Abstract
The decision to perform cardiopulmonary resuscitation (CPR) remains one of the most important and difficult decisions a physician must make. This study examined differences in CPR decision making among senior hospital clinicians. A questionnaire was sent out to consultants and specialist registrars in general medicine, elderly care and intensive care in a large UK district general hospital, with anonymous returns. Short clinical scenarios were presented, and participants stated their CPR decision and their confidence level. In total, 86 questionnaires were sent out and 54 replies (63%) were received. There were significant differences between specialties in making the decision to perform CPR and the confidence in doing so, with three cases producing polarised results within the specialties, despite equal confidence in the decision. There is lack of consensus with the CPR decisions made between specialties and within them. Formal training in recognition of futility should be encouraged for all clinicians.
Key Words: cardiopulmonary resuscitation, decisions, education, prediction models
Introduction
The decision to perform cardiopulmonary resuscitation (CPR) in the event of cardiorespiratory arrest remains one of the most important decisions a physician must make and is often one of the most difficult. There are guidelines supporting the clinical standards and ethical aspects of CPR,1–3 and there is training for doctors to recognise patients at risk of cardiorespiratory arrest,4,5 however, there is little if any formal undergraduate or postgraduate training or guidance in recognising whether CPR was not in a patients best interest. The European Resuscitation Council (ERC) and Resuscitation Council (UK) (RCUK), and many NHS trusts at a local level, do provide guidance and discussion around this difficult subject,2,6 but scrutiny of such guidance is often left to an individual's discretion and is not compulsory. The joint guidelines issued by the British Medical Association, RCUK and Royal College of Nursing in 2001 provide ethical and legal backing behind decisions not to resuscitate, but do not offer clinical guidance in identification of the appropriate patients.3 Recent National Institute for Health and Clinical Excellence (NICE) guidelines on management of the acutely ill adult in hospital fail to recommend that a decision on CPR should be made as part of routine best care for patients.7 The RCUK guidelines have recognised the importance of a doctors' early education in acute and critical care, but this is not yet widespread practice in the UK.6,8
There have been many studies published in the past on survival after in-hospital cardiac arrest, but far less on predictors of failure. The use of morbidity scores to predict unsuccessful CPR has provided some objective tools in the identification of patients who will not survive CPR. The pre-arrest morbidity score (PAM),9 prognosis after resuscitation score (PAR),10 and the modified PAM index (MPI)11 have been proposed, and subsequently independently validated in a UK hospital.12 Above a certain threshold, all of these models have 100% specificity, but with low sensitivity, ie they cannot predict specifically who will not survive CPR, but, over a given score, do reliably predict failure.
A previous study in a UK hospital identified that 97% of junior doctors felt that some CPR decisions where inappropriate, and in 48% of cases the main reason given was failure of senior medical staff to make a ‘do not resuscitate’ order.13 Furthermore, a medical emergency team in an Australian hospital decided that 23% of cases they were called to as an emergency should not be for resuscitation.14 There has been recent debate with regard to the benefits and ethics of attempts at resuscitation in the frail and elderly, with a prevailing opinion that the current guidelines would benefit from review.15
This study was designed as a pilot to establish if there were differences in attitudes and confidence in decision making among senior clinicians in general internal medicine (GIM), elderly care (EC), and intensive care medicine (ICM) in CPR decisions using six fictitious clinical scenarios.
Methods
A questionnaire was sent out to all consultants, staff grades, associate specialists and specialist registrars (SpRs) in GIM, EC and ICM of a large district general hospital (DGH) in the UK. Specialist registrars were included because they are authorised to make do not attempt resuscitation (DNAR) orders out of hours within the trust, with appropriate senior discussion if necessary. This process was via internal mail and the responses were anonymous. Participants were invited to circle a ‘Yes’ or ‘No’ beside the statement ‘This patient should be for CPR’ after each of six short clinical scenarios (Box 1). The questionnaire was not designed to be specifically discriminatory; each scenario was based around plausible, common on-call cases. Clinicians were then asked to rate their confidence on a scale of 1 to 5, with 1 as ‘not at all’ and 5 as ‘very’ after each CPR decision. Contributors where able to add free text to the replies.
Data were calculated using Microsoft Access (2000) and SPSS version 14.0. Data were analysed using the Mann Whitney U-test; the term ‘significant’ refers to a p value of <0.05.
After the initial breakdown of results, staff grades and associate specialists were placed in the consultant group (as the on-call responsibilities are the same). Those who failed to identify their specialty were excluded from final analysis. Case-by-case analysis of the decisions and level of confidence were made between consultants and SpRs (all specialties), and between specialties with both grades combined.
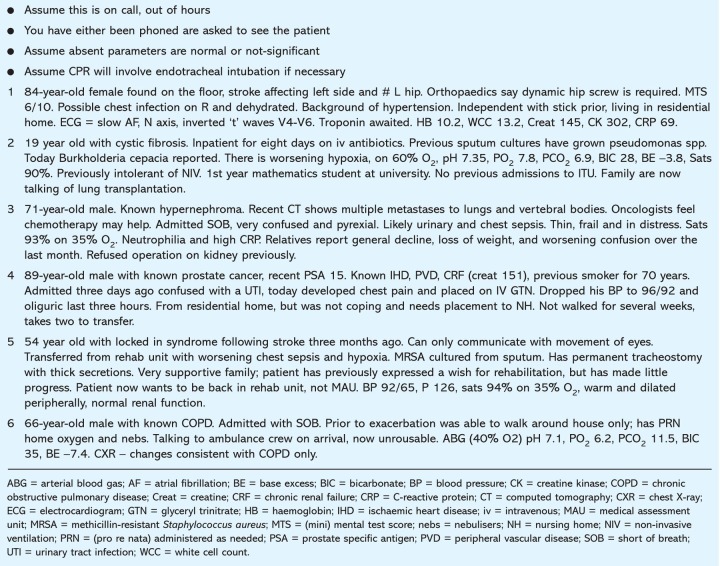
Box 1. Summary of the six scenarios.
Pre-arrest scores for prediction of outcome after CPR were calculated for each case scenario using the three scoring systems discussed above. Absent values or information were scored as normal.
Results
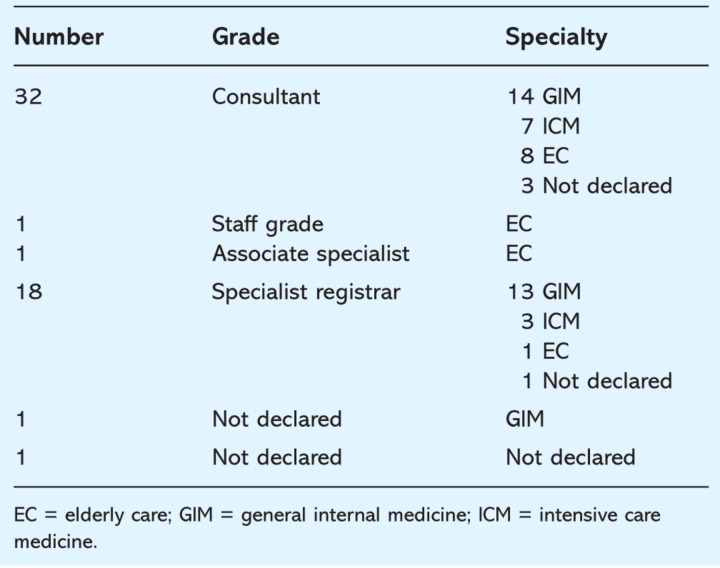
In total, 86 questionnaires were sent out and 54 replies were received, a response rate of 62.8%. A full breakdown is provided in Table 1.
Table 1.
Breakdown of respondents.
Cardiopulmonary resuscitation decisions
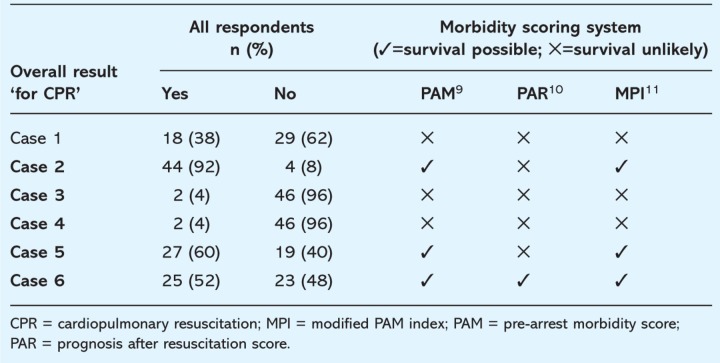
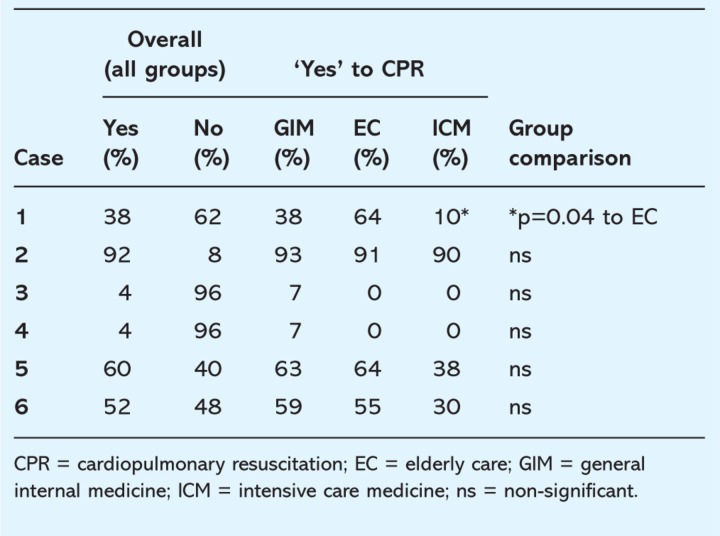
Table 2 provides the overall results of all replies in this survey, coupled with the predicted outcome using the PAM, PAR and MPI models for each case. In Cases 3 and 4, two physicians in each case felt CPR would be appropriate however these were not the same two for both cases. A case-by-case breakdown is summarised in Table 3. Further sub-analysis by grade and specialty (eg comparing GIM SpRs with ITU SpRs) was not possible due to the low numbers.
Table 2.
Overall responses (all groups) with results of predicted outcome from morbidity scores for each case.
Table 3.
Comparison within groups and confidence of decision with each case.
Confidence
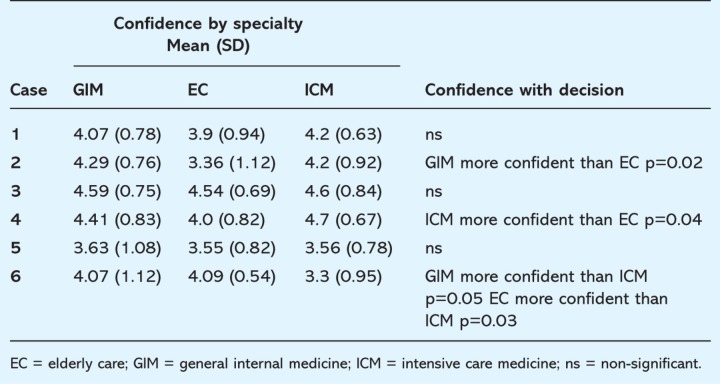
A summary of confidence in the CPR decision, broken down by specialty, is provided in Table 4. In Cases 1, 5 and 6 there was no significant difference between confidence in the decision, whether it was ‘Yes’ or ‘No’, regardless of specialty. In the remaining cases, the numbers in either the ‘Yes’ or ‘No’ group were too small for statistical comparison (data not provided). There were no significant differences between consultants and SpRs with decision or confidence throughout all six cases (data not provided).
Table 4.
Mean confidence in decision by speciality and case.
Discussion
This is the first paper that examines differences in attitudes to resuscitation decisions between different medical specialties among middle and senior grade doctors. Our study has shown there was no significant difference between consultants and SpRs in their decision making and degrees of confidence in doing so, this is encouraging and reflects congruity of attitudes and perhaps practice. All of the specialties showed high levels of confidence, mean 4.05 (range 3.3–4.7). This is reassuring in that the clinicians called upon to make a decision on CPR feel confident to do so. What is concerning, however, is that many of the individuals concluded upon opposing decisions, despite equal confidence in them. This is apparent both between, and within, the three groups of clinicians.
The cases presented were all fictitious, nevertheless, they were all plausibly based around common medical problems that are dealt with in a DGH. The exact nature of each clinical case and an individual's response should not be of concern; however some of the issues arising from the cases are discussed below.
Cases 3 and 4 produced results overwhelmingly in favour of DNAR, and this was congruent with the pre-arrest scores that reflected no chance of success in these scenarios. It is encouraging therefore that clinicians are able to recognise futility and act upon it. Conversely, Cases 1, 5 and 6 all produced polarised results within, and between, groups. In each of the cases the confidence in the decision made, be it ‘Yes’ or ‘No’, was not significantly different, regardless of which group a physician was in. This means that despite different decisions, each party felt equally confident in them. In Case 6 the pre-arrest scores all suggested a chance of success, and yet 48% of the cohort favoured a DNAR order.
In Case 1, ICM were significantly more likely to decline an attempt at CPR; this is with equal confidence in the decision compared to EC, who, as a group, were more inclined to favour CPR (EC 64% ‘Yes’, ICM 10% ‘Yes’; p=0.04). In the same scenario, GIM's inclination towards declining CPR also suggested a trend of disparity with EC, although this did not reach significance (GIM 38% ‘Yes’, EC 64% ‘Yes’; p=0.1). In Case 1 there was a significant tendency toward ICM refusing CPR, and in Cases 5 and 6, there was a trend toward the same, but this was not significant. It is concerning that a group of hospital physicians would appear to have differing views and perhaps practice to others within the hospital. However, it may be argued that ICM are in the strongest position to make an informed decision with regard to ceilings of treatment, as many cases of successful CPR will be likely to be admitted to the intensive care unit. This therefore highlights possible deficiencies in training and expectations between physicians with regard to what level of treatment is reasonable, both ethically and clinically, to offer.
Case 2 presented a 19 year old with cystic fibrosis, chest sepsis and respiratory failure. The majority of all specialties agreed that CPR should be attempted in this instance (92%), with no significant difference between the groups. Elderly care were significantly less confident in their decision than the other specialties. This is perhaps not surprising, as one would not expect an elderly care physician to have much experience in this setting. It can be argued that because this finding could be anticipated, this provides some validation to this otherwise unvalidated model.
At present there is increasing training for doctors and nurses to recognise ‘at risk’ patients to try to avoid cardiopulmonary arrest. While some guidance surrounding the issues of withholding CPR does exist, there is no formal training for clinicians (as part of, for instance, a postgraduate core curriculum) on recognising where attempts at CPR, and the treatment required afterwards, may not be in a patients' best interest. Current efforts to enhance undergraduate and postgraduate training in acute and critical care are designed to augment recognition of the critically ill; it is desirable that this training should also inform clinicians in recognition of futility in the context of critical illness.
In the absence of a clear DNAR order, doctors are mandated to provide CPR in the event of cardiopulmonary arrest. In no other area of medicine is there a mandate to provide treatment that is very unlikely to succeed, but it is morally and ethically correct and reflects Article 2 of the Human Rights Act 1998 which states the right to life.16 Equally, however, clinicians must recognise where treatment would not confer benefit, and identify patients for whom cardiopulmonary arrest is an anticipated terminal event and in whom CPR is inappropriate.1,6 Indeed, under Article 3 of the Human Rights Act 1998 an individual has a right not to have inhuman or degrading treatment.16 The European Resuscitation Council guidelines state that ‘a doctor is required to only provide treatment that is likely to benefit the patient, and not required to provide treatment that would likely to be futile’.2 While it is accepted that in many cases there is no definite correct answer, this study focused on the clinical aspects of decision making for CPR, and yet showed incongruity within and between specialties. The differences of opinion expressed with equal confidence are a reflection of the difficulties in making such judgements, and in this case show that the physicians involved felt equally confident that they had made the right choice, regardless of its nature.
This has raised important issues that require further investigation and validation in a larger cohort of doctors, ideally in multicentre collaboration of general hospitals with GIM on call. This would allow appropriate power calculations and larger numbers of respondents, and thus may clarify some of the identified trends that failed to reach statistical significance. This study was designed as a pilot, and has shown that this postal format produces a good level of return (63%), and no doubt reflects interest in the important ethical issues that this raises. Future research should also attempt to examine the reasons or discriminators that lead to a clinician making a DNAR order. In this study, three cases were non-discriminatory, and three produced clearly polarised results; both instances may provide useful information with regards the clinicians' attitude towards, for instance, age, pre-morbid state or diagnosis of cancer. Such information may then enable and facilitate training in CPR decisions and recognition of futility. Additionally, the possible effect of the PAMs should be examined, to assess if they influence clinicians' behaviour in decision making.
In interpretation of this study it is important to recognise some potential limitations. It is accepted that this form of questionnaire is artificial and is no substitute to proper clinical assessment by the physician. Additionally, the scenarios did use abbreviations and terminology that were not fully explained; nevertheless, these were all based on routinely used common terminology. The effect of a clinicians' parent specialty will no doubt have a bearing on the decisions made, and this may well have been a factor in the scenarios. In most DGHs in the UK, however, clinicians are called upon to provide GIM on-call cover, and as such should have a broad experience in general medical emergencies. None of the cases presented expressed the patients' or family wishes with respect to CPR, this was a deliberate omission as the investigators were keen to focus on clinical issues. Two respondents commented in free text that they would seek the families' views for all cases, with a further 10 comments about seeking the opinion of the patient and family within the individual scenarios. This low number should be interpreted with caution because the authors did not specifically seek views on this.
To date, no PAM scoring systems have been widely adopted into clinical practice within the UK as a means to help guide clinicians in decision making for the appropriateness of CPR. Recent NICE guidance has encouraged the use of physiological scoring systems in the acute setting.7 Such systems have proven useful in the prediction of cardiopulmonary arrest, but it could be argued that reliable prediction of failure is of greater benefit to clinicians; if there is reasonable chance of success it should be taken, but if there is no chance it is ethically and morally wrong to continue to provide treatment that may be inhuman or degrading. Further efforts to devise simple, validated models that will reliably predict failure in cardiac arrest should be strongly encouraged.
Conclusion
There is no clear consensus within this group of clinicians with the resuscitation decisions made, both between specialties and within them. Furthermore, each decision is made with equal confidence, suggesting that each clinician feels that they are equally correct. Currently, the decision to not attempt CPR by a clinician is a subjective one. This study has demonstrated clear disparities in the subjective decisions made by physicians. There is therefore a strong argument for the development of validated, objective prognostic scoring systems that are relevant and easily applicable to everyday practice in hospital. There is further need for training in recognition of futility, or when an escalation in therapy, such as admission to intensive care, becomes inappropriate. Such training should play a more important role as part of the curricula for courses that teach emergency medicine and resuscitation, and indeed should be an integral part of specialty training for clinicians.
Acknowledgement
The authors are grateful to Professor Gary Smith for his advice in preparation of this article.
Reference
- 1.Gabbott D. Smith G. Mitchell S, et al. Cardiopulmonary resuscitation standards for clinical practice and training in the UK. Resuscitation. 2005;64:13–9. doi: 10.1016/j.resuscitation.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Baskett PJ. Steen PA. Bossaert L. European Resuscitation Council guidelines for resuscitation 2005. Section 8. The ethics of resuscitation and end-of-life decisions. Resuscitation. 2005;67(Suppl 1):S171–S80. doi: 10.1016/j.resuscitation.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Decisions Relating to Cardiopulmonary Resuscitation: a joint statement from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing. J Med Ethics. 2001;27:310–6. doi: 10.1136/jme.27.5.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Resuscitation Council (UK) Advanced life support course provider manual. 4th edn. London: Resuscitation Council & ERC; 2004. [Google Scholar]
- 5.Smith G. ALERT – acute life threatening events recognition and treatment, course manual. Portsmouth: University of Portsmouth; 2003. [Google Scholar]
- 6.Smith G. Prevention of in hospital cardiac arrest and decisions about cardiopulmonary resuscitation. Resuscitation Council (UK) guidelines 2005. London: Resuscitation Council (UK); 2005. [Google Scholar]
- 7.National Institute for Health and Clinical Excellence. Acutely ill patients in hospital. Recognition and response to acute illness in adults in hospital. London: NICE; 2007. [PubMed] [Google Scholar]
- 8.Royal College of Anaesthetists, Royal College of Physicians, Intensive Care Society, Resuscitation Council (UK) Cardiopulmonary resuscitation – standards for clinical practice and training. London: Resuscitation Council (UK); 2004. [Google Scholar]
- 9.George AL., Jr Folk BP., 3rd Crecelius PL. Campbell WB. Pre-arrest morbidity and other correlates of survival after in-hospital cardiopulmonary arrest. Am J Med. 1989;87:28–34. doi: 10.1016/s0002-9343(89)80479-6. [DOI] [PubMed] [Google Scholar]
- 10.Ebell MH. Prearrest predictors of survival following in-hospital cardiopulmonary resuscitation: a meta-analysis. J Fam Pract. 1992;34:551–8. [PubMed] [Google Scholar]
- 11.Dautzenberg PL. Broekman TC. Hooyer C. Schonwetter RS. Duursma SA. Review: patient-related predictors of cardiopulmonary resuscitation of hospitalized patients. Age Ageing. 1993;22:464–75. doi: 10.1093/ageing/22.6.464. [DOI] [PubMed] [Google Scholar]
- 12.Bowker L. Stewart K. Predicting unsuccessful cardiopulmonary resuscitation (CPR): a comparison of three morbidity scores. Resuscitation. 1999;40:89–95. doi: 10.1016/S0300-9572(99)00008-8. [DOI] [PubMed] [Google Scholar]
- 13.Morgan R. Westmoreland C. Survey of junior hospital doctors' attitudes to cardiopulmonary resuscitation. Postgrad Med J. 2002;78:413–5. doi: 10.1136/pmj.78.921.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parr MJ. Hadfield JH. Flabouris A. Bishop G. Hillman K. The Medical Emergency Team: 12 month analysis of reasons for activation, immediate outcome and not-for-resuscitation orders. Resuscitation. 2001;50:39–44. doi: 10.1016/S0300-9572(01)00323-9. [DOI] [PubMed] [Google Scholar]
- 15.Conroy SP. Luxton T. Dingwall R. Harwood RH. Gladman JR. Cardiopulmonary resuscitation in continuing care settings: time for a rethink? BMJ. 2006;332:479–82. doi: 10.1136/bmj.332.7539.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.British Medical Association. The impact of the Human Rights Act 1998 on medical decision making. London: BMA; 2000. [Google Scholar]