Abstract
Advances in medical genetics are increasingly impacting on clinical practice outside specialist genetic services. It is widely acknowledged that physicians will need to use genetics knowledge and skills in order to incorporate these advances into patient care. In order to determine priority areas for genetics education for non-genetics specialist registrars, an educational needs assessment was undertaken. Consultants from cardiology, dermatology, neurology and genetics identified genetics knowledge, skills and attitudes required by non-genetics specialty trainees. From these, and informed by trainees' views of genetic education, six genetics learning outcomes that non-genetics medical specialty trainees should attain by the end of their training have been identified, each linked to core knowledge, skills and attitudes. These core concepts can be taught with reference to specialty-specific conditions to highlight their relevance to clinical practice. The results of this study are informing the genetic component of postgraduate medical training curricula.
Key Words: curriculum, educational strategies, genetics education, learning outcomes, specialist trainees
Background
Developments in genetics are increasingly impacting on the clinical practice of healthcare professionals outside specialist genetic services.1–3 Genetic advances have led to new therapeutics in oncology, such as trastuzumab (Herceptin®)4 and to new molecular prognostic tests based on the pattern of expression of genes in tumours.5 Advances in genetics have also led to an increased understanding of, and availability of genetic testing for, major disorders caused by mutations in single genes. This improved understanding has led to new therapeutic strategies, such as the current trial of losartan in Marfan syndrome,6 and the identification of new targets for potential therapeutics such as filaggrin in ichthyosis vulgaris and atopic dermatitis (eczema).7,8 Additionally, a new generation of whole genome association studies, such as that recently published by the Wellcome Trust Case Control Consortium,9 are leading to an improved understanding of the genetics of complex diseases.
Although it is now recognised that a range of medical specialist groups need an understanding of genetics, studies have suggested that current educational programmes are not adequately preparing doctors in this regard.1,2,10,11 In a recent study, people with or at risk of genetic conditions and parents of children affected by a genetic condition expressed the belief that there is a need for greater awareness of genetic aspects of conditions among healthcare professionals, and that consultants in different medical specialties, such as cardiology, neurology and paediatrics, could play a greater role in providing information about the genetic basis of the condition.12
A review of genetics education for UK health professionals in 2002 highlighted the need for such education to be based on an understanding of what health professionals need to know, encompassing what health professionals say they need and what experts think they need.2 In the UK core learning outcomes and competences in genetics have since been identified for nurses, midwives and health visitors,13 general practitioners,14 and non-genetics healthcare professionals.15 This paper describes the development of core learning outcomes in genetics for non-genetics specialist registrars (SpRs), based on a study to identify the genetic knowledge, skills and attitudes required in clinical practice within three specialties: cardiology, dermatology and neurology.
Trainees' views of genetics education
A key component of the study was a series of group interviews with SpRs from cardiology (n=24), dermatology (n=21) and neurology (n=8) from the West Midlands and South Western deaneries, the results of which have been previously published.11 It was important to explore trainees' views of genetics in order to take into account the reality of their experiences and priorities. Trainees stressed the importance of tailoring genetics education to be directly relevant to their daily clinical practice and prioritised topics related to the diagnosis and management of particular diseases.
What genetic knowledge, skills and attitudes do specialist registrars need for clinical practice?
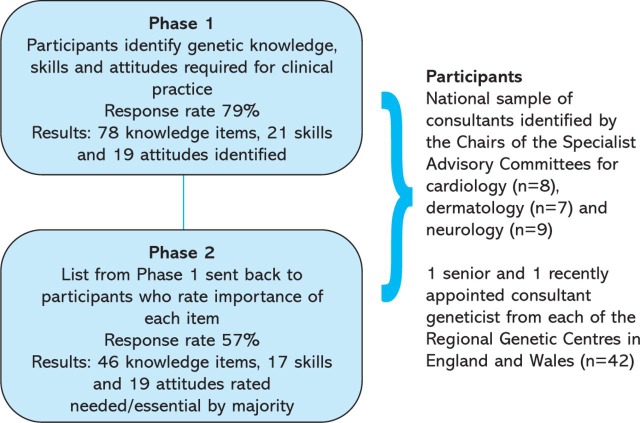
In order to ground genetics education in clinical practice the development process involved practitioners from different medical specialties, as well as genetic consultants. A modified Delphi process, an established technique for curriculum development,16 was used (summarised in Fig 1). The process was conducted between December 2002 and February 2005 and involved a national sample of consultants from cardiology, dermatology, neurology and genetics. This sample comprised one senior and one recently appointed consultant geneticist from each of the regional genetic centres in England and Wales (n=42), and a national sample of consultants identified by the Chairs of the Specialist Advisory Committees for cardiology (n=8), dermatology (n=7) and neurology (n=9).
Fig. 1.
The modified Delphi process.
In Phase 1, participants were invited to access and complete an anonymous online survey. An open question asked respondents to identify the ‘core’ genetic knowledge, skills and attitudes relevant to all specialties, as well as those relevant to cardiology, dermatology and neurology (respondents were asked to complete those sections relevant to their expertise). The response rate for Phase 1 was 79%. When the results were collated, the survey identified 78 knowledge items, 21 skills and 19 attitudes considered by participants to be relevant to all specialties. There was a high level of congruence between the responses from different specialties regarding these ‘core’ components. The items considered specialty specific consisted of lists of conditions relevant to that specialty.
The results from Phase 1 formed the basis of Phase 2, in which participants were asked to indicate, for each item, whether they thought it was ‘essential for inclusion’ in training, ‘needs to be included’, ‘useful for inclusion’ or ‘not needed’. The response rate for Phase 2 was 57%. In total, 46 core knowledge items, 17 core skills and 19 core attitudes were rated ‘essential’ or ‘needed’ by the majority of respondents. There was no significant difference between ratings given by geneticists compared to those given by consultants from other specialties for nearly all topic areas, the exception being the genetic basis of cancer, which geneticists rated significantly higher than non-geneticists (p<0.001, calculated using the Mann-Whitney U test).
Participants were also asked to identify teaching priorities in genetics and, notably, the topics considered most important were those most directly relevant to clinical practice. These were: understanding when and how to make a referral to clinical genetics; taking and interpreting a family history; and identifying families with genetic disorders. Open comments stressed the importance of focusing on the clinical application of genetics in practice given the information overload that SpRs face within their training.
Developing learning outcomes: a consultation process
Based on the results of the Delphi process, and informed by the earlier study of trainees' views on genetics education, the research team identified six overarching learning outcomes in genetics for non-genetics SpRs. Learning outcomes specify what is to be achieved by the learner, describing how the trainee can apply their learning to practice. This reflects current educational practice which stresses the importance of outcome-based education.17 Each learning outcome was linked to the relevant knowledge, skills and attitudes considered most important by Delphi participants. The next stage was consultation with representatives from different specialties in order to explore the appropriateness of these learning outcomes for trainees from a range of specialties.
The learning outcomes were discussed with the Joint Committee on Medical Genetics and endorsed by specialist training leads from UK regional genetics centres as being appropriate and applicable to SpRs in all medical specialties. In order to emphasise the relevance of genetics to clinical practice, specialist training leads confirmed that these core concepts are best taught using examples from the relevant specialty. For example, to achieve the learning outcome ‘be able to recognise basic patterns of inheritance’, the three main Mendelian patterns of inheritance (autosomal dominant, autosomal recessive and X-linked recessive) could be taught using conditions relevant to the clinical practice of trainees in each specialty. For instance, autosomal dominant inheritance could be illustrated through Marfan syndrome for cardiology trainees, while tuberous sclerosis could be selected for dermatology trainees and Huntington's disease for neurology trainees. Work with other specialties is ongoing to identify relevant conditions for case studies.
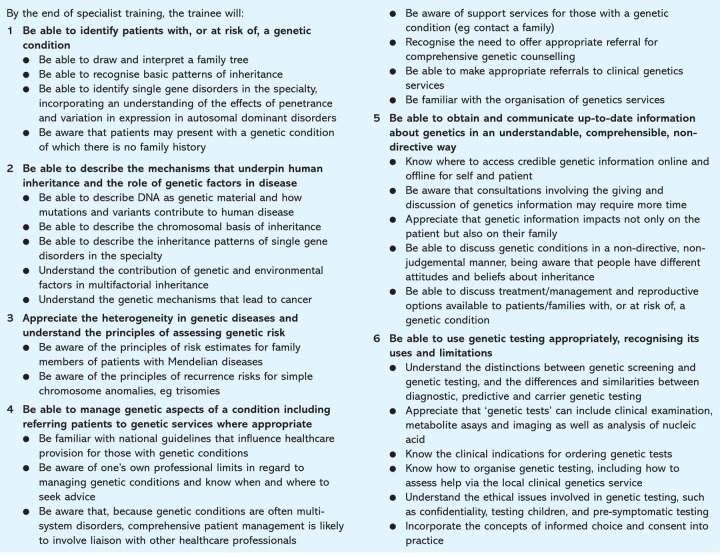
Consultation with non-genetics specialty education bodies began in spring 2006. The proposed learning outcomes were submitted to a number of specialty advisory boards and the Joint Committee on Higher Medical Training (now the Joint Royal Colleges of Physicians Training Board). Following this consultation the genetics learning outcomes for non-genetics SpRs were revised in August 2007 and are shown in Box 1.
Conclusions
This paper has described the development of core learning outcomes in genetics for non-genetics SpRs. The six learning outcomes reflect three key areas in which genetics impacts on clinical practice:
identifying patients
clinical management
communicating genetic information.
Firstly, clinicians fulfil a crucial role in identifying patients with, or at risk of, a genetic condition (learning outcome 1). In order to do this, they require an understanding of the mechanisms that underpin human inheritance and the role of genetic factors in disease, as well as an appreciation of the heterogeneity in genetic diseases and understanding of the principles of assessing genetic risk (learning outcomes 2 and 3). Secondly, clinicians are involved in clinical management of genetic conditions, including referring patients to genetic services and using genetic testing appropriately (learning outcomes 4 and 6). Thirdly, clinicians need to be able to communicate up-to-date information about genetics in an understandable and non-directive way (learning outcome 5).
The learning outcomes provide a useful framework for education, identifying educational priorities for genetics which are grounded in the reality of clinical practice and build upon genetics learning outcomes for medical students and Foundation trainees.18,19 In addition, these priorities are reflected in learning outcomes for the first two years of run-through specialist training.20 The learning outcomes presented in this paper therefore build on earlier learning to provide a continuum of genetics education throughout medical training.
Focusing education on the most important topics for clinical practice is essential to ensure that the limited time available for genetics education is used productively. The need for such education to be highly relevant to clinical practice has been emphasised by Delphi participants, specialist training leads from regional genetics centres and in previous research exploring trainees' views.11 The NHS National Genetics Education and Development Centre is working with a range of medical specialties to develop this work further and support genetics education for medical trainees at all levels of training.
Box 1. Core genetic learning outcomes for non-genetics medical specialty trainees.
Acknowledgments
We would like to thank all those involved in the Delphi process and the trainees involved in group interviews. The project to identify core genetic knowledge, skills and attitudes was funded by the Department of Health (DH) and conducted by the Centre for Research in Medical and Dental Education at the University of Birmingham and by the Centre for Education in Medical Genetics at Birmingham Women's Hospital. The development of core learning outcomes was conducted by the NHS National Genetics Education and Development Centre, which is funded by the DH and Welsh Assembly Government.
Reference
- 1.Van Langen IM. Birnie E. Leschot NH. Bonsel GJ. Wilde AAM. Genetic knowledge and counselling skills of Dutch cardiologists: sufficient for the genomics era? Eur Heart J. 2003;24:560–6. doi: 10.1016/S0195-668X(02)00522-5. [DOI] [PubMed] [Google Scholar]
- 2.Burton H. Addressing genetics delivering health. A strategy for advancing the dissemination and application of genetics knowledge throughout our health professions. Cambridge: Public Health Genetics Unit; 2003. [Google Scholar]
- 3.Collins FS. Guttmacher AE. Genetics moves into the medical mainstream. JAMA. 2001;286:2322–4. doi: 10.1001/jama.286.18.2322. [DOI] [PubMed] [Google Scholar]
- 4.Gschwind A. Fischer OM. Ullrich A. The discovery of receptor tyrosine kinases: targets for cancer therapy. Nat Rev Canc. 2004;4:361–70. doi: 10.1038/nrc1360. [DOI] [PubMed] [Google Scholar]
- 5.Van't Veer LJ. Dai H. van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415:530–6. doi: 10.1038/415530a. [DOI] [PubMed] [Google Scholar]
- 6.Lacro RV. Dietz HC. Wruck LM, et al. Rationale and design of a randomized clinical trial of beta-blocker therapy (atenolol) versus angiotensin II receptor blocker therapy (losartan) in individuals with Marfan syndrome. Am Heart J. 2007;154:624–31. doi: 10.1016/j.ahj.2007.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith FJ. Irvine AD. Terron-Kwiatkowski A, et al. Loss-of-function mutations in the gene encoding filaggrin cause ichthyosis vulgaris. Nat Genet. 2006;38:337–42. doi: 10.1038/ng1743. [DOI] [PubMed] [Google Scholar]
- 8.Palmer CN. Irvine AD. Terron-Kwiatkowski A, et al. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor in atopic dermatitis. Nat Genet. 2006;38:441–6. doi: 10.1038/ng1767. [DOI] [PubMed] [Google Scholar]
- 9.Wellcome Trust Case Control Consortium. Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007;447:661–78. doi: 10.1038/nature05911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hayflick SJ. Eiff MP. Will the learners be learned? Genet Med. 2002;4:43–4. doi: 10.1097/00125817-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Burke S. Stone A. Bedward J. Thomas H. Farndon P. A ‘neglected part of the curriculum’ or ‘of limited use’? Views on genetics training by non-genetics trainees and implications for delivery. Genet Med. 2006;8:109–15. doi: 10.1097/01.gim.0000200159.19920.b5. [DOI] [PubMed] [Google Scholar]
- 12.Burke S. Bennett C. Bedward J. Farndon P. The experiences and preferences of people receiving genetic information from healthcare professionals. Birmingham: NHS National Genetics Education and Development Centre; 2007. www.geneticseducation.nhs.uk. [Google Scholar]
- 13.Kirk M. Fit for practice in the genetics era: a competence based education framework for nurses, midwives and health visitors. Glamorgan: Genomics Policy Unit; 2003. [Google Scholar]
- 14.Burke S. Stone A. Martyn M. Thomas H. Farndon P. Genetic education for GP registrars. Birmingham: University of Birmingham; 2005. [Google Scholar]
- 15.NHS National Genetics Education and Development Centre and Skills for Health. Competences for genetics in clinical practice. Birmingham: NHS National Genetics Education and Development Centre and Skills for Health; 2007. www.geneticseducation.nhs.uk. [Google Scholar]
- 16.Wilson S. Eagles JM. Platt JE. McKenzie H. Core undergraduate psychiatry: what do non-specialists need to know? Med Educ. 2007;41:698–702. doi: 10.1111/j.1365-2923.2007.02790.x. [DOI] [PubMed] [Google Scholar]
- 17.Postgraduate Medical Education and Training Board. Guide for curricula writing. London: PMETB; 2005. [Google Scholar]
- 18.NHS National Genetics Education and Development Centre. Genetics learning outcomes for medical students. Birmingham: NHS National Genetics Education and Development Centre and Skills for Health; 2007. www.geneticseducation.nhs.uk. [Google Scholar]
- 19.Foundation Programme. Foundation Programme Curriculum. www.foundationprogramme.nhs.uk.
- 20.Federation of the Royal Colleges of Physicians. The physician of tomorrow: curriculum for core medical training and acute care common stem (medicine) (acute medicine level 1) London: PMETB; 2006. www.pmetb.org.uk. [Google Scholar]