Abstract
Background
Contralateral prophylactic mastectomy (CPM) may be unnecessary from an oncologic perspective; therefore, the debate persists about the value of CPM in women with early stage unilateral breast cancer. Given finite healthcare resources, this study aims to evaluate the cost of contralateral prophylactic mastectomy and breast reconstruction.
Study Design
Women with unilateral breast cancer undergoing either unilateral mastectomy or unilateral mastectomy with CPM and immediate breast reconstruction (IBR) were selected from the Truven MarketScan databases between 2009 and 2013. Demographic and treatment data were recorded, and over an 18-month follow-up period, the treatment cost was tallied. A log-transformed linear model was used to compare cost between the groups.
Results
A total of 2,343 women were identified who met our inclusion criteria with 1,295 undergoing unilateral mastectomy and 1,048 undergoing CPM. Complication rates within 18 months were similar for women undergoing unilateral mastectomy and CPM (39% vs. 42%, p=0.17). Management with unilateral mastectomy with reconstruction required an adjusted cumulative mean cost of $33,557. CPM with reconstruction was an additional $11,872 in expenditure (p<0.001). The cost of initial procedures (mean difference, $6,467) and secondary procedures (mean difference, $2,455) were the greatest contributors to cost.
Conclusion
In women with unilateral breast cancer, CPM with reconstruction is more costly. The increased monetary cost of CPM may be offset by improved quality of life. However, this financial reality is an important consideration when ongoing efforts towards reimbursement reform may not pay for CPM if outcomes data are not presented to justify this procedure.
Introduction
Breast cancer is a substantial public health burden with approximately 250,000 new cases of breast cancer diagnosed in 20161. Advances in breast cancer treatment and surveillance have led to improved 5-year survival. According to the Surveillance, Epidemiology, and End Results database, 89.7% of women with breast cancer survive at least five years after diagnosis1. Despite improvements in detection, treatment and survival, many women diagnosed with unilateral breast cancer are opting for contralateral prophylactic mastectomy (CPM) to decrease their breast-cancer related risk in the contralateral breast2,3.
The rate of CPM has more than doubled in the past decade4. This rising trend favoring CPM continues in spite of the absence of a clear survival advantage over unilateral mastectomy5–7. This may be due in part to non-oncologic benefits including quality of life from the patient’s perspective. Women undergoing CPM with immediate breast reconstruction (IBR) have been reported to have an improvement in breast-cancer related anxiety and satisfaction with their breasts8,9. These intangible benefits may be drivers in the decision for CPM. Nevertheless, concerns exist in the oncologic community about this trend. The American Society of Breast Surgeons recently produced a consensus statement advising against CPM in average-risk women, in whom the procedure does not provide oncologic benefit10.
With the notion that CPM is potentially unnecessary from an oncologic standpoint in many patients, information on the financial burden of CPM on the healthcare system is needed. Single institution studies have demonstrated higher short-term healthcare costs of CPM in average-risk women11. On the other hand, cost-effectiveness of CPM compared to routine surveillance has been demonstrated for average-risk women younger than 70 years of age12. However, little is known about the cost of CPM with IBR on the national level. Hence, the purpose of our study is to evaluate healthcare resource utilization with mastectomy and reconstruction in women undergoing unilateral mastectomy and CPM using a nationwide database.
Methods
Data Source and Sample
We used the Truven MarketScan Research Databases, including the Commercial Claims and Encounters Database and the Medicare Supplemental and Coordination of Benefits Database, between 2009 and 2013. The Truven MarketScan Databases contain inpatient and outpatient encounters of employees, their spouses and dependents covered by employer-sponsored health insurance and Medicare Advantage or supplemental insurance. This database contains over 230 million de-identified patients with longitudinal healthcare-related encounters recorded for the entirety of enrollment in the health plan13. Encrypted patient identification numbers are used to connect encounters, resource utilization, pharmacy information, and health plan details. Given the de-identified nature of the data, our study obtained exempt status from our Institutional Review Board.
We included women, age 18 or older, with diagnosed unilateral breast cancer who underwent mastectomy with IBR during the study period. We then separated the patients into two groups: patients undergoing unilateral mastectomy with IBR (unilateral mastectomy) and patients undergoing a unilateral mastectomy with contralateral prophylactic mastectomy and IBR (CPM). We excluded all patients with bilateral synchronous breast cancer, patients with a previous personal history or family history of breast cancer, patients with a personal history of ovarian cancer, and patients with BRCA1/2 genetic mutations. As the intent of the study was to focus on patients with early stage breast cancer, patients who underwent neoadjuvant chemotherapy and adjuvant radiotherapy were also excluded given that these are typically patients with advanced disease. See document, Supplemental Digital Content 1, which includes a list of Current Procedural Terminal (CPT) codes and International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis or procedure codes (ICD-9-CM). We excluded all patients undergoing delayed breast reconstruction. All exclusion criteria were determined via ICD-9 codes.
Dependent Variable
The cumulative cost of care for the patient groups in an 18-month period following surgery was our outcome variable. The consumer price index from 2015 was used to adjust the cost value. The components of cumulative cost included the cost of the index procedure, secondary procedures, complications, clinic visits, emergency department visits, and hospital readmissions. Index procedure costs comprised of the cost of the mastectomy, the associated breast reconstruction, and the hospital stay. For women undergoing unilateral mastectomy, secondary procedures included symmetry procedures for the contralateral breast. Adjuvant chemotherapy was also included in the cumulative cost variable. We also calculated the expenditure associated with the individual components of the total cost.
Explanatory Variables
Variables of interest comprised patient characteristics and healthcare utilization. Patient demographic data collected included age, median household income, type of reconstruction (implant vs. autologous), and Elixhauser comorbidity score, obtained via appropriate ICD-9CM codes14,15. The occurrence and timing of postoperative complications were also recorded. Complications collected were patient-level breast complications and included infection, wound healing complications, hematoma, seroma, reconstruction failure, implant complications, and autologous reconstruction complications. Healthcare utilization was then obtained and consisted of clinic visits, emergency department (ED) visits, and hospital readmissions.
Statistical Analysis
The association between women who underwent CPM and patient demographic data, healthcare utilization, and cost were examined using Chi-square test. We used a log-transformed multivariable linear regression model to investigate the relationship between CPM and cost. In the model, we controlled for patient and hospital characteristics. We calculated predicted cost and the corresponding 95% confidence interval from the models. The data analysis was generated using SAS 9.4 (Copyright © SAS Institute Inc, Cary, NC, USA.).
Results
During the study period (2009-2013), 2,343 women met our inclusion criteria and had at least 18 months of continuous enrollment with postoperative data. Our cohort included 1,295 women (55%) who underwent unilateral mastectomy with reconstruction and 1,048 women (45%) who underwent unilateral mastectomy with CPM and reconstruction (Table 1). Women choosing CPM had higher preoperative risk, as measured by Elixhauser comorbidity score (p=0.004). Fewer women who had CPM required chemotherapy (24% in the CPM group vs 33% in the unilateral mastectomy group, p-value = <0.001). There were no differences in the distribution of the type of reconstruction (implant vs autologous) between the study groups.
Table 1.
Patient Clinical Characteristics and Demographic Data
| Patient characteristics | Unilateral Mastectomy | CPM | P values |
|---|---|---|---|
| Total | 1,295 (55%) | 1,048 (45%) | |
| Type of Reconstruction | |||
| Implant | 1,122 (87%) | 892 (85%) | 0.32 |
| Autologous | 173 (13%) | 156 (15%) | |
| Age | |||
| 18-34 | 48 (4%) | 74 (7%) | <0.001 |
| 35-44 | 249 (19%) | 286 (27%) | |
| 45-54 | 546 (42%) | 419 (40%) | |
| 55-64 | 369 (28%) | 225 (21%) | |
| 65 and older | 83 (6%) | 44 (4%) | |
| Quartile of median house income | |||
| Quartile1 (<=$46,910) | 217 (17%) | 132 (13%) | 0.03 |
| Quarile2 ($46,910 to $51,920) | 217 (17%) | 185 (18%) | |
| Quartile3 ($51,920 to $58,900) | 358 (28%) | 309 (29%) | |
| Quartile4 (> $58,900) | 350 (27%) | 306 (29%) | |
| Missing | 153 (12%) | 116 (11%) | |
| Comorbidity score | |||
| Quartile1 (≤12) | 328 (25%) | 290 (28%) | 0.004 |
| Quartile2 (13-20) | 284 (22%) | 204 (19%) | |
| Quartile3 (21-27) | 281 (22%) | 178 (17%) | |
| Quartile4 (≥ 27) | 402 (31%) | 376 (36%) | |
| Region | |||
| North east | 266 (21%) | 287 (27%) | <0.001 |
| North central | 297 (23%) | 224 (21%) | |
| South | 445 (34%) | 300 (29%) | |
| West | 262 (20%) | 221 (21%) | |
| Missing | 25 (2%) | 16 (2%) | |
| Chemo within 18 months | |||
| No | 873 (67%) | 792 (76%) | <0.001 |
| Yes | 422 (33%) | 256 (24%) |
Overall, complication rates were slightly higher in the CPM group both at 30 days and 18 months postoperatively. However, these differences did not reach statistical significance (Table 2). Patients undergoing CPM had fewer clinic visits than those who underwent unilateral mastectomy (Table 3). Utilization of the emergency department followed a similar pattern with 8% of women who underwent CPM using the emergency department compared to 11% of women who underwent unilateral mastectomy (p-value= <0.001) (Figure 1). Postoperative hospital readmission rates did not significantly differ based on surgical intervention.
Table 2.
Complication rates
| Unilateral Mastectomy | CPM | P values | |
|---|---|---|---|
| Complications within 30 days | |||
| No | 1,139 (88%) | 907 (87%) | 0.34 |
| Yes | 156 (12%) | 141 (13%) | |
| Complications within 18 months | |||
| No | 790 (61%) | 609 (58%) | 0.17 |
| Yes | 505 (39%) | 439 (42%) |
Table 3.
Clinic and Hospital Utilization within 18 Months Post-Reconstruction
| Patient characteristics | Unilateral Mastectomy | CPM | P values |
|---|---|---|---|
| Clinic visits | <0.001 | ||
| <=4 | 328 (25%) | 396 (38%) | |
| 5-8 | 338 (26%) | 228 (22%) | |
| 9-14 | 309 (24%) | 214 (20%) | |
| >14 | 320 (25%) | 210 (20%) | |
| ED visits | |||
| No | 1,149 (89%) | 966 (92%) | 0.006 |
| Yes | 146 (11%) | 82 (8%) | |
| Hospital readmission | |||
| No | 1,086 (84%) | 888 (85%) | 0.60 |
| Yes | 209 (16%) | 160 (15%) |
ED: emergency department
Figure 1.
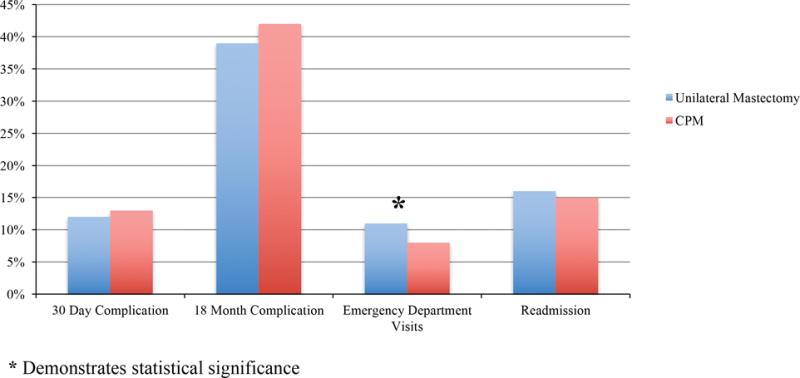
Complications, Emergency Department Visits, and Hospital Readmission Rates by Surgery Type
Table 4 outlines the cost of healthcare utilization of the two groups. The cost of the index oncologic and reconstructive procedure was significantly higher for the women undergoing CPM ($17,095 for CPM vs. $10,628 for unilateral mastectomy, p-value= <0.001). Women who underwent CPM had a higher cumulative cost within 18 months ($37,811 for CPM vs. $33,557 for the unilateral mastectomy, p-value= <0.001) with a mean difference in cost between the cohorts of $4,254 (Table 4). Secondary procedures within 18 months of mastectomy and reconstruction were significantly higher in patients undergoing CPM ($8,317 for CPM vs. $5,862 for unilateral mastectomy, p-value= <0.001). The cost related to clinic visits was higher after unilateral mastectomy ($1,543 vs $1,260, p< 0.001). No significant differences in cost were observed for postoperative complications, emergency department visits, and hospital readmissions between the two groups.
Table 4.
Cost of Utilization Comparing Unilateral Mastectomy to CPM
| Mean values | Unilateral mastectomy (SD) | CPM (SD) | P values* |
|---|---|---|---|
| Cumulative cost within 18 months | 33,557 (44,072) | 37,811 (44,885) | <0.001 |
| Cost of index procedures | 10,628 (15,088) | 17,095 (26,309) | <0.001 |
| Cost of adjuvant chemotherapy | 12,438 (33,033) | 9,117 (32,049) | <0.001 |
| Cost of complications within 30 days | 1,593 (15,307) | 1,738 (10,476) | 0.222 |
| Cost of complications within 18 months | 4,627 (17,807) | 4,722 (13,384) | 0.118 |
| Cost of secondary procedures within 18 months | 5,862 (6,986) | 8,317 (12,567) | <0.001 |
| Cost of clinic visits | 1,543 (2,503) | 1,260 (1,300) | <0.001 |
| Cost of ED visits within 18 months | 232 (2,633) | 378 (5,946) | 0.008 |
| Cost of readmission within 18 months | 2,746 (10,290) | 1,983 (8,051) | 0.383 |
ED: emergency department; SD: standard deviation
After separating the cohorts by reconstruction type, CPM was cumulatively more expensive for autologous reconstruction ($68,492 for CPM versus $49,013 for unilateral mastectomy, p< 0.001) and for implant-based reconstruction ($32,446 for CPM versus $31,174 for unilateral mastectomy, p< 0.001) (Table 5). Women who underwent CPM with autologous and implant-based breast reconstruction had a more costly index oncologic and reconstruction procedure as compared to unilateral mastectomy (p-value=<0.001). However, the cost of secondary procedures for autologous breast reconstruction were similar between CPM and unilateral mastectomy (p-value: 0.248); while patients undergoing CPM and implant-based reconstruction had significantly higher expenditure for secondary procedures when compared to women undergoing unilateral mastectomy and implant-based reconstruction ($8,143 for CPM versus $6,010 for unilateral mastectomy, p-value <0.001).
Table 5.
Cost of Utilization Separated by Reconstruction Type
| Mean values | Unilateral mastectomy (SD) | CPM (SD) | P values* |
|---|---|---|---|
| Autologous-Based Reconstruction | |||
| Cumulative cost within 18 months | 49,013 (53,148) | 68,492 (59,690) | <0.001 |
| Cost of index procedures | 27,439 (25,978) | 48,902 (48,629) | <0.001 |
| Cost of adjuvant chemotherapy | 11,797 (38,285) | 10,232 (36,645) | 0.602 |
| Cost of complications within 30 days | 6,813 (18,052) | 7,349 (21,058) | 0.483 |
| Cost of complications within 18 months | 3,498 (13,963) | 5,953 (20,427) | 0.057 |
| Cost of secondary procedures within 18 months | 4,898 (6,662) | 9,310 (17,263) | 0.248 |
| Cost of clinic visits | 1,339 (1,657) | 1,096 (1,187) | 0.029 |
| Cost of ED visits within 18 months | 536 (6,044) | 117 (796) | 0.378 |
| Cost of readmission within 18 months | 3,701 (15,699) | 2,095 (8,616) | 0.908 |
| Implant-Based Reconstruction | |||
| Cumulative cost within 18 months | 31,174 (42,025) | 32,446 (39,421) | <0.001 |
| Cost of index procedures | 8,036 (10,436) | 11,533 (13,924) | <0.001 |
| Cost of adjuvant chemotherapy | 12,537 (32,165) | 8,922 (31,195) | <0.001 |
| Cost of complications within 30 days | 4,290 (17,753) | 4,263 (11,487) | 0.160 |
| Cost of complications within 18 months | 1,299 (15,489) | 1,001 (7,262) | 0.847 |
| Cost of secondary procedures within 18 months | 6,010 (7,026) | 8,143 (11,556) | <0.001 |
| Cost of clinic visits | 1,574 (2,608) | 1,288 (1,318) | <0.001 |
| Cost of ED visits within 18 months | 185 (1,543) | 424 (6,436) | 0.013 |
| Cost of readmission within 18 months | 2,599 (9,179) | 1,963 (7,953) | 0.326 |
In multivariable analysis, receipt of CPM was predictive of higher cost (adjusted mean difference in cumulative cost between CPM and unilateral mastectomy: $11,872 ($8,920-$15,029), p<0.001) (Table 6). Patients with complications or patients requiring readmission had increased expenditure. However, emergency department visits and number of clinic visits within 18 months were not predictive of increased spending. Increased cost was associated with autologous breast reconstruction (adjusted mean difference in cumulative cost between autologous and implant reconstruction: $37,136 95% CI: $31,016-43,853, p<0.001).
Table 6.
Linear Log Logistic Regression of Reconstruction and Cost
| Adjusted mean difference in cumulative cost (95% CI) | P values | Adjusted mean cumulative cost | |
|---|---|---|---|
| Mastectomy lateral | |||
| Unilateral | Ref | Ref | 33,557 |
| Bilateral | 11,872 (8,920-15,029) | <0.001 | 45,429 |
| Type of Reconstruction | |||
| Implant | Ref | Ref | 31,737 |
| Autologous | 37,136 (31,016-43,853) | <0.001 | 68,873 |
| Complications | |||
| No | Ref | Ref | 29,663 |
| Yes | 15,370 (12,349-18,608) | <0.001 | 45,033 |
| Age | |||
| 18-34 | Ref | Ref | 36,666 |
| 35-44 | −482 (−5,853-5,826) | 0.872 | 36,185 |
| 45-54 | −1,388 (−6,445-4,516) | 0.625 | 35,278 |
| 55-64 | −4,198 (−9,030-1,480) | 0.139 | 32,469 |
| 65 and older | −1,852 (−8,219-5,941) | 0.615 | 34,815 |
| Quartile of median house income | |||
| Quartile 1 (≤ $46,910) | Ref | Ref | 32,031 |
| Quartile 2 ($46,910 to $51,920) | 2,347 (−1,211-6,316) | 0.205 | 34,377 |
| Quartile 3 ($51,920 to $58,900) | 1,531 (−1,621-5,009) | 0.354 | 33,561 |
| Quartile 4 (> $58,900) | 11,183 (7,108-15,683) | <0.001 | 43,214 |
| Comorbidity score | |||
| Quartile 1 (≤ 12) | Ref | Ref | 31,903 |
| Quartile 2 (13-20) | −1,217 (−4,034-1,884) | 0.428 | 34,377 |
| Quartile 3 (21-27) | 1,301 (−1,834-4,763) | 0.43 | 33,561 |
| Quartile 4 (≥ 27) | −891 (−3,434-1,879) | 0.517 | 43,214 |
| ED visits | |||
| No | Ref | Ref | 33,339 |
| Yes | 3,491 (−370-7,803) | 0.078 | 36,830 |
| Readmissions | |||
| No | Ref | Ref | 31,349 |
| Yes | 22,048 (17,210-27,368) | <0.001 | 53,396 |
| Number of clinic visits within 18 months | |||
| ≤4 | Ref | Ref | 24,408 |
| 5-8 | 2,040 (−239-4,535) | 0.081 | 26,448 |
| 9-14 | 1,280 (−981-3,759) | 0.277 | 25,688 |
| >14 | −357 (−2,554-2,060) | 0.763 | 24,051 |
ED: emergency department
Discussion
Healthcare costs in the United States are considerable and continue to rise. In 2015, healthcare expenditure accounted for 17.8% of the gross domestic product, in comparison to 17.4% in 201416. Given the substantial financial burden of healthcare in the United States, policymakers are moving towards value-based healthcare and bundling of payments. CPM represents a surgical procedure that warrants a closer evaluation with a focus on resource utilization given the controversy that surrounds its widespread application. In this study of nationwide insurance claims data on reconstructed patients, we found that CPM is significantly more expensive than unilateral mastectomy. The index procedures (mastectomy and reconstruction) and secondary revision of the reconstructive procedures were the largest contributors to the observed differences in cost. Over the 18-month postoperative period, this increased cost for CPM persisted despite significantly lower clinic and emergency department utilization.
Value in healthcare has been defined as outcomes relative to monetary cost17. In the current political climate, policymakers advocate for improved value either by reducing cost or improving outcomes. In the field of surgery, outcomes are heterogeneous, intrinsically condition-specific and move beyond the morbidity and mortality associated with the surgery itself18. These outcomes must be assessed at the patient level19. For breast reconstruction including CPM, outcomes can range from postoperative complications to patient-reported assessments of postoperative well-being. Breast cancer patients choose CPM for a variety of reasons. These reasons must be factored into the outcome equation and may trump the lack of survival benefit of CPM in low-risk women. Therefore, in the discussion of value of CPM, healthcare policymakers with the help of plastic surgery professional societies, providers, and patients need to deliver quality measures to improve outcomes and subsequently the value of CPM. The Medicare Access and CHIP Reauthorization Act (MACRA) was passed in 2015 and pushes the healthcare system towards a value-based payment model with the purpose of improving outcomes at a lower cost20–22. Within MACRA, quality assurance programs were formed to provide performance measures for healthcare delivery. The American Society of Plastic Surgeons (ASPS), in compliance with MACRA, has developed unique quality performance assessments for plastic surgeons. These measure sets evaluate providers on the quality of care they deliver, improvement in clinical practice, resource utilization, and advancement of care information23. They are aimed at minimizing complications, thus improving plastic surgery outcomes. However, as outcomes encompass more than surgical complications, a broader holistic view is essential.
In the absence of an increased risk for future breast cancer, women diagnosed with unilateral breast cancer opt for CPM for a variety of reasons. Gaining an understanding of factors that influence women’s decisions for CPM has been critical in efforts made to better guide patients through these complex decisions, avoid overtreatment, and improve outcomes. Anxiety after treatment is a primary example of an outcome, unrelated to morbidity, that patients find to be important. In a multicenter prospective assessment of patient reported outcomes in women undergoing CPM or unilateral mastectomy with reconstruction, women who underwent CPM were found to have higher levels of anxiety prior to mastectomy9. Following mastectomy, the levels of anxiety in these patients who had undergone CPM or unilateral mastectomy were similar9. Other studies have corroborated this finding, citing anxiety, worry of cancer recurrence, and need for less surveillance as some reasons for decisions in favor of CPM2,24–26. Furthermore, a desire for symmetry with improved breast aesthetics has also been identified as an additional factor impacting decisions for CPM27–29. A recent qualitative study on a reconstructed cohort of patients with unilateral early stage breast cancer found that, although desires for symmetry were not the primary reason for decisions made in favor of CPM, they played a supportive role2. Patients report improved satisfaction with breasts after CPM with bilateral implant reconstruction when compared to those who have undergone unilateral mastectomy with similar reconstruction9. These non-oncologic factors must be factored into the discussion on outcomes and value of CPM for breast cancer patients.
A primary concern with widespread use of CPM is the potential for increased postoperative morbidity. Studies have reported on higher surgical complication rates of CPM when compared to unilateral mastectomy9,28,30–32. Our study, utilizing a nationwide generalizable all private insurance database, did not reveal a significant difference in complications rates at both 30 days postoperatively and 18 months postoperatively when comparing CPM with unilateral mastectomy. This difference from other reports in the literature is likely due to limitations in data abstraction unique to the claims database. However, despite similar complication rates, the cost of CPM remained significantly higher than the cost of unilateral mastectomy. This increased expenditure in women choosing CPM as compared to those opting for unilateral mastectomy was present for the index oncologic and reconstructive procedure ($17,095 vs $10,628, p= <0.001), for secondary procedures ($8,317 vs $5,862, p= <0.001), and overall within 18 months of reconstruction ($29,954 vs $22,661, p= <0.001). Similar findings were reported in a single institution retrospective study by Deshmukh et al., concluding that in the short-term CPM significantly increased healthcare utilization with a 16.9% increase in total cost as compared to patients not managed with CPM11. Furthermore, patients undergoing CPM were more likely to have breast reconstruction, and as expected, receipt of reconstruction was more costly. Other studies however, have analyzed the cost-effectiveness of CPM in comparison to routine surveillance in the long-term12,33. A study by Mattos et al. utilized a simplified decision tree analysis and determined that CPM with reconstruction was cost-effective when the incidence of breast cancer exceeded 0.6% per year33. Zendejas et al. found that CPM was less costly then surveillance for women diagnosed with unilateral breast cancer who were younger than 70 years of age12. However, post-mastectomy reconstruction was not part of the cost variable in this study. Though cost-effectiveness is beyond the scope of this study, these findings are logical and highlight the balance that is needed when evaluating the cost of CPM to the healthcare system. This study on the financial implications of CPM is just one piece in the discussion of value, and robust outcomes data are needed to justify the increased cost of CPM.
This study has a number of limitations. We utilized data from the Truven MarketScan databases over a 5-year time period and were unable to study the long-term cost implications of CPM. Furthermore, MarketScan only includes information from commercially insured patients or those with private Medicare supplemental insurance, thus limiting the generalizability of this study to other insurers or the uninsured. Our analyses did not include race or ethnicity, as these data points are unavailable in MarketScan. Race has been shown to have and influence on medical expenditure for breast cancer treatment including inpatient, outpatient, and medication costs34. In using a claims database, there lacks granularity regarding clinical characteristics including family history and adoption status of the patients. Therefore, we could not control for these factors.
Conclusions
As nationwide rates of CPM continue to rise, the cost of CPM to the healthcare system remains a public health predicament. CPM is significantly more expensive for the index oncologic and reconstructive procedure, secondary procedures, and cumulatively within 18 months of surgical treatment. However, monetary cost is only part of the equation in the discussion of value of CPM, and all outcomes, including complications and patient-reported outcomes, must be factored into the determination of value for CPM.
Supplementary Material
Supplemental Digital Content 1: See document which shows the Diagnosis and Procedure Codes.
Acknowledgments
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number 2 K24-AR053120-06. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Financial Disclosure Statement: The authors have nothing to disclose.
Authorship Roles
Jessica I. Billig, MD: Study design, data analysis, manuscript writing, final approval of manuscript
Anthony Duncan, BSc: Study design, manuscript writing, final approval of manuscript
Lin Zhong, MD, MPH: Study design, data collection, data analysis, manuscript writing, final approval of manuscript
Oluseyi Aliu, MD, MS: Study design, manuscript writing, final approval of manuscript
Erika D. Sears, MD, MS: Study design, manuscript writing, final approval of manuscript
Kevin C. Chung, MD, MS: Study design, manuscript writing, final approval of manuscript
Adeyiza O. Momoh, MD: Study design, manuscript writing, final approval of manuscript
This study was deemed IRB exempt from University of Michigan Institutional Review Board.
References
- 1.Howlander N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review. Bethesda, MD: National Cancer Institute; pp. 1975–2013. April 2016 ed. [Google Scholar]
- 2.Buchanan PJ, Abdulghani M, Waljee JF, et al. An Analysis of the Decisions Made for Contralateral Prophylactic Mastectomy and Breast Reconstruction. Plastic and reconstructive surgery. 2016;138:29–40. doi: 10.1097/PRS.0000000000002263. [DOI] [PubMed] [Google Scholar]
- 3.Ager B, Butow P, Jansen J, Phillips KA, Porter D. Contralateral prophylactic mastectomy (CPM): A systematic review of patient reported factors and psychological predictors influencing choice and satisfaction. Breast. 2016;28:107–20. doi: 10.1016/j.breast.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2007;25:5203–9. doi: 10.1200/JCO.2007.12.3141. [DOI] [PubMed] [Google Scholar]
- 5.Tuttle TM, Jarosek S, Habermann EB, et al. Increasing rates of contralateral prophylactic mastectomy among patients with ductal carcinoma in situ. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2009;27:1362–7. doi: 10.1200/JCO.2008.20.1681. [DOI] [PubMed] [Google Scholar]
- 6.Lostumbo L, Carbine NE, Wallace J. Prophylactic mastectomy for the prevention of breast cancer. The Cochrane database of systematic reviews. 2010:CD002748. doi: 10.1002/14651858.CD002748.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M. Growing Use of Contralateral Prophylactic Mastectomy Despite no Improvement in Long-term Survival for Invasive Breast Cancer. Annals of surgery. 2016 doi: 10.1097/SLA.0000000000001698. [DOI] [PubMed] [Google Scholar]
- 8.Koslow S, Pharmer LA, Scott AM, et al. Long-term patient-reported satisfaction after contralateral prophylactic mastectomy and implant reconstruction. Annals of surgical oncology. 2013;20:3422–9. doi: 10.1245/s10434-013-3026-2. [DOI] [PubMed] [Google Scholar]
- 9.Momoh AO, Cohen WA, Kidwell KM, et al. Tradeoffs Associated With Contralateral Prophylactic Mastectomy in Women Choosing Breast Reconstruction: Results of a Prospective Multicenter Cohort. Annals of surgery. 2016 doi: 10.1097/SLA.0000000000001840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boughey JC, Attai DJ, Chen SL, et al. Contralateral Prophylactic Mastectomy Consensus Statement from the American Society of Breast Surgeons: Additional Considerations and a Framework for Shared Decision Making. Annals of surgical oncology. 2016 doi: 10.1245/s10434-016-5408-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deshmukh AA, Cantor SB, Crosby MA, et al. Cost of contralateral prophylactic mastectomy. Annals of surgical oncology. 2014;21:2823–30. doi: 10.1245/s10434-014-3759-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zendejas B, Moriarty JP, O’Byrne J, Degnim AC, Farley DR, Boughey JC. Cost-effectiveness of contralateral prophylactic mastectomy versus routine surveillance in patients with unilateral breast cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2011;29:2993–3000. doi: 10.1200/JCO.2011.35.6956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Danielson E. Health Research Data for the Real World: The MarketScan Databases (White Paper) Ann Arbor, MI: Truven Analytics; 2014. [Google Scholar]
- 14.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 15.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Medical care. 2009;47:626–33. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 16.Centers of Medicare and Medicaid. National Health Expenditures 2015 Highlights. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/highlights.pdf. Accessed March 4, 2017.
- 17.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–81. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 18.Atkins JH, Fleisher LA. Value from the Patients’ and Payers’ Perspectives. Anesthesiol Clin. 2015;33:651–8. doi: 10.1016/j.anclin.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harv Bus Rev. 2011;89:46–52. 4, 6-61 passim. [PubMed] [Google Scholar]
- 20.Medicare Access CHIP Reauthorization Act of 2015. Library of Congress. 2015 Available at: https://www.congress/gov/bill/114th-congress/house-bill/2. Accessed April 22, 2016.
- 21.Squitieri L, Chung KC. Value-Based Payment Reform and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015: A Primer for Plastic Surgeons. Plastic and reconstructive surgery. 2017 doi: 10.1097/PRS.0000000000003431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quality Payment Program. Centers for Medicare and Medicaid Services; 2016. Available at: https://qpp.cms.gov. Accessed April 22, 2016. [Google Scholar]
- 23.American Society of Plastic Surgeons (ASPS) Participate in MIPS. Available at: https://www.plasticsurgery.org/for-medical-professionals/health-policy/macra/participate-in-mips. Accessed April 22, 2016.
- 24.Rosenberg SM, Sepucha K, Ruddy KJ, et al. Local Therapy Decision-Making and Contralateral Prophylactic Mastectomy in Young Women with Early-Stage Breast Cancer. Annals of surgical oncology. 2015;22:3809–15. doi: 10.1245/s10434-015-4572-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borstelmann NA, Rosenberg SM, Ruddy KJ, et al. Partner support and anxiety in young women with breast cancer. Psycho-oncology. 2015;24:1679–85. doi: 10.1002/pon.3780. [DOI] [PubMed] [Google Scholar]
- 26.Rendle KA, Halley MC, May SG, Frosch DL. Redefining Risk and Benefit: Understanding the Decision to Undergo Contralateral Prophylactic Mastectomy. Qualitative health research. 2015;25:1251–9. doi: 10.1177/1049732314557085. [DOI] [PubMed] [Google Scholar]
- 27.Ashfaq A, McGhan LJ, Pockaj BA, et al. Impact of breast reconstruction on the decision to undergo contralateral prophylactic mastectomy. Annals of surgical oncology. 2014;21:2934–40. doi: 10.1245/s10434-014-3712-8. [DOI] [PubMed] [Google Scholar]
- 28.Crosby MA, Garvey PB, Selber JC, et al. Reconstructive outcomes in patients undergoing contralateral prophylactic mastectomy. Plastic and reconstructive surgery. 2011;128:1025–33. doi: 10.1097/PRS.0b013e31822b6682. [DOI] [PubMed] [Google Scholar]
- 29.Pinell-White XA, Kolegraff K, Carlson GW. Predictors of contralateral prophylactic mastectomy and the impact on breast reconstruction. Annals of plastic surgery. 2014;72:S153–7. doi: 10.1097/SAP.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 30.Boughey JC, Hoskin TL, Hartmann LC, et al. Impact of reconstruction and reoperation on long-term patient-reported satisfaction after contralateral prophylactic mastectomy. Annals of surgical oncology. 2015;22:401–8. doi: 10.1245/s10434-014-4053-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller ME, Czechura T, Martz B, et al. Operative risks associated with contralateral prophylactic mastectomy: a single institution experience. Annals of surgical oncology. 2013;20:4113–20. doi: 10.1245/s10434-013-3108-1. [DOI] [PubMed] [Google Scholar]
- 32.Silva AK, Lapin B, Yao KA, Song DH, Sisco M. The Effect of Contralateral Prophylactic Mastectomy on Perioperative Complications in Women Undergoing Immediate Breast Reconstruction: A NSQIP Analysis. Annals of surgical oncology. 2015;22:3474–80. doi: 10.1245/s10434-015-4628-7. [DOI] [PubMed] [Google Scholar]
- 33.Mattos D, Gfrerer L, Reish RG, et al. Lifetime Costs of Prophylactic Mastectomies and Reconstruction versus Surveillance. Plastic and reconstructive surgery. 2015;136:730e–40e. doi: 10.1097/PRS.0000000000001763. [DOI] [PubMed] [Google Scholar]
- 34.Ekwueme DU, Allaire BT, Guy GP, Jr, Arnold S, Trogdon JG. Treatment Costs of Breast Cancer Among Younger Women Aged 19-44 Years Enrolled in Medicaid. Am J Prev Med. 2016;50:278–85. doi: 10.1016/j.amepre.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1: See document which shows the Diagnosis and Procedure Codes.


