Abstract
Objectives. To quantify the increased disease burden caused by US health care sector life cycle greenhouse gas (GHG) emissions of 614 million metric tons of carbon dioxide equivalents in 2013.
Methods. We screened for health damage factors that linked GHG emissions to disease burdens. We selected 5 factors, based on appropriate temporal modeling scales, which reflect a range of possible GHG emissions scenarios. We applied these factors to health care sector emissions.
Results. We projected that annual GHG emissions associated with health care in the United States would cause 123 000 to 381 000 disability-adjusted life-years in future health damages, with malnutrition being the largest damage category.
Conclusions. Through their contribution to global climate change, GHG emissions will negatively affect public health because of an increased prevalence of extreme weather, flooding, vector-borne disease, and other effects. As the stewards of global health, it is important for health care professionals to recognize the magnitude of GHG emissions associated with health care itself, and the severity of associated health damages.
The central finding of The Lancet Commission on Health and Climate Change, that tackling climate change could be the greatest global health opportunity of the 21st century, resulted in several Commission recommendations to accelerate actions. These included the call for research to quantify disease burden and for health professional leadership to unite all actors behind the common cause of public health.1
The US health care system contributes significantly to country-wide air and water pollution, and hence, to pollution-related health damages.2 US health care activities were responsible for 9% to 10% of national greenhouse gas (GHG) emissions in 2013, which occurred both directly from health care facilities and vehicles, and in larger part, indirectly from upstream production of electricity, drugs, medical devices and supplies, and other goods and services that feed into the health care sector. Taken together, direct and indirect GHG emissions are called life cycle emissions or the carbon footprint of US health care. These life cycle emissions results update and corroborate earlier work by Chung and Meltzer.3
In addition to GHG emissions, health care–associated emissions of several other types of pollutants were also quantified,2 including those that contribute to acid rain (12% of the national total), photochemical smog (10%), and respiratory disease (9%). Public health damages from exposure to non-GHG emissions were subsequently estimated at 405 000 disability-adjusted life-years (DALYs) annually. Most of these DALYs were attributable to particulate matter emissions. These health damages are comparable in magnitude to preventable medical errors,2 but they are incurred indirectly by the general public rather than directly by patients. They are also partially preventable, because reducing wasted resources that do not benefit patient outcomes also reduces upstream emissions and their associated damages.4
We considered the possible range of health damages from health care–related GHG emissions specifically. These damages were not included in our earlier estimates of health care sector emission disease burden because of the wide variation in approaches used in their estimation―such as the socioeconomic and emission scenarios considered, inclusion or exclusion of particular health effects, potential adaptive responses, and modeling parameters―that can lead to order-of-magnitude differences in damage factors. Potential impacts of climate change on human health, well-being, and security have been characterized in detail and include thermal stress, flooding and extreme events, radiation, air pollution, infectious disease, malnutrition, and potential conflicts (bit.ly/1RIYUkC). The World Health Organization estimated that in 2004 climate change caused 141 000 additional deaths worldwide on an annual basis, with a projected 250 000 additional annual deaths that will occur from 2030 to 2050, considering the factors of heat stress, malaria, diarrhea, and malnutrition, and using an average GHG emissions scenario (bit.ly/1tGJ5RS). We linked these future global health damages to the portion of global GHG emissions of the US health care system.
METHODS
We utilized health damage factors (in units of DALYs or additional deaths per mass unit of GHG emission) derived for integrated assessment by Tang et al.5 and de Schryver et al.6 Both groups used a multistep approach to assess relative risks to public health caused by climate change. First, the authors linked GHG emissions scenarios to expected temperature changes in various regions, based on global climate model results assembled by the Intergovernmental Panel on Climate Change (IPCC) to the year 2100. Tang et al.5 considered the 4 major emissions scenarios used by the IPCC in their 2001 and 2007 assessment reports, namely the Special Report on Emissions Scenarios (SRES): A1B (balanced emphasis on all energy sources), A2 (regionally oriented economic development), B1 (global environmental sustainability), and B2 (local environmental sustainability); de Schryver et al.6 just considered the A1B scenario. These scenarios reflected distinct rates of population growth and economic growth, levels of international cooperation, and energy technology focus. The different GHGs (carbon dioxide, methane, nitrous oxide, sulfur hexafluoride, and certain hydrofluorocarbons and chlorofluorocarbons) were expressed in carbon dioxide equivalents (CO2e), which represent their ability to absorb and re-emit radiation back to the Earth’s surface over their lifetimes, relative to that of CO2.
The authors then projected temperature changes that would result from each emission scenario and multiplied them by region-specific relative risk factors for several temperature-dependent health effects. Risks included malaria, diarrhea, malnutrition, cardiovascular disease, coastal and inland flooding and subsequent landslides, based on estimates from Ezzati et al.7 for the period up to 2030.
Finally, the authors used the resulting relative risk effects from global warming to scale the baseline (no warming) burden of disease estimates for 2030 from Mathers and Loncar,8 and extended the burden of disease estimates out to 2100. The final health damage factors calculated by Tang et al.5 and de Schryver et al.6 ranged from 1.13 × 10−8 to 1.76 × 10−5 DALYs/kg CO2e emitted, depending on the socioeconomic and emissions scenarios considered, inclusion or exclusion of particular health effects, inclusion of potential adaptive responses, and the modeling parameters, such as the discount rate and the temperature change modeling time horizon (20 years, 100 years, or infinite).
We used only damage factors estimated with customary 100-year global warming potential values, which resulted in a range of 2.00 to 6.20 × 10−7 DALYs/kg CO2e. We calculated total GHG-related DALYs for the US health care sector by multiplying this range of health damage factors by earlier estimates of US health care GHG emissions for the year 2013 of 614 million tons CO2e, which was obtained using Economic Input-Output Life Cycle Assessment methods and US Government health expenditure data and economic tables.2
RESULTS
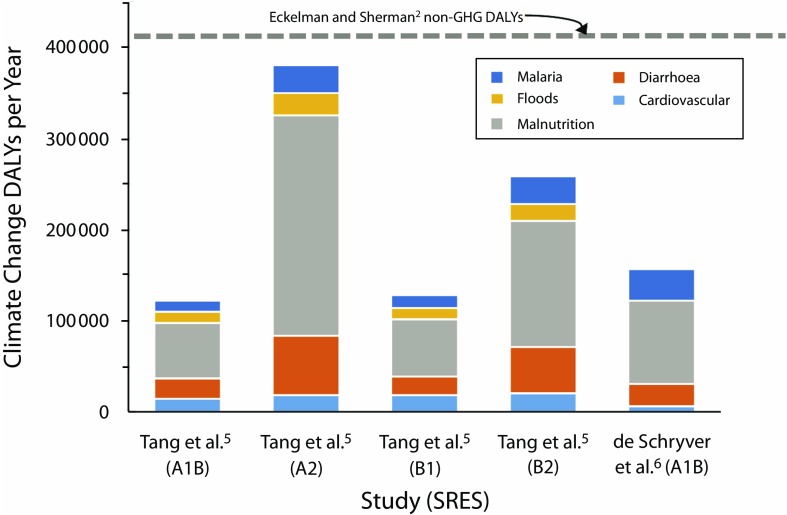
We estimated that life cycle GHG emissions associated with US health care activities will cause an additional 123 000 to 381 000 DALYs annually (Figure 1) based on 2013 health care sector life cycle emissions. We used the same proportions of disease contributions to total DALYs for each health damage factor reported in Tang et al.5 and de Schryver et al.6 In all cases, the largest potential health damages were attributable to malnutrition (49%–63% of the total), which will particularly affect regions with large populations and agricultural areas located on floodplains or lacking irrigation, including much of Africa and parts of South and Southeast Asia. Increased incidence of diarrhea and malaria are the other main contributors to total DALYs, because of lengthening warm seasons and expanding geographic ranges of disease vectors.
FIGURE 1—
Estimates for Disability-Adjusted Life-Years (DALYs) Caused by Greenhouse Gas (GHG) Emissions Associated With US Health Care in 2013
Note. A1B, A2, B1, and B2 denote the main Special Report Emissions Scenarios (SRES) used by the Intergovernmental Panel on Climate Change (IPCC) used in their Third (2001) and Fourth (2007) Assessment Reports. DALYs from health care sector life cycle emissions of pollution other than GHGs reported by Eckelman and Sherman2 are shown for comparison.
Adding the average estimate of 209 000 DALYs to the earlier figure reported by Eckelman and Sherman2 for non-GHG results increased US health care–related public health damages to a total of 614 000 DALYs per year for all emission types. Because actual global GHG emissions exceeded those predicted in the SRES scenarios for the early 21st century,9 the health damage factors we used may well underestimate actual health damages over the coming decades.
DISCUSSION
Health care–related pollution represents a notable portion of total US emissions for multiple pollutant classes.2 Using health damage factors to project the potential impacts of these emissions on public health helps to translate the sometimes abstract issues of climate change and environmental sustainability to metrics that are familiar to health care professionals. National health care sector emission disease burden could serve as a new global health metric,10 and development of methods for international comparisons are underway. Such efforts could engage health care leadership globally and be leveraged to increase climate change adaptation and mitigation as a public health priority as called for by The Lancet Commission.1 Furthermore, because health professionals interface with the public, their engagement could serve as a multiplier for an engaged citizenry armed with a greater awareness of the potential health impacts of climate change.
PUBLIC HEALTH IMPLICATIONS
Although non-GHG emissions have primarily local or regional impacts, the deleterious effects of GHG emissions will be global. Efforts to improve the carbon footprint of the US health care system will thus have worldwide environmental and health co-benefits,11 and should be included in efforts to improve health care quality and safety, following the “health in all policies” principle.12
ACKNOWLEDGMENTS
J. D. Sherman was supported by the Anesthesia Patient Safety Foundation 2015 to 2016 award.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed because no human participants were involved in this study.
Footnotes
See also Frumkin, p. S56.
REFERENCES
- 1.Watts N, Adger WN, Agnolucci P et al. Health and climate change: policy responses to protect public health. Lancet. 2015;386(10006):1861–1914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 2.Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PLoS One. 2016;11(6):e0157014. doi: 10.1371/journal.pone.0157014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung JW, Meltzer DO. Estimate of the carbon footprint of the US health care sector. JAMA. 2009;302(18):1970–1972. doi: 10.1001/jama.2009.1610. [DOI] [PubMed] [Google Scholar]
- 4.Brown LH, Buettner PG, Canyon DV. The energy burden and environmental impact of health services. Am J Public Health. 2012;102(12):e76–e82. doi: 10.2105/AJPH.2012.300776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang L, Ii R, Tokimatsu K, Itsubo N. Development of human health damage factors related to CO2 emissions by considering future socioeconomic scenarios. Int J Life Cycle Assess. 2015:1–12. [Google Scholar]
- 6.De Schryver AM, Brakkee KW, Goedkoop MJ, Huijbregts MA. Characterization factors for global warming in life cycle assessment based on damages to humans and ecosystems. Environ Sci Technol. 2009;43(6):1689–1695. doi: 10.1021/es800456m. [DOI] [PubMed] [Google Scholar]
- 7.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360(9343):1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 8.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raupach MR, Marland G, Ciais P et al. Global and regional drivers of accelerating CO2 emissions. Proc Natl Acad Sci U S A. 2007;104(24):10288–10293. doi: 10.1073/pnas.0700609104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frumkin H, Hess J, Luber G, Malilay J, McGeehin M. Climate change: the public health response. Am J Public Health. 2008;98(3):435–445. doi: 10.2105/AJPH.2007.119362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haines A, McMichael AJ, Smith KR et al. Public health benefits of strategies to reduce greenhouse-gas emissions: overview and implications for policy makers. Lancet. 2009;374(9707):2104–2114. doi: 10.1016/S0140-6736(09)61759-1. [DOI] [PubMed] [Google Scholar]
- 12.Moulton AD. Toward a national climate change health coalition. Am J Public Health. 2016;106(10):1763–1764. doi: 10.2105/AJPH.2016.303331. [DOI] [PMC free article] [PubMed] [Google Scholar]