The National Early Warning Score Development and Implementation Group (NEWSDIG) was a group convened by the Royal College of Physicians to develop a new early warning score (EWS) system that would be validated, easily learnt and used, and widely implemented. The Acute Medicine Task Force1 that reported in 2007 noted that ‘a number of basic assessment tools or “early warning scores” are currently in use nationwide’ and commented that ‘there is no justification for the continued use of multiple different early warning scores to assess illness severity’. It went on to recommend that
…the physiological assessment of all patients should be standardised across the NHS with the recording of a minimum clinical data set resulting in a ‘NHS early warning (NEW) score’. This will provide a standardised record of illness severity and urgency of need, from first assessment and throughout the patient journey.
The intention was to deliver a ‘track and trigger’ tool that could provide consistency of assessment of illness severity across the NHS and provide a valuable baseline from which to evaluate the patient's clinical progress. The ‘track’ part of this is the identification of relevant physiological parameters that may become abnormal during ill health – the ‘trigger’ being the score that results in an adequate clinical response to these changes. NEWSDIG recognised that many individual hospitals and Trusts were using their own locally developed EWS and that the group had to develop a system which would be evidence-based and properly validated. NEWSDIG incorporated membership from many stakeholder groups including patients, the national outreach forum, critical care and acute medicine medical and nursing staff, and the ambulance service. It reviewed many of the existing EWS systems being used to ensure that the NEWS incorporated as many of the best, evidence-based elements as possible. The prototype NEWS was then tested against a large vital signs database to ensure that it did reveal those patients who were likely to require clinical intervention.
Although NEWSDIG started in 2009, it only reported its work in 2012,2 as care was taken to develop and validate NEWS, but also to ensure that NEWS was user-friendly and easily learnt. To facilitate the latter it was felt that the development of an e-learning package would be the most effective way of widespread access to adequate training. This may be found at http://tfinews.ocbmedia.com/home/ and demonstrates the ease with which the use of NEWS may be learnt. The tool itself had to be user friendly with physiological abnormalities easily identified and scored, thus a colour-coded chart was developed (Fig 1).
Fig 1.
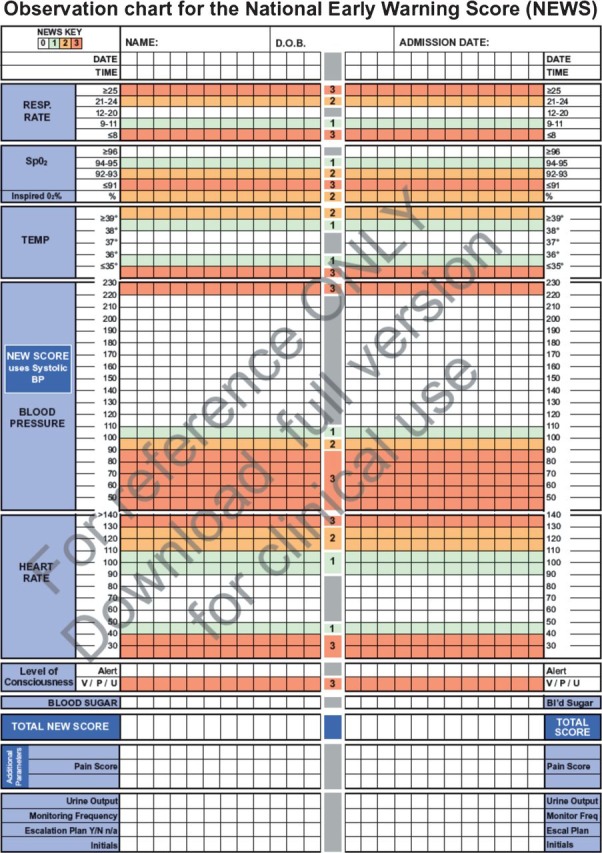
The NEWS observation chart. This chart is reproduced here for reference only. For clinical use, please visit www.rcplondon.ac.uk/resources/national-early-warning-score-news where full-sized versions with instructions and guidance may be downloaded.
As NEWS has been released3 and promoted for use, it seems that the intention of the NEWSDIG group remains relatively unclear. A recent British Medical Journal editorial was subtitled ‘A new standard should help identify patients in need of critical care’.4 In many ways this misses the point of NEWS, simply because of the phrase ‘critical care’. Implicit in this phrase are the separate departments and teams within the hospital that offer augmented levels of care. The use of NEWS has to be far wider than that. The intention should be to detect patients both at presentation and, by continued surveillance, at any time during their hospital stay who need simple but prompt intervention to correct their perturbed physiology and, hopefully, by prompt local intervention prevent the need for transfer to a critical care environment. The ease of use of the NEWS system has to be supplemented, of course, by locally approved and effective response mechanisms. Recording of NEWS is only the first step and involvement of professionals with appropriate competences, that have previously been defined, has to be in place to facilitate the correct response for the patients’ needs. While this may involve critical care and outreach teams there must be an emphasis on development of these competences as widely as possible. These competences must also include recognition when referral for a more senior member of the team is required. The NEWSDIG report also states that NEWS is not designed to replace all other assessment systems but should be used to augment processes that are already proven and in existence. Concern has been expressed about specific patient groups including those experiencing neurological injury. It should be noted that NEWS has not been promoted to replace well established systems such as the Glasgow Coma Scale.5 Similarly there is no intention that the use of NEWS should supplant the most important face-to-face interaction between the clinician and the patient. This is particularly pertinent as it is well recognised that there are circumstances where patients become critically unwell without necessarily showing abnormal physiological signs.
Despite these caveats it is accepted that prompt recognition of physiological deterioration saves lives. There are, however, very few clinical trials of early warning scores.6 Adoption of NEWS with review of the effectiveness of this tool on a large scale can potentially provide assurance of the relevance of this tool in quality patient care. The support for the tool has been remarkable.7 We now face the challenge of getting NEWS implemented. The effectiveness of any EWS is dependent on accuracy of measurement of the physiological parameters themselves and the subsequent recording and score calculation. Electronic solutions should be forthcoming to help with the latter. Support from many organisations and individual clinicians has been demonstrated but we have to ensure that clinical staff moving from post to post in the NHS don't have to learn a new EWS with each new hospital and that patients will indeed benefit from a system that is used reliably and completely. It is to be hoped that the ease of training, and of use, will make it attractive for wide adoption, and then we can really see a step change towards better management of the acutely ill patient.
References
- 1.Royal College of Physicians. Acute medical care: the right person, in the right setting—first time. London: RCP; 2007. [Google Scholar]
- 2.Royal College of Physicians. National Early Warning Score (NEWS): Standardising the assessment of acute illness severity in the NHS. Report of a working party. London: RCP; 2012. [Google Scholar]
- 3.Hawkes N. Royal College recommends national system to recognise deteriorating patients. BMJ. 2012;345:e5041. doi: 10.1136/bmj.e5041. [DOI] [PubMed] [Google Scholar]
- 4.McGinnley A. Pearse R. A national early warning score for acutely ill patients. BMJ. 2012;345:e5310. doi: 10.1136/bmj.e5310. [DOI] [PubMed] [Google Scholar]
- 5.Teasdale G. Rapid response 14 August 2012. Royal college recommends national system to recognise deteriorating patients. BMJ. 2012;345:e5041. doi: 10.1136/bmj.e5041. [DOI] [PubMed] [Google Scholar]
- 6.Kyriacos U. Jelsma J. Jordan S. Monitoring vital signs using early warning scoring systems: a review of the literature. Journal of Nursing Management. 2011;19:311–320. doi: 10.1111/j.1365-2834.2011.01246.x. [DOI] [PubMed] [Google Scholar]
- 7.Kmietowicz Z. Doctors urge hospitals to adopt national system for scoring acutely ill patients. BMJ. 2012;345:e513. doi: 10.1136/bmj.e5135. [DOI] [PubMed] [Google Scholar]


