Abstract
Purpose
To investigate whether working conditions (number of 24-h shifts, number of calls, sedentary work, job strain, effort–reward imbalance, and physical demands) are associated with elevated blood pressure and hypertension among professional firefighters.
Methods
A total of 330 (321 males and 9 females) firefighters were chosen for this study among the Southern California firefighters who participated in a work and obesity project. Working conditions were measured with a firefighter-specific occupational health questionnaire. Blood pressure was clinically assessed, and hypertension was defined according to the contemporary standard classification.
Results
About 11 % of the firefighters had hypertension. Fifty percent of the hypertensive firefighters (mostly mild hypertensive) had uncontrolled high blood pressure. Hypertension was more prevalent in male, older, and high-rank firefighters and firefighter who reported low numbers of daily calls. In male firefighters who were normotensive or hypertensive without taking anti-hypertensive medication, additional 24-h shifts in the past month increased the risk of elevated diastolic blood pressure (DBP) than those who reported a standard work schedule (eight to eleven 24-h shifts). Particularly, firefighters who reported sixteen 24-h shifts had 5.0 mmHg higher DBP (p < 0.01). Body mass index attenuated the association between number of shifts and blood pressure to some extent. Firefighters who reported “increased job demands over the past years” had 3.0 mmHg (p = 0.06) higher systolic blood pressure. Other working conditions were not associated with elevated blood pressure and hypertension.
Conclusions
Many additional 24-h shifts and increased job demands were risk factors for elevated blood pressure in male firefighters. Optimal collective and individual workload and improved hypertension management are warranted for enhancing the cardiovascular health of firefighters.
Keywords: Job strain, Effort–reward imbalance, Hypertension, Body mass index, Anti-hypertensive medication, Health-related behaviors
Introduction
Hypertension is a well-established risk factor for coronary heart disease, stroke, and total mortality in both general populations (Chobanian et al. 2003; James et al. 2014) and firefighters (Geibe et al. 2008; Kales et al. 2007; Yang et al. 2013). About 1.2 million firefighters are among the occupational groups with high hypertension prevalence in the USA (Davila et al. 2012). However, little is known about the occupational risk factors for hypertension or elevated blood pressure among firefighters (Feairheller 2015), which is an essential information for building a comprehensive prevention strategy to address hypertension or elevated blood pressure, and CVD among firefighters.
Kales et al. (2009) proposed four possible occupational risk factors for hypertension among US emergency responders, including firefighters: shift work (including overtime work), irregular physical exertion including sedentary work, noise exposure, and job strain (a combination of high job demands and low job control). However, there are no epidemiological studies of firefighters that examine the suggested occupational risk factors in relation to clinically assessed high blood pressure or hypertension. Also, some of the suggested occupational risk factors may no longer be relevant to contemporary US firefighters. For example, the proposed relationship between job strain and hypertension by Kales et al. (2009), based on the Quality of Employment Surveys in the 1970s, may no longer be relevant due to a substantial change (expansion) of firefighter occupational roles as first respondents dealing with non-fire medical emergency calls as well as fire-related calls since the 1970s (Choi et al. 2011). Choi et al. (2014a) reported that most professional firefighters from Southern California reported high physical and psychological job demands as expected, but also reported high job control rather than low job control.
Furthermore, despite some evidence for shift work or overtime work as a risk factor for clinically assessed high blood pressure or hypertension in non-firefighter working populations (Hayashi et al. 1996; Kubo et al. 2013; Nakamura et al. 2012; Ohlander et al. 2015; Ohira et al. 2000; Sakata et al. 2003; Souza et al. 2015; Su et al. 2008; Suwazono et al. 2008), none of the studies examined the impact of the unique shift schedules of most US professional firefighters who work a 24-h shift work schedule, including frequent additional/overtime 24-h shifts (Choi et al. 2014b). Also, most of the studies have considered only shift work or overtime as the occupational risk factor in analyses. Thus, there is a possibility that their findings represent a residual confounding effect due to unmeasured occupational risk factors such as job strain, effort–reward imbalance, and physical job demands (Gilbert-Ouimet et al. 2014; Virkkunen et al. 2007).
The purpose of this study is to investigate whether physical and psychosocial working conditions (number of 24-h shifts, number of calls, sedentary work, job strain, effort–reward imbalance, and physical demands) are risk factors for elevated blood pressure or hypertension among professional firefighters. We used the data set of the FORWARD study (Choi et al. 2011) in which multiple occupational hazards were examined in Southern California professional firefighters, along with their clinical resting blood pressure.
Methods
Background: FORWARD study
The main purpose of the FORWARD study (2010–2013) was to explore occupational and behavioral risk factors for obesity in firefighters who work for a fire department in Southern California (Choi et al. 2011). The study was strongly supported by both the fire department and a local union of the International Association of Fire Fighters (IAFF). The protocol of the FORWARD study was reviewed and approved by the Institutional Review Board (IRB) of the University of California, Irvine. All firefighters gave written informed consent for their participation in the study. Phase I of the study involved developing a firefighter-specific work and health questionnaire (called hereafter the FORWARD study questionnaire) through four focus groups with 20 firefighters of different ranks from January to April 2011 (Dobson et al. 2013). Phase II of the study was a cross-sectional study using the FORWARD study questionnaire and various weight-related health outcomes measured at a university clinic (Choi et al. 2016a). A random sample of 365 firefighters (356 males and 9 females) from the total population of about 800 firefighters in the fire department participated in the survey (participation rate, 84 % of 436 firefighters) when they visited the university clinic for their biennial wellness and fitness (WEFIT) medical examinations between May 2011 and December 2012. In Phase III of the study, among the survey participants, a random selection of 83 firefighters were additionally recruited for a sub-study (participation rate, 50 %) between September 2011 and July 2012 in which firefighters were asked to wear a physical activity monitor and record their food intake in a diary for 1 on-duty day (24-h) and 1 off-duty day (24-h). Furthermore, for short-term test–rest reliability of the FORWARD study questionnaire, the sub-study participants were asked to fill out a short version of the FORWARD study questionnaire 1–8 weeks after they completed the full version (Choi et al. 2014a).
Firefighters for the current study (330 firefighters)
Among the 365 firefighters who participated in the FORWARD study survey, we sequentially excluded the firefighters who were rookies (having <1 year of employment at the fire department) or who had special job titles (e.g., medical director, training officer, investigator) (N = 16), or who did not have valid information on blood pressure (N = 3), or who did not have valid information on the other study variables in the current study (N = 16). Thus, 330 (321 male and 9 female) firefighters were included in the current study. There were no substantial differences in age, gender, rank, race/ethnicity, education, and systolic and diastolic blood pressures between the 330 firefighters selected for this study and the 365 firefighters who originally participated in the FORWARD study.
Study outcome: blood pressure and hypertension
Firefighter resting blood pressures were measured by experienced nurses at the WEFIT clinic with an aneroid sphygmometer (Welch Allyn CE0050) based on a standard assessment protocol (5 min rest in a sitting position). Blood pressure (BP) was measured twice consecutively with a time interval of 1 min and averaged for analysis. Hypertension (HT) was defined as systolic blood pressure (SBP) ≥140 mmHg, ≥90 mmHg of diastolic blood pressure (DBP), or taking anti-hypertensive medication (Chobanian et al. 2003).
Main exposures: working conditions
Working conditions of the firefighters were measured with the FORWARD study questionnaire: number of 24-h shifts in the past month, number of calls on a typical 24-h shift, sedentary work, psychological job demands, job control, extrinsic effort at work, rewards, and physical job demands. On a typical 24-h shift (e.g. from 0800 to 0800), firefighters can sleep at night at the fire station, but frequently they can be woken for emergency calls. The standard shift schedule is 10–11 24-h shifts per month; however, many firefighters work voluntarily and involuntarily additional 24-h shifts beyond their standard work schedule (Choi et al. 2014b). Number of 24-h shifts in the past month (including overtime, backfill and/or shift trade) was measured with one item each. The reference group was those who reported 8–11 shifts in the past month with consideration of the standard work schedule (10–11 shifts per month) and the possibility of missing up to 2 shifts due to urgent non-duty issues. Among the 30 firefighters in the reference group, 1 firefighter reported 8 shifts and 3 firefighters reported 9 shifts in the past month. The 17 firefighters who reported 0–6 shifts in the past month were those who worked at headquarters (N = 4), or those who worked at fire stations (N = 13) and had just returned to work after a long break or an occupational injury. Sedentary work was measured with the single item (“My job often requires sitting for long periods of time.”) with the four-point Likert response set (strongly disagree to strongly agree) drawn from the MIDUS II study (Choi et al. 2010; Ryff et al. 2007). The number of calls on a typical 24-h shift was measured with a single question and divided into three groups (low, medium, and high) based on tertiles for analyses (see Table 1).
Table 1.
Distributions of blood pressure and hypertension among 330 (321 males and 9 females) professional firefighters
| Systolic blood pressure (mmHg)
|
Diastolic blood pressure (mmHg)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | <120 [% (N)] |
120–139 [% (N)] |
140–159 [% (N)] |
160–168 [% (N)] |
Mean (SD) | <80 [% (N)] |
80–89 [% (N)] |
90–99 [% (N)] |
100–101 [% (N)] |
|
| Total (N = 330, 100 %) | 111.9 (11.8) | 75.5 (249) | 21.8 (72) | 2.4 (8) | 0.3 (1) | 75.8 (7.6) | 60.6 (200) | 34.8 (115) | 3.6 (12) | 0.9 (3) |
| Non-hypertensive (N = 294, 89.1 %) | 110.0***a (9.6) | 81.6 (240) | 18.4 (54) | 74.7***a (6.7) | 66.3 (195) | 33.7 (99) | ||||
| Hypertensive (N = 36, 10.9 %) | 127.6***a (16.1) | 25.0 (9) | 50.0 (18) | 22.2 (8) | 2.8 (1) | 85.0***a (8.9) | 13.9 (5) | 44.4 (16) | 33.3 (12) | 8.3 (3) |
| Taking anti-hypertensive medications? | ||||||||||
| Yes (N = 24, 6.7 %) | 121.0***b (12.9) | 37.5 (9) | 54.2 (13) | 8.3 (2) | 81.3***b (7.9) | 20.8 (5) | 58.3 (14) | 20.8 (5) | ||
| No (N = 12, 3.6 %) | 140.7***b (13.8) | 41.7 (5) | 50.0 (6) | 8.3 (1) | 92.3***b (5.8) | 16.7 (2) | 58.3 (7) | 25.0 (3) | ||
All female firefighters were non-hypertensive
p < 0.01 at ANOVA test between non-hypertensives and hypertensives
p < 0.01 at ANOVA test between anti-hypertensive medication takers and non-takers
Job control (5 items), psychological job demands (5 items), physical job demands (1 item), extrinsic effort (2 items), and reward (4 items) were measured with the standard items of the Job Content Questionnaire (JCQ) (Karasek et al. 1985) and the Effort–Reward Imbalance Questionnaire (ERIQ) (Siegrist et al. 2004). Generally, the firefighters reported high job control, high psychological job demands, high physical job demand, high extrinsic effort, and high job reward (Choi et al. 2014a). There was little variation in the responses of the firefighters to each of the JCQ and ERIQ items (Choi et al. 2014a). However, there were four items showing some response variation (i.e., >20 % of agree/strongly agree or disagree/strongly disagree): 1 JCQ job control (“lot of say”) and 2 JCQ psychological job demands items (“not asked to do an excessive amount of work” and “conflicting demands”) and 1 ERIQ extrinsic effort item (“Over the past years, my job has become more and more demanding,” hereafter called “more demanding job over the past years”). Thus, the analyses were conducted with the 4 (3 JCQ and 1 ERIQ) items showing some response variation at the item level as well as with the scales; job control, psychological job demands, and job strain (the combination of low job control and high psychological job demands using the median cut-points), extrinsic effort, reward, and effort–reward imbalance (the combination of high effort and low rewards using the median cut-points). Physical demand (“My job requires lots of physical effort”) was also included in analyses, although 95.7 % of the firefighters agreed or strongly agreed to the questionnaire item.
The responses of firefighters to the questionnaire items of the aforementioned working conditions were stable during 1–8 weeks (Choi et al. 2014a, 2016a) or were validated against objective measures (sitting time from physical activity monitors or administrative call records of the fire department) (Choi et al. 2016a).
Health-related behaviors at work and during the leisure time
Exercise (i.e., moderate or vigorous level of physical activity for more than 30 min) at fire station (1 item) or during leisure time (1 item), consumption of high-fiber fruits and vegetables (1 item), smoking or using tobacco products (1 item), sleep hours at fire station (1 item), and sleep hours at home (1 item) were measured with the FORWARD study questionnaire. Detailed information about these items was described in our previous study (Choi et al. 2016b). The information on the use of anti-hypertensive medications and alcohol consumption was extracted by the research team staff from firefighters’ WEFIT medical examination records. Since the proportion of heavy alcohol drinkers (>2 drinks per day) was very low (<3 %), they were grouped together with the moderate alcohol drinkers for the multivariate analyses (see below).
Mental health and obesity
Mental health was measured with the standard 12-item General Health Questionnaire (GHQ) (Goldberg 1972). The GHQ items were scored according to the 0-1-2-3 scoring formula. The high- and low-psychological-distress groups were defined using the median of the GHQ scores. Post-traumatic syndrome (PTSD) was measured with the standard four items (Prins et al. 2003), and cases were defined as firefighters who agreed on all or three out of the four items. Kales et al. (2009) listed PTSD as a possible risk factor for hypertension among emergency respondents, including firefighters. The adiposity of the firefighters was assessed by an experienced exercise physiologist during their WEFIT medical examinations using three different measures, including body mass index (BMI), waist circumference (WC), and body fat percent (BFP) (Choi et al. 2016b). In the current study, the results of BMI were very similar to those using WC and BFP. Thus, only the results with BMI are presented here. In our previous study (Choi et al. 2016a), the number of 24-h shifts in the past month was associated with all three adiposity measures.
Other variables
Age, race/ethnicity (whites and non-whites), education, job title, and worksite (fire station and headquarters) were measured with questions in the FORWARD survey questionnaire. For the multivariate analyses, job title was simplified into two groups based on similar rank and tasks (firefighters/firefighter apparatus engineers and captains/chiefs).
Statistical analyses
We examined first the distributions of BP and HT among the firefighters. The univariate associations of the study variables, including working conditions, with BP and HT were examined by analysis of variance (ANOVA) and Chi-squared test, respectively, in the whole sample of firefighters (N = 330). These univariate analyses were replicated by gender, the use of anti-hypertensive medication, and the worksite, due to the protective effect of estrogen against hypertension in premenopausal women (Maas and Franke 2009) and the influence of anti-hypertensive medication on BP (Mackenzie et al. 2009). In addition, four firefighters who worked at headquarters and did not typically work a 24-h schedule were older (on average, 6 years) than firefighters working at a fire station and were all captains or chiefs.
The multivariate analyses for BP were conducted in a subsample of male firefighters (N = 294) who worked at a fire station and were not taking anti-hypertensive medication. Due to the small sample sizes of female firefighters (N = 9), firefighters working at headquarters (N = 4), and firefighters who worked at a fire station and were taking anti-hypertensive medication (N = 22), they were excluded from the multivariate analyses for BP. Only the variables that were at least marginally (p < 0.20) significant risk factors for SBP and DBP in the univariate analyses were considered in the multivariate analyses. The working condition variables, if significant in the univariate analyses, were examined in relation to SBP and DBP using the following multivariate models: after adjustment for the other psychosocial working conditions and sociodemographic variables (Model 1) and additionally after adjustment for health-related behaviors, sleep, mental health variables, and BMI (Model 2). The second adjustment procedure was to see any mediation effects of health-related behaviors, sleep, mental health variables, and BMI on the associations between psychosocial working conditions and BP (Ohlander et al. 2015). The final multivariate models for Model 1 and Model 2 were determined with the four indicators (R square, sum of squares for error, estimated error variance, and Mallows’s Cp) about the explanatory power and parsimoniousness of the competing multivariate models (Kleinbaum et al. 1998, pp 390–392). Analysis of covariance (ANCOVA) was used for the multivariate analyses with BP, and if necessary, subsequently pairwise comparisons (Rothman 1990) were conducted.
The multivariate analyses for HT were conducted in the 317 male firefighters at fire stations (excluding 9 female firefighters and 4 male firefighters working at headquarters) with Cox’s proportional hazards models (Breslow 1974; Lee and Chia 1993) including the variables that were significant in the univariate analyses.
Results
Distributions of SBP, DBP, and HT
Among the 330 firefighters, the means of SBP and DBP were 111.9 ± 11.8 and 75.8 ± 7.6 mmHg, respectively (Table 1). Thirty-six male firefighters (10.9 %) had hypertension. Among those with hypertension, two-thirds were taking anti-hypertensive medication, while a third were not taking anti-hypertensive medication. Fifty percent of the 36 firefighters with hypertension had uncontrolled blood pressures (≥140 mmHg for systolic blood pressure or ≥90 mmHg for diastolic blood pressure): 12 firefighters with hypertension were not taking anti-hypertensive medication, and 6 firefighters with hypertension were taking anti-hypertensive medication. However, most of the firefighters with uncontrolled blood pressure had mild hypertension (140–159 mmHg for SBP and 90–99 mmHg for DBP). There was a significant difference in SBP and DBP between those firefighters with and without hypertension and also between firefighters who were and were not taking medications for hypertension (Table 1).
The univariate associations of the study variables with SBP and DBP among 330 firefighters
The detailed distributions of the study variables among the 330 firefighters are presented in Table 2. The mean ages of 321 male and 9 female firefighters were 42.0 ± 8.6 and 37.8 ± 7.9 years, respectively. Most firefighters are white, have some college or were high school graduates, firefighters/engineers, and worked at fire stations.
Table 2.
Distributions of study variables, systolic and diastolic blood pressures, and hypertension in 330 (321 males and 9 females) professional firefighters
| Study variables | Category | Subcategory | % (N = 330) | Systolic BP, mm Hg: M (SD) |
Diastolic BP, mm Hg: M (SD) |
Hypertension (%) |
|---|---|---|---|---|---|---|
| Sociodemographic | Age | 25–34 | 25.2 | 109.6 (9.8)*** | 73.0 (7.1)*** | 1.2*** |
| 35–44 | 31.8 | 110.4 (10.3)*** | 75.5 (7.1)*** | 6.7*** | ||
| 45–54 | 37.0 | 113.8 (13.5)*** | 77.5 (7.8)*** | 17.2*** | ||
| 55–61 | 6.1 | 117.2 (13.2)*** | 79.6 (7.7)*** | 35.0*** | ||
| Sex | Men | 97.3 | 112.2 (11.8)*** | 76.0 (7.6)** | 11.2***a | |
| Women | 2.7 | 100.0 (5.2)*** | 70.6 (7.9)** | 0.0***a | ||
| Race/ethnicity | Non-Hispanic white | 81.5 | 112.1 (12.2) | 76.3 (7.5) | 12.3* | |
| Hispanic/Asian/others | 18.5 | 110.8 (10.2) | 75.7 (7.7) | 4.9* | ||
| Marital status | Married or living with | 78.2 | 112.0 (11.3) | 76.0 (7.6) | 10.9 | |
| partner | ||||||
| Others | 21.8 | 111.4 (13.6) | 75.4 (7.8) | 11.1 | ||
| Education | Some college or high school | 52.7 | 113.4 (11.8)** | 76.1 (7.0) | 12.6 | |
| College or Graduate school | 47.3 | 110.2 (11.7)** | 75.5 (8.3) | 9.0 | ||
| Job title | Firefighters/Engineers | 69.7 | 111.7 (11.7) | 75.5 (7.8) | 7.4*** | |
| Captains/Chiefs | 30.3 | 112.2 (12.2) | 76.7 (7.3) | 19.0*** | ||
| Worksite | Fire station | 98.8 | 111.7 (11.8)* | 75.8 (7.7) | 10.4** | |
| Headquarters | 1.2 | 121.3 (16.2)* | 77.0 (8.2) | 50.0** | ||
| Psychosocial working conditions | Number of 24-h shifts in the past month | 0–6 | 5.2 | 115.6 (11.02)* | 77.3 (5.7)* | 17.6 |
| 8–11 | 9.1 | 108.2 (7.3)* | 73.4 (7.6)* | 13.3 | ||
| 12–21 | 85.8 | 112.0 (12.2)* | 76.0 (7.7)* | 10.2 | ||
| 0–6 | 5.2 | 115.6 (11.02) | 77.3 (5.7) | 17.6 | ||
| 8–11 | 9.1 | 108.2 (7.3) | 73.4 (7.5)* | 13.3 | ||
| 12 | 21.5 | 111.2 (13.9) | 76.1 (8.5)* | 11.3 | ||
| 13 | 12.4 | 111.7 (11.6) | 76.0 (8.3)* | 17.1 | ||
| 14 | 23.3 | 113.5 (13.0) | 76.3 (7.2)* | 11.7 | ||
| 15 | 11.2 | 110.8 (11.1) | 73.3 (6.9)* | 2.7 | ||
| 16 | 10.6 | 113.1 (11.0) | 78.3 (8.5)* | 5.7 | ||
| 17–21 | 6.7 | 110.5 (8.0) | 76.0 (4.4)* | 9.1 | ||
| Sedentary work | Strongly disagree | 8.2 | 112.9 (14.8) | 76.0 (9.1) | 7.4 | |
| Disagree | 54.8 | 111.0 (10.9) | 75.3 (7.4) | 9.4 | ||
| Agree | 27.3 | 113.4 (12.8) | 76.4 (7.6) | 14.4 | ||
| Strongly agree | 9.7 | 111.8 (11.4) | 77.2 (7.9) | 11.1 | ||
| Number of calls on a typical 24-h shift | 0–4 | 28.5 | 111.8 (13.2) | 76.3 (8.6) | 22.3*** | |
| 5–7 | 38.8 | 112.6 (12.5) | 75.8 (7.6) | 7.8*** | ||
| 8–14 | 32.7 | 111.1 (9.6) | 75.5 (6.9) | 4.6*** | ||
| More demanding job over the past years | Strongly disagree/disagree | 30.9 | 110.2 (10.4)* | 75.3 (6.8) | 10.8 | |
| Agree/strongly agree | 69.1 | 112.6 (12.4)* | 76.1 (8.0) | 11.0 | ||
| Health-related behaviors | Exercise at work | ≥2 days/week | 87.9 | 111.7 (11.9) | 75.6 (7.7)* | 10.0* |
| ≤ 1 day/week | 12.1 | 112.8 (11.4) | 77.6 (7.2)* | 17.5* | ||
| Exercise during leisure time | ≥2 days/week | 73.6 | 111.6 (11.3) | 75.4 (7.5)* | 8.6** | |
| ≤1 day/week | 26.4 | 112.6 (13.2) | 77.2 (7.9)* | 17.2** | ||
| High-fiber fruits/vegetable consumption | High (5–6 servings/day) | 13.3 | 109.0 (12.4)* | 73.5 (7.6)** | 4.5* | |
| Low (0–4 servings/day) | 86.7 | 112.3 (11.7)* | 76.2 (7.6)** | 11.9* | ||
| Smoking/users of tobacco products | Current smokers/users | 10.0 | 113.1 (11.2) | 78.1 (7.9)* | 15.2 | |
| Ex-smokers/users | 25.5 | 112.8 (11.4) | 76.6 (7.5)* | 13.1 | ||
| Never-smokers/users | 64.5 | 111.3 (12.1) | 75.2 (7.6)* | 9.4 | ||
| Alcohol consumption | No | 13.3 | 111.0 (10.7) | 76.3 (6.9) | 6.8 | |
| Moderate/Heavyb | 86.7b | 112.0 (12.0) | 75.8 (7.8) | 11.5 | ||
| Antihypertensive medication | No | 92.7 | 111.2 (11.5)*** | 75.4 (7.5)*** | 3.9*** | |
| Yes | 7.3 | 121.0 (12.9)*** | 81.3 (7.8)*** | 100.0*** | ||
| Sleep and health | Sleep hours at fire station | 2.5 to <5 h | 15.8 | 110.9 (9.9) | 75.4 (7.0) | 1.9*** |
| 5 or 6 h | 61.2 | 111.9 (12.2) | 75.6 (7.9) | 9.9*** | ||
| >6 to 8.5 hc | 23.0 | 112.4 (12.2) | 76.9 (7.3) | 19.7*** | ||
| Sleep hours at home | 4 to <7 h | 17.8 | 113.4 (13.0) | 76.6 (8.1) | 21.1** | |
| 7 or 8 h | 72.6 | 111.9 (11.8) | 75.7 (7.4) | 8.6** | ||
| >8 to 10 h | 9.7 | 110.2 (10.7) | 75.2 (8.7) | 9.7** | ||
| Psychological distress | Low (0–9) | 56.4 | 112.4 (12.6) | 75.7 (8.2) | 13.6* | |
| High (10–28) | 43.6 | 111.3 (10.9) | 76.1 (6.9) | 7.7* | ||
| PTSD | No | 94.2 | 111.8 (11.8) | 75.9 (7.7) | 10.9 | |
| Yes | 5.8 | 113.6 (12.8) | 75.2 (6.5) | 10.5 | ||
| Obesity | <30 kg/m2 | 77.6 | 110.6 (11.6)*** | 74.9 (7.5)*** | 8.6** | |
| ≥30 kg/m2 | 22.4 | 116.4 (11.5)*** | 79.0 (7.3)*** | 18.9** |
p < 0.20,
p < 0.05, and
p < 0.01 at analysis of variance (ANOVA) test for blood pressure and Chi-square test for hypertension
Based on the significance test of a gamma coefficient
The percent of heavy drinkers (2.1 %) were included
1 firefighter reported 10 h of sleep
As expected, both SBP and DBP were significantly higher in older firefighters, male firefighters, firefighters taking anti-hypertensive medication, and obese firefighters (Table 2). SBP was significantly higher in firefighters having some college or high school education, and firefighters working at the headquarters (who were older and captains/chiefs). DBP was significantly lower in the firefighters reporting 5–6 servings of high-fiber fruits and vegetables per day compared to those reporting fewer servings of high-fiber fruits and vegetables per day. Less exercise at work and during leisure time, and smoking/using tobacco products were marginally (p < 0.20) associated with DBP, while they were not associated with SBP. Sleep hours at the fire station and at home, psychological distress, and PTSD were not associated with BP.
BP did not vary much by sedentary work and number of calls on a typical 24-h shift (Table 2). Also it did not change much by job strain, job control, psychological job demands, the 3 JCQ items showing some response variation, effort, reward, effort–reward imbalance, and physical demands (not shown here).
However, BP was higher in the firefighters who reported 12–21 shifts or 0–6 shifts (which included four firefighters who worked at headquarters and thirteen firefighters who worked at fire stations) than in those who reported the standard work schedule (8–11 shifts) in the past month (Table 2). When we restricted the analysis to the 295 male firefighters who worked at fire stations and were not taking anti-hypertensive medication (Table 3A), there were a marginally significant difference in SBP (p = 0.095) and a significant difference in DBP (p = 0.038) among the firefighters by the number of 24-h shifts in the past month. Interestingly, both SBP and DBP were higher in the firefighters who reported 0–6 shifts in the past month than in those who reported 8–11 shifts or 12–21 shifts in the past month. In addition, compared to the standard work schedule group, two subgroups of the 12–21 shifts group (14 shift and 16 shifts groups) had significantly higher blood pressure: 4.9–5.6 mmHg for SBP and 4.2–6.7 mmHg for DBP (Table 3A; Fig. 1). Among the 22 male firefighters who worked at fire stations and were taking anti-hypertensive medication, SBP and DBP were also greater in the firefighters who reported 12–21 shifts than in those who reported 8–11 shifts in the past month. However, the differences in DBP by the number of 24-h shifts in the past month were much smaller in the 22 male firefighters who worked at fire stations and were taking anti-hypertensive medication than in the 295 male firefighters who worked at fire stations and were not taking anti-hypertensive medication.
Table 3.
Distributions of psychosocial working conditions, systolic and diastolic blood pressures, and hypertension in (A) 295 male firefighters who worked at fire stations and were not taking anti-hypertensive medications and (B) 22 male firefighters who worked at fire station and were taking anti-hypertensive medications
| Psychosocial working condition | Subcategory | N (%) | SBP (mmHg)
|
DBP (mmHg)
|
Hypertension (%) | ||
|---|---|---|---|---|---|---|---|
| M (SD) | Pairwise comparison (p value) | M (SD) | Pairwise comparison (p value) | ||||
| (A) 295 male firefighters | |||||||
| 0–6 | 11 (3.7) | 114.5 (8.6) | 0.069 | 77.0 (5.4) | 0.062 | 0.0 | |
| Number of 24-h shifts in the past month | 8–11 (reference) | 25 (8.5) | 107.1 (6.3) | Ref. | 72.0 (6.1) | Ref. | 0.0 |
| 12–21 | 259 (87.8) | 111.7 (11.7) | 0.050 | 75.8 (7.5) | 0.014 | 4.6 | |
| ANOVA test: p value | 0.095 | 0.038 | |||||
| 0–6 | 11 (3.7) | 114.5 (8.6) | 0.070 | 77.0 (5.4) | 0.060 | 0.0 | |
| 8–11 | 25 (8.5) | 107.9 (6.3) | Ref. | 72.0 (6.1) | Ref. | 0.0 | |
| 12 | 63 (21.4) | 110.9 (13.6) | 0.155 | 75.8 (8.4) | 0.029 | 4.8 | |
| 13 | 36 (12.2) | 110.8 (10.9) | 0.215 | 74.8 (8.0) | 0.150 | 5.6 | |
| 14 | 71 (24.1) | 112.8 (12.3) | 0.031 | 76.2 (7.0) | 0.015 | 5.6 | |
| 15 | 36 (12.2) | 111.4 (10.8) | 0.148 | 73.6 (6.7) | 0.398 | 2.8 | |
| 16 | 34 (11.5) | 113.5 (11.0) | 0.033 | 78.7 (8.3) | 0.001 | 5.9 | |
| 17–21 | 19 (6.4) | 110.1 (7.5) | 0.382 | 75.8 (4.3) | 0.090 | 0.0 | |
| ANOVA test: p value | 0.414 | 0.026 | |||||
| More demanding over the past years | Strongly disagree/disagree | 93 (31.5) | 109.6 (10.1) | Ref. | 74.8 (6.6) | Ref. | 4.3 |
| Agree/strongly agree | 202 (68.5) | 112.3 (11.8) | 0.059 | 75.9 (7.8) | 0.225 | 4.0 | |
| (B) 22 male firefighters | |||||||
| Number of 24-h shifts in the past month | 0–6 | 1 (4.5) | 121.0 (NA) | 0.826 | 80.0 (NA) | 0.978 | 100 |
| 8–11 (reference) | 4 (18.2) | 117.5 (7.5) | Ref. | 80.3 (12.7) | Ref. | 100 | |
| 12–21 | 17 (77.3) | 121.4 (15.0) | 0.622 | 82.1 (7.0) | 0.694 | 100 | |
| ANOVA test: p value | 0.883 | 0.905 | |||||
| More demanding over the past years | Strongly disagree/disagree | 7 (31.8) | 121.0 (8.1) | Ref. | 80.9 (8.4) | Ref. | 100 |
| Agree/strongly agree | 15 (68.2) | 120.5 (15.6) | 0.942 | 82.0 (7.8) | 0.757 | 100 | |
ANOVA analysis of variance, NA not applicable, Ref. the reference group for pairwise comparisons
Fig. 1.
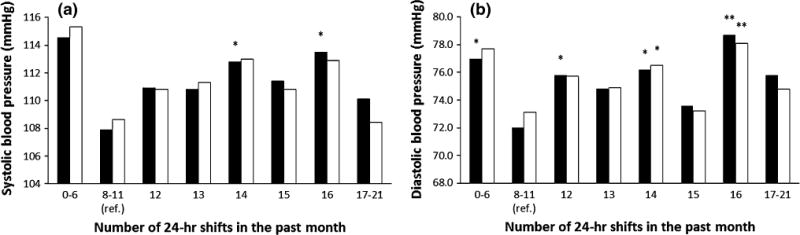
Associations of the number of 24-h shifts in the past month with systolic blood pressure (a) and diastolic blood pressure (b) in 295 male firefighters who worked at fire stations and were not taking anti-hypertensive medication (the reference group: 8–11 shifts). The black bars indicate the results from the univariate analysis, and the white bars indicate the results from the multivariate analysis after controlling for age, education, more demanding job over the past years, and body mass index. *p < 0.05 and **p < 0.01
With regard to the ERIQ item (“more demanding job over the past years), SBP was 2.6 mmHg higher (p = 0.059) in the firefighters who agreed or strongly agreed to the item than in those who disagreed or strongly disagreed among the 295 male firefighters (Table 3A). However, SBP did not differ by the ERIQ item among the 22 male firefighters who worked at fire stations and were taking anti-hypertensive medication (Table 3B). DBP was higher in the firefighters who agreed or strongly agreed to the item than in those who disagreed or strongly disagreed to the item in both the 295 male and 22 male firefighters (Table 3A, B), but the difference was marginal.
In the 9 female firefighters, there was no significant change in BP by the number of 24-h shifts in the past month or the ERIQ item (“more demanding job over the past years).
Multivariate associations with SBP and DBP among the 295 male firefighters
Age, education, the number of 24-h shifts in the past month, and the ERIQ item were included in the final Model 1. Age, education, the number of 24-h shifts in the past month, the ERIQ item, and BMI were included in the final Model 2. Although exercise at work and during leisure time, consumption of high-fiber fruits and vegetables, and smoking were at least marginally significant in the univariate analyses, they turned out to be insignificant in the multivariate model (an alternative model of the final Model 2) also including age, education, the number of 24-h shifts in the past month, the ERIQ item, and BMI. Also, the final Model 2 was more parsimonious than the alternative final Model 2, although their explanatory power was very comparable to each other. Thus, we chose the final Model 2 over the alternative final Model 2.
A similar pattern of BP by the number of 24-h shifts in the past month was observed in the 295 male firefighters who worked at fire stations and were not taking anti-hypertensive medication using analysis of covariance (ANCOVA) tests. Compared to the standard work schedule group, SBP was 3.0 mmHg (p = 0.20) and 6.6 mmHg (p = 0.10) higher in the 12–21 shifts and 0–6 shifts groups, respectively (Model 2 in Table 4). DBP was also 2.6 mmHg (p = 0.08) and 4.6 mmHg (p = 0.07) higher in the 12–21 shifts and 0–6 shifts groups, respectively. In the detailed multivariate analyses after dividing the 12–21 shifts group into the six subgroups, as in the univariate analyses, the two subgroups (14 shifts and 16 shifts) had substantially higher SBP and DBP than the standard work schedule group: 4.3–4.4 mmHg (p < 0.20) for SBP and 3.4–5.0 mm Hg (p < 0.05) for DBP (Table 4; Fig. 1a, b). BMI attenuated the association between the number of 24-h shifts in the past month and BP to some extent, particularly in the subgroup of firefighters who reported 17–21 shifts in the past month (Table 4).
Table 4.
Multivariate associations between number of 24-h shifts in the past month and more demanding over the past years with systolic and diastolic blood pressures in 295 male firefighters who worked at fire stations and were not taking anti-hypertensive medications
| Category | Subcategory | Systolic blood pressure (mm Hg)
|
Diastolic blood pressure (mm Hg)
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1: M (SE) | Pairwise comparison (p value) | Model 2: M (SE) | Pairwise comparison (p value) | Model 1: M (SE) | Pairwise comparison (p value) | Model 2: M (SE) | Pairwise comparison (p value) | ||
| Number of 24-h shifts in the past month | 0–6 | 114.9 (3.4) | 0.076 | 115.2 (3.3) | 0.099 | 77.5 (2.2) | 0.048 | 77.7 (2.1) | 0.068 |
| 8–11 (reference) | 107.7 (2.3) | Ref. | 108.6 (2.2) | Ref. | 72.3 (1.5) | Ref. | 73.1 (1.4) | Ref. | |
| 12–21 | 111.7 (0.7) | 0.092 | 111.6 (0.7) | 0.202 | 75.8 (0.4) | 0.022 | 75.7 (0.4) | 0.080 | |
| ANCOVA test: p values | 0.141 | 0.229 | 0.048 | 0.123 | |||||
| 0–6 | 115.0 (3.4) | 0.076 | 115.3 (3.3) | 0.099 | 77.5 (2.2) | 0.048 | 77.7 (2.1) | 0.068 | |
| 8–11 | 107.7 (2.3) | Ref. | 108.6 (2.2) | Ref. | 72.3 (1.4) | Ref. | 73.1 (1.4) | Ref. | |
| 12 | 110.5 (1.4) | 0.289 | 110.8 (1.4) | 0.418 | 75.5 (0.9) | 0.061 | 75.7 (0.9) | 0.118 | |
| 13 | 111.2 (1.9) | 0.227 | 111.3 (1.9) | 0.359 | 74.9 (1.2) | 0.165 | 74.9 (1.2) | 0.317 | |
| 14 | 112.9 (1.3) | 0.050 | 113.0 (1.3) | 0.091 | 76.3 (0.9) | 0.017 | 76.5 (0.8) | 0.041 | |
| 15 | 111.3 (1.9) | 0.227 | 110.8 (1.8) | 0.460 | 73.6 (1.2) | 0.495 | 73.2 (1.2) | 0.979 | |
| 16 | 113.4 (1.9) | 0.053 | 112.9 (1.9) | 0.147 | 78.5 (1.2) | 0.001 | 78.1 (1.2) | 0.008 | |
| 17–21 | 109.4 (2.6) | 0.619 | 108.4 (2.6) | 0.949 | 75.6 (1.7) | 0.128 | 74.8 (1.6) | 0.446 | |
| ANCOVA test: p values | 0.422 | 0.458 | 0.031 | 0.044 | |||||
| More demanding job over the past years | Strongly disagree/disagree | 109.6 (1.2) | Ref. | 109.2 (1.2) | Ref. | 74.8 (0.8) | Ref. | 74.8 (0.7) | Ref. |
| Agree/strongly agree | 112.3 (0.8) | 0.058 | 112.3 (0.8) | 0.059 | 75.9 (0.5) | 0.229 | 75.9 (0.5) | 0.235 | |
Model 1: after controlling for age, education, and more demanding job over the past years (for the analysis of the number of 24-h shifts in the past month) or more demanding over the past years (for the analysis of more demanding job over the past years). Model 2: Model 1 plus additionally after controlling for body mass index
M mean, SE standard error, ANCOVA analysis of covariance, Ref. the reference group for pairwise comparisons
In the multivariate analyses as in the univariate analyses, SBP was 3.1 mmHg higher (p = 0.06) in the firefighters who agreed or strongly agreed to the ERIQ item (“more demanding job over the past years) than in those who disagreed or strongly disagreed among the 295 male firefighters (Table 4). A similar pattern was observed for DBP, but the difference (1.1 mmHg) was small (p = 0.24). Overall, BMI did not affect the association between the ERIQ item and blood pressure.
In the final multivariate model (Model 2 in Table 4), among the aforementioned covariates, only age and BMI were significant (p < 0.01) risk factors for SBP and DBP. None of the health-related behaviors in the final model were associated with SBP or DBP.
Univariate associations of working condition variables with HT among the 330 firefighters
Hypertension was significantly more prevalent in the firefighters who reported 0–4 calls per shift than in those who reported 5–7 calls per shift and 8–14 calls per shift (22.3 vs. 7.8 and 4.6 %, respectively). It was also more prevalent in captains and chiefs than in firefighters and engineers. Two out of the 4 (50 %) firefighters working at headquarters were hypertensive, while the prevalence of hypertension was 10.4 % among the 326 firefighters who worked at fire stations.
However, the number of 24-h shifts in the past month was not associated with hypertension, although hypertension was more prevalent in the 0–6 shifts in the past month than in the standard work schedule group (Table 2). Neither the ERIQ item (“more demanding job over the past years”), nor sedentary work was associated with hypertension. The other working conditions (job strain, job control, psychological job demands, the 3 JCQ items showing some response variation, effort, reward, effort–reward imbalance, and physical demands) was not associated with hypertension (not shown here).
Age, sex, race/ethnicity, exercise at work and during leisure time, consumption of high-fiber fruits and vegetables, use of anti-hypertensive medication, sleep hours at fire station and at home, psychological distress, and obesity were at least marginally (p < 0.20) associated with hypertension in the univariate analyses (Table 2).
Multivariate associations of working condition variables with HT among 317 male firefighters
The prevalence ratio of the firefighters who reported 0–4 calls on a typical 24-h shifts for hypertension was 2.39 (95 % confidence interval 0.68–8.40, p = 0.17), compared to those who reported 8–14 calls per shift, in the multivariate Cox proportional hazards model (after controlling for age, race/ethnicity, exercise at work and during leisure time, consumption of high-fiber fruits and vegetables, sleep hours at fire station and at home, the GHQ scores, and BMI) among the 317 male firefighters who worked at a fire station. Age was the only significant risk factor for hypertension in the multivariate analyses among the 317 male firefighters. In particular, the differences in the prevalence of HT by job title, number of calls on a typical 24-h shift, and sleep hours at home appeared to be nonsignificant (p > 0.20) after controlling for age.
Discussion
To the best of our knowledge, this is the first epidemiological study that examines multiple physical and psychosocial working conditions (number of 24-h shifts, number of calls, sedentary work, job strain, effort–reward imbalance, and physical demands) among professional firefighters in relation to clinical BP and HT. The prevalence of hypertension was about 11 %. Half of the firefighters with hypertension had uncontrolled high BP. None of the working conditions were identified as a significant risk factor for HT in the current study, although hypertension was more prevalent in male, older, and high-rank firefighters and firefighter who reported low numbers of daily calls. Increased job demands over the past years and additional 24-h shifts in the past month were associated with increased SBP and DBP, respectively, in the male firefighters who were normotensive or hypertensive without taking medication. Adiposity (BMI) attenuated the associations between number of 24-h shifts and DBP to some extent. Other working conditions (number of calls, sedentary work, job strain, effort–reward imbalance, and physical demands) were not associated with BP or HT in the current study. This study indicates that firefighter stakeholders should make continuous efforts to achieve and maintain an optimal level of firefighter collective and individual workload. Also this study suggests that hypertension management needs to be further improved among hypertensive firefighters.
This study empirically supports that additional 24-h shifts may increase the risk of blood pressure among professional firefighters, which is in line with the proposition of Kales et al. (2009). This is also consistent with the previous studies in non-firefighter working populations (Hayashi et al. 1996; Kubo et al. 2013; Nakamura et al. 2012; Ohira et al. 2000; Souza et al. 2015; Su et al. 2008; Suwazono et al. 2008). However, this study is very unique in demonstrating that long work hours/overtime is an independent significant risk factor among 24-h shift workers, after adjustment for multiple other occupational risk factors (job strain, effort–reward imbalance, and physical demands), which has been unclear (Gilbert-Ouimet et al. 2014; Peter et al. 1999; Virkkunen et al. 2007). Most studies on shift work and BP was a comparison of shift workers with non-shift (daytime) workers (Kubo et al. 2013; Ohira et al. 2000; Suwazono et al. 2008). The studies on long work hours and BP (Hayashi et al. 1996; Nakamura et al. 2012) were a comparison among daytime workers. Also, none of the studies on shift work or long work hours/overtime considered other occupational risk factors (job strain, effort–reward imbalance, and physical demands) in analyses.
On the other hand, several previous studies (Gholami Fesharaki et al. 2014; Knutsson et al. 1988; Murata et al. 1999; Puttonen et al. 2009; Sfreddo et al. 2010) did not support the association between shift work and BP. However, some methodological weaknesses in the studies need to be considered. Most of the studies (Gholami Fesharaki et al. 2014; Knutsson et al. 1988; Puttonen et al. 2009; Sfreddo et al. 2010) were cross-sectional studies, which are more vulnerable to a healthy worker effect (e.g., healthier workers recruited to shift work, switched to non-shift work over time, or retired) than longitudinal studies. Also none of the studies considered the use of anti-hypertensive medication in analyses, which could significantly underestimate the association between shift work and BP. Although Murata et al. (1999) reported no significant association between shift work and BP in a longitudinal study on a relatively small sample of workers (N < 200), SBP increase over 10 years was 4 mmHg greater in shift workers without hypertension than in daytime workers without hypertension.
The association between number of 24-h shifts and DBP in the current study did not appear to be mediated by health-related behaviors (eating, exercise, and sleep hours), psychological distress, and PTSD. However, BMI (and other adiposity measures) attenuated the association between number of 24-h shifts and BP to some extent, particularly in the firefighters who reported 17–21 shifts in the past month in the current study. It is similar to the study by Ohlander et al. (2015) in German autoworkers where the impact of shift work without nights (vs. day shifts) on hypertension was significantly mediated by BMI and physical inactivity. However, the significant associations of 14 and 16 shifts in the past month with DBP, after adjustment for BMI, points to another possible mechanism by which many additional 24-h shifts may increase DBP in professional firefighters: frequent circadian misalignment. Mean arterial blood pressure was 3 mmHg higher during circadian misalignment than during circadian alignment in an experimental study with 10 human subjects (Scheer et al. 2009). Scheer et al. (2009) suggested that circadian misalignment may increase mean arterial blood pressure by increasing total peripheral resistance, cardiac output, or blood volume.
However, in the current study, there was no significant association between number of 24-h shifts and HT. This finding needs to be interpreted carefully because this cross-sectional study is limited in being able to capture all possible changes that a hypertensive firefighter makes to reduce the detrimental impact of many additional 24-h shifts on his/her cardiovascular health: reducing additional 24-h shifts, taking a long break or sick leave (hypertension of a firefighter is covered by the firefighter presumptive disability law in many US states, including California) (Kales et al. 2009), changing their worksite (e.g. to headquarters), or retiring earlier if the status of hypertension is highly uncontrollable (>180 mmHg for SBP and >100 mmHg for DBP) (National Fire Protection Association 2007). In fact, the findings of the current study support some of those possibilities. First, the prevalence of hypertension appeared to be higher in the firefighters who worked at fire stations and reported 0–6 shifts in the past month, compared to those who reported standard work schedule or 12–21 shifts in the past month. The firefighters who worked at fire stations and reported 0–6 shifts in the past month just returned to work after a long break or sick leave at the time of the FORWARD study survey. Most of the firefighters would have worked additional 24-h shifts in the following months given that most firefighters in the current fire department do additional 24-h shifts. We observed anecdotally in another recent study with a group of firefighters from the same fire department (Choi 2015) that one firefighter reported 4 shifts in the past month and then reported 14-shifts in the following month when the same questionnaire item was administered again. Second, the prevalence of hypertension was higher in the firefighters who worked at headquarters than in who worked at a fire station. Firefighters who initially worked at fire stations doing a 24-h shift schedule, including additional shifts, might later choose to work at headquarters and quit working a 24-h shift schedule. Future longitudinal studies are needed to clarify the association between number of 24-h shifts and hypertension in firefighters.
Our finding of an association between increased job demands over the past years and SBP in the current study is also unique. We could not find any comparable studies that have examined the effect of increased job demands over the past years (assessed with one ERIQ effort item) on clinical blood pressure, although Ohlin et al. (2007) reported that high job demands at baseline (assessed with the JCQ psychological job demand scale) was longitudinally associated with increased BP in a Swedish working population. The ERI effort item may reflect the intensified job demands in the majority of the firefighters in the current study during the FORWARD study period. There was a substantial delay in hiring and training new firefighters to replace older retiring firefighters during the FORWARD study period partly due to insufficient financial resources in the fire department just after the global economic crisis in the late 2000s.
Physical demands, job strain, effort–reward imbalance, and sedentary work were not associated with BP or HT in the current study. It should be noted that there was little variation in physical demands, job strain, and effort–reward imbalance in our single occupation sample of firefighters, which is a prerequisite for examining them as the risk factors for BP or HT in an epidemiological study. The association between sedentary work and HT has not been supported in a recent longitudinal study (Saidj et al. 2015), although it could indirectly increase the risk of HT through obesity.
The prevalence of hypertension in our sample of Southern California firefighters was lower than that in a group of Massachusetts firefighters in the late 1990s (Soteriades et al. 2003): 11 vs. 20–24 %. But it was similar to that in a recent survey (Poston et al. 2013) in a larger sample of firefighters from 10 US fire departments across the nation with a good firefighter WEFIT program: 11 vs. 12 % (self-reported). The prevalence of uncontrolled hypertension was lower in the current study than in the study with Massachusetts firefighters in the late 1990s (Soteriades et al. 2003): 50 vs. 74 %. This may indicate that the overall cardiovascular health of US firefighters has improved over the two decades as the firefighter WEFIT program has spread across US fire departments.
Implications for prevention of hypertension among professional firefighters
The current study indicates that many additional 24-h shifts (e.g., 16 shifts in the past month) may significantly increase the risk of elevated blood pressure among professional firefighters, independent of health-related behaviors and adiposity. Our previous study also pointed to the increased risk of many additional 24-h shifts for obesity among firefighters (Choi et al. 2016a). Furthermore, several US firefighter fatality cases involved multiple consecutive 24-h shifts (National Institute for Occupational Safety and Health, 2008, 2011). All of these support introducing a limit to the number of 24-h shifts that a firefighter can work in a month or a year, which we expect will significantly improve the cardiovascular health of US professional firefighters. Recently, the fire department and the local firefighter union in the current study agreed on a firefighter workload policy limiting the number of annual voluntary 24-h shifts that a firefighter can work (equivalent to 15 shifts per month, on average) in order to share the burden of additional 24-h shifts more equally among the firefighters.
This study also suggests that intensified work over a couple of years may raise the level of blood pressure among firefighters. Firefighter stakeholders should make efforts to continuously maintain an optimal level of collective firefighter workforce. The fire department in the current study was able to complete the recruitment and training of new firefighters (firefighter academy) in November 2011 after the last one in July 2009.
The high prevalence of uncontrolled hypertension (50 %) among hypertensive firefighters deserves discussion. Most of the uncontrolled hypertensive firefighters were mild hypertensive and were not taking anti-hypertensive medication. Given the uncertainty of the benefits of pharmacological treatment of mild hypertension (Diao et al. 2012), we think that a priority to control hypertension (hypertension management) among the uncontrolled hypertensive firefighters should be given to non-pharmacological approaches such as avoiding many additional 24-h shifts and improving health-related behaviors, including weight management.
Limitations
This study has several limitations. First, this study is a cross-sectional study so we cannot be sure of the temporal relationships of the number of 24-h shifts in the past month and increased job demands over the past years with increased blood pressure. Future longitudinal studies are needed to clarify the temporal relationships among firefighters. Second, the information on numbers of 24-h shifts in the past month and increased job demands over the past years was self-reported, although its good short-term (1–8 weeks) test–retest reliability was confirmed in the FORWARD study (Choi et al. 2014a, 2016a). Using long-term administrative records of fire departments will improve the quality of exposure assessment in future research. Third, this study was not able to examine whether occupational noise exposure, one of the four possible occupational risk factors for hypertension in firefighters (Kales et al. 2009), is a risk factor for hypertension among firefighters. Firefighters can be exposed to a short-term, high level of noise during their emergency operations (e.g. sirens and using extraction equipment) (Neitzel et al. 2013). However, we observed during the current study that firefighters regularly wore headsets with a dual function of noise protection and internal communication on fire trucks and engines when they responded to calls. Also, there was no association between number of calls on a typical 24-h shift and blood pressure in the current study. Thus, we think that the impact of occupational noise exposure of firefighters on the results of the current study, if any, would not be substantial.
Acknowledgments
We express our sincere thanks to a fire department and a local union of the International Association of Fire Fighters (IAFF) in Southern California for their support and input in this study. The fire department and union had no decision-making role in the decision to publish study results or the content of the publication. This study was supported by the Centers for Disease Control and Prevention (CDC)/National Institute for Occupational Safety and Health (NIOSH) (Grant #, 5R21OH009911-02). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC/NIOSH.
Footnotes
Compliance with ethical standards
Conflict of interest: The authors declare that they have no conflict of interest.
References
- Breslow N. Covariance analysis of censored survival data. Biometrics. 1974;30(1):89–99. [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ, Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute. National High Blood Pressure Education Program Coordinating Committee Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Choi B. A worksite obesity intervention study in US firefighters: a participatory action research approach. Presented at the 31st international congress on occupational health; May 31 to June 5, 2015; Seoul, South Korea. 2015. [Google Scholar]
- Choi B, Schnall P, Yang H, Dobson M, Landsbergis P, Israel L, Karasek R, Baker D. Sedentary work, low physical job demand, and obesity in US workers. Am J Ind Med. 2010;53(11):1088–1101. doi: 10.1002/ajim.20886. [DOI] [PubMed] [Google Scholar]
- Choi B, Schnall P, Dobson M, Israel L, Landsbergis P, Galassetti P, Pontello A, Kojaku S, Baker D. Exploring occupational and behavioral risk factors for obesity in firefighters: a theoretical framework and study design. Saf Health Work. 2011;2(4):301–312. doi: 10.5491/SHAW.2011.2.4.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi B, Ko S, Dobson M, Schnall PL, Garcia-Rivas J, Israel L, Baker D. Short-term test–retest reliability of the Job Content Questionnaire and Effort-Reward Imbalance Questionnaire items and scales among professional firefighters. Ergonomics. 2014a;57(6):897–911. doi: 10.1080/00140139.2014.904008. [DOI] [PubMed] [Google Scholar]
- Choi B, Schnall PL, Dobson M, Garcia-Rivas J, Kim H, Zaldivar F, Israel L, Baker D. Very long (>48 hours) shifts and cardiovascular strain in firefighters: a theoretical framework. Ann Occup Environ Med. 2014b;26(1):5. doi: 10.1186/2052-4374-26-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi B, Dobson M, Schnall P, Garcia-Rivas J. 24-hour work shifts, sedentary work, and obesity in male firefighters. Am J Ind Med. 2016a;59(6):486–500. doi: 10.1002/ajim.22572. [DOI] [PubMed] [Google Scholar]
- Choi B, Steiss D, Garcia-Rivas J, Kojaku S, Schnall P, Dobson M, Baker D. Comparison of body mass index with waist circumference and skinfold-based percent body fat in firefighters: adiposity classification and associations with cardiovascular disease risk factors. Int Arch Occup Environ Health. 2016b;89(3):435–448. doi: 10.1007/s00420-015-1082-6. [DOI] [PubMed] [Google Scholar]
- Davila EP, Kuklina EV, Valderrama AL, Yoon PW, Rolle I, Nsubuga P. Prevalence, management, and control of hypertension among US workers: does occupation matter? J Occup Environ Med. 2012;54(9):1150–1156. doi: 10.1097/JOM.0b013e318256f675. [DOI] [PubMed] [Google Scholar]
- Diao D, Wright JM, Cundiff DK, Gueyffier F. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev. 2012;8:CD006742. doi: 10.1002/14651858.CD006742.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobson M, Choi B, Schnall PL, Wigger E, Garcia-Rivas J, Israel L, Baker DB. Exploring occupational and health behavioral causes of firefighter obesity: a qualitative study. Am J Ind Med. 2013;56(7):776–790. doi: 10.1002/ajim.22151. [DOI] [PubMed] [Google Scholar]
- Feairheller DL. Blood pressure and heart rate responses in volunteer firefighters while wearing personal protective equipment. Blood Press Monit. 2015;20(4):194–198. doi: 10.1097/MBP.0000000000000120. [DOI] [PubMed] [Google Scholar]
- Geibe JR, Holder J, Peeples L, Kinney AM, Burress JW, Kales SN. Predictors of on-duty coronary events in male firefighters in the United States. Am J Cardiol. 2008;101:585–589. doi: 10.1016/j.amjcard.2007.10.017. [DOI] [PubMed] [Google Scholar]
- Gholami Fesharaki M, Kazemnejad A, Zayeri F, Rowzati M, Akbari H. Historical cohort study of shift work and blood pressure. Occup Med. 2014;64(2):109–112. doi: 10.1093/occmed/kqt156. [DOI] [PubMed] [Google Scholar]
- Gilbert-Ouimet M, Trudel X, Brisson C, Milot A, Vézina M. Adverse effects of psychosocial work factors on blood pressure: systematic review of studies on demand-control-support and effort-reward imbalance models. Scand J Work Environ Health. 2014;40(2):109–132. doi: 10.5271/sjweh.3390. [DOI] [PubMed] [Google Scholar]
- Goldberg DP. The detection of psychiatric illness by questionnaire: a technique for the identification and assessment of nonpsychotic psychiatric illness. Oxford University Press; London: 1972. [Google Scholar]
- Hayashi T, Kobayashi Y, Yamaoka K, Yano E. Effect of overtime work on 24-hour ambulatory blood pressure. J Occup Environ Med. 1996;38(10):1007–1011. doi: 10.1097/00043764-199610000-00010. [DOI] [PubMed] [Google Scholar]
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- Kales SN, Soteriades ES, Christophi CA, Christiani DC. Emergency duties and deaths from heart disease among firefighters in the United States. N Engl J Med. 2007;356:1207–1215. doi: 10.1056/NEJMoa060357. [DOI] [PubMed] [Google Scholar]
- Kales SN, Tsismenakis AJ, Zhang C, Soteriades ES. Blood pressure in firefighters, police officers, and other emergency responders. Am J Hypertens. 2009;22:11–20. doi: 10.1038/ajh.2008.296. [DOI] [PubMed] [Google Scholar]
- Karasek RA, Gordon G, Pietrokovsky C, Frese M, Pieper C, Schwartz J. Job content questionnaire and user’s guide. University of Southern California/University of Massachusetts; Los Angeles (CA)/Lowell (MA): 1985. [Google Scholar]
- Kleinbaum DG, Kupper LL, Muller KE, Nizam A. Applied regression analysis and multivariate methods. Books/Cole; Pacific Grove: 1998. [Google Scholar]
- Knutsson A, Akerstedt T, Jonsson BG. Prevalence of risk factors for coronary artery disease among day and shift workers. Scand J Work Environ Health. 1988;14(5):317–321. doi: 10.5271/sjweh.1913. [DOI] [PubMed] [Google Scholar]
- Kubo T, Fujino Y, Nakamura T, Kunimoto M, Tabata H, Tsuchiya T, Kadowaki K, Odoi H, Oyama I, Matsuda S. An industry-based cohort study of the association between weight gain and hypertension risk among rotating shift workers. J Occup Environ Med. 2013;55(9):1041–1045. doi: 10.1097/JOM.0b013e31829731fd. [DOI] [PubMed] [Google Scholar]
- Lee J, Chia KS. Estimation of prevalence rate ratios for cross sectional data: an example in occupational epidemiology. Br J Ind Med. 1993;50:861–862. doi: 10.1136/oem.50.9.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas AH, Franke HR. Women’s health in menopause with a focus on hypertension. Neth Heart J. 2009;17(2):68–72. doi: 10.1007/BF03086220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie IS, McEniery CM, Dhakam Z, Brown MJ, Cockcroft JR, Wilkinson IB. Comparison of the effects of antihypertensive agents on central blood pressure and arterial stiffness in isolated systolic hypertension. Hypertension. 2009;54(2):409–413. doi: 10.1161/HYPERTENSIONAHA.109.133801. [DOI] [PubMed] [Google Scholar]
- Murata K, Yano E, Shinozaki T. Impact of shift work on cardiovascular functions in a 10-year follow-up study. Scand J Work Environ Health. 1999;25(3):272–277. doi: 10.5271/sjweh.434. [DOI] [PubMed] [Google Scholar]
- Nakamura K, Sakurai M, Morikawa Y, Miura K, Ishizaki M, Kido T, Naruse Y, Suwazono Y, Nakagawa H. Overtime work and blood pressure in normotensive Japanese male workers. Am J Hypertens. 2012;25(9):979–985. doi: 10.1038/ajh.2012.37. [DOI] [PubMed] [Google Scholar]
- National Fire Protection Association (NFPA) NFPA 1582: standard on comprehensive occupational medical program for fire department. National Fire Protection Association; Quincy: 2007. [Google Scholar]
- National Institute for Occupational Safety and Health (NIOSH) (Fire fighter fatality investigation report F2007-22).After working three consecutive 24-hour shifts and fighting an extensive structure, a 47-year old career LT suffers sudden cardiac death during physical fitness training—California. 2008 http://www.cdc.gov/niosh/fire/reports/face200722.html.
- National Institute for Occupational Safety and Health (NIOSH) (Fire fighter fatality investigation report F2011-01).Fire fighter suffers heart attack while fighting grass fire and dies 2 days later—California. 2011 http://www.cdc.gov/niosh/fire/pdfs/face201101.pdf.
- Neitzel R, Hong O, Quinlan P, Hulea R. Pilot task-based assessment of noise levels among firefighters. Int J Ind Ergon. 2013;43(6):479–486. doi: 10.1016/j.ergon.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohira T, Tanigawa T, Iso H, Odagiri Y, Takamiya T, Shimomitsu T, Hayano J, Shimamoto T. Effects of shift work on 24-hour ambulatory blood pressure and its variability among Japanese workers. Scand J Work Environ Health. 2000;26(5):421–426. doi: 10.5271/sjweh.563. [DOI] [PubMed] [Google Scholar]
- Ohlander J, Keskin MC, Stork J, Radon K. Shift work and hypertension: prevalence and analysis of disease pathways in a German car manufacturing company. Am J Ind Med. 2015;58(5):549–560. doi: 10.1002/ajim.22437. [DOI] [PubMed] [Google Scholar]
- Ohlin B, Berglund G, Rosvall M, Nilsson PM. Job strain in men, but not in women, predicts a significant rise in blood pressure after 6.5 years of follow-up. J Hypertens. 2007;25(3):525–531. doi: 10.1097/HJH.0b013e32801220fa. [DOI] [PubMed] [Google Scholar]
- Peter R, Alfredsson L, Knutsson A, Siegrist J, Westerholm P. Does a stressful psychosocial work environment mediate the effects of shift work on cardiovascular risk factors? Scand J Work Environ Health. 1999;25(4):376–381. doi: 10.5271/sjweh.448. [DOI] [PubMed] [Google Scholar]
- Poston WS, Haddock CK, Jahnke SA, Jitnarin N, Day RS. An examination of the benefits of health promotion programs for the national fire service. BMC Public Health. 2013;13:805. doi: 10.1186/1471-2458-13-805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, Sheikh JI. The Primary Care PTSD Screen (PC-PTSD): development and operating characteristics (PDF) Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- Puttonen S, Kivimäki M, Elovainio M, Pulkki-Råback L, Hintsanen M, Vahtera J, Telama R, Juonala M, Viikari JS, Raitakari OT, Keltikangas-Järvinen L. Shift work in young adults and carotid artery intima-media thickness: the Cardiovascular Risk in Young Finns study. Atherosclerosis. 2009;205(2):608–613. doi: 10.1016/j.atherosclerosis.2009.01.016. [DOI] [PubMed] [Google Scholar]
- Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46. [PubMed] [Google Scholar]
- Ryff C, Almeida DM, Ayanian JS, Carr DS, Cleary PD, Coe C, Davidson R, Krueger RF, Lachman ME, Marks NF, et al. MidlifeDevelopment in the United States (MIDUS II), 2004-2006 [Computer file] Ann Arbor (MI): Interuniversity Consortium for Political and Social Research [distributor]; 2007. (ICPSR04652-v1). 2007-03-22. [DOI] [Google Scholar]
- Saidj M, Jørgensen T, Jacobsen RK, Linneberg A, Oppert JM, Aadahl M. Work and leisure time sitting and inactivity: effects on cardiorespiratory and metabolic health. Eur J Prev Cardiol. 2015 doi: 10.1177/2047487315619559. [DOI] [PubMed] [Google Scholar]
- Sakata K, Suwazono Y, Harada H, Okubo Y, Kobayashi E, Nogawa K. The relationship between shift work and the onset of hypertension in male Japanese workers. J Occup Environ Med. 2003;45(9):1002–1006. doi: 10.1097/01.jom.0000085893.98441.96. [DOI] [PubMed] [Google Scholar]
- Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA. 2009;106(11):4453–4458. doi: 10.1073/pnas.0808180106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sfreddo C, Fuchs SC, Merlo AR, Fuchs FD. Shift work is not associated with high blood pressure or prevalence of hypertension. PLoS One. 2010;5(12):e15250. doi: 10.1371/journal.pone.0015250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist J, Starke D, Chandola T, Godin I, Marmot M, Niedhammer I, Peter R. The measurement of effort-reward imbalance at work: European comparisons. Soc Sci Med. 2004;58(8):1483–1499. doi: 10.1016/S0277-9536(03)00351-4. [DOI] [PubMed] [Google Scholar]
- Soteriades ES, Kales SN, Liarokapis D, Christiani DC. Prospective surveillance of hypertension in firefighters. J Clin Hypertens. 2003;5(5):315–320. doi: 10.1111/j.1524-6175.2003.02058.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza BB, Monteze NM, de Oliveira FL, de Oliveira JM, de Freitas Nascimento S, Marques do NascimentoNeto R, Sales ML, Souza GG. Lifetime shift work exposure: association with anthropometry, body composition, blood pressure, glucose and heart rate variability. Occup Environ Med. 2015;72(3):208–215. doi: 10.1136/oemed-2014-102429. [DOI] [PubMed] [Google Scholar]
- Su TC, Lin LY, Baker D, Schnall PL, Chen MF, Hwang WC, Chen CF, Wang JD. Elevated blood pressure, decreased heart rate variability and incomplete blood pressure recovery after a 12-hour night shift work. J Occup Health. 2008;50(5):380–386. doi: 10.1539/joh.l7056. [DOI] [PubMed] [Google Scholar]
- Suwazono Y, Dochi M, Sakata K, Okubo Y, Oishi M, Tanaka K, Kobayashi E, Nogawa K. Shift work is a risk factor for increased blood pressure in Japanese men: a 14-year historical cohort study. Hypertension. 2008;52(3):581–586. doi: 10.1161/HYPERTENSIONAHA.108.114553. [DOI] [PubMed] [Google Scholar]
- Virkkunen H, Härmä M, Kauppinen T, Tenkanen L. Shift work, occupational noise and physical workload with ensuing development of blood pressure and their joint effect on the risk of coronary heart disease. Scand J Work Environ Health. 2007;33(6):425–434. doi: 10.5271/sjweh.1170. [DOI] [PubMed] [Google Scholar]
- Yang J, Teehan D, Farioli A, Baur DM, Smith D, Kales SN. Sudden cardiac death among firefighters ≤45 years of age in the United States. Am J Cardiol. 2013;112(12):1962–1967. doi: 10.1016/j.amjcard.2013.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]


