Abstract
The burden of liver disease in the UK is increasing and much of this is managed in district general hospitals (DGHs). Previous studies of liver services have focused on specialist units. This study assessed the provision of liver services in non-specialist units. A questionnaire-based survey was conducted to assess resources, staffing and clinical management of liver disease. Replies were received from 61 consultant gastroenterologists working in DGHs across the UK. The data show inadequate consultant numbers and limited availability of nurse specialists, hepatobiliary pathologists and radiologists. There is marked variability in the management of hepatitis C, variceal bleeding and hepatorenal syndrome. Liver databases and outcomes are rarely kept. There are significant shortfalls in the provision of liver services across DGHs. This supports the need for managed clinical networks and data collection as proposed in the National Plan for Liver Services.
Key Words: health manpower (N05.300.420.400), liver diseases (MeSH C06.552), quality of health care (N05.715)
Introduction
The burden of liver disease is increasing in the UK, as illustrated by the recent rise in deaths from cirrhosis secondary to alcohol and hepatitis C.1–3 In 2001, the Department of Health identified areas for specialist commissioning for hepatology.4 With only six transplant and 28 non-transplant liver centres in England, the bulk of liver medicine will initially be delivered in district general hospitals (DGHs).5 Little is known of the capacity of these hospitals to deal with the increasing demands of liver disease.
Methods
A questionnaire was sent to one consultant gastroenterologist in each of the 116 UK DGHs. Consultants were identified from a list of members of the British Society of Gastroenterology (BSG), and the first listed member from each hospital was included in the survey. In addition, the questionnaire was sent to a non-gastroenterologist physician in the same hospital to assess the extent of hepatology provision by general physicians. Information was sought about staffing levels, facilities and the management of acute and chronic conditions, namely variceal bleeding, hepatorenal syndrome, hepatitis C and autoimmune hepatitis.
Results
In total, 61 gastroenterologists (53%) and 26 non-gastroenterologists (22%) replied to the questionnaire. In view of the low return rate from general physicians, the results quoted refer to gastroenterologists' responses unless stated otherwise. The median hospital catchment population was 250,000 (range 100,000–800,000). The median number of consultant gastroenterologists per hospital was three (range 1–7), and a median number per 100,000 population of 1.0 (0.7–2.0). Only one hospital had a consultant who specialised exclusively in hepatology, and five (8%) had a declared interest. Of the gastroenterology consultants, 44% had not spent any time training in pure hepatology as a registrar or senior registrar.
Workload/staffing
Liver disease was estimated to account for a mean of 20% of outpatient and inpatient workload. Of the consultants, 88% felt that their workload due to liver disease was increasing and 26% of them held specific liver clinics. Non-gastroenterologist physicians estimated that liver disease accounted for a mean of 9% (range 0–60%) of their inpatient work and 6% (0–40%) of their outpatient work.
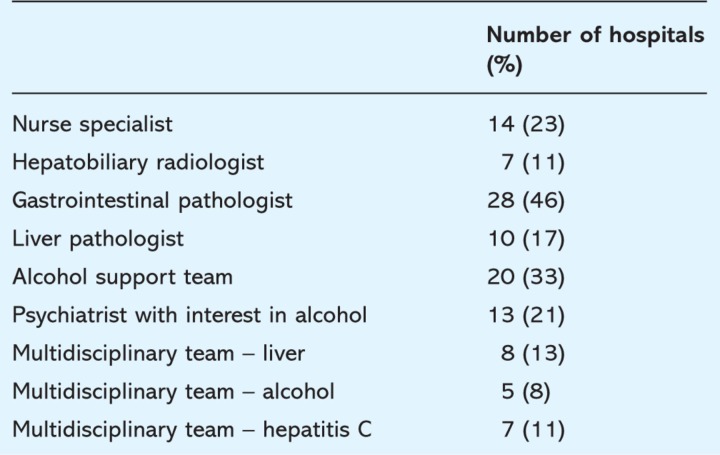
Table 1 shows the support facilities available to consultants from other colleagues. Where present, nurse specialists were most commonly employed to assist with management of hepatitis C (11%), followed by alcohol-related illnesses (2%). A quarter of these posts were funded by drug companies, with the remainder funded by the trusts.
Table 1.
Availability of allied health care professionals.
Facilities
Of the responses, 36 consultants (59%) felt that access to renal services for liver patients was easy. However, 33% felt that their local intensive care unit (ICU) was often reluctant to accept liver patients. The most common reason quoted for this reluctance was a perceived poor outcome (28%), with some feeling that intensivists lacked expertise in liver disease patients (15%) or discriminated against patients with alcoholic liver disease (13%).
Liver biopsies
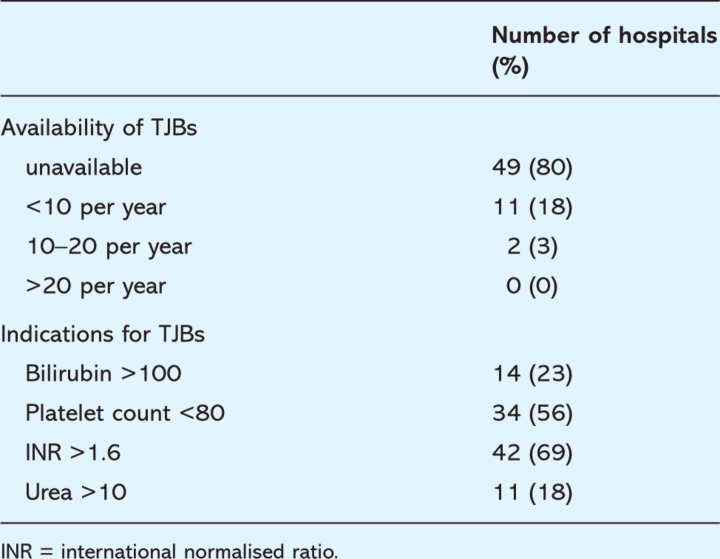
Ultrasound-assisted liver biopsies were available routinely in 41 hospitals (67%) but were restricted to targeted lesions in almost a third (18 hospitals, 30%). As a result, ‘blind’ biopsies were performed by some consultants (39%) and registrars (16%). Table 2 shows the availability of transjugular liver biopsies (TJBs), and the perceived indications for requesting a transjugular approach. The number of TJBs performed annually at each centre was small (median 3, range 1–18).
Table 2.
Availability of transjugular liver biopsies (TJBs)
Variceal haemorrhage
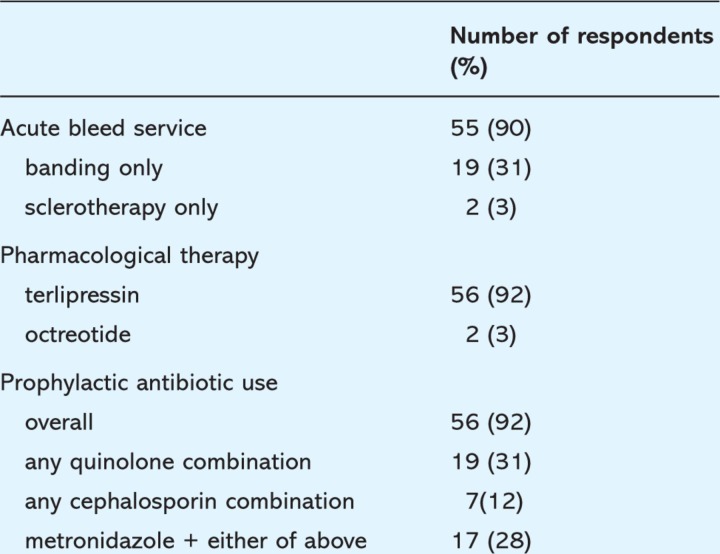
Table 3 shows the acute management of variceal haemorrhage. The use of terlipressin has been widely adopted, although a small number continue to use octreotide (3%) or vasopressin (2%). Vasoconstrictor therapy is continued for a median of three days (range 2–7 days). Despite this, a median of 3.5 Sengstaken–Blakemore tubes (range 0–20) are inserted at each hospital per year.
Table 3.
Acute management of variceal haemorrhage.
In the event of a re-bleed, 92% of respondents would repeat the endoscopy, with 69% considering transjugular intrahepatic portosystemic shunt (TIPSS) insertion and 79% considering referral to a liver centre. For gastric varices, 67% of consultants would refer for TIPSS, with 39% considering banding or injection, and 20% opting for glue injection. Only seven consultants (11%) kept outcome data on variceal haemorrhage. However, respondents estimated mortality to be 20% range (5–50%).
Hepatorenal syndrome
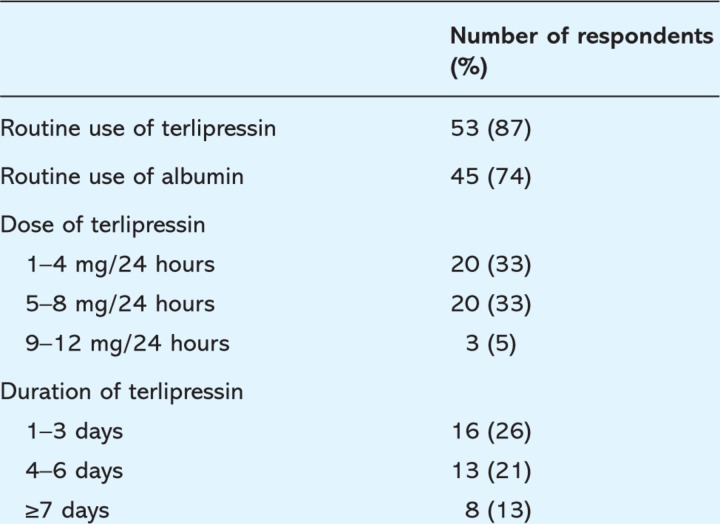
Table 4 shows the management of hepatorenal syndrome (HRS). A median of 10 (1–50) cases per unit are seen each year. The use of terlipressin and albumin is not universal. The most common reason for not using terlipressin was a perceived lack of efficacy (8%), followed by inexperience in its use (7%) and cost (3%). The median dose of terlipressin given over 24 hours was 5 mg (range 1–12). Duration of therapy also varied (median 3.5 days, range 2–14). Of the surveyed consultants, 38% did not refer any cases of HRS to a liver centre.
Table 4.
Management of hepatorenal syndrome.
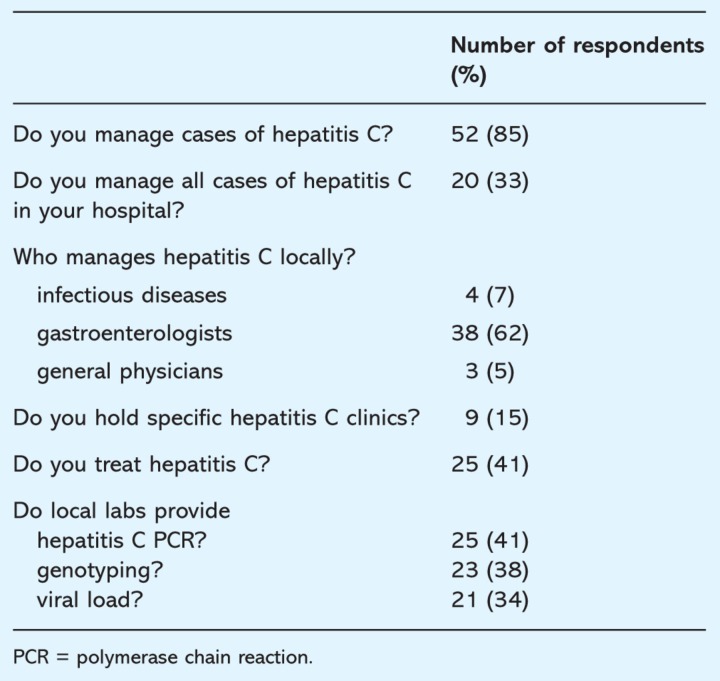
Hepatitis C
Table 5 shows the management of hepatitis C in the surveyed DGHs. Almost all consultants treating hepatitis C claim that they did so in line with the National Institute for Health and Clinical Excellence (NICE) guidelines. However, 21% would treat genotype 2 or 3 disease without biopsy. Funding issues remain a barrier to treatment in some units with 34% reporting difficulties financing antiviral therapies. Of the 26 non-gastroenterologist general physicians who replied, three (12%) were managing antiviral treatments for hepatitis C.
Table 5.
Management of hepatitis C.
Liver transplantation
The majority of consultants (88%) felt that access to transplant units was good and the median number of patients referred each year for liver transplantation was three (range 0–10) per unit. Only a minority of consultants (21%) complete a comprehensive pre-transplant work-up locally. The number of post-transplant patients under local follow up was 4.5 (range 0–30) suggesting that the majority of patients had to travel to their transplant centre on a regular basis. Only 31% of consultants had a shared care protocol with their local transplant unit.
Only 11% of consultants had a database of liver patients. Of the respondents, only 44% were aware of the National Plan for Liver Services and the majority of these were unaware of how it would affect their practice. Opinions of the likely impact of the plan included ‘the end of hepatology in DGHs’, ‘the need for consultant expansion’, ‘increased service commitments’, ‘more resources locally’ and ‘more specialisation’.
Discussion
In an era of increasing mortality from liver disease, it is clear that hepatology services at DGHs throughout the UK remain limited in many areas. The BSG recently calculated the workload for an average DGH and estimated a need for six full-time consultant gastroenterologists.7 Current levels are only half of this and this will restrict opportunities for consultants to subspecialise as hepatologists. Furthermore, training opportunities in hepatology have been restricted in the past, and this is reflected in the low proportion of consultants who trained at a liver unit. The infrastructure to run a liver service is not in place with significant shortages in radiology, pathology, alcohol support services and multidisciplinary meetings. The utility of nurse specialists in delivering liver services for hepatitis C has been highlighted, but the availability of nurse specialists remains limited to just a quarter of hospitals.8
The availability of ultrasound-assisted liver biopsies is good, with two-thirds performing all biopsies under ultrasound guidance. Access to TJBs remains poor, with only one-fifth of hospitals offering this approach. Lack of familiarity with this technique may explain the marked variability in the criteria used when determining which patients require a transjugular approach.
Variceal bleeding and HRS carry a high mortality and have been subject to recent developments in their management.9–11 The majority of units in our survey offer an acute gastrointestinal bleed service, although a recent report has raised concerns about the organisation of these services with as many as 64% reporting that arrangements were ‘unsatisfactory’.12 Most hospitals use a combination of sclerotherapy and band ligation for varices, and administer terlipressin. The use of antibiotic prophylaxis has been shown to reduce mortality in variceal bleeding.13 Although almost all respondents routinely use antibiotics, a significant proportion are using untested combinations which may not offer the necessary spectrum of cover. Salvage therapy for recurrent variceal bleeding appears to be addressed adequately although the high number of Sengstaken–Blakemore tubes used by some units may reflect inexperience of managing variceal bleeding or suboptimal endoscopic technique.
If untreated, HRS carries a 90% mortality rate. Terlipressin leads to improved renal function in approximately two-thirds of cases and has been adopted by many for the treatment of HRS.14 The dose and duration used is highly variable and the optimal regimen remains unclear: studies have used doses varying between 0.5 and 2 mg every four to six hours with no adequate dose comparisons. The addition of albumin has been shown to improve the effect of terlipressin and it is disappointing that more than 10% of gastroenterologists still use terlipressin alone.
It is clear from recent data that it is possible to predict short-term mortality in cirrhotic patients and the implementation of local guidelines may improve the acceptance of liver patients to the ICU.15
Hepatitis C will become an increasing part of the workload for gastroenterologists with 0.5% of the UK population being affected.16 The majority of consultants are unable to provide a complete hepatitis C service, lacking the supporting services required by the National Plan for Liver Services and NICE guidelines.17 It is encouraging that all consultants currently treating hepatitis C have switched from using standard interferon to pegylated interferon.
Conclusion
The current survey shows that provision of liver services at a DGH level is insufficient to meet current demand and ill-equipped to deal with the increasing burden of liver disease. There are marked deficiencies in consultant numbers and support from nurse specialists and allied medical specialties such as radiology, pathology and psychiatry. Access to facilities including laboratory tests and interventional radiology is patchy. There is wide variation in the management of many common liver diseases, such as hepatitis C, variceal haemorrhage and HRS. Most gastroenterologists do not have databases of their liver patients and outcome measures for many interventions are lacking making it difficult to compare the impact of the local variations on patient care. Although a previous survey of English ‘liver centres’ identified shortfalls in the service provision, the current results show that the resources available at many DGHs are even more limited.5 The data support the need for the implementation of the National Plan for Liver Services and the formation of managed clinical networks in hepatology.
Reference
- 1.Leon DA. McCambridge J. Liver cirrhosis mortality rates in Britain from 1950 to 2002: an analysis of routine data. Lancet. 2006;367:52–6. doi: 10.1016/S0140-6736(06)67924-5. [DOI] [PubMed] [Google Scholar]
- 2.Mohson AH. Trent HCV Study Group. The epidemiology of hepatitis C in a UK population of 5.12 million. Gut. 2001;48:707–13. doi: 10.1136/gut.48.5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Health. Annual report 2001. Liver cirrhosis – starting to strike at younger age groups. London: DH; 2001. www.doh.gov.uk/publications/Annualreports. [Google Scholar]
- 4. www.dh.gov.uk/PolicyAndGuidance/HealthAndSocialCareTopics/SpecialisedServicesDefinition/fs/en.
- 5.Williams R. Provision of specialist liver services in England. 2004. July www.bsg.org.uk/pdf_word_docs/hepservices.doc.
- 6.Moore K. Thursz M. Mirza DF. National Plan for Liver Services – specialised services for hepatology, hepatobiliary and pancreatic surgery 2003. Report prepared for The British Association for the Study of the Liver. www.basl.org.uk/resources.htm.
- 7.Royal College of Physicians. Consultant physicians working with patients: the duties, responsibilities and practice of physicians in general medicine and the specialties. 3rd edn. London: RCP; 2005. [Google Scholar]
- 8.Dusheiko G, editor; Rosenberg W, editor; Miles A, editor. The effective management of hepatitis C infection. UK key advances in clinical practice series 2001. London: Aesculapius Medical Press; 2001. [Google Scholar]
- 9.McCormick PA. O'Keefe C. Improving prognosis following a first variceal haemorrhage over four decades. Gut. 2001;49:682–5. doi: 10.1136/gut.49.5.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laine L. Planas R. Nevens F, et al. Treatment of the acute bleeding episode. In: De Franchis R, editor. Portal hypertension IV: Proceedings from the Fourth Baveno International Consensus Workshop. Oxford: Blackwell Publishing; 2006. pp. 217–42. [Google Scholar]
- 11.Cardenas A. Gines P. Hepatorenal syndrome: Current concepts. In: De Franchis R, editor. Portal hypertension IV: Proceedings from the Fourth Baveno International Consensus Workshop. Oxford: Blackwell Publishing; 2006. pp. 201–16. [DOI] [Google Scholar]
- 12.Gyawali P. Suri D. Barrison I, et al. A discussion of the British Society of Gastroenterology survey of emergency gastroenterology workload. Clin Med. 2007;7:585–8. doi: 10.7861/clinmedicine.7-6-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bernard B. Grange JD. Khac EN, et al. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology. 1999;29:1655–61. doi: 10.1002/hep.510290608. [DOI] [PubMed] [Google Scholar]
- 14.Gines P. Torre A. Terra C. Guevara M. Review article: pharmacological treatment of hepatorenal syndrome. Aliment Pharmacol Ther. 2004;20(Suppl3):57–62. doi: 10.1111/j.1365-2036.2004.02115.x. [DOI] [PubMed] [Google Scholar]
- 15.Cholongitas E. Senzolo M. Patch D, et al. Risk factors, sequential organ failure assessment and model for end-stage liver disease scores for predicting short term mortality in cirrhotic patients admitted to intensive care unit. Aliment Pharmacol Ther. 2006;23:883–93. doi: 10.1111/j.1365-2036.2006.02842.x. [DOI] [PubMed] [Google Scholar]
- 16.Department of Health. Hepatitis C strategy for England. London: DH; 2002. [Google Scholar]
- 17.National Institute for Clinical Excellence. Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of chronic hepatitis C. London: NICE; 2004. www.nice.org.uk/page.aspx?0=ta075guidance. [Google Scholar]