Abstract
Fatigue and stress-related illnesses often become diagnoses of exclusion after extensive investigation. ‘Tired all the time’ is a frequent reason for referral to the endocrine clinic, the implicit question being – is there a subtle endocrine pathology contributing to the patient's symptoms? Often initial assessment suggests not but there are no clear data to address the question of whether overt pathology will develop in the future. This study observed outcomes after five years in 101 consecutive and unselected referrals to secondary care for ‘fatigue? cause’, where initial assessment did not suggest treatable endocrine pathology. The findings suggest that the clinical diagnosis of fatigue, based on history and tests to exclude anaemia, hypothyroidism and diabetes, is secure: these patients do not subsequently demonstrate excess morbidity and mortality, and their presenting symptoms are not early features of significant endocrine pathology.
Key Words: chronic fatigue, clinical reasoning, subclinical thyroid disease
Introduction
Chronic fatigue is a common complaint, associated with frequent primary care consultations, and often becoming a diagnosis of exclusion after extensive investigation and referral to a number of specialist services.1,2 Because fatigue is so non-specific, patients can find themselves passed from one specialist to another, deepening their conviction that organic disease must be the cause. Laboratory investigation may be duplicated, extensive and often unproductive, with implications for cost in distress to the patient and in use of resources.3 The chronic fatigue syndrome is a manifestation of psychological and pathological processes, not all of which are easily labelled in the conventional medical model.4,5 It is likely that, as science progresses, some of these disease processes will be definitively characterised but at the current time a significant proportion of patients are referred to endocrinology. This is entirely reasonable, as many endocrine conditions have an insidious onset with diagnosis after months or years of ill health. A common clinical scenario is an individual with a spectrum of non-specific symptoms and minimal physical signs where initial investigations are normal. It is possible to reassure the individual that there is no significant disease at that point but there are no clear data to address the question of whether overt pathology will develop in the future. This paper reports audit findings for a cohort of patients seen in an endocrinology clinic with fatigue, including outcome data at five or more years later.
Subjects and methods
Consecutive and unselected referrals from primary care to the endocrinology service over a four-year period (1995–99) were identified from the clinic database. Referrals were included in the dataset if the primary reason for referral or primary symptom was fatigue. By implication the referring doctor suspected an underlying endocrine pathology. Patients were excluded if a definitive diagnosis was subsequently made. Thus patients who had been diagnosed with overt hypo- or hyperthyroidism prior to clinic referral or as a result of the referral were excluded from the cohort. Initial clinical assessment included history, physical examination and simple investigations: thyroid function, biochemistry, liver function tests, blood count and plasma glucose. Patients were only included if clinical assessment did not identify a clear underlying pathology to explain the individual's symptoms.
In this report we have combined a retrospective analysis of the original referral and medical records with a review of the individual's health at least five years later. Demographic data, nature and duration of symptoms prior to referral, and past medical or psychiatric history were acquired from review of original case notes. Outcome data after at least five years were obtained from hospital records, postal questionnaires to patients and their primary care practitioners, and the UK Office of National Statistics. Patients were asked if they had suffered any serious medical problems in the intervening years. Patients were then asked if they currently suffered from: fatigue, poor motivation, low mood, tiredness, anxiety or weight control problems. The same questions were asked of their primary care doctor. Local Research Ethics Committee approval was obtained for the study. Data were analysed using Microsoft Office Excel 2003 and SPSS version 14.0. Independent samples t-tests were used to compare means.
Results
In total, 101 patients were include in the study. Four main themes were identified as the reason for referral. The primary care doctor suspected the final diagnosis of the first group was likely to be chronic fatigue but felt that endocrine pathology needed to be excluded. Referrals in this group included the phrases ‘chronic fatigue’, ‘post-viral fatigue’ or ‘myalgic encephalomyelitis’ (ME).
Fatigue was a major symptom for the second group but the primary care doctor suspected a specific endocrine diagnosis as the underlying pathology. Suggested potential diagnoses included Addison's disease, acromegaly, Cushing's syndrome, hypopituitarism, phaeochromocytoma, carcinoid syndrome and hypoglycaemia. If specialist review supported the possibility of such a diagnosis then appropriate endocrine investigations were conducted. Ten patients underwent further endocrine investigation, with normal results.
A third group of referrals were those where the patient or primary care doctor had questioned whether fatigue was the result of known thyroid disease: patients with positive thyroid antibodies (but normal thyroid function) or those with previously diagnosed hypothyroidism established on thyroid hormone replacement who remained symptomatically unwell despite normal serum free thyroxine (FT4) and thyroid stimulating hormone (TSH) (19 subjects).
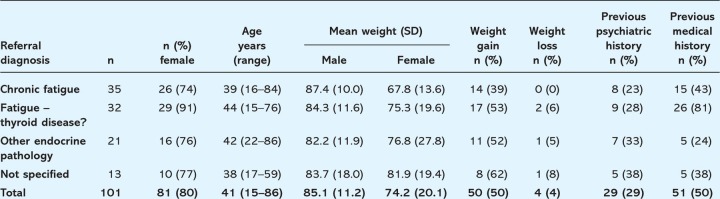
Finally there was a small group of individuals where fatigue, together with a variety of other symptoms, was mentioned in the referral letter but no specific diagnosis was suggested. Table 1 displays the demographics of the 101 patients according to the referral group as detailed above. The majority of patients in each group were female, most marked in the group of individuals where the clinical question related to thyroid disease. Patients were relatively young with a mean age of 41 years and this was similar across each of the four groups. Weight gain was a frequent complaint (50% of patients) and present more frequently in those individuals with a specific query of thyroid or other endocrine disease. Importantly weight loss prior to referral was very unusual in this group, reported in just four individuals of whom two were on calorie-restricted diets. None of the patients were underweight. Although weight was recorded at each clinic visit height was not, therefore individual calculations of body mass index (BMI) were not possible. However, mean BMI can be estimated assuming that the height of the subjects included in this study is similar to the population mean for this age group (165 cm for women, 178 cm for men). Using these figures, mean BMI for the women in this study was 24.9 kg/m2 and 27.6 kg/m2 for the men. Thus although subjects overall were not underweight in this cohort they are below the population mean (women population mean 26.8 (SE 0.20) kg/m2, men 26.8 (SE 0.23) kg/m2) for this age group. This trend differed between the referral groups. Women presenting with a primary diagnosis of chronic fatigue weighed less than women presenting with a concern over primary endocrine or thyroid diagnosis (p=0.028). Women referred with query thyroid or endocrine disease were overweight and above the population mean weight for this age group. The number of referrals for men in each group is too small to analyse but the weight appears similar in each group.
Table 1.
Age, gender, weight at presentation, history of weight change and relevant past medical history for 101 men and women referred to the endocrine clinic for investigation of fatigue. Individuals are classified by the suggested diagnosis in the referral letter from the primary care physician.
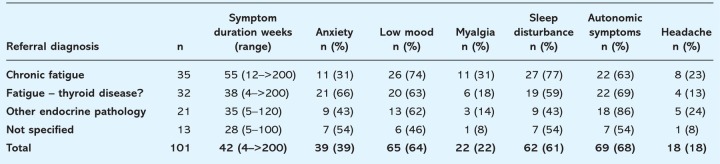
A significant number of patients in each group had a previous psychiatric history, predominantly anxiety or depression, with one case of psychotic illness. Previous significant medical history was primarily seen in those individuals referred with the question of whether or not their fatigue was the result of known thyroid disease; not unsurprisingly this past medical history mostly equated to previous thyroid disease. Table 2 lists the symptoms according to the referral diagnosis. Symptoms were chronic in all groups (mean 42 weeks). All patients by definition presented with fatigue and in addition low mood, sleep disturbance and autonomic symptoms such as flushing, palpitations, tremor, and thermolability were also common. There were also marked differences between groups, with anxiety being less common and myalgia being more common in the group referred with a primary diagnosis of chronic fatigue. Sleep disturbance was also reported more commonly in this group.
Table 2.
Symptoms at presentation in 101 subjects according to referral diagnosis. Fatigue as a presenting symptom was universal.
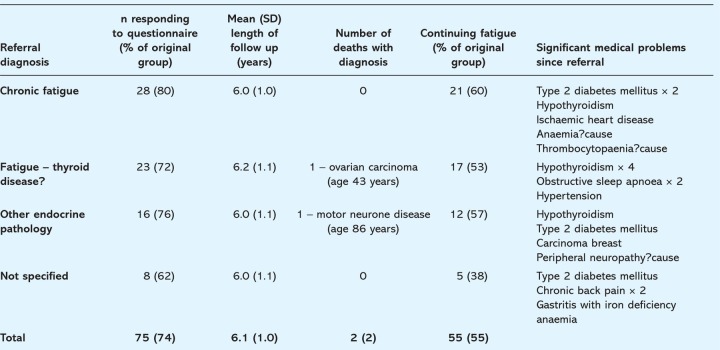
Of the 101 patients, 99 (99%) were alive at follow up. The two deaths resulted from metastatic ovarian cancer and motor neurone disease. Questionnaire responses were received for 75 patients, of whom 55 continued to experience problems with fatigue, poor motivation and/or mood disturbance. An updated medical history was also obtained from the hospital records and primary care physician. A number of new medical problems were reported (Table 3), with 10 new endocrine diagnoses, not including those patients with previously diagnosed (and treated) thyroid disease. Fasting glucose levels at clinic in two of the four patients with subsequent type 2 diabetes would be labelled as impaired fasting glycaemia by current standards, although were within the normal range used at that time. For the other two patients, no laboratory glucose measurement was performed when seen in the endocrine clinic, which may have led to a delay in diagnosis.
Table 3.
Subsequent symptoms and diagnoses at a mean of six years' follow up. Percentages displayed are for those of the whole cohort (101 subjects).
Discussion
Chronic fatigue remains a controversial diagnosis, frequently without clear explanation.6 As it remains a diagnosis of exclusion there will always be uncertainty. It is often the case that individuals are seen by a number of specialists without a definitive diagnosis ever being made. In each case the question must be asked how far should investigation proceed before we say that a conclusion must be drawn? There is often an unstated view that, if only the correct test were performed, the diagnosis would be clear and treatment possible. This is certainly true for referrals to the endocrine clinic: many endocrinopathies present with non-specific symptoms including fatigue, and require very specific tests to make the diagnosis without necessarily having any abnormality detected on baseline investigations. However, as this study illustrates, the majority of patients referred with ‘fatigue?endocrine’ required no specialised endocrine investigation.
The intention of this paper is not to debate the pathogenesis or treatment of chronic fatigue syndrome but rather to inform the decision-making process by providing information about the long-term outcome for these individuals. Our results suggest that, in the absence of more specific symptoms, the diagnosis of chronic fatigue can be made following a detailed history and examination together with a panel of baseline investigations. Following this it can be concluded with some confidence that the patient does not have a specific diagnosis that has been missed and will manifest later. Specifically the symptoms are not an early manifestation of an illness that will result in their death within the next six years.
A number of common themes could be seen within the study group. As has previously been shown females form the majority of referrals for fatigue.7,8 The ages of the group are relatively young and there is a high incidence of previous psychiatric disease. Weight loss was very unusual and weight gain relatively common. While the medical diagnoses combining fatigue and weight loss are many, and often serious, there are very few conditions that combine fatigue with weight gain, other than hypothyroidism and diabetes. The latter two disorders are readily excluded by simple investigations. Other rarities may need to be considered as a cause of fatigue and weight gain such as Cushing's syndrome, insulinoma or hypopituitarism but the management strategy detailed above should identify these.
A significant group within this cohort were individuals with a concern over thyroid dysfunction as the cause for their fatigue. This group includes patients with known (treated) hypothyroidism, those with transient borderline TSH elevation (but not overt thyroid disease), and those with normal thyroid function but positive thyroid antibodies. There is much interest, including from patient groups, over so-called subclinical hypothyroidism. Patients with minimal TSH elevation or suppression are often described as having subclinical thyroid disease, but by definition, signs and symptoms are absent. There is epidemiological evidence of the increased risk of atrial fibrillation and osteoporosis in individuals with subclinical hyperthyroidism, but the link between subclinical hypothyroidism and cardiovascular disease appears less clear-cut.9–14 In addition, no randomised studies have evaluated the benefit of thyroxine replacement in patients with subclinical hypothyroidism on important cardiac end points. A recent consensus statement recommended against treatment of ‘mild’ hypothyroidism, however not all clinicians (and patients) would agree.15,16
There are limitations to this study. As the patient cohort had been selected for referral to secondary care, the results may not be applicable to all chronically fatigued patients in primary care. Follow-up questionnaires were received for 74% of the original cohort, raising the possibility of selection bias towards patients with continuing symptoms. The follow up was, however, supported by contacting the primary care physician and separately tracing deaths within the cohort. There were only two deaths in the group and the causes were unrelated to the presentation with chronic fatigue.
Although the absence of organic disease may reassure the doctor, ongoing fatigue may impose considerable distress on the patient.2 Treatment with selective serotonin re-uptake inhibitors may be effective, even in the absence of depression.17 Other potentially useful interventions include cognitive behavioural therapy (CBT), lifestyle modification, and complementary therapies. On systematic review, CBT seems to be the most beneficial intervention for chronic fatigue.18
In this cohort, symptoms had already been present for many weeks (or longer) at the time of presentation to the endocrine clinic, and unfortunately they were still present in over half the patients over five years later. The longevity of fatigue symptoms has been previously documented.19 At the current time tools to successfully treat this difficult problem are lacking but the data provide useful additional information that can be given to the patient and is likely to help in their understanding of this condition. A significant proportion of patients with chronic fatigue do accept a psychological explanation for their symptoms.5
The degree of certainty with which the diagnosis can be made, without the nagging concern that ‘something has been missed’, may bring the patient to treatment earlier and avoid the often unproductive re-referrals to other specialties that can lead to a lifetime's quest for organic disease that is not present. Physicians can be confident in explaining to the individual that they are unlikely to be missing any other sinister pathology and that in itself is an important message.
Reference
- 1.Bates DW. Schmidt W. Buchwald D, et al. Prevalence of fatigue and chronic fatigue syndrome in a primary care practice. Arch Intern Med. 1993;153:2759–65. [PubMed] [Google Scholar]
- 2.Risdale L. Evans A. Jerrett W, et al. Patients who consult with tiredness: frequency of consultation, perceived causes of tiredness and its association with pyschological distress. Br J Gen Pract. 1994;44:413–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Lane TJ. Matthews DA. Manu P. The low yield of physical examinations and laboratory investigations of patients with chronic fatigue. Am J Med Sci. 1990;299:313–8. doi: 10.1097/00000441-199005000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Elnicki DM. Shockcor WT. Brick JE. Evaluating the complaint of fatigue in primary care: Diagnoses and outcomes. Am J Med. 1992;93:303–6. doi: 10.1016/0002-9343(92)90237-6. [DOI] [PubMed] [Google Scholar]
- 5.Kirk J. Douglass R. Nelson E, et al. Chief complaint of fatigue: A prospective study. J Fam Pract. 1990;30:33–41. [PubMed] [Google Scholar]
- 6.Wessely S. Nimnuan C. Sharpe M. Functional somatic syndromes: one or many? Lancet. 1999;354:936–9. doi: 10.1016/S0140-6736(98)08320-2. [DOI] [PubMed] [Google Scholar]
- 7.Kroenke K. Wood DR. Mangelsdoff D, et al. Chronic fatigue in primary care. Prevalence, patient characteristics and outcome. JAMA. 1988;260:929–34. [PubMed] [Google Scholar]
- 8.Gallagher AM. Thomas JM. Hamilton WT. White PD. Incidence of fatigue symptoms and diagnoses presenting in UK primary care from 1990 to 2001. J R Soc Med. 2004;97:571–5. doi: 10.1258/jrsm.97.12.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cappola AR. Fried LP. Arnold AM, et al. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA. 2006;295:1033–41. doi: 10.1001/jama.295.9.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sawin CT. Geller A. Wolf PA, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med. 1994;331:1249–52. doi: 10.1056/NEJM199411103311901. [DOI] [PubMed] [Google Scholar]
- 11.Parle JV. Maisonneuve P. Sheppard MC. Boyle P. Franklyn JA. Prediction of all-cause and cardiovascular mortality in elderly people from one low serum thyrotropin result: a 10-year cohort study. Lancet. 2001;358:861–65. doi: 10.1016/S0140-6736(01)06067-6. [DOI] [PubMed] [Google Scholar]
- 12.Faber J. Galloe AM. Changes in bone mass during prolonged subclinical hyperthyroidism due to L-thyroxine treatment: a meta-analysis. Eur J Endocrinol. 1994;41:421–4. doi: 10.1530/eje.0.1300350. [DOI] [PubMed] [Google Scholar]
- 13.Walsh JP. Bremner AP. Bulsara MK, et al. Subclinical thyroid dysfunction as a risk factor for cardiovascular disease. Arch Intern Med. 2005;165:2467–72. doi: 10.1001/archinte.165.21.2467. [DOI] [PubMed] [Google Scholar]
- 14.Biondi B. Palmieri EA. Lombardi G. Fazio S. Effects of subclinical thyroid dysfunction on the heart. Ann Intern Med. 2002;137:904–14. doi: 10.7326/0003-4819-137-11-200212030-00011. [DOI] [PubMed] [Google Scholar]
- 15.Surks MI. Ortiz E. Sawin CT, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA. 2004;291:228–38. doi: 10.1001/jama.291.2.228. [DOI] [PubMed] [Google Scholar]
- 16.Gharib H. Tuttle RM. Baskin HJ, et al. Consensus statement: subclinical thyroid dysfunction: a joint statement on management from the American Association of Clinical Endocrinologists, the American Thyroid Association and The Endocrine Society. J Clin Endocrinol Metab. 2005;90:581–5. doi: 10.1210/jc.2004-1231. [DOI] [PubMed] [Google Scholar]
- 17.Hartz A. Bentler S. Brake K. Kelly M. The effectiveness of citalopram for idiopathic fatigue. J Clin Psychiatry. 2003;64:927–35. doi: 10.4088/JCP.v64n0811. [DOI] [PubMed] [Google Scholar]
- 18.Whiting P. Bagnall AM. Sowden AJ, et al. Interventions for the treatment and management of chronic fatigue syndrome: a systematic review. JAMA. 2001;286:1360–8. doi: 10.1001/jama.286.11.1360. [DOI] [PubMed] [Google Scholar]
- 19.Schmaling K. Fieldlak J. Katon W. Bader J. Buchwald D. Prospective study of the prognosis of unexplained chronic fatigue in a clinic based cohort. Psychosom Med. 2003;65:1047–54. doi: 10.1097/01.PSY.0000088587.29901.69. [DOI] [PubMed] [Google Scholar]