Abstract
Background
Mental and substance use disorders are common and often persistent, with many emerging in early life. Compared to adult mental and substance use disorders, the global burden attributable to these disorders in children and youth has received relatively little attention.
Method
Data from the Global Burden of Disease Study 2010 was used to investigate the burden of mental and substance disorders in children and youth aged 0–24 years. Burden was estimated in terms of disability-adjusted life years (DALYs), derived from the sum of years lived with disability (YLDs) and years of life lost (YLLs).
Results
Globally, mental and substance use disorders are the leading cause of disability in children and youth, accounting for a quarter of all YLDs (54.2 million). In terms of DALYs, they ranked 6th with 55.5 million DALYs (5.7%) and rose to 5th when mortality burden of suicide was reattributed. While mental and substance use disorders were the leading cause of DALYs in high-income countries (HICs), they ranked 7th in low- and middle-income countries (LMICs) due to mortality attributable to infectious diseases.
Conclusions
Mental and substance use disorders are significant contributors to disease burden in children and youth across the globe. As reproductive health and the management of infectious diseases improves in LMICs, the proportion of disease burden in children and youth attributable to mental and substance use disorders will increase, necessitating a realignment of health services in these countries.
Keywords: Children and youth, disability-adjusted life years, global burden of disease, mental and substance use disorders
Introduction
Young people aged 0–24 years make up 44% of the world’s population (United Nations, 2011). While the global population continues to age, this is happening at a much slower pace in low- and middle income countries (LMICs). In these countries, children and youth make up 47% of the population compared to 30% in high-income countries (HICs). Most importantly, 91% of the world’s children and youth live in LMICs (United Nations, 2011). Given that the prominent youth bulge has the potential to drive future global economic prosperity, the health and well-being of young people is an asset for the individual and their broader communities (Sawyer et al. 2012).
Mental and substance use disorders are major contributors to health-related disability in children and youth (Gore et al. 2011; Sawyer et al. 2012; WHO, 2014). Half of all cases of mental disorders develop by age 14 years although most remain undetected and untreated until later in life (Patel et al. 2007; WHO, 2014). This is concerning given the immediate and long-term adverse consequences on an individual’s health and non-health outcomes. For example, a young person with conduct disorder is at increased risk of an array of negative consequences including poor educational achievement (Fergusson et al. 1993), increased risk of drug and alcohol use (Hopfer et al. 2013), unemployment, (Colman et al. 2009), and higher rates of criminality (Kjelsberg, 2002). In recent years, high prevalence of mental and substance use disorders have been consistently reported in national youth surveys conducted in a number of countries (Sawyer et al. 2001; Green et al. 2005; Ravens-Sieberer et al. 2008; Kessler et al. 2012). For example, the US National Comorbidity Survey Adolescent Supplement found the point prevalence of any DSM-IV disorder was 23.4% (Kessler et al. 2012). Prospective longitudinal studies have found that the majority of children and youth experience a mental and/or substance use disorder prior to reaching adulthood (Moffitt et al. 2010; Copeland et al. 2011). Investigating the global and country-level burden attributable to mental and substance use disorders in children and youth is important from both an epidemiological and global health policy standpoint, particularly given the large proportion of children and youth living in LMICs. This paper explores both the magnitude and patterns in the burden of mental and substance use disorders in young people aged 0–24 years while also identifying the limitations presented by the available epidemiological data and burden estimation methodology. Burden is investigated using data from the Global Burden of Disease Study 2010 (GBD 2010). GBD 2010 was one of the largest research undertakings in the health field, generating over 1 billion results for deaths, years of life lost due to premature mortality (YLLs), years lived with disability (YLDs) and disability-adjusted life years (DALYs), covering 291 causes for 187 countries aggregated into 21 regions, seven super-regions and the entire globe (Lim et al. 2012; Lozano et al. 2012; Murray et al. 2012; Salomon et al. 2012a, b; Vos et al. 2012; Wang et al. 2012). The main trends were clear: humans across the globe were living longer albeit sicker with disease burden shifting from communicable to non-communicable diseases in almost every region (Murray et al. 2012). As such, GBD 2010 provides a platform for comprehensively exploring of the global burden of mental and substance use disorders in children and youth.
Method
Given that ‘childhood’, ‘adolescence’, and ‘youth’ are ambiguous terms allocated to varying age ranges, we use the term ‘children and youth’ to describe young people aged from 0–24 years of age’. The methodology of GBD 2010 relating to mental and substance use disorders has been described comprehensively in previous publications (Lozano et al. 2012; Murray et al. 2012; Vos et al. 2012; Whiteford et al. 2013). Here, we give a brief explanation of the methodology utilized for each burden metric with a focus on considerations for the child and youth age group. A flowchart showing the GBD methodology step-by-step is available online (see Supplementary material).
Case definitions
Mental and substance disorders were defined according to the Diagnostic and Statistical Manual of Mental Disorders (DSM; APA, 2000) and the International Classification of Diseases (ICD; WHO, 1992). Inclusion required individual disorders to meet the threshold for a case according to at least one of these diagnostic criteria. Twenty disorders were included for burden quantification: major depressive disorder (MDD), dysthymia, anxiety disorders (as a single cause), bipolar disorder, schizophrenia, conduct disorder, attention-deficit/hyperactivity disorder (ADHD), autism, Asperger’s syndrome, anorexia nervosa, bulimia nervosa, idiopathic intellectual disability, cannabis dependence, cocaine dependence, amphetamine dependence, opioid dependence, other drug dependence (a residual category), alcohol dependence, fetal alcohol syndrome, and a residual category of other mental and substance use disorders. Idiopathic intellectual disability was the remaining component once all other intellectual disability had been re-attributed to specific causes (e.g. neonatal encephalopathy) in order to avoid double counting. Certain major disorder groups, e.g. personality disorders, were not included because of exceedingly sparse epidemiological data (Erskine et al. 2013). The burden of these disorder groups was therefore represented in either the ‘other mental and substance use disorder’ or ‘other drug use disorder’ residual categories.
Disability-adjusted life years (DALYs)
DALYs are the metric of overall burden utilized by GBD 2010, calculated by summing years lived with disability (YLDs) and years of life lost due to premature mortality (YLLs). As such, DALYs represent both non-fatal (YLDs) and fatal (YLLs) burden with 1 DALY equivalent to the loss of 1 year of healthy life.
Years lived with disability (YLDs)
YLDs are calculated by multiplying the number of prevalent cases by a disability weight. Systematic reviews were conducted for each mental and substance use disorder (with the exception of the residual categories and idiopathic intellectual disability) according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al. 2009). Electronic databases (PsycINFO, Medline, EMBASE) were searched while grey literature was also explored and experts were consulted for additional data sources. Studies were required to be representative of the general population, use DSM (APA, 2000) or ICD (WHO, 1992) criteria, and have been published since 1980. In order to maximize data inclusion, estimates derived from both DSM and ICD were included. To meet DSM or ICD criteria, a study needed to have used structured diagnostic instruments with validated crosswalks to DSM/ICD diagnoses. The initial literature search was conducted for the period 1980–2008 but manual checks of the literature were conducted in consultation with experts up until 2011. Estimates of prevalence, incidence, remission, duration, and excess mortality were extracted while details of study methodology were also recorded. Only point or past-year prevalence was accepted given demonstrated recall bias associated with lifetime estimates (Moffitt et al. 2010; Compton & Lopez, 2014; Takayanagi et al. 2014). For incidence, we used hazard rates with person-years of follow-up as the denominator. For mortality, standardized mortality ratios or relative risks were extracted while remission estimates required data on the proportion of cases fully remitted from a given disorder over a specified period of time. The methods and results of the systematic reviews for individual mental and substance use disorders have been published previously (Ferrari et al. 2011, 2013b; Baxter et al. 2013; Charlson et al. 2013; Degenhardt et al. 2013, 2014a, b; Erskine et al. 2013). The majority of available data were for prevalence, with data for other parameters (incidence, remission, mortality) generally only measured in HICs.
There was a lack of data for certain disorders and countries and, for some estimates, there were high levels of between-study variability caused by differing methodologies. In order to adjust for this variability and impute missing data, available epidemiological data for each disorder were entered into DisMod-MR. This Bayesian meta-regression tool utilizes a negative-binomial model of disease prevalence, incidence, remission, and case-fatality rates, and fits models using a randomized Markov-Chain Monte Carlo algorithm (Vos et al. 2012). DisMod-MR applies internal consistency between data points from different epidemiological parameters while study-level covariates are used to adjust for between-study heterogeneity. In order to predict epidemiological estimates for countries and/or parameters with no available raw data, the tool uses country-level covariates and random effects at the country, region, and super-region level. Furthermore, an advantage for inference is that DisMod-MR calculates 95% uncertainty around all estimations, propagated from the raw epidemiological estimates. Disorder-specific DisMod-MR modelling strategies and output have been published elsewhere (Charlson et al. 2013; Degenhardt et al. 2013, 2014a, b; Erskine et al. 2013; Ferrari et al. 2013a). For the purpose of GBD 2010, prevalent cases were estimated using DisMod-MR’s age-, sex-, year-, region- and country-specific prevalence output and United Nations corresponding population data (United Nations, 2011).
In order to calculate YLDs, disability weights were also required for each disorder and for health states within certain disorders (e.g. mild, moderate, severe MDD). New disability weights were developed for GBD 2010 through population surveys conducted in Bangladesh, Indonesia, Peru, Tanzania, and the USA (n = 13 902), and an open-access internet survey (n = 16 328) available in multiple languages. In both surveys, participants were presented with pairwise comparisons selected from the 220 health states and asked to rate which of the two they considered the more ‘unhealthy’. Health states were presented as lay vignettes which were required to use only simple, nonclinical language and restricted to 435 words in length. In order to derive disability weights, responses were fixed on a 0 (healthy) to 1 (death) scale, anchored using a selection of ‘population health equivalence’ questions comparing health benefits of different lifesaving or disease-prevention programs. Survey vignettes and their disability weights have been published elsewhere (Salomon et al. 2012a).
The disability weights for anxiety disorders, MDD, and the drug use disorders were adjusted to account for changes in severity within the course of the disorder. The severity proportions were derived from three adult health surveys: the 1997 Australian National Survey of Mental Health and Wellbeing in adults (NSMHW) (Australian Bureau of Statistics, 1997), the US National Epidemiological Survey on Alcohol and Related Conditions (NESARC) 2000–2001 and 2004–2005 (US National Institutes of Health National Institute on Alcohol Abuse and Alcoholism, 2006), and the US Medical Expenditure Panel Survey (MEPS) (Agency for Healthcare Research and Quality, 2009). No data for children or youth were used in these analyses. These proportions adjusted for the number of cases in the mild, moderate, and severe categories as well as cases asymptomatic at time of survey. Given that the MEPS, NESARC and NSMHW made use of only an adult sample, data from the Great Smoky Mountains Study (GSMS) were used to adjust for time spent asymptomatic versus symptomatic in ADHD and conduct disorder (Ezpeleta et al. 2001; Erskine et al. 2013). Similarly, severity adjustments for bipolar disorder and schizophrenia were informed by a separate literature review investigating the severity and health states of low prevalence disorders which are not always well represented in population surveys (Ferrari et al. 2012). Finally, co-morbidity between diseases and injuries included in GBD 2010 was accounted for through the use of microsimulations which created hypothetical populations to estimate the probability of an individual having multiple conditions. Disability weights were then adjusted downwards accordingly.
YLDs for each disorder were then calculated by multiplying their respective disability weight by the number of prevalent cases. This was done for each country, sex, age group, and time period.
Years of life lost due to premature mortality (YLLs)
Of the 291 diseases and injuries included in GBD 2010, 235 causes of mortality were identified. Cause of death estimates were based on a comprehensive database spanning 1980–2010 which consisted of vital registration, mortality surveillance, verbal autopsy and other sources (Lozano et al. 2012). ICD codes were mapped to the GBD 2010 cause list, and deaths coded to unclear causes or to conditions unlikely to be causes of death were re-assigned via standard algorithms (Lozano et al. 2012). Accidental poisoning deaths due to drugs or alcohol were recoded to those substance use disorder categories except in the case of accidental poisonings due to drugs occurring in children. YLLs were calculated by multiplying the number of deaths by the number of years estimated to be left at time of death based on standard life expectancy (e.g. 80 years if death occurred at 5 years with life expectancy estimated to be 85). YLLs were calculated by age, sex, and country. Uncertainty was calculated for all estimates by taking 1000 draws for each sex, age, and country. Mortality estimates were based on 17 258 country-years of data from 126 countries. YLLs were calculated for illicit drug use disorders, alcohol use disorders, schizophrenia, anorexia nervosa, and the residual group of other mental disorders. There was no cause-of-death data for the other mental disorders given no deaths were attributed directly to them. Important to note, suicide was classed as a separate cause in the injuries group given the physical injury of suicide was considered the cause of death rather than any underlying mental disorder.
Attributable burden
In response to the absence of suicide YLLs from mental and substance use disorder burden, supplementary comparative risk assessment (CRA) analyses have been conducted to quantify the additional burden attributable to mental and substance use disorders as risk factors for suicide (Ferrari et al. 2014). These data were used to investigate the proportion of suicide YLLs that could be re-assigned from physical injury to mental and substance use disorders in those aged between 0 and 24 years. Given that GBD 2010 found suicide YLLs were highest (15%) in those aged between 20 and 24 years, this is a particularly important consideration (Wang et al. 2012). The association between mental and substance use disorders and suicide is well recognized with relative-risks ranging from 2.7 (95% uncertainty interval (UI) 1.7–4.3) for MDD and 9.8 (95% UI 9.0–10.7) for alcohol dependence (Ferrari et al. 2014). The CRA framework employed by GBD 2010 compares the current health status with an optimum exposure distribution which has the lowest possible risk. In this case, the theoretical minimum was the counterfactual status of absence of mental or substance use disorders in the population (Lim et al. 2012). The GBD 2010 methodology to estimate attributable burden involved conducting a systematic review and meta-analysis to estimate the pooled relative risk of suicide in those with mental and substance use disorders compared to the general population. This pooled relative-risk estimate was then combined with DisMod-MR prevalence outputs for each mental and substance use disorder to calculate population attributable fractions (PAFs). Finally, these PAFs were multiplied by the corresponding suicide YLLs to estimate suicide burden attributable to mental and substance use disorders by sex, age, year, region, and country. Attributable suicide burden was estimated for mental and substance use disorders found to be associated with an elevated risk of mortality. These were MDD, anxiety disorder, bipolar disorder, schizophrenia, anorexia nervosa, alcohol dependence, opioid dependence, amphetamine dependence, and cocaine dependence. The methodology and data input for calculating the proportion of suicide burden attributable to mental and substance use disorders has been described in detail elsewhere (Ferrari et al. 2014).
Results
Globally in 2010, mental and substance use disorders were responsible for 55.5 million (values in parentheses are 95% uncertainty intervals) DALYs (49.6–61.2 million) in people aged 0–24 years. Overall, they were the 6th leading cause of DALYs in children and youth, accounting for 5.7% (5.0–6.3) of total disease burden in this age group. Mental and substance use disorders were the leading cause of global disability accounting for 54.2 million (48.5–60.0 million) YLDs, equivalent to a quarter of disability in children and youth worldwide (24.9%, 21.7–28.7).
Table 1 shows the number of DALYs (in 1000 s) attributable to each mental and substance use disorder in males and females. In children and youth, eating disorders were the only mental disorders with associated mortality while all substance use disorders (except cannabis dependence) contributed to fatal burden. Deaths from suicide (including those due to an underlying mental or substance use disorder) or vehicular accidents resulting from alcohol were classified respectively to self-harm and transport injuries in GBD 2010. Furthermore, while YLLs directly attributable to schizophrenia were calculated (Whiteford et al. 2013), none of these were attributed to those aged <25 years in GBD 2010. This resulted in mental and substance use disorders contributing 1.3 million (1.0–1.6 million) YLLs, equivalent to 0.2% (0.1–0.2) of all YLLs in children and youth globally. MDD was the leading cause of YLDs and DALYs in both males and females. The remaining mood disorders, anxiety disorders, and eating disorders were greater contributors to burden in females while conduct disorder, ADHD, autism spectrum disorders, and substance use disorders contributed more burden in males.
Table 1.
Number (in 1000 s) of DALYs, YLDs, and YLLs attributable to mental and substance use disorders in males and females aged 0–24 years in 2010
| DALYs (95% uncertainty)
|
YLDs (95% uncertainty)
|
YLLs (95% uncertainty)
|
||||
|---|---|---|---|---|---|---|
| Disorder | Males | Females | Males | Females | Males | Females |
| Major depressive disorder | 7433 (6293–8540) | 11676 (9988–13441) | 7433 (6293–8540) | 11676 (9988–13441) | 0 (0–0) | 0 (0–0) |
| Dysthymia | 1205 (951–1449) | 1602 (1309–1927) | 1205 (951–1449) | 1602 (1309–1927) | 0 (0–0) | 0 (0–0) |
| Bipolar disorder | 959 (649–1247) | 1125 (763–1490) | 959 (649–1247) | 1125 (763–1490) | 0 (0–0) | 0 (0–0) |
| Schizophrenia | 361 (252–477) | 286 (195–375) | 361 (252–477) | 286 (195–375) | 0 (0–0) | 0 (0–0) |
| Anxiety disorders | 3371 (2752–4020) | 5932 (4778–7096) | 3371 (2752–4020) | 5932 (4778–7096) | 0 (0–0) | 0 (0–0) |
| Eating disorders | 36 (26–46) | 542 (400–675) | 10 (5–15) | 511 (371–646) | 26 (18–35) | 31 (21–41) |
| Conduct disorder | 4132 (2997–5235) | 1623 (1173–2048) | 4132 (2997–5235) | 1623 (1173–2048) | 0 (0–0) | 0 (0–0) |
| Attention deficit hyperactivity disorder | 331 (240–422) | 93 (69–117) | 331 (240–422) | 93 (69–117) | 0 (0–0) | 0 (0–0) |
| Autism | 1437 (1208–1682) | 460 (385–538) | 1437 (1208–1682) | 460 (385–538) | 0 (0–0) | 0 (0–0) |
| Asperger’s syndrome | 1394 (1149–1639) | 311 (254–369) | 1394 (1149–1639) | 311 (254–369) | 0 (0–0) | 0 (0–0) |
| Idiopathic intellectual disability | 404 (305–508) | 247 (181–317) | 404 (305–508) | 247 (181–317) | 0 (0–0) | 0 (0–0) |
| Cannabis dependence | 689 (484–888) | 387 (279–496) | 689 (484–888) | 387 (279–496) | 0 (0–0) | 0 (0–0) |
| Amphetamine dependence | 595 (385–814) | 348 (222–473) | 591 (384–792) | 346 (214–469) | 4 (4–5) | 2 (2–2) |
| Cocaine dependence | 226 (136–325) | 101 (55–146) | 221 (126–318) | 99 (57–143) | 5 (4–6) | 2 (2–2) |
| Opioid dependence | 1653 (1266–2016) | 718 (547–889) | 1260 (908–1614) | 528 (365–683) | 392 (256–529) | 190 (132–245) |
| Other drug use disorders | 1101 (813–1384) | 607 (456–759) | 781 (531–1032) | 426 (283–561) | 321 (208–437) | 181 (127–238) |
| Alcohol use disorders | 2909 (2210–3606) | 798 (614–994) | 2816 (2121–3536) | 774 (592–979) | 92 (48–140) | 23 (8–39) |
| Other mental and substance use disorders | 210 (167–254) | 228 (177–281) | 161 (123–201) | 208 (155–259) | 49 (33–65) | 20 (13–26) |
| All mental and substance use disorders | 28446 (25260–31629) | 27085 (24282–29929) | 27557 (24499–30795) | 26636 (23762–29417) | 889 (611–1168) | 449 (337–568) |
DALYs, Disability-adjusted life years; YLDs, years lived with disability; YLLs, years of life lost;
Eating disorders are inclusive of anorexia nervosa and bulimia nervosa. Alcohol use disorders are inclusive of alcohol dependence and fetal alcohol syndrome.
Fig. 1 shows the rate of DALYs (per 100 000) in 2010 for mental and substance use disorders within each age group prior to 25 years of age. Drug use disorders account for all mental and substance use disorder burden in those aged <1 year, reflecting the burden attributable to babies born with drug dependence. Substance use disorders become large contributors to burden from late adolescence onwards. Burden attributable to MDD and dysthymia begins in early childhood and increases throughout youth while ADHD and conduct disorder contribute most of their DALYs during childhood and early adolescence.
Fig. 1.
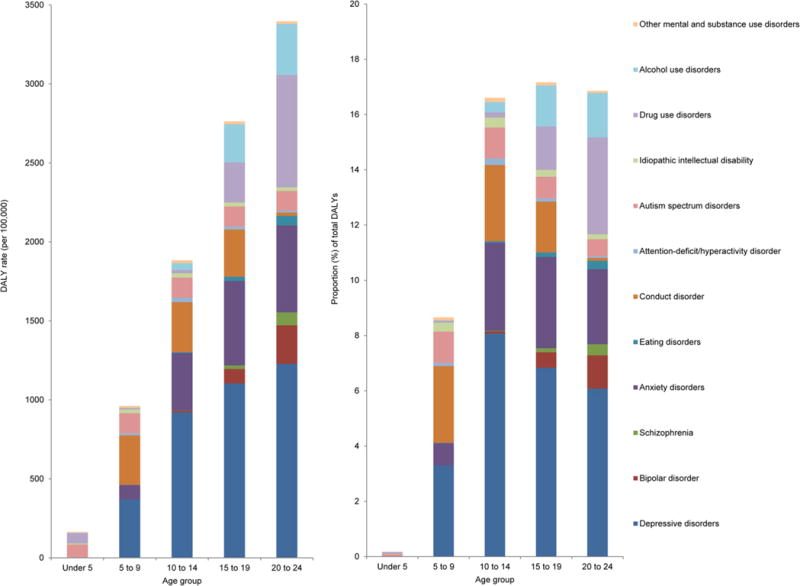
Disability-adjusted life year (DALY) rates (per 100 000) and proportions (%) for mental and substance use disorders for persons in each age group across childhood and youth in 2010.
In both HICs (consisting of the Western Europe, Australasia, high-income North America, and high-income Asia Pacific regions) and LMICs, mental and substance use disorders were the leading cause of YLDs in children and youth with 34.8% (29.9–40.5) and 23.8% (20.6–27.2) respectively. Fig. 2 shows the proportion of DALYs for 0–24 years attributable to each of the 21 main cause groups in HICs and LMICs. Mental and substance use disorders were the leading cause of DALYs in HICs, contributing 8.3 million (7.4–9.3 million) DALYs equivalent to 20.8% (18.2–23.4) of the total burden of disease in children and youth. However, in LMICs the proportion of disease burden in children and youth attributable to mental and substance use disorders was smaller due to the ongoing mortality arising from other diseases. Over half of all DALYs in these countries were attributable to communicable, maternal, neonatal, and nutritional disorders as shown in Fig. 2. Thus, mental and substance use disorders were the 7th highest cause of disease burden in LMICs, accounting for 5.0% (4.5–5.7) of total burden (47.2 million, 42.5–52.2 million DALYs).
Fig. 2.

Proportion of total disability-adjusted life years in high-income countries and low- and middle-income countries attributable to each main cause group for persons aged 0–24 years in 2010.
Fig. 3 demonstrates the proportion of total DALYs in children and youth accounted for by mental and substance use disorders at the country level. The vast majority of sub-Saharan Africa along with South Asia had the lowest proportions of burden attributable to mental and substance disorders in children and youth while HICs had the highest proportions. However, despite clear trends in burden, many of these differences in proportions between countries were within wide bounds of uncertainty which resulted from the lack of epidemiological data, particularly for LMICs.
Fig. 3.

Proportion of disability-adjusted life years attributable to mental and substance disorders in each country for children and youth in 2010. South Sudan, Western Sahara, and French Guiana were not included for burden calculations in GBD 2010.
While mental and substance use disorders contribute less burden proportionately in regions such as sub-Saharan Africa, the patterns are continually evolving as disease prevalence changes. For example diarrhea, lower respiratory infections, meningitis, and other common infectious diseases collectively were responsible for 157.3 million DALYs (138.3–176.8 million) in sub-Saharan Africa in 1990; equivalent to 40.0% (35.0–45.3%) of total burden for children and youth in that region. By 2010, this dropped to 95.7 million DALYs (86.3–104.6 million) or 24.9% (22.2–27.6%). Conversely, mental and substance use disorders contributed 5.3 million DALYs (4.8–5.9 million) or 1.3% (1.2–1.5%) in 1990. By 2010, this increased to 2.3% [2.1–2.6%; 8.9 million DALYs (8.1–9.8 million)] of total DALYs in children and youth in sub-Saharan Africa.
The burden estimates presented thus far exclude any excess deaths attributable to mental and substance use disorders as risk factors for suicide. After burden reattribution, mental and substance use disorders were responsible for an additional 6.3 million suicide YLLs in children and youth across the globe in 2010. This was equivalent to mental and substance use disorders explaining 59% of all suicide YLLs for children and youth in GBD 2010. Adding these attributable suicide YLLs increased the burden of mental and substance use disorders from 55.5 million to 61.8 million DALYs and their proportion of total DALYs from 5.7% to 6.3%, subsequently pushing their DALY ranking up from 6th to 5th place. Fig. 4 shows the additional suicide burden attributable to mental and substance use disorders in each child and youth age group.
Fig. 4.
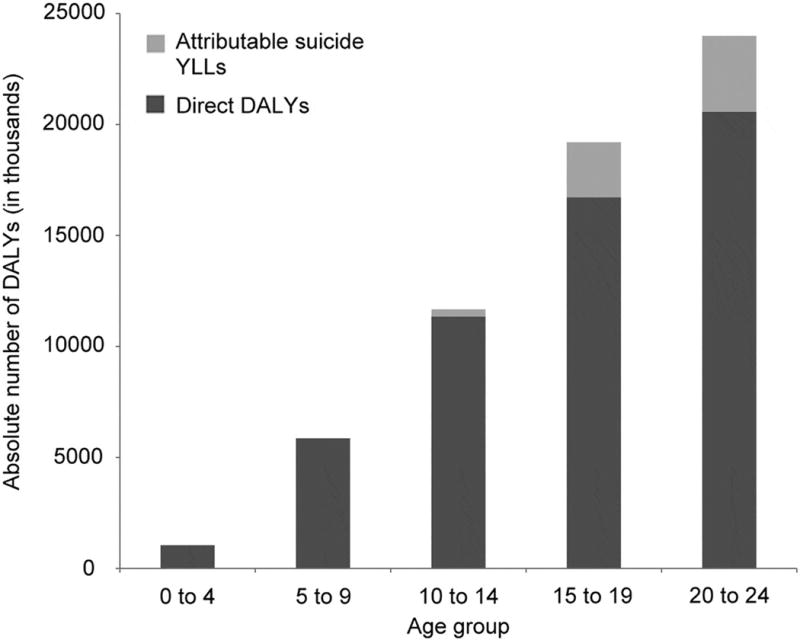
Additional suicide burden attributable to mental and substance use disorders for each age group across childhood and youth, over and above disability-adjusted life years (DALYs) assigned as a direct cause. Attributable suicides years of life lost (YLL) were only evident from the age of 5 years onwards.
Discussion
Mental and substance use disorders are the leading cause of disability in children and youth worldwide and the sixth leading cause of DALYs. Currently in LMICs, a large proportion of burden in children and youth is still accounted for by infectious diseases and neonatal disorders (Fig. 2). However, these diseases are gradually being addressed through increased vaccination rates, greater accessibility to treatment, improved pre- and post-natal care, extension of education, delay of marriage, and better nutrition, sanitation and water quality (Lozano et al. 2012; Murray et al. 2012; Wang et al. 2012). As this trend continues and deaths due to these diseases are prevented, the proportion of DALYs attributable to infectious diseases and neonatal disorders will decrease. Improved infant survival will also result in greater absolute numbers of children living to the ages at which mental and substance use disorders are most prevalent. Specific services and prevention strategies for mental and substance use disorders are largely unavailable in LMICs (Saraceno et al. 2007). Health resources will be required to meet this future demand. Service delivery for children and youth with mental and substance use disorders in LMICs will be further complicated by co-occurring social adversities (Walker et al. 2011) such as intimate partner violence (Devries et al. 2013), childhood sexual abuse (Chen et al. 2010), conflict (Charlson et al. 2012), and poverty (Patel and Kleinman, 2003). Nevertheless, LMICs have an opportunity to devote their resources to implementing effective service systems for children and youth with mental and substance use disorders, unfettered by the inertia of outdated yet entrenched ineffective systems now retained in many HICs (The Economist, 2008; Lewis et al. 2012).
Previous longitudinal studies have found that individuals who develop their mental or substance use disorder at a young age are at an increased risk of chronic or recurrent mental disorders and disabling physical conditions in adulthood (Zoccolillo, 1992; Bardone et al. 1996, 1998; Wilens et al. 1997; Fergusson and Woodward, 2002; Odgers et al. 2007). While identification and treatment of mental and substance use disorders during childhood and youth is desirable, effective prevention strategies are likely to have the greatest capacity to reduce burden. This is a challenge with mental and substance use disorders having complex and intertwined risk factors (e.g. genetics, poverty, parental mental illness, childhood adversity) which are difficult to modify and quantify. Identifying risk factors (e.g. child abuse and neglect, bullying, intimate partner violence) that are both quantifiable and modifiable through targeted intervention strategies is an immediate priority (Scott et al. 2014). Investment is also needed in programmes that have the potential to reduce the likelihood of mental and developmental disorders in childhood such as parenting skills training (Furlong et al. 2012) and maternal mental health interventions (Rahman et al. 2013). Reducing poverty has been shown to be followed by a reduction in childhood mental disorder (Costello et al. 2003), although addressing issues such as poverty, gender inequality, and social exclusion on a global scale requires significant investment and impetus. Furthermore, the increasing proportion of burden attributable to mental and substance use disorders in children and youth in LMICs will also demand integrated care for both mental and substance use disorders and physical health conditions (Collins et al. 2013; Ngo et al. 2013; Patel et al. 2013).
GBD 2010 quantifies burden in terms of health loss ‘within the skin’ of the individual with, for example, the impact on family and educational outcomes not considered. This is particularly problematic in children and youth who are dependent on family or carers and for whom the disorder can adversely alter their educational trajectory, social development, employability, and adaptive functioning (Mannuzza et al. 1993; Bardone et al. 1996, 1998). Furthermore, the increased risk of other health conditions in adulthood as a result of mental and substance use disorders in childhood and youth is not represented in the GBD 2010 framework nor is the increased risk of intentional or unintentional harm to victims by young people with conditions, such as conduct disorder, who are more likely to engage in violent behaviour (Apter et al. 1995).
Furthermore, the true extent of the association between mortality and mental and substance use disorders in children and youth was not reflected in the direct YLL burden estimations. Mortality was only attributed to a mental or substance use disorder if that disorder was the direct cause of death according to ICD-10 guidelines (WHO, 1992) meaning that most deaths in individuals with a mental disorder were attributed to the direct physical cause of death. While our burden reattribution analyses allowed the inclusion of suicide in mental and substance use disorder burden post-GBD 2010, these analyses could only include disorders which had both evidence of excess mortality and sufficient data on the relative risk of suicide. Thus, while the inclusion of attributable suicide burden substantially increased mental and substance use disorder DALYs, it still does not reflect suicide burden which may be attributable to other mental disorders such as conduct disorder (Marttunen et al. 1991; Brent et al. 1993; Apter et al. 1995), ADHD (Chronis-Tuscano et al. 2010; Nigg, 2013), and pervasive developmental disorders (Raja et al. 2011; Mayes et al. 2013). Furthermore, current evidence was insufficient to attribute other non-fatal and fatal burden to mental and substance use disorders, e.g. injury burden to ADHD and/or conduct disorder. These limitations mean GBD 2010 underestimates the full extent of the burden arising from mental and substance use disorders in children and youth.
Burden estimations are inevitably limited by lack of data which is particularly noticeable for children and youth (Whiteford et al. 2013), for ‘childhood’ mental disorders such as conduct disorder and ADHD (Erskine et al. 2013), and for LMICs (Degenhardt et al. 2011; Ferrari et al. 2011, 2013b; Baxter et al. 2013; Charlson et al. 2013; Erskine et al. 2013) which often have the largest proportions of individuals aged <25 years (United Nations, 2011). This limitation gives GBD 2010 burden estimates large uncertainty ranges and makes it difficult to detect regional differences or changes over time which are often most informative for policy makers and global organizations. As more epidemiological data for mental and substance use disorders in children and youth becomes available, particularly in LMICs, the uncertainty surrounding burden estimates will lessen and allow more concrete conclusions to be drawn.
Despite limitations, GBD 2010 found mental and substance use disorders to be the leading cause of disability in children and youth across the globe. In terms of DALYs, mental and substance use disorders were the leading cause of total burden in HICs and the seventh leading cause in LMICs, ranking them as the sixth leading contributor to disease burden in children and youth worldwide. With reductions in infectious diseases and neonatal disorders in LMICs, the proportion of disease burden attributable to mental and substance use disorders will grow, and health services, particularly in LMICs, need to adapt to meet the changing health needs of their populations (Dua et al. 2011; Ertem and WHO, 2012; Collins et al. 2013; Ngo et al. 2013; Patel et al. 2013).
Supplementary Material
Acknowledgments
This research received no specific grant from any funding agency, commercial or not-for-profit sectors. H.E.E., A.J.F., H.A.W., and J.G.S. are affiliated with the Queensland Centre for Mental Health Research which receives its core funding from the Queensland Department of Health. T.V. received funding for GBD 2010 from the Bill and Melinda Gates Foundation. G.P. is supported by a NHMRC Senior Principal Research Fellowship. These funding agencies had no involvement in this study. We thank all those who contributed to the burden estimates in GBD 2010.
Footnotes
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291714002888.
Declaration of Interest
None.
References
- Agency for Healthcare Research and Quality. United States Medical Expenditure Panel Survey 2000–2009. Agency for Healthcare Research and Quality; Rockville, USA: 2009. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Apter A, Gtohelf D, Orbach I, Weizman R, Ratzoni G, Har-Even D, Sam T. Correlation of suicidal and violent behavior in different diagnostic categories in hospitalized adolescent patients. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:912–918. doi: 10.1097/00004583-199507000-00015. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics. Mental Health and Wellbeing: Profile of Adults, Australia 1997. Australian Bureau of Statistics; Canberra, Australia: 1997. [Google Scholar]
- Bardone AM, Moffitt TE, Caspi A, Dickson N, Silva PA. Adult mental health and social outcomes of adolescent girls with depression and conduct disorder. Development and Psychopathology. 1996;8:811–829. [Google Scholar]
- Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:594–601. doi: 10.1097/00004583-199806000-00009. [DOI] [PubMed] [Google Scholar]
- Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychological Medicine. 2013;43:897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Friend AMY, Roth C, Schweers JOY, Balach L, Baugher M. Psychiatric risk factors for adolescent suicide: a case-control study. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:521–529. doi: 10.1097/00004583-199305000-00006. [DOI] [PubMed] [Google Scholar]
- Charlson FJ, Ferrari AJ, Flaxman AD, Whiteford HA. The epidemiological modelling of dysthymia: Application for the Global Burden of Disease Study 2010. Journal of Affective Disorders. 2013;151:111–120. doi: 10.1016/j.jad.2013.05.060. [DOI] [PubMed] [Google Scholar]
- Charlson FJ, Steel Z, Degenhardt L, Chey T, Silove D, Marnane C, Whiteford HA. Predicting the impact of the 2011 conflict in Libya on population mental health: PTSD and depression prevalence and mental health service requirements. PLoS ONE. 2012;7:e40593. doi: 10.1371/journal.pone.0040593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, Elamin MB, Seime RJ, Shinozaki G, Prokop LJ, Zirakzadeh A. Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis. Mayo Clinic Proceedings. 2010;85:618–629. doi: 10.4065/mcp.2009.0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BG, Pelham WE, Applegate B, Dahlke A, Overmyer M, Lahey BB. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2010;67:1044–1051. doi: 10.1001/archgenpsychiatry.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, Insel TR, Chockalingam A, Daar A, Maddox YT. Grand challenges in global mental health: integration in research, policy, and practice. PLoS Medicine. 2013;10:e1001434. doi: 10.1371/journal.pmed.1001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colman I, Murray J, Abbott RA, Maughan B, Kuh D, Croudace TJ, Jones PB. Outcomes of conduct problems in adolescence: 40 year follow-up of national cohort. British Medical Journal (Clinical Research Edition) 2009;338:1–8. doi: 10.1136/bmj.a2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Lopez MF. Accuracy in reporting past psychiatric symptoms: The role of cross-sectional studies in psychiatric research. JAMA Psychiatry. 2014;71:233–234. doi: 10.1001/jamapsychiatry.2013.4111. [DOI] [PubMed] [Google Scholar]
- Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:252–261. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello E, Compton SN, Keeler G, Angold A. Relationships between poverty and psychopathology: a natural experiment. Journal of the American Medical Association. 2003;290:2023–2029. doi: 10.1001/jama.290.15.2023. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Baxter AJ, Lee YY, Hall W, Sara GE, Johns N, Flaxman A, Whiteford HA, Vos T. The global epidemiology and burden of psychostimulant dependence: Findings from the Global Burden of Disease Study 2010. Drug and Alcohol Dependence. 2014a;137:36–47. doi: 10.1016/j.drugalcdep.2013.12.025. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Bucello C, Calabria B, Nelson P, Roberts A, Hall W, Lynskey M, Wiessing L. What data are available on the extent of illicit drug use and dependence globally? Results of four systematic reviews. Drug and Alcohol Dependence. 2011;117:85–101. doi: 10.1016/j.drugalcdep.2010.11.032. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Charlson F, Mathers B, Hall WD, Flaxman AD, Johns N, Vos T. The global epidemiology and burden of opioid dependence: results from the global burden of disease 2010 study. Addiction. 2014b;109:1320–1333. doi: 10.1111/add.12551. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Ferrari AJ, Calabria B, Hall WD, Norman RE, Mcgrath J, Flaxman AD, Engell RE, Freedman GD, Whiteford HA, Vos T. The global epidemiology and contribution of cannabis use and dependence to the global burden of disease: results from the GBD 2010 study. PLoS ONE. 2013;8:e76635. doi: 10.1371/journal.pone.0076635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, Astbury J, Watts CH. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Medicine. 2013;10:e1001439. doi: 10.1371/journal.pmed.1001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dua T, Barbui C, Clark N, Fleischmann A, Poznyak V, Van Ommeren M, Yasamy MT, Ayuso-Mateos JL, Birbeck GL, Drummond C, Freeman M, Giannakopoulos P, Levav I, Obot IS, Omigbodun O, Patel V, Phillips M, Prince M, Rahimi-Movaghar A, Rahman A, Sander JW, Saunders JB, Servili C, Rangaswamy T, Unützer J, Ventevogel P, Vijayakumar L, Thornicroft G, Saxena S. Evidence-based guidelines for mental, neurological, and substance use disorders in low- and middle-income countries: summary of WHO recommendations. PLoS Medicine. 2011;8:e1001122. doi: 10.1371/journal.pmed.1001122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erskine HE, Ferrari AJ, Nelson P, Polanczyk GV, Flaxman AD, Vos T, Whiteford HA, Scott JG. Research review: epidemiological modelling of attention-deficit/hyperactivity disorder and conduct disorder for the Global Burden of Disease Study 2010. Journal of Child Psychology and Psychiatry. 2013;54:1263–1274. doi: 10.1111/jcpp.12144. [DOI] [PubMed] [Google Scholar]
- Ertem I & World Health Organisation. Developmental Difficulties in Early Childhood: Prevention, Early Identi fication, Assessment and Intervention in Low- and Middle-Income Countries: a Review. World Health Organisation; Geneva: 2012. [Google Scholar]
- Ezpeleta L, Keeler G, Erkanli A, Costello EJ, Angold A. Epidemiology of psychiatric disability in childhood and adolescence. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2001;42:901–914. doi: 10.1111/1469-7610.00786. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MT. The effects of conduct disorder and attention deficit in middle childhood on offending and scholastic ability at age 13. Journal of Child Psychology and Psychiatry. 1993;34:899–916. doi: 10.1111/j.1469-7610.1993.tb01097.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- Ferrari A, Saha S, Mcgrath J, Norman R, Baxter A, Vos T, Whiteford H. Health states for schizophrenia and bipolar disorder within the Global Burden of Disease 2010 Study. Population Health Metrics. 2012;10:16. doi: 10.1186/1478-7954-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari AJ, Baxter AJ, Whiteford HA. A systematic review of the global distribution and availability of prevalence data for bipolar disorder. Journal of Affective Disorders. 2011;134:1–13. doi: 10.1016/j.jad.2010.11.007. [DOI] [PubMed] [Google Scholar]
- Ferrari AJ, Charlson FJ, Norman RE, Flaxman AD, Patten SB, Vos T, Whiteford HA. The epidemiological modelling of major depressive disorder: application for the Global Burden of Disease Study 2010. PLoS ONE. 2013a;8:e69637. doi: 10.1371/journal.pone.0069637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari AJ, Norman RE, Freedman G, Baxter AJ, Pirkis JE, Harris MG, Page A, Carnahan E, Degenhardt L, Vos T, Whiteford HA. The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the Global Burden of Disease Study 2010. PLoS ONE. 2014;9:e91936. doi: 10.1371/journal.pone.0091936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari AJ, Somerville AJ, Baxter AJ, Norman R, Patten SB, Vos T, Whiteford HA. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychological Medicine. 2013b;43:471–481. doi: 10.1017/S0033291712001511. [DOI] [PubMed] [Google Scholar]
- Furlong M, Mcgilloway S, Bywater T, Hutchings J, Smith SM, Donnelly M. Behavioural and cognitive-behavioural group-based parenting programmes for early-onset conduct problems in children aged 3 to 12 years. Cochrane Database of Systematic Reviews. 2012;(2) doi: 10.1002/14651858.CD008225.pub2. Art. no. CD008225. [DOI] [PubMed] [Google Scholar]
- Gore FM, Bloem PJN, Patton GC, Ferguson J, Joseph V, Coffey C, Sawyer SM, Mathers CD. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377:2093–2102. doi: 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- Green H, Mcginnity A, Meltzer H, Ford T, Goodman R. Mental Health of Children and Young People in Great Britain 2004 Palgrave. Macmillan; Hampshire: 2005. [Google Scholar]
- Hopfer C, Salomonsen-Sautel S, Mikulich-Gilbertson S, Min S-J, Mcqueen M, Crowley T, Young S, Corley R, Sakai J, Thurstone C, Hoffenberg A, Hartman C, Hewitt J. Conduct disorder and initiation of substance use: a prospective longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:511–518.e4. doi: 10.1016/j.jaac.2013.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello E, Greif Green J, Gruber MJ, Heeringa S, Merikangas KR, Pennell B-E, Sampson NA, Zaslavsky AM. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 2012;69:372–380. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjelsberg E. DSM-IV conduct disorder symptoms in adolescents as markers of registered criminality. European Child and Adolescent Psychiatry. 2002;11:2–9. doi: 10.1007/s007870200001. [DOI] [PubMed] [Google Scholar]
- Lewis T, Synowiec C, Lagomarsino G, Schweitzer J. E-health in low- and middle-income countries: findings from the Center for Health Market Innovations. Bulletin of the World Health Organization. 2012;90:332–340. doi: 10.2471/BLT.11.099820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Bessler A, Malloy P, Lapadula M. Adult outcome of hyperactive boys: educational achievement, occupational rank, and psychiatric status. Archives of General Psychiatry. 1993;50:565–576. doi: 10.1001/archpsyc.1993.01820190067007. [DOI] [PubMed] [Google Scholar]
- Marttunen MJ, Aro HM, Henriksson MM, Lönnqvist JK. Mental disorders in adolescent suicide: DSM-III-R Axes I and II diagnoses in suicides among 13- to 19-year-olds in Finland. Archives of General Psychiatry. 1991;48:834–839. doi: 10.1001/archpsyc.1991.01810330058009. [DOI] [PubMed] [Google Scholar]
- Mayes SD, Gorman AA, Hillwig-Garcia J, Syed E. Suicide ideation and attempts in children with autism. Research in Autism Spectrum Disorders. 2013;7:109–119. [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine. 2010;40:899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. British Medical Journal (Clinical Research Edition) 2009;339:332–336. [Google Scholar]
- Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Ngo VK, Rubinstein A, Ganju V, Kanellis P, Loza N, Rabadan-Diehl C, Daar AS. Grand challenges: integrating mental health care into the non-communicable disease Agenda. PLoS Medicine. 2013;10:e1001443. doi: 10.1371/journal.pmed.1001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clinical Psychology Review. 2013;33:215–228. doi: 10.1016/j.cpr.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odgers CL, Caspi A, Broadbent JM, Dickson N, Hancox RJ, Harrington H, Poulton R, Sears MR, Thomson WM, Moffitt TE. Prediction of differential adult health burden by conduct problem subtypes in males. Archives of General Psychiatry. 2007;64:476–484. doi: 10.1001/archpsyc.64.4.476. [DOI] [PubMed] [Google Scholar]
- Patel V, Belkin GS, Chockalingam A, Cooper J, Saxena S, Unützer J. Grand challenges: integrating mental health services into priority health care platforms. PLoS Medicine. 2013;10:e1001448. doi: 10.1371/journal.pmed.1001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Flisher AJ, Hetrick S, Mcgorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369:1302–1313. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bulletin of the World Health Organization. 2003;81:609–615. [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Fisher J, Bower P, Luchters S, Tran T, Yasamy MT, Saxena S, Waheed W. Interventions for common perinatal mental disorders in women in low- and middle-income countries: a systematic review and meta-analysis. Bulletin of the World Health Organization. 2013;91:593–601. doi: 10.2471/BLT.12.109819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raja M, Azzoni A, Frustaci A. Autism spectrum disorders and suicidality. Clinical Practice and Epidemiology in Mental Health. 2011;7:97–105. doi: 10.2174/1745017901107010097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravens-Sieberer U, Wille N, Erhart M, Bettge S, Wittchen H-U, Rothenberger A, Herpertz-Dahlmann B, Resch F, Hölling H, Bullinger M, Barkmann C, Schulte-Markwort M, Döpfner M. Prevalence of mental health problems among children and adolescents in Germany: results of the BELLA study within the National Health Interview and Examination Survey. European Child & Adolescent Psychiatry. 2008;17(Suppl. 1):22–33. doi: 10.1007/s00787-008-1003-2. [DOI] [PubMed] [Google Scholar]
- Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012a;380:2129–2143. doi: 10.1016/S0140-6736(12)61680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon JA, Wang H, Freeman MK, Vos T, Flaxman AD, Lopez AD, Murray CJL. Healthy life expectancy for 187 countries, 1990–2010: a systematic analysis for the Global Burden Disease Study 2010. Lancet. 2012b;380:2144–2162. doi: 10.1016/S0140-6736(12)61690-0. [DOI] [PubMed] [Google Scholar]
- Saraceno B, Van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J, Sridhar D, Underhill C. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370:1164–1174. doi: 10.1016/S0140-6736(07)61263-X. [DOI] [PubMed] [Google Scholar]
- Sawyer MG, Arney FM, Baghurst PA, Clark JJ, Graetz BW, Kosky RJ, Nurcombe B, Patton GC, Prior MR, Raphael B, Rey JM, Whaites LC, Zubrick SR. The mental health of young people in Australia: key findings from the child and adolescent component of the national survey of mental health and well-being. Australian & New Zealand Journal of Psychiatry. 2001;35:806–814. doi: 10.1046/j.1440-1614.2001.00964.x. [DOI] [PubMed] [Google Scholar]
- Sawyer SM, Afifi RA, Bearinger LH, Blakemore S-J, Dick B, Ezeh AC, Patton GC. Adolescence: a foundation for future health. Lancet. 2012;379:1630–1640. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- Scott JG, Moore SE, Sly PD, Norman RE. Bullying in children and adolescents: a modifiable risk factor for mental illness. Australian and New Zealand Journal of Psychiatry. 2014;48:209–212. doi: 10.1177/0004867413508456. [DOI] [PubMed] [Google Scholar]
- Takayanagi Y, Spira AP, Roth KB, Gallo JJ, Eaton WW, Mojtabai R. Accuracy of reports of lifetime mental and physical disorders: results from the baltimore epidemiological catchment area study. JAMA Psychiatry. 2014;71:273–280. doi: 10.1001/jamapsychiatry.2013.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Economist. The limits of leapfrogging. The Economist. 2008 ( http://www.economist.com/node/10650775) Accessed 4 August 2014.
- United Nations. World Population Prospects – The 2010 Revision. United Nations; New York: 2011. [Google Scholar]
- US National Institutes of Health National Institute on Alcohol Abuse and Alcoholism. National Epidemiologic Survey on Alcohol and Related Conditions Wave 1 and Wave 2. National Institutes of Health; Bethesda, MD, USA: 2006. [Google Scholar]
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker SP, Wachs TD, Grantham-Mcgregor S, Black MM, Nelson CA, Huffman SL, Baker-Henningham H, Chang SM, Hamadani JD, Lozoff B, Gardner JMM, Powell CA, Rahman A, Richter L. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011;378:1325–1338. doi: 10.1016/S0140-6736(11)60555-2. [DOI] [PubMed] [Google Scholar]
- Wang H, Dwyer-Lindgren L, Lofgren KT, Rajaratnam JK, Marcus JR, Levin-Rector A, Levitz CE, Lopez AD, Murray CJL. Age-specific and sex-specific mortality in 187 countries, 1970–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2071–2094. doi: 10.1016/S0140-6736(12)61719-X. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N, Burstein R, Murray CJL, Vos T. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Biederman J, Mick E, Faraone SV, Spencer T. Attention Deficit Hyperactivity Disorder (ADHD) is associated with early onset substance use disorders. Journal of Nervous and Mental Disease. 1997;185:475–482. doi: 10.1097/00005053-199708000-00001. [DOI] [PubMed] [Google Scholar]
- WHO. ICD-10 Classi fication of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. World Health Organisation; Geneva: 1992. [Google Scholar]
- WHO. Health for the World’s Adolescents – a Second Chance in the Second Decade. World Health Organisation; Geneva, Switzerland: 2014. [Google Scholar]
- Zoccolillo M. Co-occurrence of conduct disorder and its adult outcomes with depressive and anxiety disorders: a review. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:547–556. doi: 10.1097/00004583-199205000-00024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


