Abstract
Non-invasive ventilation (NIV) has become the standard of care for most patients with ventilatory failure due to an acute exacerbation of chronic obstructive pulmonary disease (COPD). In all but a small minority, even of the very sickest, there is little to be lost by at least a short trial of NIV. In patients with acute cardiogenic pulmonary oedema, NIV results in a more rapid physiological improvement and resolution of dyspnoea, but the benefits in terms of survival have been called into question by two recent randomised controlled trials. There are no randomised controlled trials of NIV in patients with acute ventilatory failure due to obesity but the outcome from invasive ventilation is poor and the results of NIV encouraging. Finally, NIV may have a role during the transition from active care, aimed to extend life, to palliative care.
Key Words: chronic obstructive pulmonary disease (COPD), cardiogenic pulmonary oedema, respiratory failure, obesity, palliative care
Introduction
Non-invasive ventilation (NIV) now has a major role in the management of patients presenting with respiratory failure on the acute medical take. It has a number of potential advantages compared with invasive mechanical ventilation (IMV). The obvious attraction is the avoidance of intubation and its attendant complications. Its use opens up new opportunities in the management of patients with ventilatory failure, particularly with regard to location and the timing of intervention. With NIV, paralysis and sedation are not needed and ventilation outside the intensive care unit (ICU) is an option; given the considerable pressure on ICU beds in some countries, the high costs and as admission, for some patients, is a distressing experience1 this is an attractive option. Ventilatory support can be introduced at an earlier stage in the evolution of ventilatory failure and it is possible with NIV to give very short periods of support, which in some cases may be sufficient to reverse the downward spiral into life-threatening ventilatory failure. Patients can cooperate with physiotherapy and eat normally. Intermittent support is possible. Patients can start mobilising at an early stage and can communicate with medical and nursing staff and with their family; this is likely to reduce feelings of powerlessness and anxiety associated with ventilatory support.2 A reduction in complications, particularly infections, is a consistent and important finding.3,4 However NIV does have limitations. Concerns have been voiced that it may delay endotracheal intubation (ETI) and mechanical ventilation, resulting in a worse outcome.5,6 NIV may be time consuming for medical and nursing staff, though in part this may represent a learning effect. Some patients find the mask claustrophobic and unpleasant. Facial pressure sores occur in 2% of patients.3
The use of NIV for patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD), cardiogenic pulmonary oedema, acute hypercapnic respiratory failure due to obesity and an emerging role in the management of patients at the end of life will be reviewed in this article.
Acute exacerbations of chronic obstructive pulmonary disease
Prospective randomised controlled trials (RCTs) of the use of NIV in AECOPD have been performed in a variety of different locations and healthcare systems and in patients with exacerbations of varying severity. A meta-analysis of these studies has shown more rapid improvements in respiratory rate and pH, a reduction in the need for intubation and improved survival, reduced complications and length of hospital stay.7 These studies all excluded patients who required immediate IMV. The concern has been voiced that, particularly in the more severely ill, NIV may be harmful by delaying the institution of the ‘gold’ standard therapy, namely IMV.6 However Conti and colleagues8 reported a prospective RCT of NIV versus immediate ETI and MV in patients with an exacerbation of COPD. Not surprisingly their patients were sicker than those reported in previous studies, as evidenced by a mean pH of 7.2. There were two important messages from this study. Firstly, in these sicker patients they showed that NIV was no worse than ETI and MV. Secondly, in those who could be managed successfully with NIV there was an advantage both in the short term (reduced duration of ICU stay) but also in the year after hospital discharge (fewer readmissions and patients needing de novo long-term oxygen therapy). The intubation rate of 52% in the NIV group was higher than in other RCTs, which is not surprising given that these were a sicker group of patients. In common with other studies, some patients were still excluded, including those intubated prior to transfer to the ICU or those with respiratory arrest or pauses.
There is now evidence to support a clear strategy for the management of hypercapnic ventilatory failure in patients with AECOPD. Initial management should be focused on the prompt institution of standard medical therapy with steroids, nebulised bronchodilators and antibiotics and/or diuretics if indicated. Controlled oxygen, targeting a saturation of 88–92%9 is most important. Arterial blood gas tensions should be repeated after an appropriate interval, usually one to two hours.10 Approximately 20% of patients acidotic on arrival in accident and emergency can be expected to improve, with pH returning into the normal range with these interventions alone.11 NIV is recommended in hypercapnic patients when the pH remains less than 7.35 and the respiratory rate greater than 23 breaths per minute.12 Ten patients need to be treated with NIV to avoid one intubation. If the pH is <7.35 but >7.30, 80% of patients will get better with standard medical therapy13 and if the patient declines NIV, or is poorly tolerant, it is reasonable to adopt a wait-and-see approach, with monitoring of the clinical status, particularly respiratory rate, and repeat arterial blood gas analysis. If pH <7.3 the outcome without NIV is much worse with approximately 50% of patients meeting criteria for intubation and an increased mortality; NIV is therefore strongly advised. If pH <7.25 NIV is still strongly advised, accepting a higher likelihood of failure, but with clear advantages from NIV both in the short term, but also after discharge.8
Contraindications to NIV should be considered relative rather than absolute and have usually been included in guidelines because of theoretical concerns and because they have been exclusion criteria for the RCTs rather than having been positively shown to be harmful. NIV has been used in patients previously deemed unsuitable for NIV, namely those with coma.14 In a prospective, uncontrolled study of 958 patients receiving NIV for ARF 95 (10.1%) had a Glasgow Coma Scale score on ICU admission <8. In the subgroup of patients with COPD, the success rate in those with severe encephalopathy was 86%, which is excellent given the severity of the respiratory failure. A trial of NIV is reasonable in all but a small minority of patients presenting to hospital with an acidotic AECOPD.
Cardiogenic pulmonary oedema
There have been seven systematic reviews published since 2005. Overall there was a significant reduction in mortality for those patients treated with continuous positive airway pressure (CPAP) (relative risk 0.59, 95% confidence interval (CI) 0.28 to 0.90, p=0.015) and a trend towards improved survival with NIV.15 Both CPAP (relative risk 0.44, 95% CI 0.29 to 0.66, p=0.0003) and NIV (relative risk 0.50, 95% CI 0.27 to 0.90, p=0.02) showed benefit when intubation was an outcome. There was no difference in any outcome when CPAP and NIV were compared. There was a trend towards an increase in myocardial infarction (MI) rate with NIV, but this was largely due to the weighting of one study.16 Two recent trials have been published or presented at international conferences since the results of the systematic reviews. These may result in the reappraisal of the role of NIV in ACPO.
In the 3CPO trial,17 a multicentre open prospective randomised controlled trial, patients were randomised to one of three treatment arms: standard oxygen therapy delivered by variable delivery oxygen mask with resevoir bag, CPAP or bilevel ventilation. There was no difference between seven-day mortality for standard oxygen therapy (9.8%) and non-invasive ventilation (CPAP and bilevel ventilation, 9.5%; p=0.87). The combined end-point of seven-day death or intubation rate was similar irrespective of NIV modality (11.7% ν 11.1%, CPAP ν bilevel ventilation respectively; p=0.81). In comparison to standard oxygen therapy, NIV was associated with greater reductions in breathlessness, heart rate, acidosis and hypercapnia at one hour. There were no treatment-related adverse events. There were no differences in other secondary outcomes, such as MI rate, intubation, length of hospital stay or critical care admission rate.
In another trial,18 120 patients were enrolled in three French emergency departments to either CPAP or NIV. There was no difference between interventions for any outcome. Respiratory distress and physiology improved in both arms. Only 3% of patients required intubation and one died within the first 24 hours. Exploratory analysis of patients with and without hypercapnia did not change the rate of improvement or the difference between interventions. It is of interest that 68 potentially eligible patients had non-invasive support applied pre-hospital and 11 were intubated.
These results are contrary to findings of the meta-analyses despite similar improvements in physiological and gas exchange variables. The 3CPO trial was adequately powered and recruited more patients than the total combined experience of all the studies included in the meta-analyses.
There are a number of reasons why the 3CPO trial findings do not support the previous results and the conclusions drawn from meta-analyses. The discrepancy between results from a large multicentre randomised controlled trial and previous pooled data are not unique and the limitations of meta-analysis are well reported.19 Individual trials were composed of small treatment group sizes that varied between nine and 65 patients with recruitment rates of only 10–30% (cf 62% randomised in the 3CPO trial). In the meta-analyses, the small total number of outcome events was well below the recommended threshold of 20020 and this limits the generalisability of any findings. There is concern of reporting, publication and recruitment bias in individual published studies that will be compounded by pooled analysis.
Although not mandated, the 3CPO trial recommended a set of co-treatments for recruited patients. This specifically included buccal and intravenous nitrates. Approximately 90% of patients received this intervention. It is possible that the cardiovascular beneficial effects of NIV in acute cardiogenic pulmonary oedema have been masked by another treatment working, in particular nitrates, by the same mechanism, ie a reduction in preload and afterload. Indeed, Crane identified pre-hospital nitrate as being the only factor associated with improved mortality in a UK observational study of patients with ACPO.21 Co-treatments in previous small trials have often been incompletely characterised and documented and it is therefore unclear whether there is consistency in these treatments across trials.
The 3CPO trial may have failed to reveal a difference because the intervention was ineffectively delivered. Over 80% of sites had previous experience of NIV prior to the trial starting. There was a comprehensive training programme for all centres to ensure operator competence and consistency throughout the trial. Mean pressures for both CPAP (10 cm H2O) and NIPPV (14/7 cm H2O) are highly comparable with previous studies. Mean times of delivery of the intervention were a little over two hours, suggesting that the patients were physiologically and symptomatically significantly better within this short timeframe and again are similar to the recent data from France.18 There was crossover between interventions in all three arms of the 3CPO trial and these were analysed on an intention-to-treat basis. There were differing reasons with respiratory distress and hypoxia being more likely in the control arm and lack of patient tolerance in the two intervention arms. After these patients were removed from primary outcome analysis there remained no significant difference between groups, although mortality rates were lower.
Previous trials have indicated that the physiological improvement seen with NIV is translated into a reduction in tracheal intubation rates.15,22 In contrast, the 3CPO trial found no benefit in reducing intubation rates by NIV. Reasons for this are unclear but may reflect the differing patient populations, concomitant therapies and thresholds for intubation and mechanical ventilation across different countries, clinical environments and time periods. Intubations rates in the standard therapy arms vary from 35–65% in initial trials to 5–7% for recent trials in emergency department settings, despite similar severity of illness, in hospital mortality and length of hospital stay. Intubation rates in the intervention arms have also fallen considerably over time with some initial trials reporting intubation rates of up to 35% whereas recent reports have consistently suggested rates of around 5%. Indeed, a recent trial18 from France reported a 3% intubation rate, almost identical to that in the 3CPO trial. Given that the present and previous trials were by necessity ‘open’, there is concern of treatment bias with a differing threshold for intervention according to treatment allocation. It is important to note that intubation did not correlate with mortality in the 3CPO trial. Finally it has been suggested that the patients recruited were less unwell than those in other studies; in terms of the physiological disturbance these patients were in fact at the sickest end of the patients studied and indeed, in contrast to other studies, acidosis (mean pH 7.22) and hypercapnia (mean PaCO2 7.6 kPa) were invariable.
Obesity
Obesity has reached epidemic proportions and it is projected that this will worsen, with 50% of UK adults having a body mass index >30 kg/m2 by 2030. Obesity affects lung function and a study of 4,332 admissions in the USA found that mortality at 18 months was significantly worse in the obese, compared to the non-obese (23% ν 9%).23 There are no randomised controlled trials of the use of NIV in patients with ventilatory failure secondary to obesity. The outcome from invasive ventilation is generally poor and a case series in which patients who received NIV were compared with those who refused it showed a survival advantage for those receiving NIV (97% ν 42%)24; it should be stressed that this was not controlled and that there may have been other reasons for the observed difference. Particular problems with NIV in very obese patients include upper airway obstruction during sleep and the fact that the impedance to inflation may be very high requiring either the use of volume ventilators or the novel mode of volume-assured pressure support.25 Finally, there are major practical problems associated with nursing critically ill patients who are very obese. In numerical terms this patient group is very likely to increase; certainly the number of patients requiring home ventilation because of obesity hypoventilation is increasing year-on-year and in one study patients with obesity now comprise the largest single group.26
Palliative care
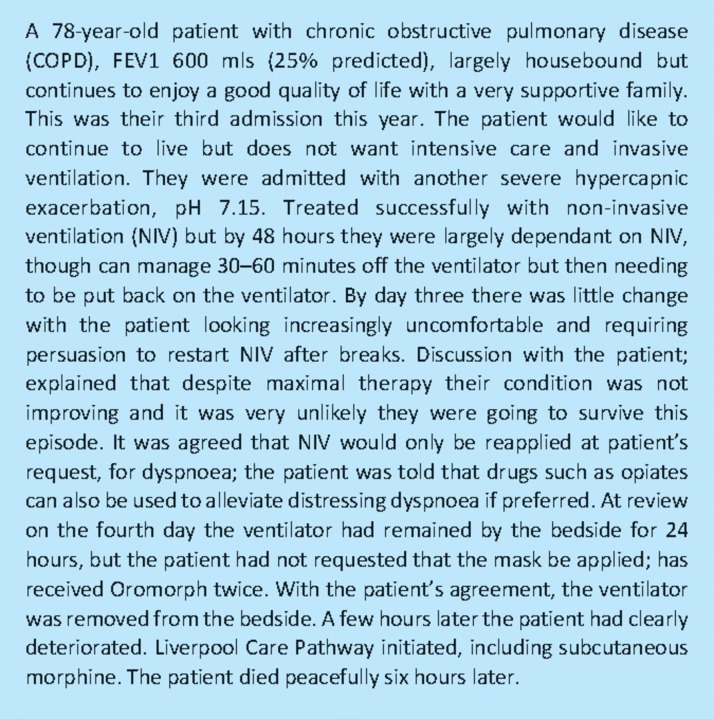
Finally there is an emerging role for NIV in the management of patients with end-stage COPD. It is well recognised that these patients receive suboptimal palliative care27; in part this relates to the great difficulty in recognising when the end is near. The boundary between life-sustaining therapy and palliation can move on a daily basis during an exacerbation as a patient's condition deteriorates.28 One of the biggest challenges facing doctors now and in the future is knowing when ‘enough is enough’.29 NIV provides a useful alternative to life-sustaining therapy, with limited palliative care, ie invasive ventilation, or medical therapy alone, which for patients with severe respiratory failure may well not be sufficient to sustain life, but does allow effective palliative care. With NIV, patients retain a real say in their care and because assisted ventilation is not all or nothing it is possible to move relatively easily between life-sustaining and palliative care. An example is given in Box 1.
Box 1. An example case.
Conclusions
There is now a robust evidence base for the use of NIV in AECOPD. NIV should be considered primarily as a means of preventing, rather than a direct alternative to, IMV but there is little to be lost except in a few situations by a short trial of NIV. The 3CPO trial has unequivocally demonstrated the safety of both NIPPV and CPAP in patients with acute cardiogenic pulmonary oedema and clearly shows that there is no increased risk of myocardial infarction with NIPPV. CPAP equipment is, in general, less complex and cheaper and, therefore, has advantages over NIPPV. In addition, a number of simple systems allow the delivery of 100% oxygen. In the majority of patients, medical therapy should be the primary treatment and NIV reserved for those who have significant respiratory distress and failure or those not improving with standard medical therapy. In the future there is likely to be an increasing role for NIV in patients with respiratory failure as a consequence of severe obesity and for managing patients who still want life-sustaining treatment, but when it is clear that this is no longer working then the transition to a more palliative approach should be made.
References
- 1.Easton C, MacKenzie F. Sensory-perceptual alterations: delirium in the intensive care unit. Heart Lung. 1988;17:229–37. [PubMed] [Google Scholar]
- 2.Seneff MG, Wagner DP, Wagner RP, Zimmerman JE, Knaus WA. Hospital and 1-year survival of patients admitted to intensive care units with acute exacerbation of chronic obstructive pulmonary disease. JAMA. 1995;274:1852–7. [PubMed] [Google Scholar]
- 3.Brochard L, Mancebo J, Wysocki M, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1995;333:817–22. doi: 10.1056/NEJM199509283331301. [DOI] [PubMed] [Google Scholar]
- 4.Girou E, Brun-Buisson C, Taille S, Lemaire F, Brochard L. Secular trends in nosocomial infections and mortality associated with noninvasive ventilation in patients with exacerbation of COPD and pulmonary edema. JAMA. 2003;290:2985–991. doi: 10.1001/jama.290.22.2985. [DOI] [PubMed] [Google Scholar]
- 5.Ambrosino N. Noninvasive mechanical ventilation in acute respiratory failure. Eur Respir J. 1996;9:795–807. doi: 10.1183/09031936.96.09040795. [DOI] [PubMed] [Google Scholar]
- 6.Wood KA, Lewis L, Von Harz B, Kollef MH. The use of noninvasive positive pressure ventilation in the emergency department. Chest. 1998;113:1339–46. doi: 10.1378/chest.113.5.1339. [DOI] [PubMed] [Google Scholar]
- 7.Lightowler JV, Wedzicha JA, Elliott MW, Ram FS. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ. 2003;326:185–9. doi: 10.1136/bmj.326.7382.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Conti G, Antonelli M, Navalesi P, et al. Noninvasive vs conventional mechanical ventilation in patients with chronic obstructive pulmonary disease after failure of medical treatment in the ward: a randomized trial. Inten Care Med. 2002;28:1701–7. doi: 10.1007/s00134-002-1478-0. [DOI] [PubMed] [Google Scholar]
- 9.O'Driscoll BR, Howard LS, Davison AG, on behalf of the British Thoracic Society BTS guideline for emergency oxygen use in adult patients. Thorax. 2008;63(Suppl_6):vi1–68. doi: 10.1136/thx.2008.102947. [DOI] [PubMed] [Google Scholar]
- 10.Roberts CM, Brown JL, Reinhardt AK, et al. Non-invasive ventilation in chronic obstructive pulmonary disease: management of acute type 2 respiratory failure. Clin Med. 2008;8:517–21. doi: 10.7861/clinmedicine.8-5-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Plant PK, Owen J, Elliott MW. One year period prevalence study of respiratory acidosis in acute exacerbation of COPD; implications for the provision of non- invasive ventilation and oxygen administration. T. horax. 2000;55:550–4. doi: 10.1136/thorax.55.7.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.British Thoracic Society Standards of Care Committee Non-invasive ventilation in acute respiratory failure. Thorax. 2002;57:192–211. doi: 10.1136/thorax.57.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet. 2000;355:1931–5. doi: 10.1016/S0140-6736(00)02323-0. [DOI] [PubMed] [Google Scholar]
- 14.Diaz GG, Alcaraz AC, Talavera JCP, et al. Non-invasive positive-pressure ventilation to treat hypercapnic coma secondary to respiratory failure. Chest. 2005;127:952–60. doi: 10.1378/chest.127.3.952. [DOI] [PubMed] [Google Scholar]
- 15.Peter JV, Moran JL, Phillips-Hughes J, Graham P, Bersten AD. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet. 2006;367:1155–63. doi: 10.1016/S0140-6736(06)68506-1. [DOI] [PubMed] [Google Scholar]
- 16.Mehta S, Jay GD, Woolard RH, et al. Randomized, prospective trial of bilevel versus continuous positive airway pressure in acute pulmonary oedema. Crit Care Med. 1997;25:620–8. doi: 10.1097/00003246-199704000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Gray A, Goodacre S, Newby DE, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med. 2008;359:142–51. doi: 10.1056/NEJMoa0707992. [DOI] [PubMed] [Google Scholar]
- 18.Moritz F, Brousse B, Gellee B, et al. Continuous positive airway pressure versus bilevel noninvasive ventilation in acute cardiogenic pulmonary edema: a randomized multicenter trial. Ann Emerg Med. 675;50:666–75. doi: 10.1016/j.annemergmed.2007.06.488. [DOI] [PubMed] [Google Scholar]
- 19.LeLorier J, Gregoire G, Benhaddad A, Lapierre J, Derderian F. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536–42. doi: 10.1056/NEJM199708213370806. [DOI] [PubMed] [Google Scholar]
- 20.Flather MD, Farkouh ME, Pogue JM, Yusuf S. Strengths and limitations of meta-analysis: larger studies may be more reliable. Controlled Clinical Trials. 1997;18:568–79. doi: 10.1016/S0197-2456(97)00024-X. [DOI] [PubMed] [Google Scholar]
- 21.Crane SD. Epidemiology, treatment and outcome of acidotic, acute, cardiogenic pulmonary oedema presenting to an emergency department. Euro J Emerg Med. 2002;9:320–4. doi: 10.1097/00063110-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Masip J, Roque M, Sanchez B, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA. 2005;294:3124–30. doi: 10.1001/jama.294.24.3124. [DOI] [PubMed] [Google Scholar]
- 23.Nowbar S, Burkart KM, Gonzales R, et al. Obesity-associated hypoventilation in hospitalized patients: prevalence, effects, and outcome. Am J Med. 2004;116:1–7. doi: 10.1016/j.amjmed.2003.08.022. [DOI] [PubMed] [Google Scholar]
- 24.Perez de Llano LA, Golpe R, Ortiz Piquer M, et al. Short-term and long-term effects of nasal intermittent positive pressure ventilation in patients with obesity-hypoventilation syndrome. Chest. 2005;128:587–94. doi: 10.1378/chest.128.2.587. [DOI] [PubMed] [Google Scholar]
- 25.Storre JH, Seuthe B, Fiechter R, et al. Average volume-assured pressure support in obesity hypoventilation: a randomized crossover trial. Chest. 2006;130:815–21. doi: 10.1378/chest.130.3.815. [DOI] [PubMed] [Google Scholar]
- 26.Janssens JP, Derivaz S, Breitenstein E, et al. Changing patterns in long-term noninvasive ventilation: a 7-year prospective study in the Geneva Lake area. Chest. 2003;123:67–79. doi: 10.1378/chest.123.1.67. [DOI] [PubMed] [Google Scholar]
- 27.Gore JM, Brophy CJ, Greenstone MA. How well do we care for patients with end stage chronic obstructive pulmonary disease (COPD)? A comparison of palliative care and quality of life in COPD and lung cancer. Thorax. 2000;55:1000–6. doi: 10.1136/thorax.55.12.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lanken PN, Terry PB, Delisser HM, et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Resp Crit Care Med. 2008;177:912–27. doi: 10.1164/rccm.200605-587ST. [DOI] [PubMed] [Google Scholar]
- 29.Bradley N. Obituary: Kieran Sweeney. BMJ. 2010;340:c733. [Google Scholar]