptide hormone regulating iron metabolism. Clin Chim Acta. 2011;412:823–830. doi: 10.1016/j.cca.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 17.Zhao N, Zhang AS, Enns CA. Iron regulation by hepcidin. J Clin Invest. 2013;123:2337–2343. doi: 10.1172/JCI67225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bekri S, Gual P, Anty R, Luciani N, Dahman M, Ramesh B, Iannelli A, Staccini-Myx A, Casanova D, Ben Amor I, et al. Increased adipose tissue expression of hepcidin in severe obesity is independent from diabetes and NASH. Gastroenterology. 2006;131:788–796. doi: 10.1053/j.gastro.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 19.Xue D, Zhou CX, Shi YB, Lu H, He XZ. Decreased expression of ferroportin in prostate cancer. Oncol Lett. 2015;10:913–916. doi: 10.3892/ol.2015.3363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li JJ, Meng X, Si HP, Zhang C, Lv HX, Zhao YX, Yang JM, Dong M, Zhang K, Liu SX, et al. Hepcidin destabilizes atherosclerotic plaque via overactivating macrophages after erythrophagocytosis. Arterioscler Thromb Vasc Biol. 2012;32:1158–1166. doi: 10.1161/ATVBAHA.112.246108. [DOI] [PubMed] [Google Scholar]
- 21.Zhang S, Chen Y, Guo W, Yuan L, Zhang D, Xu Y, Nemeth E, Ganz T, Liu S. Disordered hepcidin-ferroportin signaling promotes breast cancer growth. Cell Signal. 2014;26:2539–2550. doi: 10.1016/j.cellsig.2014.07.029. [DOI] [PubMed] [Google Scholar]
- 22.Asukai K, Kawamoto K, Eguchi H, Konno M, Nishida N, Koseki J, Noguchi K, Hasegawa S, Ogawa H, Yamada D, et al. Prognostic impact of peritumoral IL-17-positive cells and IL-17 axis in patients with intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2015;22(Suppl 3):S1524–S1531. doi: 10.1245/s10434-015-4782-y. [DOI] [PubMed] [Google Scholar]
- 23.Kulaksiz H, Fein E, Redecker P, Stremmel W, Adler G, Cetin Y. Pancreatic beta-cells express hepcidin, an iron-uptake regulatory peptide. J Endocrinol. 2008;197:241–249. doi: 10.1677/JOE-07-0528. [DOI] [PubMed] [Google Scholar]
- 24.D'Angelo G. Role of hepcidin in the pathophysiology and diagnosis of anemia. Blood Res. 2013;48:10–15. doi: 10.5045/br.2013.48.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pietrangelo A. Hereditary hemochromatosis: Pathogenesis, diagnosis, and treatment. Gastroenterology. 2010;139:393–408. doi: 10.1053/j.gastro.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 26.De Domenico I, Ward DM, Kaplan J. Hepcidin and ferroportin: The new players in iron metabolism. Semin Liver Dis. 2011;31:272–279. doi: 10.1055/s-0031-1286058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ciniselli CM, De Bortoli M, Taverna E, Varinelli L, Pizzamiglio S, Veneroni S, Bonini C, Orlandi R, Verderio P, Bongarzone I. Plasma hepcidin in early-stage breast cancer patients: No relationship with interleukin-6, erythropoietin and erythroferrone. Expert Rev Proteomics. 2015;12:695–701. doi: 10.1586/14789450.2015.1099436. [DOI] [PubMed] [Google Scholar]
- 28.Ward DG, Roberts K, Brookes MJ, Joy H, Martin A, Ismail T, Spychal R, Iqbal T, Tselepis C. Increased hepcidin expression in colorectal carcinogenesis. World J Gastroenterol. 2008;14:1339–1345. doi: 10.3748/wjg.14.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Q, Wang L, Ma Y, Wu X, Jin L, Yu F. Increased hepcidin expression in non-small cell lung cancer tissue and serum is associated with clinical stage. Thorac Cancer. 2014;5:14–24. doi: 10.1111/1759-7714.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guo W, Zhang S, Chen Y, Zhang D, Yuan L, Cong H, Liu S. An important role of the hepcidin-ferroportin signaling in affecting tumor growth and metastasis. Acta Biochim Biophys Sin (Shanghai) 2015;47:703–715. doi: 10.1093/abbs/gmv063. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.