Abstract
The modified early warning score (MEWS) was developed as a track and trigger tool for the prompt identification of seriously ill patients on an acute medical ward. This paper examines its value in the setting of an acute medical admissions unit (MAU) and compares it to biochemical markers of acute and chronic disease. Three hundred unselected acute admissions to the MAU of the Queen Elizabeth Hospital, Gateshead, were assessed. Correlations between MEWS score and C-reactive protein (CRP) and albumin separately were assessed, and then the relationship between MEWS and the CRP/albumin ratio across the age spectrum was examined. The findings demonstrated a strong correlation between the MEWS score and CRP/albumin ratio (r=0.88, p<0.001) across the whole age spectrum. Length of stay correlated poorly with MEWS (r=0.08) and CRP/albumin ratio (r=0.15). Overall mortality was 5% and was predicted by both tools, with a MEWS score of >4 (relative risk (RR)=7.8) outperforming a CRP/albumin of >2 (RR=2.6). MEWS remains the gold standard for assessing outcome in acute medical admissions, but does have limitations in the elderly (those aged over 70 years). A raised CRP/albumin ratio was less sensitive for overall mortality than MEWS. It did, however, appear to be of greater value in the elderly, especially in those with acute exacerbations of chronic disease. Neither test accurately predicted length of stay.
Key Words: albumin, C-reactive protein, death, early warning system, length of stay, outcome
Introduction
The concept of an early warning system (EWS) for detecting potentially unstable patients originated in surgery and was first described 10 years ago. It was based on regular assessment of five basic physiological parameters by trained nursing staff and was shown to be useful in tracking patients perioperatively and triggering an appropriate clinical response in those whose parameters deteriorated, leading to a increasing EWS. The concept was subsequently modified for acute medical patients (MEWS) where it was validated and shown to be effective in predicting prognosis with a MEWS score of five or more reported to be associated with a worse outcome.1
There are conflicting data on the applicability of MEWS to undifferentiated medical patients admitted to an acute MAU setting. One study demonstrated no relationship between MEWS score and in-hospital deaths, while another has reported correlations with mortality and length of stay.2,3 However, its applicability across the age ranges represented in an acute medical setting have not been examined. Given the pressure on acute hospital beds and the frequent ‘fast tracking’ of patients from MAU to appropriate specialist wards, the adoption of prognostic markers for disease severity and length of stay may prove invaluable in choosing which patients to move, when and where. There is evidence-based guidance on the severity of organ-specific disease in a number of areas such as community-acquired pneumonia (CURB 65 scores), acute cerebrovascular disease (ABCD guidelines) and acute gastrointestinal bleeding (Blatchford score) but little validated data exist for the large number of often elderly patients with acute on chronic disease who frequently have multiple pathology.4–6 This study explored the possible role of using markers of acute and chronic disease to assess prognosis in this setting and compared this approach with the use of MEWS to see if either offers benefits to clinical practice.
Methods
Real-time data on a total of 300 admissions to the acute medical assessment unit (MAU) of Queen Elizabeth Hospital, Gateshead, over the first three weeks of two years (2004 and 2006) were collected during standard working hours. The data were collected using identical methodology by two of the authors (EF and EC) and patients were consecutive and unselected. Initial information recorded included age, gender, date of admission, past illnesses, reason(s) for admission, admission values of C-reactive protein (CRP) and albumin and their baseline MEWS score using verified criteria (Table 1). Data at discharge or death which included their outcome and length of stay, together with all confirmed new or adjusted diagnoses were also collected.
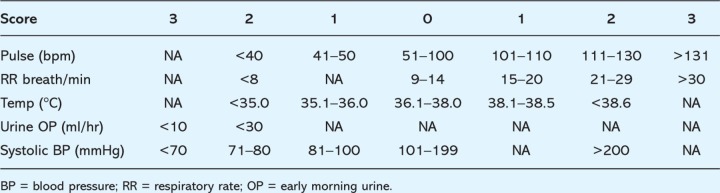
Table 1.
To show the adapted modified early warning score (MEWS) scoring table used for medical patients.
The information was analysed to show the distribution of all patients' MEWS scores at admission and to compare these scores with overall length of stay for survivors. Overall mortality was calculated and was also compared to baseline MEWS scores. In order to assess the potential impact of age the data were reanalysed by age in decades. MEWS were compared against acute (CRP) and chronic (albumin) markers of disease to assess potential correlation. This led to the development of the concept of the CRP/albumin ratio as a potential marker of disease severity. This was in turn compared to MEWS, and to length of stay and mortality. Further analyses of the influence of age and cause of death on the value of CRP/albumin ratios were then performed.
Statistical analysis was performed using logistic regression to produce correlation coefficients between a number of variables. The relative risks (RRs) of elevated MEWS and CRP/albumin ratios for death were calculated using χ2 analysis. The standard statistics package (SPSS) was used for all calculations.
Results
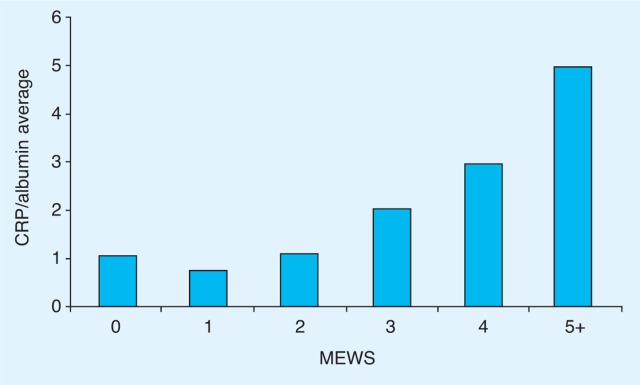
There were no differences in the demographic data from the two data collection periods so data were amalgamated for the purposes of analysis. The median age of the 300 patients was 73 years (range 16–99) and 43% were male. A wide range of diagnoses were represented across the spectrum of acute admissions with the most common categories being acute chest pain (18%), exacerbation of airways disease (16%), sepsis (12%), syncope (7%), gastrointestinal bleeding (5%) and acute cerebrovascular disease (3%). The median MEWS score was 1 (range 0–8) while the median value of the CRP/albumin ratio was 1.3 (range 0.05–32). The overall correlation of MEWS with individual values of CRP (r=0.67, p=0.01) and albumin (r=0.43, p=0.03) is shown in Fig 1, while the highly significant correlation of MEWS with CRP/albumin ratio is shown in Fig 2 (r=0.88; p=0.001).
Fig. 1.
The relationship between modified early warning score (MEWS), and C-reactive protein (CRP) and albumin.
Fig. 2.
The relationship between C-reactive protein (CRP)/albumin ratio and the modified early warning score (MEWS).
The median length of hospital stay was five days (range 1–93). The overall in-hospital mortality was 5% with all but three deaths in patients over the age of 70 years. The correlation between MEWS and length of hospital stay was poor with an insignificant correlation coefficient of 0.08. The correlation of CRP/albumin ratio with length of stay was only slightly better at 0.15 and again failed to achieve statistical significance.
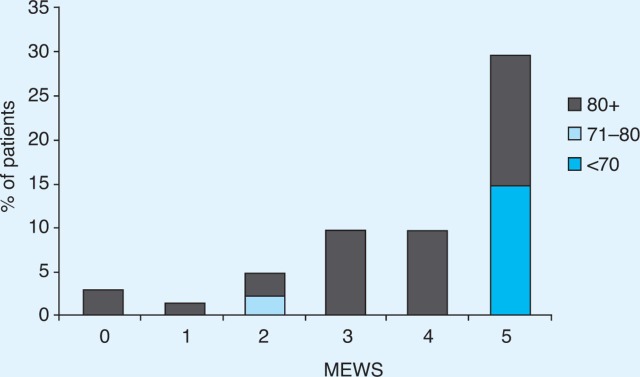
The relationship between MEWS and mortality is shown in Fig 3. Mortality increased with rising MEWS scores, from under 5% in patients with scores of 0 to 2, to 30% for those with scores of 5 or more. Age was an important factor with no one below 70 years of age dying with a MEWS score of less than 5.
Fig. 3.
Link between mortality and the modified early warning score (MEWS) by decade.
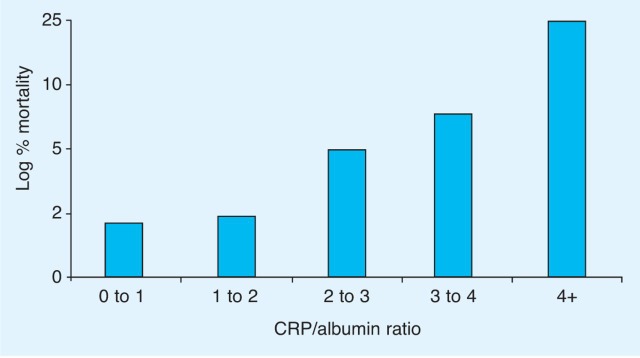
The relationship between CRP/albumin and mortality is shown in Fig 4. Mortality rose from 5% in patients with ratios under 2, to 25% for those with scores over 4. The median values of CRP/albumin ratio were greater in those dying than in those who survived to discharge (4.61 ν 1.29; p=0.036). Most deaths associated with an elevated CRP/albumin ratio were in patients with an acute exacerbation of a chronic condition, while those dying suddenly from vascular causes usually had a normal ratio.
Fig. 4.
The relationship between C-reactive protein (CRP)/albumin ratio and log percentage mortality.
The RR of dying was significantly raised in patients with a MEWS >4 (RR=7.8) and in individuals with a CRP/albumin ratio >2 (RR=2.6). Age had a significant effect on these predictors of mortality. Of the 12 deaths in patients over 70 years of age, only three had a MEWS score >4, while six had a CRP/albumin ratio >2. This indicates a sensitivity for death of 25% for MEWS >4 and of 50% for CRP/albumin ratio >2 in those in or beyond their eighth decade.
Discussion
Recent guidance from the National Institute for Health and Clinical Excellence recommends the use of a track and trigger tool for the triage of acutely ill patients admitted to hospital.7 Data confirm the value of MEWS as a tool to predict outcome in such patients. Mortality was strongly correlated with admission MEWS and a value of over 4 was associated with a mortality of 30%. However, there were clear limitations in the predictive value of MEWS with regard to mortality in those patients in their eighth decade and beyond. This has not previously been reported but, with our increasingly aged population, this becomes an important finding and should not be overlooked.
A raised CRP generally suggests an acute infective or inflammatory process, while a low albumin is most often associated with chronic disease, often linked with nutritional deficiency. These investigations are readily available, usually within minutes of acute admission, and are often performed automatically as part of an admission profile. Both showed strong individual correlations with MEWS scores, and the ratio of CRP/albumin correlated particularly well with MEWS. This ratio, like MEWS, correlated with the risk of dying in hospital. The use of the CRP/albumin ratio was generally less robust than MEWS as a predictor of death in younger patients but appeared to be less influenced by increasing age.
Neither of the assessments correlated well with length of stay. This is due in part to confounding by the early death of those patients with high scores who were clearly very sick. Even when these data are excluded from analysis, neither MEWS nor CRP/albumin ratio could be shown to offer a confident prediction of likely discharge date. Smaller numbers of daily discharges with time again reduced the statistical power of the comparison, but the main reasons for the failure of both markers of illness severity to correlate with length of stay were non-medical factors. These usually related to personal or social circumstances. If we had collected information relating to the date that patients were deemed medically fit for discharge, as opposed to the date they actually left hospital, a correlation may have been evident. Perhaps such a study should be undertaken to examine this and to highlight lost bed days?
As our population continues to increase in age and in longevity, the need to deal with an increasing burden of acute and chronic illness is evident. Although primary prevention is increasingly effective and more chronic illness is dealt with in primary care, there are increasing numbers of hospital admissions with acute or acute on chronic problems.8 Given the restraints on hospital resources, a system which allows for effective triage and prompt intervention for the sickest patients is to be encouraged, and MEWS would appear to be broadly fit for this purpose. Patients with MEWS scores of 0 or 1 may be considered for early discharge, perhaps via a short-stay unit if investigations are awaited.9 Those with scores of 2 to 4 often need transfer to an appropriate base ward, while those with scores of 5 or more frequently require more intensive care, often with involvement of the critical care outreach team. Resourcing of each of these clinical areas may be informed by examining the range of MEWS scores in resident patients to ensure the appropriate staffing levels and skill mix are provided. Subsequent audit of clinical outcome is greatly facilitated by the use of scoring systems.
The development of acute elderly care admission areas has recently found favour.10 Given that the median age of acute medical admissions is now over 70 years of age, these resources are likely to be stretched. The use of the CRP/albumin ratio may offer some advantages in this clinical setting, whereas the ability of MEWS to predict mortality declines after the age of 70. This tool appears to be most useful in assessing patients with acute exacerbations of chronic disease but may be less valuable in predicting the outcome of acute single-system disease where other clinical scores have already been validated.4–6
In summary, deaths due to single-organ disease in patients aged under 70 years are more accurately predicted by MEWS, while outcome in older patients with chronic disease may be more closely related to the CRP/albumin ratio. Neither tool was shown to offer a confident prediction of length of hospital stay in this study.
Reference
- 1.Subbe CP. Kruger M. Rutherford P. Gemmel I. Validation of a modified early warning score in medical admissions. QJM. 2001;94:521–6. doi: 10.1093/qjmed/94.10.521. [DOI] [PubMed] [Google Scholar]
- 2.Subbe CP. Davies RG. Williams E. Rutherford P. Gemmel I. Effect of introducing the modified early warning score on clinical outcomes, cardiopulmonary arrests and intensive care utilisation in acute medical admissions. Anaesthesia. 2003;58:775–803. doi: 10.1046/j.1365-2044.2003.03258.x. [DOI] [PubMed] [Google Scholar]
- 3.Paterson R. MacLeod DC. Thetford D, et al. Prediction of in-hospital mortality and length of stay using an early warning scoring system: clinical audit. Clin Med. 2006;6:281–4. doi: 10.7861/clinmedicine.6-3-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lim WD. van der Eeden MM. Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital; an international derivation and validation study. Thorax. 2003;58:377–83. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothwell PM. Giles MF. Flossman E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet. 2005;366:29–38. doi: 10.1016/S0140-6736(05)66702-5. [DOI] [PubMed] [Google Scholar]
- 6.Blatchford O. Murray WR. Blatchford M. A risk score to predict need for treatment for upper gastrointestinal haemorrhage. Lancet. 2000;356:1318–21. doi: 10.1016/S0140-6736(00)02816-6. [DOI] [PubMed] [Google Scholar]
- 7.National Institute for Health and Clinical Excellence. Acutely ill patients in hospital: recognition of and response to acute illness in adults in hospital. London: NICE; 2007. pp. 1–8. [PubMed] [Google Scholar]
- 8.Almond S. Where is the sharp end and how did we get here? Clin Med. 2007;7:105–8. doi: 10.7861/clinmedicine.7-2-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Downing H. Scott C. Kelly CA. Evaluation of a dedicated short-stay unit for medical admissions. Clin Med. 2008;8:18–29. doi: 10.7861/clinmedicine.8-1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Royal College of Physicians. Management of the older medical patient: teamwork in the journey of care. London: RCP; 2000. pp. 1–8. [Google Scholar]