Abstract
The aims were two-fold: to examine prevalence and correlates of lifetime potentially traumatic event (PTE) exposure and to explore the relationships between PTE exposure and mental health outcomes (i.e., trauma related distress, alcohol use quantity and frequency, depression symptoms, and anxiety symptoms) within a large sample of college freshmen. 6120 participants, consisting of three cohorts of incoming freshman at a large southeastern university, completed an online assessment battery measuring a multitude of factors including PTEs, personality, relationships (i.e., parental and peer), and mental health. The majority (81.8%) of participants endorsed experiencing at least one PTE within their lifetime and 39.0% reported at least one interpersonal trauma (i.e., physical assault, sexual assault, other unwanted or uncomfortable sexual situation). The average number of PTE categories endorsed was 1.71 (SD=1.30), and 8.7% of participants reported experiencing four or more separate PTE categories pre-college entry. Female gender and peer deviance were consistently associated with PTE exposure and symptoms of psychopathology. Furthermore, a history of interpersonal PTE exposure was associated with increased alcohol use (i.e., frequency and quantity), trauma related distress, depressive symptoms, and anxiety symptoms. The data demonstrate high prevalence PTE exposure among young adults and the clinical significance of a PTE history.
1. Introduction
Epidemiological studies suggest that upwards of 80% of US adults are exposed to at least one traumatic event during their lifetime (Breslau et al., 1998a; Kessler et al., 2005). Exposure to potentially traumatic events (PTEs) has been associated with an increased risk of psychiatric disorders including posttraumatic stress disorder (PTSD), generalized anxiety disorder, panic disorder, borderline personality disorder (Bandelow et al., 2005), psychosis (Read et al., 2005; van Nierop et al., 2014) depression, and problematic alcohol and drug use (Kilpatrick et al., 2003). Although PTEs are broadly associated with increased risk for psychopathology (Amstadter et al., 2013), the majority of those exposed do not develop negative mental health outcomes (Bonanno, 2004). Multiple phenotypic domains may be particularly relevant to PTE risk and post-PTE functioning including demographics/early environmental factors, PTE characteristics, and factors associated with resilience. However, these variables have not been examined concurrently, impeding the field’s ability to identify targets of relative importance for potential intervention.
Demographic characteristics and early environment not only influence the ways in which individuals will respond to a PTE, but also their risk of PTE exposure. Sex differences have been identified, whereby men possess greater risk for many types of PTE exposure (Breslau, 2002) while women exhibit increased risk of developing PTSD symptoms upon exposure to PTEs (Perrin et al., 2013). Age also affects risk, with individuals in late adolescence/early adulthood (i.e., 16–25 year-olds) being at greatest risk for PTE exposure and development of PTSD symptoms (Breslau et al., 1998b). Early environmental risk factors, such as poor perceived parenting (Lima et al., 2014; Punamaki et al., 2001) may also confer increased risk to PTE exposure. Specifically, permissive or authoritarian type parenting styles have been linked with poor outcomes following trauma exposure (Yeates et al., 2001) and greater risk of accidental injury among children (Morrongiello et al., 2006). Another early environmental factor associated with heightened risk of PTE exposure is exposure to peer deviance, which pertains to delinquent behavior of peers (e.g., drug use) (Rubens et al., 2013). Peer deviance has been identified as an antecedent for future delinquent acts (Elliott and Menard, 1996) which may increase the likelihood of PTE exposure. Trait-like individual difference characteristics, such as personality dimensions, also influence risk for PTE exposure and PTSD symptoms, with neuroticism consistently associated with both PTE risk (Jaksic et al., 2012; Kendler et al., 2003) and subsequent symptoms (Perrin et al., 2014).
In addition to demographic and early environment characteristics, facets of the PTE itself can influence how an individual responds to and recovers from the PTE. Specifically, greater PTE “load” (i.e., number of PTEs occurring over an individual’s lifetime) confers increased risk for psychiatric symptom development (Kaysen et al., 2010; Mollica et al., 1998; Shih et al., 2010). Interpersonal (e.g., physical or sexual assault) compared to non-interpersonal PTEs (e.g., accidental injury via transportation accidents) are also related to greater conditional probability of post-PTE psychopathology (Breslau et al., 1991). Furthermore, evidence indicates that survivors of interpersonal PTEs, particularly sexual assault, are at increased risk for additional assault (i.e., revictimization) compared to those without a prior history of assault (Nishith et al., 2000).
Conversely, factors associated with resilience, or one’s ability to withstand adversity, may also influence the impact of trauma exposure and related symptoms (Bonanno et al., 2007). Previous research on symptomatology post-PTE exposure demonstrates a “buffering” effect of social support against symptoms of PTSD, depression and other associated difficulties (Pietrzak et al., 2009). Low levels of perceived social support reflect higher endorsement of a PTSD diagnosis, symptoms of depression, and alcohol abuse (Meyer et al., 2012). One’s perceived ability to manage distress following PTE exposure has been also been associated with the construct of resilience (Benight and Bandura, 2004; Cieslak et al., 2009; Schwarzer et al., 2012). Specifically, individuals possessing positive perceptions regarding their ability to tolerate distress report fewer symptoms of PTSD and general distress post trauma exposure, whereas lower levels of positive perceptions may contribute to the use of ineffective coping strategies (Benight and Harper, 2002; Kibler and Lyons, 2004). Thus, inclusion of potential protective factors, such as social support and perceived resilience, are important for understanding risk of post-PTE mental health.
Although the field of traumatic stress has made great strides in examining risk and protective factors related to post-PTE functioning, there is a need for large-scale studies employing comprehensive assessment batteries within diverse populations at increased risk for trauma exposure. College students represent one such population. Not only are students characterized as the age group at highest risk for PTE exposure (i.e., 16–25 year-olds; (Breslau, 2009), but they are also at greatest risk for interpersonal PTE exposure (Breslau et al., 2008). Due to elevated risk of onset of many psychiatric disorders associated with emerging adulthood, the transition to college represents a discrete, high-risk developmental period suitable for the investigation of PTE. Therefore, there is a need to examine a wide range of potential risk and protective factors in order to determine the potential unique effects of each variable, as they are likely correlated. Prior studies have often looked at a limited number of potential risk/protective factors, and thus, the inclusion of variables within multiple domains in simultaneous models could provide the opportunity to determine if these variables afford independent associations with PTE exposure and mental health phenotypes. Conversely, it could also aid in determining if the prior associations reported in the literature were better accounted for by shared variance with other correlated risk/protective factors (unmeasured in prior studies). Thus, examining a multitude of variables across domains simultaneously could aid in identifying the relative importance of each variable. Moreover, although independent study of many of these variables among college populations has occurred (Anders et al., 2012; Read et al., 2011), research in this area could be further extended via concurrent examination across multiple risk and protective domains in a diverse, large sample. Additionally, a differential relationship may exist between these factors when PTEs and mental health are considered outcomes. Therefore, it is necessary to parse out the relationships between these theoretically relevant variables and PTE exposure and mental health outcomes independently in an effort to obtain a more thorough understanding of factors that contribute to each phenotype.
The present study uses data from the Spit for Science study (S4S), an ongoing university-wide research project located in the southeast United States, which assesses genetic and environmental influences on substance use and psychiatric disorders in a representative majority of incoming freshman at a large urban university. The first aim of the present study examines the prevalence of PTEs overall and by sex among incoming freshmen from the first three cohorts of S4S (N=6120) to determine if sex-specific patterns of PTE exposure found in general community samples are replicated in this college sample. Based on extant literature, we hypothesized that males would endorse higher rates of PTE exposure. The second aim of the study examines the association between demographic characteristics (i.e., sex, race), early environmental factors (i.e., neuroticism, parental relationship, peer deviance), and risk of PTE exposure. In line with existing literature, it was hypothesized that peer deviance, neuroticism, and poor perceived parental relationship would be positively correlated with risk of PTE exposure. The third aim of the study examines the relationships between PTE characteristics (i.e., cumulative load across interpersonal and accidental PTE types), early environmental factors, and resilience (i.e., perceived social support and perceived resilience) with regard to mental health phenotypes (i.e., trauma related distress, anxiety symptoms, depression symptoms, and alcohol use quantity and frequency). We hypothesized that greater interpersonal (compared to accidental) PTE load would be positively related to alcohol use (quantity and frequency), trauma related distress, anxiety, and depression symptoms, while greater perceived social support and resilience would be associated with decreased symptom endorsement.
2. Methods
2.1. Participants
The present study includes baseline (i.e., freshman year) data from the first three cohorts of S4S (N=6120). From 2011 to 2013, all incoming freshman aged≥18 years were invited to participate in a university-wide research study on college behavioral health. Invitations were sent to 11,328 individuals, with a 67% response rate. Approximately 2 weeks before arrival on campus, information was mailed to all incoming freshmen and (separately) their parents. The week before Welcome Week all eligible freshmen (age 18 or older) received an e-mail through their university e-mail account inviting them to participate in the project. Participants were representative of the broader student population attending Virginia Commonwealth University (VCU), in terms of both gender and race/ethnicity. The VCU Institutional Review Board (IRB) approved all study procedures and informed consent was obtained from all study participants. Study data were collected and managed using REDCap (Research Electronic Data Capture), hosted at VCU (Harris et al., 2009). REDCap is a secure, web-based application designed to support data capture for research studies, providing 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to statistical packages; and 4) procedures for importing data from external sources. Participants completed an online survey during the fall of their freshman year in REDCap assessing a variety of factors including childhood experiences, personality, relationships, and behavior, receiving $10 and a t-shirt as compensation. Detailed information concerning recruitment can be found in (Dick et al., 2014).
Given the large-scale nature of the S4S study, measures were necessarily abbreviated to reduce participant burden. Modifications occurred based on previous administrations of the S4S survey following examination of the results from the item response model fitting. Items were dropped due to redundancy and retained based on providing discrimination along the range of the latent factor scale.
2.2. Sample characteristics
During the years of 2011–2013, 6120 freshman attending VCU (Mage=18.42, SD=0.47; 61.6% female) participated in the S4S study. Race was dummy-coded and separated into three categories with Caucasian (51.5%) set as the reference group. Of the participants, 19.0% were African American, 16.0% were Asian, and 13.5% were grouped into the ‘Other’ category, including American Indian/Native Alaskan, Hispanic/Latino, Native Hawaiian/Other Pacific Islander, more than one race, and unknown.
2.3. Measures
2.3.1. PTE exposure
PTE exposure was assessed using an abbreviated version of the Life Events Checklist (Gray et al., 2004). Participants were asked to report on the occurrence of five different stressful events: natural disasters, physical assaults, sexual assaults, other unwanted or uncomfortable sexual experiences, and transportation accidents. Response options were “yes” or “no” to items regarding whether each stressful event occurred “before the past 12 months”, “during the past 12 months”, or “never happened to me”. If a participant endorsed that the event occurred either “before the past 12 months”, or “during the past 12 months”, it was considered a positive endorsement of PTE exposure prior to college. If a participant did not endorse any of the aforementioned option or reported that the events “never happened to me”, it was considered a negative endorsement of PTE history. Items were also summed to yield a ‘cumulative PTE’ score that encompassed number of lifetime PTE categories occurring prior to college entrance. Categories were further clustered by interpersonal (i.e., physical assaults, sexual assaults, other unwanted or uncomfortable sexual experiences) and non-interpersonal/accidental (i.e., natural disasters and transportation accidents) PTEs. An item assessing serious illness or injury was additionally included from a separate measure utilized in the assessment battery. The item was derived from an instrument developed by Kendler and colleagues (1999), which assesses a number of stressful events that may have occurred within an individual’s lifetime (e.g., broken engagement, housing difficulties), as a similar item exists in the full Life Events Checklist (Gray et al., 2004).
2.3.2. Family relations
The Parenting Styles Inventory (Steinberg et al., 1992) was used to examine family relations and consists of two subscales, parental involvement and autonomy granting. Questions are asked in reference to the parent(s)/guardian(s) the participant lived with throughout childhood. Items were scored on a Likert-type scale, ranging from 1 (strongly agree) to 4 (strongly disagree). The parental involvement subscale consists of three items (α=0.71) regarding the degree of parental involvement in the child’s life (e.g., “My parents knew who my friends were”). Items were reverse scored and summed such that higher scores indicated greater parental involvement. Autonomy granting was assessed with three items (α=0.60) that asked about freedom granted by parents throughout childhood (e.g., “My parents told me that their ideas were correct and that I should not question them”). Items were summed such that higher scores indicated greater autonomy granted by parents.
2.3.3. Peer deviance
Peer deviance was measured by six items previously created to assess conduct disorder and peer deviance (Kendler et al., 2008). Items asked how many friends the participant regularly interacted with exhibited potentially deviant behaviors within the past year (e.g., smoked cigarettes, been in trouble with the law). Responses were scored on a 5-point Likert-type scale from 0 (None) to 4 (All) with higher scores indicating higher levels of deviance among peers. The scale showed high reliability in this sample (α=0.94). Items were summed such that higher scores indicated greater levels of peer deviance.
2.3.4. Personality
A modified version of the Big Five Inventory (John and Srivastava, 1999) measured personality characteristics. The scale includes five 3-item sub-scales consisting of Extraversion (α=0.85), Agreeableness (α=0.71), Conscientiousness (α=0.80), Neuroticism (α=0.80), and Openness (α=0.71). Responses were scored on a 5-point Likert-type scale from 1 (disagree Strongly) to 5 (agree strongly). Although existing literature suggests a relationship between neuroticism and PTE exposure, the other subscales were also analyzed to determine if auxiliary relationships were present. Items within each subscale were summed such that higher scores indicated greater autonomy levels of each personality factor.
2.3.5. Social support
Social support was evaluated via three items from the modified version of the Medical Outcomes Study module (Sherbourne and Stewart, 1991). “Someone available to give good advice about a crisis”. Responses were made on a Likert-type scale of 0 (none of the time) to 3 (all of the time) and summed (α=0.74), with higher scores representing greater perceived social support. Items were summed such that higher scores indicated greater social support.
2.3.6. Resilience
Two items from the Connor-Davidson Resilience Scale (CD-RISC; (Connor and Davidson, 2003) assessed resilience (e.g., “I am able to adapt to change” I tend to bounce back after illness and hardship). Responses were made on a Likert-type scale of 0 (not true at all) to 4 (true nearly all the time) and summed (α=0.67), with higher scores indicating higher levels of resilience.
2.3.7. Trauma related distress
If a participant endorsed a PTE on the Life Events Checklist (Gray et al., 2004) or the single item derived from stressful events measure (Kendler et al., 1999a, 1999b), they were to respond to a PTSD screener item. The PTSD screener item was derived from the Primary Care PTSD Screen (PC-PTSD), previously used in screening PTSD symptoms in primary care settings (Prins et al., 2003). The item asks whether the participant experienced nightmares, attempts to avoid thoughts or reminders of the potentially traumatic experience, hyper-vigilance, and feelings of detachment. Endorsement of this item was used as indication of a positive lifetime history of trauma related distress.
2.3.8. Alcohol use
At each assessment, two items measured current alcohol use: average alcohol use frequency and quantity during the past 30 days. Alcohol use frequency was assessed via a single item “During the past 30 days, on how many days did you drink one or more drinks of an alcoholic beverage? “ and alcohol use quantity was assessed by the item “On the days that you drank during the past 30 days, how many drinks did you usually have each day? “ Continuous scores were created and the frequency (range=0–30) and quantity (range=0–21 [more than 21 drinks]) variable were used in the present analyses.
2.3.9. Depression and anxiety
The Symptom Checklist-90 Short Version (Hardt and Gerbershagen, 2001) is a 27-item instrument designed to measure mental health status. The SCL was used in the current study to assess depression (four items; α=0.84) and anxiety (four items; α=0.88) over the past month. Responses were made on a Likert-type scale of 1 (not at all) to 5 (extremely). Items within each subscale were summed such that higher scores indicated greater symptoms.
2.4. Analyses
Under Aim 1, descriptive statistics determined the prevalence of each form of PTE within the whole sample and by sex. Under Aim 2, three logistic regression analyses determined correlates of the three PTE exposure variables (i.e., any PTE exposure, any interpersonal PTE exposure, and any accidental PTE) using predictor variables in three theoretically derived areas (i.e., sex, race, personality, and early environment) entered in one level. Under Aim 3, a series of regression analyses identified variables within each predictor set (e.g., demographics, early environment, personality, interpersonal and accidental PTE load, trauma related distress, resilience) with regard to psychiatric phenotypes. Statistical significance was defined as p < 0.05. All analyses were conducted in SPSS (Version 21).
3. Results
3.1. Aim 1: prevalence of PTEs by sex
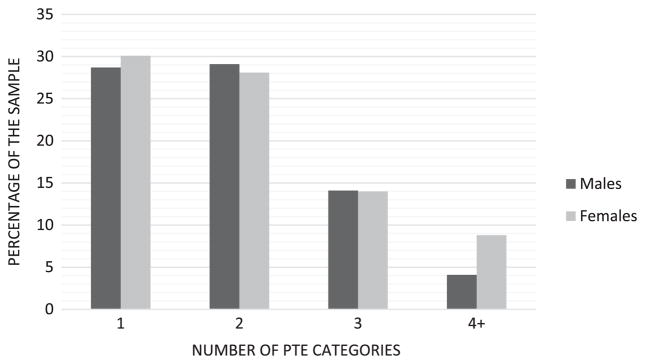
81.8% (n=4897) of individuals participating in the study reported experiencing at least one PTE event within their lifetime. Of the full sample, 39% (n=2295) of participants reported experiencing any interpersonal PTE, while 76.6% (n=4595) endorsed lifetime exposure to any accidental PTE. Males endorsed significantly higher rates of physical assault than females, and females reported significantly higher rates of any PTE, any interpersonal PTE, sexual assault, and other unwanted sexual experiences compared to males. Men and women did not significantly differ on endorsement of any accidental PTE (Table 1). Furthermore, the cumulative PTE load reported by females within the sample (M=1.66, SD=1.25) was significantly greater than that reported by males (M=1.47, SD=1.15) (t(5,5594)=−5.74, p < 0.001). 8.7% of the overall sample endorsed four or more PTEs prior to college (Fig. 1).
Table 1.
Lifetime prevalence of exposure to potentially traumatic events by sex.
| Males n=2247 | Females n=3751 | χ2 | Total N=6120 | ||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| % | SE | % | SE | % | SE | ||
| Any PTE | 79.1 | 0.009 | 83.5 | 0.006 | 18.61*** | 81.8 | 0.005 |
| Any Interpersonal PTE | 35.4 | 0.010 | 41.2 | 0.008 | 19.30*** | 39.0 | 0.006 |
| Physical assault | 29.8 | 0.010 | 21.8 | 0.007 | 47.17*** | 24.9 | 0.006 |
| Sexual assault | 4.3 | 0.004 | 11.7 | 0.005 | 94.17*** | 8.9 | 0.004 |
| Other unwanted sexual experience | 11.1 | 0.007 | 28.9 | 0.008 | 253.89*** | 22.2 | 0.005 |
| Any accidental PTE | 75.6 | 0.009 | 77.2 | 0.007 | 2.14 | 76.6 | 0.005 |
| Natural disaster | 62.6 | 0.011 | 64.3 | 0.008 | 1.92 | 63.7 | 0.006 |
| Transportation accident | 43.0 | 0.010 | 43.1 | 0.008 | 0.008 | 43.2 | 0.006 |
Note
p < 0.05,
p < 0.01.
p < 0.001.
Fig. 1.
Cumulative PTE exposure categories by sex (N=6120).
3.2. Aim 2: factors contributing to increased risk of PTE exposure
Likelihood of lifetime experience of any PTE, regardless of type, was higher among women than men (OR=1.32, p < 0.01), as was risk for interpersonal PTE exposure (OR=1.31, p < 0.001; Table 2). Individuals who endorsed Asian race/ethnicity were at lower risk of experiencing any, accidental, and interpersonal PTE (ORs=0.78–0.79, ps < 0.05) compared to Caucasians. Higher levels of neuroticism were associated with increased risk of any PTE (OR=1.03, p < 0.05) and interpersonal PTE exposure (OR=1.06, p < 0.001). Higher levels of the personality factor openness (OR=1.08, p < 0.001) was associated with increased risk of exposure to interpersonal PTE, while higher levels of conscientiousness were associated with decreased risk of interpersonal PTE (OR=0.94, p < 0.001). Higher levels of extraversion were related to a significantly increased risk of accidental PTE (OR=1.03, p < 0.01). Higher parental involvement was related to decreased risk of exposure to any PTE (OR=0.93, p < 0.01) and interpersonal PTE (OR=0.88, p < 0.001) while higher levels of parental autonomy were associated with decreased risk of interpersonal PTE (ORs=0.90, ps < 0.001). Peer deviance significantly increased risk of any PTE (OR=1.04, p < 0.001), accidental (OR=1.02, p < 0.05) and interpersonal PTE exposure (OR=1.07, p < 0.001).
Table 2.
Demographic, personality, and environmental predictors of PTE categories.
| Any (n=5296) | Accidental (n=5313) | Interpersonal (n=5234) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| OR | 95% C.I. | OR | 95% C.I. | OR | 95% C.I. | |
| Demographics | ||||||
| Female (vs. male) | 1.32** | 1.13–1.55 | 1.05 | 0.91–1.22 | 1.31*** | 1.15–1.50 |
| African American (vs. Caucasian) | 0.92 | 0.76–1.12 | 0.89 | 0.74–1.06 | 1.15 | 0.98–1.35 |
| Asian (vs. Caucasian) | 0.79* | 0.64–0.97 | 0.78* | 0.65–0.94 | 0.78* | 0.65–0.94 |
| Other (vs. Caucasian) | 1.07 | 0.86–1.35 | 1.03 | 0.84–1.26 | 1.11 | 0.93–1.32 |
| Personality | ||||||
| Neuroticism | 1.03* | 1.00–1.06 | 1.02 | 1.00–1.05 | 1.06*** | 1.04–1.09 |
| Agreeableness | 1.00 | 0.97–1.04 | 1.01 | 0.97–1.04 | 0.99 | 0.96–1.01 |
| Extraversion | 1.02 | 1.00–1.05 | 1.03** | 1.01–1.06 | 1.02 | 1.00–1.04 |
| Conscientiousness | 1.00 | 0.96–1.04 | 1.01 | 0.98–1.05 | 0.94*** | 0.91–0.97 |
| Openness | 1.02 | 0.99–1.05 | 1.00 | 0.97–1.03 | 1.08*** | 1.04–1.11 |
| Early Environment | ||||||
| Parental Involvement | 0.93* | 0.88–0.99 | 0.99 | 0.94–1.04 | 0.88*** | 0.84–0.92 |
| Parental Autonomy | 0.97 | 0.94–1.00 | 0.98 | 0.95–1.01 | 0.90*** | 0.87–0.92 |
| Peer Deviance | 1.04*** | 1.03–1.06 | 1.02* | 1.01–1.03 | 1.07*** | 1.06–1.09 |
Analyses for any, accidental, and interpersonal trauma types were run among all participants in the study.
p < 0.05.
p < 0.01.
p < 0.001.
3.3. Aim 3: relationship between PTEs and mental health phenotypes
3.3.1. Trauma related distress
Among those exposed to any form of PTE (n=4897), the prevalence of trauma related distress was 35.8%, with the prevalence higher among those exposed to interpersonal PTE (55.8%) versus accidental PTE (17.5%).1 When the regression analyses were conducted with trauma related distress as the outcome, females were significantly more likely to report trauma related distress (OR=1.76, p < 0.001) (Table 3). Asian race (vs. Caucasian) was associated with lower risk for trauma related distress (OR=0.60, p < 0.001). Higher levels of neuroticism were associated with increased risk of trauma related distress (OR=1.11, p < 0.001). Cumulative counts of exposure to interpersonal and accidental PTE categories were also associated with trauma related distress (ORs=3.27, 1.44, ps < 0.001, respectively); the odds ratio for interpersonal PTEs was significantly greater than that for accidental PTEs (z=10.46, p < 0.01). Conversely, high levels of social support were associated with lower risk of trauma related distress (OR=0.93, p < 0.001).
Table 3.
Regression analyses predicting probable PTSD, alcohol quantity, alcohol frequency, and global scale index score.
| Trauma Related Distress (n=3,856) | Alcohol Frequency (n=4,534) | Alcohol Quantity (n=4,458) | Global Scale Index – Depression (n=4,733) | Global Scale Index – Anxiety (n=4,734) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||||||
| OR | 95% C.I | β | B | B 95% C.I | β | B | 95% C.I. | β | B | 95% C.I. | β | B | 95% C.I | |
| Demographics | ||||||||||||||
| Female (vs. Male) | 1.76*** | 1.47–2.10 | −0.02 | −0.14 | −0.40 to 0.12 | −0.09*** | −0.55 | −0.72 to −0.37 | 0.02 | 0.14 | −0.04–0.33 | 0.04*** | 0.23 | 0.06–0.40 |
| African American (vs. Caucasian) | 0.97 | 0.78–1.20 | −0.08*** | −0.99 | −1.31 to −0.68 | −0.07*** | −0.57 | −0.79 to −0.35 | 0.03 | 0.23 | 0.003–0.45 | −0.04*** | −0.33 | −0.53 to −0.13 |
| Asian (vs. Caucasian) | 0.60*** | 0.47–0.77 | –0.05 | −0.61 | −0.96 to 0.26 | −0.04** | −0.36 | −0.60–0−0.12 | 0.01* | 0.08 | −0.17–0.33 | 0.002 | 0.02 | −0.21 to 0.24 |
| Other (vs. Caucasian) | 0.96 | 0.78–1.20 | −0.04 | −0.55 | −0.90 to 0.20 | −0.03* | −0.30 | −0.54 to −0.06 | 0.01 | 0.09 | −0.16–0.34 | −0.02 | −0.13 | −0.35 to 0.09 |
| Personality | ||||||||||||||
| Neuroticism | 1.11*** | 1.07–1.14 | −0.02 | −0.03 | −0.08 to 0.02 | −0.03 | 0–0.03 | −0.06 to 0.01 | 0.41*** | 0.50 | 0.47–0.53 | 0.32*** | 0.32 | 0.29–0.35 |
| Agreeableness | 1.01 | 0.98–1.05 | −0.05* | −0.10 | −0.16 to −0.04 | −0.05** | −0.06 | −0.10 to −0.02 | −0.003 | −0.004 | −0.04–0.04 | −0.01 | −0.02 | −0.06 to 0.02 |
| Extraversion | 1.00 | 0.97–1.03 | 0.12*** | 0.18 | 0.14–0.22 | 0.14*** | 0.14 | 0.11–0.17 | −0.12*** | −0.15 | −0.18 to −0.12 | −0.10*** | −0.10 | −0.13 to −0.08 |
| Conscientiousness | 1.02 | 0.97–1.06 | −0.04* | −0.11 | −0.18 to −0.04 | −0.01 | −0.02 | −0.07 to 0.03 | −0.03* | −0.05 | −0.10 to −0.003 | 0.000 | 0.000 | −0.04 to 0.04 |
| Openness | 1.03 | 0.99–1.07 | −0.01 | −0.01 | −0.07 to 0.04 | −0.04** | −0.06 | −0.10 to −0.02 | 0.07*** | 0.12 | 0.08–0.16 | 0.09*** | 0.13 | 0.10–0.17 |
| Early Environment | ||||||||||||||
| Parental Involvement | 0.99 | 0.93–1.05 | 0.02 | 0.08 | −0.01 to 0.17 | 0.03 | 0.06 | 0.002–0.13 | −0.02 | −0.06 | −0.12–0.01 | −0.02 | −0.04 | −0.10 to −0.02 |
| Parental Autonomy | 0.97 | 0.93–1.00 | −0.01 | −0.02 | −0.08 to 0.03 | −0.02 | −0.03 | −0.07 to 0.004 | −0.06*** | −0.10 | −0.14 to −0.06 | −0.05** | −0.06 | −0.10 to −0.03 |
| Peer deviance | 1.01 | 1.00–1.03 | 0.43*** | 0.38 | 0.36–0.41 | 0.39*** | 0.23 | 0.21–0.25 | 0.13*** | 0.09 | 0.08–0.11 | 0.08*** | 0.05 | 0.03–0.06 |
| PTE Type Load/trauma related distress | ||||||||||||||
| Accidental | 1.44*** | 1.30–1.61 | −0.01 | −0.07 | −0.21 to 0.07 | −0.01 | −0.02 | −0.12 to 0.08 | 0.01 | 0.30 | −0.05–0.15 | −0.002 | −0.01 | −0.10 to 0.08 |
| Interpersonal | 3.27*** | 2.94–3.64 | 0.03 | 0.14 | −0.01to 0.33 | 0.03* | 0.12 | 0.01–0.24 | 0.07*** | 0.05 | 0.18–0.42 | 0.07*** | 0.26 | 0.15–0.37 |
| Trauma related distress | – | – | −0.01 | −0.08 | −0.38–0.23 | −0.03 | −0.19 | −0.40 to 0.01 | 0.08*** | 0.62 | 0.40–0.83 | 0.11*** | 0.72 | 0.53–0.91 |
| Resilience | ||||||||||||||
| Social Support | 0.93*** | 0.89–0.96 | 0.04 | 0.08 | −0.02–0.14 | 0.04* | 0.05 | −0.02–0.09 | −0.15*** | −0.24 | −0.28 to −0.20 | −0.08*** | −0.11 | −0.45 to −0.07 |
| Resilience | 1.00 | 0.94–1.06 | −0.002 | −0.005 | −0.17 to 0.10 | −0.01 | −0.01 | −0.07 to 0.05 | −0.09*** | −0.21 | −0.27 to −0.15 | −0.10*** | −0.21 | −0.26 to −0.15 |
Trauma related distress model run among those endorsing any PTE.
p < 0.05.
p < 0.01.
p < 0.001.
3.3.2. Alcohol use
African American race was associated with significantly lower alcohol use frequency in the past 30 days (β=−0.08, p < 0.001; Table 3). Conscientiousness and agreeableness were both associated with lower alcohol frequency (βs=−0.04, −0.05, ps < 0.05, respectively) while extraversion was associated with higher alcohol frequency (β=0.12, p < 0.001). Greater peer deviance was positively related to higher rates of alcohol use frequency (β=0.43, p < 0.001). Female sex (β=−0.09, p < 0.001), Asian, African American, and Other race (βs=−0.07, −0.04, −0.03, ps < 0.05), agreeableness (β=−0.05, p < 0.05), and openness (β=−0.04, p < 0.001) were associated with lower alcohol quantity in the past 30 days. However, extraversion (β=0.14, p < 0.001), a history of peer deviance (β=0.39, p < 0.001), interpersonal PTE type (β=0.03, p < 0.05), and social support (β=0.04, p < 0.05) were associated with higher alcohol quantity.
3.3.3. Depressive symptoms
Relative to Caucasians, Asian race was associated with greater symptoms of depression (β=0.01, p < 0.05). Higher levels of neuroticism and openness were associated with higher depression (βs=0.41, 0.07, ps < 0.001, respectively) while higher levels of extraversion and conscientiousness was associated with lower depression symptoms (βs=−0.12, −0.03, ps < 0.05). Greater parental autonomy was associated with lower levels of depression (β=−0.06, p < 0.001). Greater peer deviance was positively associated with higher symptoms of depression (β=0.13, p < 0.001). Interpersonal PTE type and trauma related distress were also associated with higher symptoms of depression (βs=0.07, 0.08, ps < 0.001, respectively). Additionally, social support (β=−0.15, p < 0.001) and resilience (β=−0.09, p < 0.001) were associated with lower levels of depression symptoms.
3.3.4. Anxiety symptoms
Female sex was associated with higher anxiety symptoms (β=0.04, p < 0.05), while African American race was associated with lower rates of anxiety symptoms (β=−0.04, p < 0.001). Greater levels of neuroticism and openness were associated with higher anxiety (βs=0.32, 0.09, ps < 0.001) while extraversion was associated with significantly less symptoms of anxiety (β=−0.10, p < 0.001). Greater parental autonomy was associated with lower anxiety (β=−0.05, p < 0.01). Greater peer deviance was positively related to higher rates of anxiety (β=0.08, p < 0.001). Interpersonal PTE load and trauma related distress were also associated with higher anxiety symptom endorsement (βs=0.07, 0.11, respectively, ps < 0.001). Lastly, higher ratings of social support and resilience were related to lower levels of anxiety symptoms (βs=−0.08, −0.10, respectively, ps < 0.001).
4. Discussion
The present study aimed to determine the prevalence and correlates of pre-college history of exposure to PTEs by sex, as well as to explore the relation between PTE exposure characteristics, early environmental factors, resilience, and mental health outcomes within a large, representative sample of incoming college freshman. This study represents one of the largest, most diverse, investigations of PTE and health outcomes among college students.
As hypothesized, the sample endorsed a high prevalence of PTE exposure. Interestingly, when looking at the likelihood of participants experiencing any of the PTE categories, women had a higher prevalence than men – a finding inconsistent with existing literature demonstrating higher rates of exposure among males (Breslau 2002; Tolin and Foa, 2006a). These discrepant findings may be associated with the types of traumas assessed. Certain traumas that are usually more prevalent among men were not assessed (e.g., military combat). Moreover, only five PTE types (i.e., physical assault, sexual assault, any other uncomfortable and or unwanted sexual experience, transportation accident, natural disaster) were assessed and given that two of the five were types historically more prevalent among women (i.e., sexual assault, any other unwanted and/or uncomfortable sexual experience (Tolin and Foa, 2006b)), these rates could be contributing to the higher prevalence of any PTEs among females relatives to males. Women were also at increased risk of trauma related distress following exposure to any PTE relative to men. Elevated rates of interpersonal PTEs and PTSD symptoms among women has been exhibited consistently within the trauma literature (Breslau et al., 1999, 2003; Kessler et al., 1995; Olff et al., 2007; Stein et al., 2000). Both PTE types were associated with increased risk. However, the risk of developing trauma related distress following interpersonal PTE was much higher, demonstrating that the effect sizes observed for interpersonal PTEs were significantly greater than those observed for accidental PTEs. Exposure to interpersonal PTE was also associated with increased quantity and frequency of alcohol use, anxiety, and depression symptoms.
Furthermore, 8.7% of the sample reported experiencing ≥4 PTE categories prior to college. This is of particular interest considering the young age of the present sample and previous research suggesting increased likelihood of re-victimization following PTE exposure (Elwood et al., 2011). Exposure to violence early in life significantly predicts not only negative mental health outcomes, but also further exposure to traumatic events (Blom et al., 2014). Given the relationship between exposure to interpersonal PTEs, heightened likelihood of re-victimization (Elwood et al., 2011), and negative mental health outcomes as evidenced by previous work (Pietrzak et al., 2011) and the present study, a history of trauma pre-college entry among many students raises clinical implications regarding university based prevention and multi-system intervention efforts. Increased awareness among administrators and individuals working directly with students regarding the prevalence of PTEs and potential negative mental health outcomes may serve as early identification of at-risk students. Consideration of trauma history, when students present with problematic alcohol use or other academic issues, could influence courses for intervention efforts. In addition, impact of interpersonal PTEs are of national priority with the White House Council on Women and Girls (2014) encouraging college campuses to take more active roles, “increasing obligations to prevent and respond to campus sexual assault”. The high rates of re-victimization among those exposed to PTEs more interpersonal in nature and the increased vulnerability of PTE exposure among college aged young adults underscores the importance of college based intervention programs that take into consideration a possible trauma history.
Several other factors were differentially associated with exposure to PTEs. Specifically, Asians were associated with reduced risk of interpersonal PTE, consistent with prior research (Roberts et al., 2011). Personality characteristics also demonstrated a relationship with PTE exposure, with greater degree of neuroticism and openness conferring increased risk to interpersonal PTE while high levels of extraversion were associated with accidental PTE exposure. The findings are somewhat consistent with the literature in that neuroticism is frequently linked with exposure (Breslau and Schultz, 2013; Cox et al., 2004; Lauterbach et al., 2005) while openness has been previously associated with decreased risk of PTSD symptomatology following exposure (Stevanovic et al., 2011), although research is limited regarding the personality construct and PTE exposure. Although additional research regarding the relationship between openness and interpersonal PTE exposure is warranted, it may be the willingness to engage in new activities that increases risk of experiencing an interpersonal event. Gil (2013) suggests that high levels of extraversion may be linked with increased likelihood of both PTE exposure and PTSD possibly due to an underlying tendency to partake in challenging situations. This relationship could also be a function of gene by environment correlation whereby genetic influences can impact exposure to certain environments and experiences (Dick et al., 2005).
Factors associated with early environment were relevant to both exposure and negative mental health outcomes. Although peer deviance consistently reflected increased risk of all PTE categories, parental involvement was only significantly related to decreased risk of any interpersonal PTE exposure. Level of peer deviance was a significant predictor of alcohol use while parental relationship was more relevant to internalizing symptoms (e.g., anxiety and depression symptoms). Previous research discusses the potential for early childhood adversity to negatively influence selection of peer groups and behavior (Ford, 2002). Moreover, a potential relationship between limited or problematic relationships in youth and PTE exposure has also been suggested (Greenwald, 2002).
Finally, the present study suggests that social support and self-reported resilience are associated with less symptoms of anxiety and depression, consistent with prior studies (Hourani et al., 2012; Liu et al., 2013; Pietrzak and Cook, 2013). This line of research suggests that increasing secure relationships (Tsai, et al., 2012), improving problem-solving skills (Reivich et al., 2013), strengthening levels of perceived social support and control, in addition to reducing psychosocial difficulties, (Pietrzak and Cook, 2013) may improve psychological resilience and reduce the likelihood of psychiatric symptom development. The findings underscore the need for an inclusive assessment battery to fully understand factors that are associated with both risk and resilience (Karstoft et al., 2013). Given the potentially modifiable nature of many of the implicated factors, a two-fold approach of preventative programs within this at-risk population should involve both reduction of risk and cultivation of factors affiliated with resiliency. However, as in any cross-sectional studies, causality cannot be inferred. Thus, future longitudinal studies should be conducted to determine the role of the identified correlates of PTE exposure and mental health phenotypes to best inform prevention and intervention programming.
Although the present paper adds to the literature by assessing prevalence of PTE and the relationship with mental health outcomes among a particularly at-risk population providing a baseline assessment to be utilized for future longitudinal analyses, it is not without limitations. A significant limitation lies within the cross-sectional design of the present study. Although the present analyses serve as a foundation for our future longitudinal analyses, the ability to identify causal relationships is constrained given that only baseline data is being utilized. A limited number of PTEs were assessed, and details of the traumatic events (e.g., such as life threat, age of experience, series versus singular trauma) were not included due to time constraints. Given that the time elapsed since the PTE is unknown, events that happened many years prior to the S4S assessment might have had an impact yet may be less evident at assessment. Moreover, the lack of assessment of certain PTE types may contribute to the gender differences observed within the present study; however, the items were selected based on relevance to the sample and effort required to reduce participant burden. For example, given that the base rate of combat exposure within this sample is relatively low, it was not included in the assessment. However, this marks a critical area that warrants additional investigation. It should also be noted that the PTE assessment included an option for the event occurring “in the past 12 months”, which overlaps with the first month of college. The results should be taken in light of this limitation. Although previous research has demonstrated a strong relationship between PTSD symptoms and alcohol use, the age of this sample may contribute to the absence of a significant relationship, as the participants are early in their drinking careers. Due to constraints created by attempting to assess multiple variables in one large battery, scales were necessarily shortened. Further, the single item used to assess trauma related stress was adapted from a four item PTSD screening measure which has been used successfully in primary care screening procedures (Prins et al., 2003), yet the single item utilized in the present study is likely not capable of assessing disorder symptoms in a thorough and individual manner. Moreover, it should also be noted that participants experiencing significant avoidance associated with PTSD symptoms may been less inclined to participate or respond to the items regarding PTEs and trauma related distress. Thus, the present study may not be capturing the most severe cases. Finally, multiple regressions were conducted and corrections for multiple testing were not applied given the exploratory nature of the present study. Future hypothesis driven research would benefit from corrections for multiple testing.
Despite these limitations, the present study provides insight into not only factors contributing to negative mental health outcomes but PTE exposure itself. This data will be utilized as baseline information for longitudinal studies examining the implications of PTE exposure on mental health outcomes, a relationship that is still not well understood (Weston, 2014). The data presented also has clinical implications. Given the significant need for preventative programs within this population, identification of factors potentially contributing to exposure and symptoms provides a means of determining those at higher risk. Additionally, the high rates of PTE endorsed and the relationship to alcohol use and psychopathology by this representative sample suggest that continued effort should be placed in assessing for PTE history when individuals, specifically young undergraduate adults, present with mental health difficulties.
Acknowledgments
Funding
We would like to thank the VCU students for making this study a success, as well as the many VCU faculty, students, and staff who contributed to the design and implementation of the project. Spit for Science: The VCU Student Survey is funded by NIAAA R37AA011408 (PI: KSK), with support for DMD through NIAAA K02AA018755. Additional support for the project was obtained through NIAAA P20AA107828, NCRR UL1RR031990, and Virginia Commonwealth University. These funding sources had no role in the analysis or interpretation of the data, writing of the manuscript, or the decision to submit the paper for publication. CO is currently supported by NIDA F31DA038912 and was previously supported by NIMH T32MH020030. AA is supported by Grants NAAA R01AA020179, NIAAA K02AA013239, BBRF 20066, R01MH101518, and P60MD002256.
Footnotes
Participants who endorsed any interpersonal PTE history were included in the “interpersonal PTE” group (even if they reported an accidental PTE as well), whereas those in the “accidental PTE” group reported only accidental PTEs.
Financial disclosures and/or conflicts of interest
The authors have nothing to disclose.
References
- Amstadter A, Aggen SH, Knudsen GP, Reichborn-Kjennerud T, Kendler K. Potentially traumatic event exposure, posttraumatic stress disorder, and Axis I and II comorbidity in a population-based study of Norwegian young adults. Soc Psychiatry Psychiatr Epidemiol. 2013;48(2):215–223. doi: 10.1007/s00127-012-0537-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anders SL, Frazier PA, Shallcross SL. Prevalence and effects of life event exposure among undergraduate and community college students. J Couns Psychol. 2012;59(3):449–457. doi: 10.1037/a0027753. [DOI] [PubMed] [Google Scholar]
- Bandelow B, Krause J, Wedekind D, Ruther E. Early traumatic life events, parental attitudes, family history, and birth risk factors in patients with borderline personality disorder and healthy control. Psychiatry Res. 2005;134(2):169–179. doi: 10.1016/j.psychres.2003.07.008. [DOI] [PubMed] [Google Scholar]
- Benight C, Bandura A. Social cognitive theory of posttraumatic recovery: the role of perceived self-efficacy. Behav Res Ther. 2004;42(10):1129–1148. doi: 10.1016/j.brat.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Benight C, Harper ML. Coping self-efficacy perceptions as a mediator between acute stress response and long-term distress following natural disasters. J Trauma Stress. 2002;15(3):177–186. doi: 10.1023/A:1015295025950. [DOI] [PubMed] [Google Scholar]
- Blom H, Hogberg U, Olofsson N, Danielsson I. Strong association between earlier abuse and revictimization in youth. BMC Public Health. 2014;14:715. doi: 10.1186/1471-2458-14-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA. Loss, trauma, and human resilience. Have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J Consult Clin Psychol. 2007;75(5):671–682. doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- Breslau N. Gender differences in trauma and posttraumatic stress disorder. J Gend Specif Med. 2002;5(1):34–40. [PubMed] [Google Scholar]
- Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abus. 2009;10(3):198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis G, Andreski P, Federman B, Anthony JC. Epidemiological Findings on Posttraumatic Stress Disorder and Co-morbid Disorders in The General Population, Adversity, Stress, and Psychopathology. University Press; Oxford, London: 1998a. pp. 319–328. [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Arch Gen Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler R, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit area survey of trauma. Arch Gen Psychiatry. 1998b;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: a prospective epidemiological study. Arch Gen Psychiatry. 2008;65(4):431–437. doi: 10.1001/archpsyc.65.4.431. [DOI] [PubMed] [Google Scholar]
- Breslau N, Schultz L. Neuroticism and post-traumatic stress disorder: a prospective investigation. Psychol Med. 2013;43(8):1697–1702. doi: 10.1017/S0033291712002632. [DOI] [PubMed] [Google Scholar]
- Cieslak R, Benight C, Schmidt N, Luszczynska A, Curtin E, Clark RA, Kissinger P. Predicting posttraumatic growth among Hurricane Katrina survivors living with HIV: the role of self-efficacy, social support, and PTSD symptoms. Anxiety Stress Coping: Int J. 2009;22(4) doi: 10.1080/10615800802403815. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: the connor-davidson resilience scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Cox BJ, MacPherson PS, Enns MW, McWilliams LA. Neuroticism and self-criticism associated with posttraumatic stress disorder in a nationally representative sample. Behav Res Ther. 2004;42(1):105–114. doi: 10.1016/s0005-7967(03)00105-0. [DOI] [PubMed] [Google Scholar]
- Dick DM, Nasim A, Edwards AC, Salvatore JE, Cho SB, Adkins A, Meyers J, Yan J, Cooke M, Clifford J, Goyal N, Halberstadt L, Ailstock K, Neale Z, Opalesky J, Hancock L, Donovan KK, Sun C, Riley B, Kendler K. Spit for science: launching a longitudinal study of genetic and environmental influences on substance use and emotional health at a large US university. Front Genet. 2014;5(47):1–12. doi: 10.3389/fgene.2014.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Viken RJ, Kaprio J, Pulkkinen L, Rose RJ. Understanding the covariation among childhood externalizing symptoms: genetic and environmental influences on conduct disorder, attention deficit hyperactivity disorder, and oppositional defiant disorder symptoms. J Abnorm Child Psychol. 2005;33:219–229. doi: 10.1007/s10802-005-1829-8. [DOI] [PubMed] [Google Scholar]
- Elwood LE, Smith DW, Resnick HS, Gudmundsdottir B, Amstadter AB, Hanson RF, Saunders BE, Kilpatrick DG. Predictors of rape: findings from the national survey of adolescents. J Trauma Stress. 2011;24(2):166–173. doi: 10.1002/jts.20624. [DOI] [PubMed] [Google Scholar]
- Elliott D, Menard S. Delinquent friends and delinquent behavior. Delinquency and crime: Current theories. 1996:28–67. [Google Scholar]
- Ford JD. Traumatic Victimization in Childhood and Persistent Problems With Oppositional-defiance 2002 [Google Scholar]
- Gil S. Risk factors for traumatic exposure and for Posttraumatic Stress Symptoms (PTSS) J Loss Trauma: Int Perspect Stress Coping 2013 [Google Scholar]
- Girls WHCoWa. Rape and Sexual Assault: A Renewed Call to Action. United States of America: 2014. p. 38. [Google Scholar]
- Gray M, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Greenwald R. The role of trauma in conduct disorder. J Aggress Maltreatm Trauma. 2002;6:5–23. [Google Scholar]
- Hardt J, Gerbershagen HU. Cross-validation of the SCL-27: a short psychometric screening instrument for chronic pain patients. Eur J Pain. 2001;5(2):187–197. doi: 10.1053/eujp.2001.0231. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hourani LL, Bender RH, Weimer B, Peeler R, Bradshaw M, Lane M, Larson G. Longitudinal study of resilience and mental health in marines leaving military service. J Affect Disord. 2012;139(2):154–165. doi: 10.1016/j.jad.2012.01.008. [DOI] [PubMed] [Google Scholar]
- Jaksic N, Brajkovic L, Ivezic E, Topic R, Jakovljevic M. The role of personality traits in posttraumatic stress disorder (PTSD) Psychiatr Danub. 2012;24(3):256–266. [PubMed] [Google Scholar]
- John OP, Srivastava S. The Big Five trait taxonomy: history, measurement, and theoretical perspectives. In: Pervin LA, John OP, editors. Handbook of Personality: Theory and Resesarch. 2. Guilford; New York: 1999. pp. 102–138. [Google Scholar]
- Karstoft K, Armour C, Elklit A, Solomon Z. Long-term trajectories of posttraumatic stress disorder in veterans: the role of social resources. J Clin Psychiatry. 2013;74(12):1163–1168. doi: 10.4088/JCP.13m08428. [DOI] [PubMed] [Google Scholar]
- Kaysen D, Rosen G, Bowman M, Resick PA. Duration of exposure and the dose-response model of PTSD. J Interpers Violence. 2010;25(1):63–74. doi: 10.1177/0886260508329131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Personality and the experience of enviornmental adversity. Psychol Med. 2003;33(7):1193–1202. doi: 10.1017/s0033291703008298. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Jacobson K, Myers JM, Eaves LJ. A genetically informative developmental study of the relationship between conduct disorder and peer deviance in males. Psychol Med. 2008;38(7):1001–1011. doi: 10.1017/S0033291707001821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Sullivan P, Corey LA, Gardner CO, Prescott CA. A polulation – based twin study in women of smoking initiation and nicotine dependence. Psychol Med. 1999a;29:299–308. doi: 10.1017/s0033291798008022. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA. A population-based twin study of lifetime major depression in men and women. Arch Gen Psychiatry. 1999b;56:39–44. doi: 10.1001/archpsyc.56.1.39. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demier O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kibler JL, Lyons JA. Perceived coping ability mediates the relationship between PTSD severity and heart rate recovery in veterans. J Trauma Stress. 2004;17(1):23–29. doi: 10.1023/B:JOTS.0000014672.16935.9c. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the national survey of adolescents. J Consult Clin Psychol. 2003;71(4):692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- Lauterbach D, Vora R, Rakow M. The relationship between posttraumatic stress disorder and self-reported health problems. Psychosom Med. 2005;67(6):939–947. doi: 10.1097/01.psy.0000188572.91553.a5. [DOI] [PubMed] [Google Scholar]
- Lima AR, Mello MF, Andreoli S, Fossaluza V, de Araujo CM, Jackowski AP, Bressan RA, Mari JJ. The impact of healthy parenting as a protective factor for posttraumatic stress disorder in adulthood: a case-control study. PLoS One. 2014 doi: 10.1371/journal.pone.0087117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Pang R, Sun W, Wu M, Qu P, Lu C, Wang L. Functional social support, psychological capital, and depressive and anxiety symptoms among people living with HIV/AIDS employed full-time. BMC Psychiatry. 2013;13(324) doi: 10.1186/1471-244X-13-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer EC, Zimering R, Daly E, Knight J, Kamholz BW, Gulliver SB. Predictors of posttraumatic stress disorder and other psychological symptoms in trauma-exposed firefighters. Psychol Serv. 2012;9(1):1–15. doi: 10.1037/a0026414. [DOI] [PubMed] [Google Scholar]
- Mollica RF, McInnes K, Pham T, Smith Fawzi MC, Murphy E. The dose-effect relationships between torture and psychiatric symptoms in Vietnamese ex-political detainees and a comparison group. J Nerv Ment Dis. 1998;186(9):543–553. doi: 10.1097/00005053-199809000-00005. [DOI] [PubMed] [Google Scholar]
- Morrongiello BA, Corbett M, McCourt M, Johnston N. Understanding unintentional injury risk in young children II. The contribution of caregiver supervision, child attributes, and parent attributes. J Pediatr Psychol. 2006;31(6):540–551. doi: 10.1093/jpepsy/jsj073. [DOI] [PubMed] [Google Scholar]
- Nishith P, Mechanic MB, Resick PA. Prior interpersonal trauma: the contribution to current PTSD symptoms in female rape victims. J Abnorm Psychol. 2000;109(1):20–25. [PMC free article] [PubMed] [Google Scholar]
- Olff M, Langeland W, Draijer N, Gersons BPR. Gender differences in posttraumatic stress disorder. Psychol Bull. 2007;133:183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Perrin MA, Vandeleur CL, Castelao E, Rothen S, Glaus J, Vollenweider P, Preisig M. Determinants of the development of posttraumatic stress disorder, in the general population. Soc Psychiatry Psychiatr Epidemiol. 2013;49(3):447–457. doi: 10.1007/s00127-013-0762-3. [DOI] [PubMed] [Google Scholar]
- Perrin MA, Vandeleur CL, Castelao E, Rothen S, Glaus J, Vollenweider P, Preisig M. Determinants of the development of post-traumatic stress disorder, in the general population. Soc Psychiatry Psychiatr Epidemiol. 2014;49(3):447–457. doi: 10.1007/s00127-013-0762-3. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Cook J. Psychological resilience in older U.S. veterans: results from the national health and resilience in veterans study. Depress Anxiety. 2013;30(5):432–443. doi: 10.1002/da.22083. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the national epidemiologic survey on alcohol and related conditions. J Anxiety Disord. 2011;25(3):456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Psychological resilience and postdeployment social support protect against traumatic stress and depressive symptoms in soldiers returning from operations enduring freedom and iraqi freedom. Depress Anxiety. 2009;26(8):745–751. doi: 10.1002/da.20558. [DOI] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RS, Hugleshofer D, Shaw-Hegwar J. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Prim Care Psychiatry. 2003;9:9–14. [Google Scholar]
- Punamaki R, Qouta S, El-Sarraj E. Resiliency factors predicting psychological adjustment after political violence among Palestinian children. Int J Behav Dev. 2001;25(3):256–267. [Google Scholar]
- Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand. 2005;112:330–350. doi: 10.1111/j.1600-0447.2005.00634.x. [DOI] [PubMed] [Google Scholar]
- Read JP, Ouimette P, White J, Colder C, Farrow S. Rates of DSM-IV-TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychol Trauma. 2011;3(2):148–156. doi: 10.1037/a0021260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reivich K, Gillham JE, Chaplin TM, Seligman ME. From helplessness to optimism: the role of resilience in treating and preventing depression in youth. In: Goldstein S, Brooks RB, editors. Handbook of Resilience in Children. Springer; US: 2013. pp. 201–214. [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41(1):71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubens SL, Vernberg EM, Felix ED, Canino G. Peer deviance, social support and symptoms of internalizing disorders among youth exposed to Hurricane Georges. Psychiatry: Interpers Biol Process. 2013;76(2):169–181. doi: 10.1521/psyc.2013.76.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer R, Warner LM, Schuez B, Tesch-Roemer C, Wurm S, Ziegelmann P. Effects of self-efficacy on subjective functioning, activity, and autonomy in multimorbid adults. Gerontologist. 2012;52:699–699. [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Shih RA, Schell TL, Hambarsoomian K, Belzberg H, Marshall GN. Prevalence of posttraumatic stress disorder and major depression after trauma center hospitalization. J Trauma. 2010;69(6):1560–1566. doi: 10.1097/TA.0b013e3181e59c05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MB, Walker JR, Forde DR. Gender differences in susceptibility to posttraumatic stress disorder. Behav Res Ther. 2000;38(6):619–628. doi: 10.1016/s0005-7967(99)00098-4. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Lamborn SD, Dornbusch SM, Darling N. Impact of parenting practices on adolescent achievement: authoritative parenting, school involvement, and encouragement to succeed. Child Dev. 1992;63(5):1266–1281. doi: 10.1111/j.1467-8624.1992.tb01694.x. [DOI] [PubMed] [Google Scholar]
- Stevanovic A, Franciskovic T, Colic M, Vidakovic I, Knezevic G, Vermetten E. Personality traits and PTSD after experiencing civilian war-related trauma among women in Croatia. Eur Psychiatry 2011 [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006a;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006b;132(6):959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Tsai J, Harpaz-Rotem I, Pietrzak RH, Southwick S. The role of coping, resilience, and social support in mediating the relation between PTSD and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry: Interpers Biol Process. 2012;75(2):135–149. doi: 10.1521/psyc.2012.75.2.135. [DOI] [PubMed] [Google Scholar]
- van Nierop M, Lataster T, Smeets F, Gunther N, van Zelst C, de Graaf R, ten Have M, van Dorsselaer S, Bak M, Myin-Germeys I, Veichtbauer W, van Os J, van Winkel R. Psychopathological mechanisms linking childhood traumatic experiences to psychotic symptoms: analysis of a large, representative population-based sample. Schizophr Bull. 2014;40(2):123–130. doi: 10.1093/schbul/sbt150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weston CS. Posttraumatic stress disorder: a theoretical model of the hyperarousal subtype. Front Psychiatry. 2014;5(37) doi: 10.3389/fpsyt.2014.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Barry CT, Drotar D, Wade SL, Stancin T. Neurobehavioral symptoms in childhood closed-head injuries: changes in prevalence and correlates during the first year postinjury. J Pediatr Psychol. 2001;26:79–91. doi: 10.1093/jpepsy/26.2.79. [DOI] [PubMed] [Google Scholar]