Abstract
Objectives
Intimate partner violence (IPV) is a global health issue affecting mainly women and is known to escalate during pregnancy and impact negatively on obstetric and perinatal outcomes. The aim of this study is to determine the incidence of IPV in a pregnant multicultural population and to determine the relationship between IPV reported at booking interview and maternal and perinatal outcomes.
Design
This is a retrospective population-based data study. We analysed routinely collected data (2006–2016) from the ObstetriX system on a cohort of pregnant women.
Setting and participants
33 542 women giving birth in a major health facility in Western Sydney.
Primary outcomes
Incidence of IPV, association with IPV and other psychosocial variables and maternal and perinatal outcomes.
Result
4.3% of pregnant women reported a history of IPV when asked during the routine psychosocial assessment. Fifty-four per cent were not born in Australia, and this had increased significantly over the decade. Women born in New Zealand (7.2%) and Sudan (9.1%) were most likely to report IPV at the antenatal booking visit, with women from China and India least likely to report IPV. Women who reported IPV were more likely to report additional psychosocial concerns including Edinburgh Postnatal Depression Scale scores > 13 (7.6%), thoughts of self-harm (2.4%), childhood abuse (23.6%), and a history of anxiety and depression (34.2%). Women who reported IPV were more likely to be Australian born, smoke and be multiparous and to have been admitted for threatened preterm labour (Adjusted Odds Ratio (AOR) 1.8, 95% CI 1.28 to 2.39).
Conclusions
A report of IPV at the first antenatal booking visit is associated with a higher level of reporting on all psychosocial risks, higher antenatal admissions, especially for threatened preterm labour. More research is needed regarding the effectiveness of current IPV screening for women from other countries.
Keywords: intimate partner violence, domestic violence, family violence, migrant, obstetrics, perinatal
Strengths and limitations of this study.
This was an ethnically diverse population that included all women in one hospital over a 10-year period.
Detailed psychosocial and other important variables were available.
We are unable to differentiate between immigrant and refugees.
It is likely there is under-reporting of intimate partner violence by pregnant women, particularly in some cultural groups.
Background
Intimate partner violence (IPV; physical, sexual or emotional) is a global health issue that affects mostly women (and some men) from different backgrounds and social groups. In 2016, the WHO released a global plan of action to address interpersonal violence, in particular against women, girls and against children.1 WHO stated that all forms of interpersonal violence lead to negative health outcomes and should be addressed by the health system. WHO identified health services as an appropriate entry point for addressing this.1 The Australian Personal Safety Survey estimated 186 000 women had experienced violence by a current cohabiting partner. Of those who had been pregnant, one in five (21.7%) reported that violence occurred during the pregnancy and for almost two-thirds of women (61.4%) this had been their first experience of violence in their relationship.2 The prevalence of violence during pregnancy is estimated to be between 4% and 8% of pregnant women.3
Global estimates of the prevalence of IPV range from 16.3% of ever-partnered women experiencing violence in their lifetime in East Asia to 50% of women suffering violence in Sub-Saharan Africa.4 However, these figures may be higher as the stigma and shame associated with IPV means disclosure remains low and in some cultural groups taboos about discussing what are considered to be family problems remain.5
Pregnant women exposed to IPV face many challenges; however, migrant women who are pregnant and living in a different sociocultural environment experience additional stresses in their lives, such as conflicting cultural values, social isolation, language barriers, limited economic resources, discrimination and racism.6 In many cultures, IPV is socially accepted, abuse is not always considered criminal or even incorrect, and the woman is seen as subservient to their male partner.6 A lack of knowledge about the law regarding IPV and immigration represents a challenge for migrant women as they may fear losing custody of their child/children and their immigration status.7
A meta-analysis of risk factors for domestic violence during pregnancy found across 92 studies that the average prevalence of emotional abuse was 28.4%, physical abuse was 13.8% and sexual abuse was 8%.8 The authors found that abuse before pregnancy and lower education level were strong predictors of abuse during pregnancy. A systematic review of domestic violence and perinatal mental health disorders including 67 papers found a three-fold increase in the odds of high-level depressive symptoms in the postnatal period after having experienced domestic violence during pregnancy.9 Post-traumatic stress disorder (PTSD) symptoms were also associated with a history of IPV. No studies identified a link between puerperal psychosis or eating disorders and IPV.9
The Australian government places a strong emphasis on supporting women who are pregnant with mental health and other psychosocial issues, with particular focus on early intervention, social inclusion, and recovery and service access, coordination and continuity of care.10 11 The increased recognition that social and emotional problems in the perinatal period can impact negatively on outcomes for women and their babies has led a number of Australian states and territories to introduce psychosocial assessment which includes depression screening as well as questions on IPV. This process has been supported by beyondblue and the National Perinatal Depression Initiative which has led to the production of perinatal clinical practice guidelines for healthcare professionals.12 In addition, in New South Wales (NSW) the Supporting Families Early Policy has integrated psychosocial risk assessment into routine care (Integrated Perinatal Care) during pregnancy and after the birth. The aim of this approach is to provide a coordinated network of support for mothers and their babies.13 14 All women when they book in for their pregnancy care in public hospitals (this is not routine in the private healthcare sector) receive a psychosocial assessment from midwives and then again from the child and family health nurse (CFHN) following birth and again at the 6–8 weeks’ postnatal check. The psychosocial screening tool includes the Edinburgh Postnatal Depression Scale (EPDS) and a series of questions that encompass seven key variables or areas of risk (table 1). This routine screening of pregnant women is not without its concerns regarding the specific skills required in understanding, interpreting and responding appropriately to women’s needs and the support provided to midwives to do this.14 15 This is an even more complex issue where migrant women are concerned and cultural understandings, taboos and language barriers could all have a significant influence.16
Table 1.
Psychosocial risk variables I–IV, New South Wales Department of Health (2010)
| Variables (risk factors) | Suggested format for psychosocial assessment questions |
| I. Lack of support | 1. Will you be able to get practical support with your baby? 2. Do you have someone you are able to talk to about your feelings or worries? |
| II. Recent major stressors in the last 12 months | 3. Have you had any major stressors, changes or losses recently (ie, in the last 12 months) such as, financial problems, someone close to you dying or any other serious worries? |
| III. Low self-esteem (including lack of self-confidence, high anxiety and perfectionistic traits) | 4. Generally, do you consider yourself a confident person? 5. Does it worry you a lot if things get messy or out of place? |
| IV. History of anxiety, depression or other mental health problems | 6. (a) Have you ever felt anxious, miserable, worried or depressed for more than a couple of weeks? 6. (b) If so, did it seriously interfere with your work and your relationships with friends and family? 7. Are you currently receiving, or have you in the past received, treatment for any emotional problems? |
| V. Couple’s relationship problems or dysfunction (if applicable) | 8. How would you describe your relationship with your partner? 9. (a) Antenatal: What do you think your relationship will be like after the birth? OR (b) Postnatal (in Community Health Setting): Has your relationship changed since having the baby? |
| VI. Adverse childhood experiences | 10. Now that you are having a child of your own, you may think more about your own childhood and what it was like. As a child were you hurt or abused in any way (physically, emotionally, sexually)? |
| VII. Domestic violence Questions must be asked only when the woman can be interviewed away from partner or family member over the age of 3 years. Staff must undergo training in screening for domestic violence before administering questions |
11. Within the last year, have you been hit, slapped or hurt in other ways by your partner or ex-partner? 12. Are you frightened of your partner or ex-partner? (If the response to questions 11 and 12 is ‘No’ then offer the Domestic Violence information card and omit questions 13–18) 13. Are you safe here at home?/to go home when you leave here? 14. Has your child/children been hurt or witnessed violence? 15. Who is/are your children with now? 16. Are they safe? 17. Are you worried about your child/children’s safety? 18. Would you like assistance with this? |
| Opportunity to disclose further | 19. Are there any other issues or worries you would like to mention? |
The aim of this study was to determine the incidence of IPV in a pregnant multicultural population not born in Australia compared with Australian-born women and to determine the relationship between IPV reported at booking interview and obstetric and perinatal outcomes.
Methods
Study design
This is a retrospective population-based data study. We analysed routinely collected data from the ObstetriX system on a cohort of all pregnant women giving birth in a major health facility in Western Sydney over a 10-year period (2006–2016; n=33 542).
Setting
Blacktown Hospital is located in Western Sydney, NSW, Australia and provides maternity services to over 3000 women per year. Blacktown is classified as a level 4 maternity unit, meaning it cares for women of low to moderate obstetric risk. Western Sydney is a rapidly growing area in NSW. It has a diverse population with a high proportion of young families, multiculturalism (57% not born in Australia) and significant socioeconomic disadvantage.17 Routine antenatal psychosocial assessment, which includes depression screening and questions on domestic violence, has been conducted routinely at this site since 2006 when it was introduced at Blacktown Hospital.
Data sources
This study was a retrospective review of routinely collected data for a consecutive cohort of women who delivered babies at Blacktown Hospital between 1 January 2006 and 31 May 2016. Data were sourced from the Western Sydney Local Health District ObstetriX database, an information system that collects clinical data from first antenatal visit through to discharge of mother and baby from the hospital.
Variables
Variables of interest included (1) demographics (age, country of birth and private health insurance status); (2) baseline health, obstetric characteristics and medical risks (parity, body mass index (BMI), smoking, diagnosis of hypertension, diabetes, incidence of threatened premature labour, antepartum haemorrhage; (3) psychosocial risks (evidence of IPV); (4) depressive and anxiety symptoms; (5) birth details (gestation at birth, birth type, perineal status) and (6) postnatal outcomes (Apgar scores, birth weight, admission to neonatal intensive care unit). The relationship between IPV and above-listed health outcomes were also examined.
The psychosocial screening tool questions are based on a series of known risk factors and are administered alongside the EPDS (table 1). The booking midwife administers this screening tool in the privacy of the initial antenatal booking visit when women are around 12–20 weeks’ pregnant. Partners are asked not to be present or to leave when these questions are asked. If an NSW Health Interpreter was booked for the visit, the questions were asked verbally via the interpreter.
Analysis
Positive responses to the IPV questions, collected by clinical staff at the first antenatal visit, were grouped to form the dichotomous variable ‘IPV’ or ‘no IPV’ for all women. Women were grouped in non-Australian-born and Australian-born cohorts and for the non-Australian-born cohort the seven most commonly occurring countries of birth were examined independently. Pregnancy, labour and birth events were then analysed using contingency tables and χ2 results were calculated. Logistic regression techniques were applied and reported as unadjusted and adjusted ORs and 95% CIs following adjustment for maternal age, gestation at birth, country of birth and smoking. Analysis was undertaken with IBM SPSS V.23. Due to the number of statistical tests undertaken, a p value <0.001 was set for significance.
Ethics approval was given by Western Sydney Local Health District (Protocol Number HREC2013/4/6.7 (3697) AU RED LNR/13/WMEAD/98) and an amended approval given in 2017. A waiver of individual consent was obtained due to the deidentified nature of the data.
Results
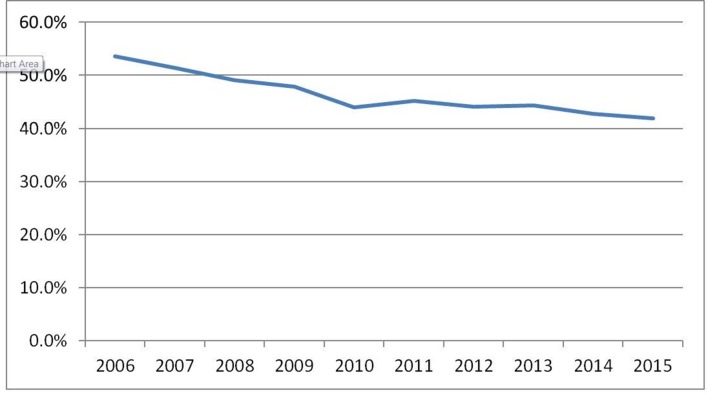
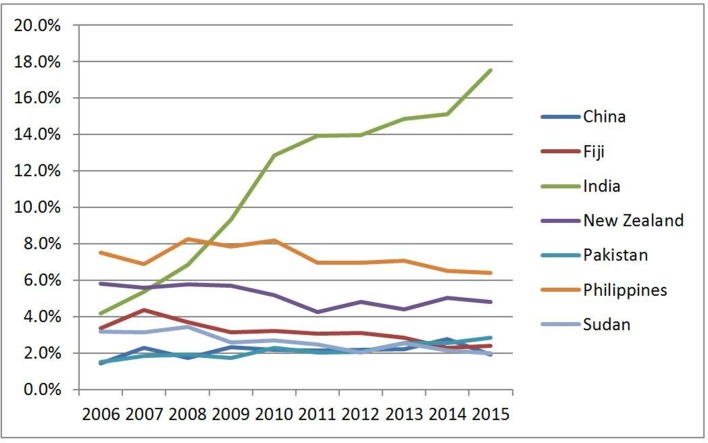
Over a 10-year period (2006–2016 inclusive), 33 542 women gave birth at the Western Sydney maternity unit. During this time, there was a decrease in the number of women giving birth who were born in Australia (figure 1). During the 10 years, the increase in women born in India was most notable (4.2%–25.7%) (figure 2). Overall, 4.3% of women reported a history of IPV. There were an additional 0.8% of women for whom screening was not undertaken due to refusal of their partner or other family member(s) to leave the interview room.
Figure 1.
Changing profile of Australian-born women expressed as a percentage of all births over time.
Figure 2.
Changing profile of non-Australian-born women expressed as a percentage of all births over time.
There were differences in demographics between Australian and non-Australian women, with Australian women being younger, more likely to be under 20 years of age and less likely to be over 35 years of age. Australian born women were more likely to have a BMI >30 (table 2).
Table 2.
Selected demographics of Australian-born and non-Australian-born women
| Australian born, n=15 459 |
Non-Australian born, n=18 083 |
P values | |
| Maternal age* | 27.7 (5.75) | 29.8 (5.11) | <0.001 |
| Teenage pregnancy | 7.9% | 1.8% | <0.001 |
| Pregnancy ≥35 years | 13.0% | 17.9% | <0.001 |
| Nulliparous | 25.0% | 26.9% | <0.002 |
| Body mass index ≥30 | 28.2% | 17.7% | <0.001 |
| Body mass index ≤18 | 3.0% | 3.0% | 0.02 |
| Private patient | 3.7% | 3.4% | 0.14 |
*Mean and SD.
During pregnancy, women born in Australia were more likely to smoke and have hypertensive disorders of pregnancy but they were less likely to have gestational diabetes and anaemia. In terms of birth outcomes, women born in Australia were more likely to have a normal vaginal birth, have an epidural and give birth in the birth centre. There was a significantly higher stillbirth rate observed in women not born in Australia (table 3).
Table 3.
Pregnancy events and outcomes of Australian-born and non-Australian-born women
| Australian born, n=15 459 |
Non-Australian born, n=18 083 |
P values | |
| Smoking | 19.7% | 4.3% | <0.001 |
| Gestational hypertension | 2.6% | 1.8% | <0.001 |
| Gestational diabetes | 6.4% | 13.6% | <0.001 |
| Admitted for threatened premature labour |
3.6% | 2.8% | <0.002 |
| Maternal anaemia | 7.7% | 10.2% | <0.001 |
| Any antepartum haemorrhage | 0.8% | 0.9% | 0.38 |
| Gestation at birth* | 39.2 (2.01) | 39.1 (1.98) | <0.001 |
| Gestation grouped | |||
| <28 weeks | 0.6% | 0.7% | 0.12 |
| 29–32 weeks | 0.4% | 0.3% | |
| 32–36 weeks | 5.3% | 5.0% | |
| 37 weeks and greater | 93.7% | 94.0% | |
| Normal vaginal birth | 66.4% | 60.6% | <0.001 |
| Instrumental birth | 8.6% | 11.2% | <0.001 |
| Caesarean section | 25.0% | 28.2% | <0.001 |
| Syntocinon usage | 46.1% | 53.9% | <0.001 |
| Place of birth | |||
| Birth centre | 9.2% | 4.9% | <0.001 |
| Born before arrival | 0.8% | 0.6% | <0.001 |
| Operating theatre | 25.0% | 28.2% | <0.001 |
| Delivery ward | 65.0% | 66.3% | <0.001 |
| Amniotomy | 51.9% | 51.4% | 0.36 |
| Epidural usage† | 19.8% | 15.3% | <0.001 |
| Third-degree and fourth-degree tears† | 0.5% | 1.5% | <0.001 |
| Episiotomy† | 14.4% | 22.6% | <0.001 |
| Postpartum haemorrhage >1500 mL | 1.2% | 1.4% | 0.38 |
| Birth weight* | 3414 (588.22) | 3290 (563.49) | <0.001 |
| Admitted to special care nursery/neonatal intensive care unit |
7.5% | 8.6% | <0.001 |
| Stillbirth rate/1000 births | 5.2 | 8.2 | <0.001 |
| 5 min Apgar <7 | 1.6% | 1.6% | 0.56 |
| Fetal anomaly | 0.8% | 0.7% | 0.38 |
*Median, IQR, Mann-Whitney U.
†As a % of vaginal births.
Women who disclosed IPV at the first antenatal booking visit over this 10-year period weighed slightly less and smoked more than twice as much compared with those who did not disclose IPV. These women were also more likely to be having a subsequent baby. During pregnancy, they were more likely to have an admission with threatened premature labour (table 4).
Table 4.
Maternal characteristics and perinatal outcomes for women who disclosed IPV at the first booking visit compared with those who have not
| IPV reported, n=1302 | IPV not reported, n=29 026 | P values | |
| Maternal age* | 28.7 (5.46) | 28.6 (6.07) | 0.29 |
| Body mass index* | 26.6 (6.54) | 27.1 (7.17) | <0.001 |
| Multiparous | 82.7% | 68.8% | <0.001 |
| Smoking | 26.8% | 11.0% | <0.001 |
| Hypertension diagnosed in pregnancy | 1.5% | 2.4% | 0.04 |
| Gestational diabetes | 9.4% | 8.6% | 0.96 |
| Threatened premature labour | 5.5% | 3.1% | <0.001 |
| Any Antepartum haemorrhage | 2.22% | 1.55% | 0.08 |
| Antenatal admission | 10.8% | 8.6% | 0.006 |
| Gestation at birth† | 39.2 (1.96) | 39.1 (1.90) | 0.12 |
| Birth type | |||
| Normal vaginal birth | 66.7 % | 61.6 % | <0.001 |
| Instrumental birth | 7.0 % | 10.9 % | <0.001 |
| Caesarean section | 26.3 % | 27.5 % | <0.001 |
| Epidural usage‡ | 29.7% | 28.3% | 0.36 |
| Third-degree and fourth-degree tears‡ | 0.46% | 1.3% | 0.01 |
| Episiotomy‡ | 18.8% | 25.5% | 0.05 |
| Postpartum blood transfusion | 1.08% | 0.83% | 0.94 |
| Birth weight* | 3349 (568.0) | 3344 (573.6) | 0.77 |
| Admitted to special care nursery/neonatal intensive care unit | 8.6% | 8.5% | 0.88 |
| Stillbirth rate/1000 births | 3.9 | 5.4 | 0.49 |
| Feeding difficulty | 38.6% | 39.6% | 0.49 |
| Male gender | 51.0% | 51.3% | 0.88 |
| Fetal growth restriction | 6.5% | 4.8% | 0.03 |
*Mean, SD and t-test.
†Median, IQR, Mann-Whitney U.
‡As a % of vaginal births.
IPV, intimate partner violence.
Overall 4.3% of women reported a history (current partner 3.5%, previous partner 0.7%, other family member 0.1%) of IPV when asked during the routine psychosocial assessment at booking in for pregnancy care. Women born in New Zealand (7.2%) and Sudan (9.1%) were most likely to report IPV at the antenatal booking visit, with women from China and India least likely to report IPV. Missing data for variables relating to IPV equated to 8.7% (table 5).
Table 5.
IPV expressed as a percentage of country of birth for the most commonly occurring countries of birth of all women assessed
| Australia, n=13 742 | India, n=3783 | Philippines, n=2193 | NZ, n=1520 | Fiji, n=939 | Sudan, n=784 | Pakistan, n=670 | China, n=655 | Other, n=6042 | Total, n=30 328 | |
| Domestic violence, current partner | 3.9% | 1.6% | 3.3% | 6.2% | 4.3% | 8.2% | 2.5% | 1.4% | 2.7% | 3.5% |
| Domestic violence, other family member | 0.1% | 0.1% | 0.0% | 0.4% | 0.2% | 0.0% | 0.0% | 0.0% | 0.0% | 0.1% |
| Domestic violence, previous partner | 1.3% | 0.2% | 0.6% | 0.6% | 0.1% | 0.9% | 0.1% | 0.2% | 0.3% | 0.8% |
| Domestic violence, any | 5.2% | 1.8% | 4.0% | 7.2% | 4.5% | 9.1% | 2.7% | 1.5% | 3.1% | 4.3% |
| Deferred questions due to partner or family members’ presence | 1.0% | 0.3% | 0.6% | 1.2% | 0.7% | 1.4% | 1.0% | 1.7% | 1.1% | 0.9% |
IPV, intimate partner violence; NZ, New Zealand.
Women who reported IPV were more likely to report concerns when psychosocial screening was attended, including EPDS > 13 (7.63%), thoughts of self-harm (2.4%), childhood abuse (23.6%) and anxiety and depression (34.2%). Women who reported IPV were more likely overall to be Australian born, smoke and be multiparous (table 6).
Table 6.
Associated psychosocial issues for pregnant women reporting intimate partner violence (IPV) compared with those who do not
| IPV reported (%) | IPV not reported (%) | P values | OR (95% CI) | |
| Edinburgh Postnatal Depression Scale ≥13 | 7.6 | 2.1 | <0.001 | 3.57 (2.84–4.47) |
| Thoughts of self-harm | 2.4 | 0.5 | <0.001 | 5.55 (3.73–8.25) |
| Illegal drug use risk | 4.30 | 0.73 | <0.001 | 6.11 (4.52–8.24) |
| Childhood abuse | 23.6 | 7.6 | <0.001 | 3.74 (3.27–4.28) |
| Pregnancy-related anxiety risk | 5.9 | 2.1 | <0.001 | 2.88 (2.26–3.67) |
| Work/relationship effect risk | 23.0 | 7.4 | <0.001 | 3.76 (3.28–4.30) |
| Anxiety/depression risk | 34.2 | 14.0 | <0.001 | 3.19 (2.84–3.60) |
| Worried about mess risk | 34.3 | 25.0 | <0.001 | 1.57 (1.39–1.76) |
| Positive response to ‘are you generally confident’ question | 75.4 | 84.6 | <0.001 | 0.24 (0.21–0.27) |
| Recent worry/stress risk | 47.2 | 22.2 | <0.001 | 3.20 (2.81–3.52) |
| Emotional support risk | 8.6 | 4.4 | <0.001 | 2.04 (1.67–2.50) |
| Mental health disorder | 7.07 | 1.72 | <0.001 | 4.36 (3.46–5.48) |
| Family history of mental health disorder | 19.1 | 10.7 | <0.001 | 1.97 (1.71–2.28) |
We examined women reporting IPV at booking and the incidence of pregnancy conditions and events compared with women with no report of IPV adjusting for smoking, parity and gestational age and found significant associations with IPV and being born in Australia, smoking, being multiparous and having threatened premature labour. Women reporting IPV were however less likely to have hypertensive disease of pregnancy (table 7).
Table 7.
OR calculations for women reporting intimate partner violence (IPV) at booking and pregnancy conditions and events when compared with women not reporting IPV (ref category is non-IPV)
| OR | AOR | |
| Australian born | 1.5 (1.31–1.64) | 1.3 (1.09–1.46) |
| Smoking | 3.0 (2.60–3.36) | 2.7 (2.30–3.20) |
| Multiparous | 2.3 (1.98–2.70) | 2.0 (1.68–2.49) |
| Gestational diabetes mellitus | 1.0 (0.87–1.24) | 1.1 (0.85–1.29) |
| Hypertensive disorders of pregnancy | 0.6 (0.39–0.97) | 0.5 (0.32–0.91) |
| Threatened premature labour | 1.8 (1.44–2.36) | 1.8 (1.28–2.39) |
| Antepartum haemorrhage | 1.5 (1.04–2.11) | 1.4 (0.95–2.19) |
| Normal vaginal birth | 1.00 | 1.00 |
| Instrumental birth | 0.6 (0.49 – 0.76) | 1.1 (0.90 – 1.25) |
| Caesarean section | 1.1 (0.94 – 1.20) | |
| Born preterm | 1.3 (1.04–1.60) | 1.0 (0.71–1.33) |
| Special care nursery/neonatal intensive care unit admission | 1.0 (0.77–1.16) | 1.0 (0.82–1.23) |
| Apgar 2 (less than 7) | 1.5 (1.00–2.12) | 1.1 (0.64–1.80) |
| Breastfed | 0.8 (0.73–0.93) | 1.0 (0.86–1.20) |
Discussion
In this study, we aimed to determine the incidence of IPV over 10 years in a pregnant multicultural population and to compare characteristics of those not born in Australia with those born in Australia. We also aimed to determine the relationship between IPV reported at the antenatal booking interview and selected obstetric and perinatal outcomes.
Australia has a large population of both economic and humanitarian migrant, and there has been a steady increase in new arrivals over the past decade in some metropolitan locations, including the study site. Understanding the specific healthcare needs of migrant women in pregnancy and following birth is important to inform health service design and delivery and ensure the best health outcomes for women and babies. We found a dramatic increase in the number of women born overseas (from 47% in 2006 to 62% in 2016) with the largest increase being in women born in India. We also found differences in demographics and obstetric outcomes between Australian-born and non-Australian-born women, with those not born in Australia tending to be older, less likely to have a BMI of > 30 compared with those born in Australia. They are also much less likely to smoke and much more likely to have gestational diabetes. These differences were identified previously in our analyses of the state-wide population.18 19
Overall, a low proportion of women disclosed IPV (4.3%). This is comparable with, or a little lower than other Australian20 and international3 studies that also estimated IPV prevalence to be between 4% and 8% of pregnant women. However, this is very likely to reflect under-reporting by women, as demonstrated by James et al, the prevalence of IPV in pregnancy is close to 20%.8 Furthermore, in NSW the IPV screening questions ask directly about physical abuse which was estimated to be around 13.8%.21
The Maternal Health Study conducted in one Australian state (Victoria) reported that the prevalence of domestic violence across the first postnatal year was 17%.20 At the 4-year follow-up, the authors found that 29% of women experienced IPV across the 4 years postbirth. This included women who were subjected to physical and or emotional and/or sexual abuse.22
In our study, women who reported IPV were more likely overall to be Australian born. We found that of the non-Australian born cohort, women born in New Zealand and in Sudan were more likely to report IPV when asked. The New Zealand sample is likely to reflect the higher Maori and Pacific Islander population in this location (Western Sydney). New Zealand research has reported a higher prevalence of IPV among Maori women and in some locations, this is over 60%.23 Studies also report that many Sudanese women experience IPV from their husbands prior to migration, and this represents a significant factor in these women’s premigration history.24
In contrast, women born in India (the largest migrant group in the study location) and those born in China were the least likely to say they experienced IPV when asked. We suggest that this reflects significant under-reporting by these women. Previous studies have reported rates of 4% in China25 and more recently James et al found a prevalence of 4.8% in China and a prevalence of 28% in India.8 This under-reporting is likely due to cultural concerns about sharing with strangers what is considered to be family business, something that is accepted in their country of origin.26
Women who reported IPV were more likely to report a raised EPDS > 13 (7.63%), thoughts of self-harm (2.4%), and anxiety and depression (34.2%). These women were also more likely to worry, report stress and have a family history of mental illness. This means they are likely to have fewer social support systems in place that could buffer or protect them and their children from the effects of IPV.27 A number of longitudinal studies of maternal well-being in Australia22 28 show a strong association between depressive symptoms in pregnancy and in the year after birth and poor partner relationship and IPV.
Another major concern reported when psychosocial screening was attended was childhood abuse (23.6%) which was significantly associated with IPV. Researchers have hypothesised that women with a history of childhood abuse may be at exceptionally high risk of revictimisation in adulthood, including rape and IPV.29–32 In the Maternal Health Study, childhood abuse was reported by a high number of women (41%), and these women were more likely to experience IPV and poor mental health.28
As noted, women who reported IPV were more likely to be Australian born, they were more likely to smoke and be multiparous. During the pregnancy, they were less likely to have hypertensive disease of pregnancy and more likely to have been admitted for threatened preterm labour (AOR 1.8, 95%CI 1.28 to 2.39). Various studies have demonstrated a significant impact of IPV on women’s health behaviours during pregnancy, including higher rates of smoking,33–35 alcohol and substance use.36–38 Experiencing IPV is a significant life stress and higher rates of mental illness, seen in this study, also correlate with high smoking rates. One study found probable major depression and generalised anxiety disorder were associated with a 93% and 44% increased odds, respectively, of being a current smoker.39
Likewise, the higher number of multiparous women reporting IPV would impact on the higher rates of normal birth seen in this group as well as the lower episiotomy rate and severe perineal trauma rate.
The impact of IPV on maternal mental health cannot be underestimated. During the pregnancy and the postpartum period, IPV is associated with depression, anxiety and PTSD.40–42 PTSD rates associated with IPV range from anywhere between 19% and 84%.43 44 Around 40% of women who experience IPV report symptoms of depression.44 45 The most serious reported outcomes of IPV during pregnancy are homicide and suicide, with maternal injury a leading cause of maternal mortality.46 47 It has been estimated that 38% of murders of women are by an intimate partner or ex-partner.1
In this study, we found women who were multiparous were more likely to disclose IPV, and this has been reported previously.48 This is important to know as women may be more prepared to disclose with a subsequent pregnancy. This may be due to their realising the impact of IPV on the child but also they may be feeling more comfortable with and trusting of the service.49 Another possibility for this higher rate of disclosure of IPV with multiparous women may be due to the fact that hopes that a coercive partner may reform once the baby has arrived are not realised. Perhaps also motherhood shifts loyalty from a non-supportive partner to a baby, and energy and affection is channelled more to the baby. This in turn may make reporting easier but may also lead to an escalation of IPV. It is really important more research is done to help understand this. It is also possible that relationship strains may be taking a toll with the presence of children and escalation of IPV. In a study undertaken in Nigeria where a much higher IPV was found in multiparous women, the authors suggest lower socioeconomic status could be a factor in this as well as this is associated with larger families.48
A number of studies have reported that women who suffer IPV during pregnancy are twice as likely to miss antenatal visit appointments or initiate antenatal care early.50 51 Women with a history of IPV are more likely to miss three or more antenatal visits compared with their non-abused counterparts (45% vs 28%).52 In addition, there are increased numbers of hospitalisation reported for these women.53 In our study, we found women were more likely to be hospitalised with threatened preterm birth if they had a history of IPV. Several studies have reported a link between insufficient antenatal care associated with IPV and adverse birth outcomes, including preterm birth and low birth weight (LBW) and small for gestational age.54–56 While we did not find an actual increase in preterm birth in this study, it is well known that preterm birth and LBW are the primary causes of neonatal morbidity and mortality.57
Health services
The WHO has identified health services as an appropriate entry point for addressing IPV, in particular against women and girls1 who bear the vast burden of IPV. Women who experience IPV are more likely to use health services than those who do not even though they rarely explicitly disclose violence as the underlying reason.1 This is even more the case when they are pregnant, and midwives and doctors are the front-line healthcare providers in this case. Unfortunately, health and other services are slow to recognise and address this violence, either because they do not recognise the signs, do not have appropriate services in place or they are simply at capacity.1
Currently, the Australian Government has a clear aim to reduce the incidence of IPV against women through public education and health promotion. However, more is required from health providers than simply asking the question. Spangaro et al found multiple pathways to disclosure with no single factor necessarily sufficient for a decision to disclose.58 While being asked the question was important in women disclosing IPV, the way the question was asked (with interest and being non-judgemental) were found to be key conditions.58 With the increasing use of computers to guide questions and document women’s responses to sensitive questions included in psychosocial screening,59 questions are raised as to how effective this will be if a trusting relationship is important in disclosure. A recent ethnographic study of psychosocial assessment and depression screening in pregnancy and following birth found that some midwives and CFHNs were reticent to ask questions related to IPV as well as childhood abuse, at times avoiding asking these questions, rewording the question or minimising women’s responses.14 60 Midwives and nurses also indicated that many women from non-English speaking backgrounds did not always understand the question being asked of them and interpreters were not always available.14 60 This suggests that we have less knowledge of how to screen for IPV among diverse cultural and linguistic groups. We also have limited information about how many women who report IPV are provided with appropriate referrals and whether they take up the referral. Our study also raises important questions around the need to have a higher level of awareness and vigilance regarding possible IPV when women report childhood abuse and other commonly gathered antenatal information.
There are current discussions among health workers and government services that screening women for IPV initially at booking and again during the third trimester could be advisable as IPV may escalate and/or women may feel more comfortable and trusting of their care provider as the pregnancy advances. This may be even more useful in continuity of care models where women are cared for by a trusted midwife who they get to know and trust. Others suggest that questions about IPV should not be asked at the first visit as is currently done as no relationship has been developed. There is little evidence as to what might be the best approach. There is debate about both the effectiveness of IPV enquiry and the most appropriate time to conduct assessments in pregnancy and after birth.61 A number of authors report that when asked, women may choose not to disclose about the abuse at the initial time of asking, for fear of their own safety but asking signifies that she can disclose at a later contact.49 As a result of this debate, there is inconsistent and at times poor uptake of screening in antenatal services in Australia.62
Strengths and limitations
There are several limitations with this study, and these include that it involves only one hospital in Western Sydney and so may not be generalisable to other areas with different populations. Also, we were unable to determine ethnicity as the variable provided is country of birth, and we could not distinguish between refugees and migrants. Other outcomes not reported here because of the nature of the dataset include urinary and faecal incontinence.63 The division of non-Australian-born women into the seven countries dilutes the data pool and limits conclusions about individual groups. There is missing data for the IPV variable as already reported, and this is more frequent in the first few years of the dataset when psychosocial screening was being introduced. The advantages of using the ObstetriX database are the large number of variables available compared with the other state-wide routine databases, such as the Perinatal Data Collection and Admitted Patient Data Collection. Socioeconomic factors which affect health such as BMI, psychosocial risk factors, marital status, education level and occupation are not collected in the latter, and adjustment for these variables cannot be undertaken when modelling statistical interactions with these databases and the use of ObstetriX provides this advantage.
Conclusion
There appears to be a relationship between psychosocial risks identified at the antenatal booking visit and a history of IPV; in particular, this is seen in women who have a history of anxiety and depression and childhood abuse. This provides maternity healthcare providers with more evidence for incorporating routine psychosocial screening during antenatal care and providing appropriate services. The fact that women with a history of IPV had more antenatal admissions, particularly for threatened preterm labour, could provide another potential warning sign for midwives and doctors. More research is needed regarding the effectiveness of current IPV screening for women from other countries.
Supplementary Material
Acknowledgments
The authors are grateful to Blacktown hospitals and Western Sydney University for supporting AMM to have time working with academics to develop research skills under the Nurse/Midwives Consultant Research and Capacity Building Scheme.
Footnotes
Contributors: HGD designed the study, assisted with analysis and wrote the paper. AMM undertook a review of the literature and helped access the data for analysis. VS consulted on the study and contributed to the writing of the paper. CT analysed the data and assisted in writing the paper.
Funding: Funding for the project came from a Western Sydney University Research Partnership grant with NSW Health.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Western Sydney Local Health District (Protocol Number HREC2013/ 4/6.7 (3697) AU RED LNR/13/WMEAD/98) and an amended approval given in 2017.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: We do not have ethics permission to share the data.
References
- 1. World Health Organisation. Global plan of action to strengthen the role of the health system within a national multisectoral response to address interpersonal violence, in particular against women and girls, and against children. Geneva: WHO Press, 2016. [Google Scholar]
- 2. Australian Bureau of Statistics. Personal safety survey, Australia (cat. no. 4906.0). Canberra: Australian Bureau of Statistics, 2013. [Google Scholar]
- 3. Devries KM, Kishor S, Johnson H, et al. Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters 2010;18:158–70. 10.1016/S0968-8080(10)36533-5 [DOI] [PubMed] [Google Scholar]
- 4. World Health Organisation. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: World Health Organisation, 2013. [Google Scholar]
- 5. Mezey GC, Bewley S. Domestic violence and pregnancy. Br J Obstet Gynaecol 1997;104:528–31. 10.1111/j.1471-0528.1997.tb11526.x [DOI] [PubMed] [Google Scholar]
- 6. Raj A, Silverman J. Violence against immigrant women: the roles of culture, context and legal immigrant status on intimate partner violence. Violence Against Women 2002;8:367–98. [Google Scholar]
- 7. Stewart DE, Gagnon AJ, Merry LA, et al. Risk factors and health profiles of recent migrant women who experienced violence associated with pregnancy. J Womens Health 2012;21:1100–6. 10.1089/jwh.2011.3415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. James L, Brody D, Hamilton Z. Risk factors for domestic violence during pregnancy: a meta-analytic review. Violence Vict 2013;28:359–80. 10.1891/0886-6708.VV-D-12-00034 [DOI] [PubMed] [Google Scholar]
- 9. Howard LM, Oram S, Galley H, et al. Domestic violence and perinatal mental disorders: a systematic review and meta-analysis. PLoS Med 2013;10:e1001452 10.1371/journal.pmed.1001452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Commonwealth of Australia. Improving maternity services in Australia, the report of the maternity services review. Canberra: Commonwealth of Australia, 2009. [Google Scholar]
- 11. Australian Government Department of Health and Ageing. Australian health ministers advisory council, national framework for universal child and family health services. Canberra: Australian Government Department of Health and Ageing, 2011. [Google Scholar]
- 12. Beyondblue. Beyondblue: the national depression initiative. Australia: Byondblue, 2011. [Google Scholar]
- 13. NSW Department of Health. NSW Health/families NSW supporting families early package—SAFE START. North Sydney: NSW Department of Health, 2009. [Google Scholar]
- 14. Rollans M, Schmied V, Kemp L, et al. ’We just ask some questions…' the process of antenatal psychosocial assessment by midwives. Midwifery 2013;29:935–42. 10.1016/j.midw.2012.11.013 [DOI] [PubMed] [Google Scholar]
- 15. Yelland JS, Sutherland GA, Wiebe JL, et al. A national approach to perinatal mental health in Australia: exercising caution in the roll-out of a public health initiative. Med J Aust 2009;191:276–9. [DOI] [PubMed] [Google Scholar]
- 16. Schmied V, Black E, Naidoo N, et al. Migrant women’s experiences, meanings and ways of dealing with postnatal depression: a meta-ethnographic study. PLoS One 2017;12 10.1371/journal.pone.0172385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. NSW Government. 2013. http://www.westernsydney.nsw.gov.au/about-western-sydney/demographics/
- 18. Dahlen HG, Schmied V, Dennis CL, et al. Rates of obstetric intervention during birth and selected maternal and perinatal outcomes for low risk women born in Australia compared to those born overseas. BMC Pregnancy Childbirth 2013;13:100 10.1186/1471-2393-13-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dahlen HG, Barnett B, Kohlhoff J, et al. Obstetric and psychosocial risk factors for Australian-born and non-Australian born women and associated pregnancy and birth outcomes: a population based cohort study. BMC Pregnancy Childbirth 2015;15:292 10.1186/s12884-015-0681-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gartland D, Hemphill SA, Hegarty K, et al. Intimate partner violence during pregnancy and the first year postpartum in an Australian pregnancy cohort study. Matern Child Health J 2011;15:570–8. 10.1007/s10995-010-0638-z [DOI] [PubMed] [Google Scholar]
- 21. Hutton JD, James DK, Stirrat GM, et al. Management of severe pre-eclampsia and eclampsia by UK consultants. Br J Obstet Gynaecol 1992;99:554–6. 10.1111/j.1471-0528.1992.tb13819.x [DOI] [PubMed] [Google Scholar]
- 22. Gartland D, Woolhouse H, Giallo R, et al. Vulnerability to intimate partner violence and poor mental health in the first 4-year postpartum among mothers reporting childhood abuse: an Australian pregnancy cohort study. Arch Womens Ment Health 2016;19:1091–100. 10.1007/s00737-016-0659-8 [DOI] [PubMed] [Google Scholar]
- 23. Gao W, Paterson J, Abbott M, et al. Impact of current and past intimate partner violence on maternal mental health and behaviour at 2 years after childbirth: evidence from the Pacific Islands Families Study. Aust N Z J Psychiatry 2010;44:174–82. 10.3109/00048670903487126 [DOI] [PubMed] [Google Scholar]
- 24. Higginbottom GM, Safipour J, Mumtaz Z, et al. "I have to do what I believe": Sudanese women’s beliefs and resistance to hegemonic practices at home and during experiences of maternity care in Canada. BMC Pregnancy Childbirth 2013;13:51 10.1186/1471-2393-13-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Leung WC, Leung TW, Lam YY, et al. The prevalence of domestic violence against pregnant women in a Chinese community. Int J Gynaecol Obstet 1999;66:23–30. 10.1016/S0020-7292(99)00053-3 [DOI] [PubMed] [Google Scholar]
- 26. Primary prevention of violence against immigrant and refugee women in Australia. Melbourne: M.C.f.W.s. Health, 2011. [Google Scholar]
- 27. Coker AL, Smith PH, Thompson MP, et al. Social support protects against the negative effects of partner violence on mental health. J Womens Health Gend Based Med 2002;11:465–76. 10.1089/15246090260137644 [DOI] [PubMed] [Google Scholar]
- 28. Giallo R, Pilkington P, McDonald E, et al. Physical, sexual and social health factors associated with the trajectories of maternal depressive symptoms from pregnancy to 4 years postpartum. Soc Psychiatry Psychiatr Epidemiol 2017;52:815–28. 10.1007/s00127-017-1387-8 [DOI] [PubMed] [Google Scholar]
- 29. Russell DE. The incidence and prevalence of intrafamilial and extrafamilial sexual abuse of female children. Child Abuse Negl 1983;7:133–46. 10.1016/0145-2134(83)90065-0 [DOI] [PubMed] [Google Scholar]
- 30. Barrios YV, Gelaye B, Zhong Q, et al. Association of childhood physical and sexual abuse with intimate partner violence, poor general health and depressive symptoms among pregnant women. PLoS One 2015;10:e0116609 10.1371/journal.pone.0116609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Coid J, Petruckevitch A, Feder G, et al. Relation between childhood sexual and physical abuse and risk of revictimisation in women: a cross-sectional survey. Lancet 2001;358:450–4. 10.1016/S0140-6736(01)05622-7 [DOI] [PubMed] [Google Scholar]
- 32. Bensley L, Van Eenwyk J, Wynkoop Simmons K. Childhood family violence history and womens risk for intimate partner violence and poor health. Am J Prev Med 2003;25:38–44. 10.1016/S0749-3797(03)00094-1 [DOI] [PubMed] [Google Scholar]
- 33. Fanslow J, Silva M, Robinson E, et al. Violence during pregnancy: associations with pregnancy intendedness, pregnancy-related care, and alcohol and tobacco use among a representative sample of New Zealand women. Aust N Z J Obstet Gynaecol 2008;48:398–404. 10.1111/j.1479-828X.2008.00890.x [DOI] [PubMed] [Google Scholar]
- 34. Bailey BA, Daugherty RA. Intimate partner violence during pregnancy: incidence and associated health behaviors in a rural population. Matern Child Health J 2007;11:495–503. 10.1007/s10995-007-0191-6 [DOI] [PubMed] [Google Scholar]
- 35. Anderson BA, Marshak HH, Hebbeler DL. Identifying intimate partner violence at entry to prenatal care: clustering routine clinical information. J Midwifery Womens Health 2002;47:353–9. 10.1016/S1526-9523(02)00273-8 [DOI] [PubMed] [Google Scholar]
- 36. Caetano R, McGrath C, Ramisetty-Mikler S, et al. Drinking, alcohol problems and the five-year recurrence and incidence of male to female and female to male partner violence. Alcohol Clin Exp Res 2005;29:98–106. 10.1097/01.ALC.0000150015.84381.63 [DOI] [PubMed] [Google Scholar]
- 37. Gilbert L, El-Bassel N, Chang M, et al. Substance use and partner violence among urban women seeking emergency care. Psychol Addict Behav 2012;26:226–35. 10.1037/a0025869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Campbell JC. Health consequences of intimate partner violence. Lancet 2002;359:1331–6. 10.1016/S0140-6736(02)08336-8 [DOI] [PubMed] [Google Scholar]
- 39. Matcham F, Carroll A, Chung N, et al. Smoking and common mental disorders in patients with chronic conditions: An analysis of data collected via a web-based screening system. Gen Hosp Psychiatry 2017;45:12–18. 10.1016/j.genhosppsych.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 40. Martin SL, Li Y, Casanueva C, et al. Intimate partner violence and women’s depression before and during pregnancy. Violence Against Women 2006;12:221–39. 10.1177/1077801205285106 [DOI] [PubMed] [Google Scholar]
- 41. Wu Q, Chen HL, Xu XJ. Violence as a risk factor for postpartum depression in mothers: a meta-analysis. Arch Womens Ment Health 2012;15:107–14. 10.1007/s00737-011-0248-9 [DOI] [PubMed] [Google Scholar]
- 42. Campo M. Domestic and family violence in pregnancy and early parenthood Overview and emerging interventions. 2016. https://aifs.gov.au/cfca/sites/default/files/publication-documents/cfca-resource-dv-pregnancy.pdf.
- 43. Woods SJ, Hall RJ, Campbell JC, et al. Physical health and posttraumatic stress disorder symptoms in women experiencing intimate partner violence. J Midwifery Womens Health 2008;53:538–46. 10.1016/j.jmwh.2008.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, et al. The impact of physical, psychological, and sexual intimate male partner violence on women’s mental health: depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. J Womens Health 2006;15:599–611. 10.1089/jwh.2006.15.599 [DOI] [PubMed] [Google Scholar]
- 45. Witt WP, Wisk LE, Cheng ER, et al. Poor prepregnancy and antepartum mental health predicts postpartum mental health problems among US women: a nationally representative population-based study. Womens Health Issues 2011;21:304–13. 10.1016/j.whi.2011.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Krulewitch CJ, Pierre-Louis ML, de Leon-Gomez R, et al. Hidden from view: violent deaths among pregnant women in the District of Columbia, 1988-1996. J Midwifery Womens Health 2001;46:4–10. 10.1016/S1526-9523(00)00096-9 [DOI] [PubMed] [Google Scholar]
- 47. Campbell JC, Glass N, Sharps PW, et al. Intimate partner homicide: review and implications of research and policy. Trauma Violence Abuse 2007;8:246–69. 10.1177/1524838007303505 [DOI] [PubMed] [Google Scholar]
- 48. Ogboghodo EO, Omuemu VO. Prevalence, pattern and determinants of domestic violence among ante-natal clinic attendees in a secondary health facility in Benin City, Edo State. J Prim Health Care 2016;28:65–75. [Google Scholar]
- 49. Salmon D, Baird KM, White P. Women’s views and experiences of antenatal enquiry for domestic abuse during pregnancy. Health Expect 2015;18:867–78. 10.1111/hex.12060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Subramanian S, Katz KS, Rodan M, et al. An integrated randomized intervention to reduce behavioral and psychosocial risks: pregnancy and neonatal outcomes. Matern Child Health J 2012;16:545–54. 10.1007/s10995-011-0875-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cha S, Masho SW. Discussions about intimate partner violence during prenatal care in the United States: the role of race/ethnicity and insurance status. Matern Child Health J 2014;18:1413–22. 10.1007/s10995-013-1381-z [DOI] [PubMed] [Google Scholar]
- 52. Dunn LL, Oths KS. Prenatal predictors of intimate partner abuse. J Obstet Gynecol Neonatal Nurs 2004;33:54–63. 10.1177/0884217503261080 [DOI] [PubMed] [Google Scholar]
- 53. New perspectives on perineal massage, and pushing. Contemporary OB/GYN 2006;51. [Google Scholar]
- 54. Vintzileos A, Ananth CV, Smulian JC, et al. The impact of prenatal care on postneonatal deaths in the presence and absence of antenatal high-risk conditions. Am J Obstet Gynecol 2002;187:1258–62. 10.1067/mob.2002.127143 [DOI] [PubMed] [Google Scholar]
- 55. Shah PS, Shah J. Maternal Exposure to Domestic Violence and Pregnancy and Birth Outcomes: A Systematic Review and Meta-Analyses. J Womens Health 2010;19:2017–31. 10.1089/jwh.2010.2051 [DOI] [PubMed] [Google Scholar]
- 56. Donovan BM, Spracklen CN, Schweizer ML, et al. Intimate partner violence during pregnancy and the risk for adverse infant outcomes: a systematic review and meta-analysis. BJOG 2016;123:1289–99. 10.1111/1471-0528.13928 [DOI] [PubMed] [Google Scholar]
- 57. Bailey BA. Partner violence during pregnancy: prevalence, effects, screening, and management. Int J Womens Health 2010;2:183–97. 10.2147/IJWH.S8632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Spangaro J, Koziol-McLain J, Zwi A, et al. Deciding to tell: qualitative configurational analysis of decisions to disclose experience of intimate partner violence in antenatal care. Soc Sci Med 2016;154:45–53. 10.1016/j.socscimed.2016.02.032 [DOI] [PubMed] [Google Scholar]
- 59. Miller E, McCaw B, Humphreys BL, et al. Integrating intimate partner violence assessment and intervention into healthcare in the United States: a systems approach. J Womens Health 2015;24:92–9. 10.1089/jwh.2014.4870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Rollans M, Schmied V, Kemp L, et al. Negotiating policy in practice: child and family health nurses' approach to the process of postnatal psychosocial assessment. BMC Health Serv Res 2013;13:133 10.1186/1472-6963-13-133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. O’Doherty L, Hegarty K, Ramsay J, et al. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst Rev 2015:CD007007 10.1002/14651858.CD007007.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Baird KM, Mitchell T. Using feminist phenomenology to explore women’s experiences of domestic violence in pregnancy. British Journal of Midwifery 2014;22:418–26. 10.12968/bjom.2014.22.6.418 [DOI] [Google Scholar]
- 63. Brown SJ, McDonald EA, Krastev AH. Fear of an intimate partner and women’s health in early pregnancy: findings from the Maternal Health Study. Birth 2008;35:293–302. 10.1111/j.1523-536X.2008.00256.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.