Key Points
Almost one-quarter of adults in Britain are drinking alcohol at hazardous or harmful levels; 6% are dependent drinkers
Dependent drinkers who have previously experienced severe withdrawal symptoms, have a history of fitting, significant comorbidities or complex social needs are best withdrawn from alcohol in hospital; benzodiazepines are the drugs of choice
Patients with severe alcoholic hepatitis should be treated with corticosteroids and supported nutritionally; the diagnosis should be biopsy-proven
Patients with alcohol-related cirrhosis with refractory decompensation, despite abstinence from alcohol for more than three months, should be considered for transplantation
Population-wide risk reduction may be achievable via change in alcohol policies, but active and responsible governmental and non-governmental interest is paramount for effective policy change
Alcohol misuse is a major issue for medical and social agencies alike. Although the harmful effects of excessive consumption are well publicised, one-quarter of adults in England still consume alcohol at hazardous or harmful levels.1 A global alcohol strategy has recently been agreed by the World Health Organization,2 supported in Britain by extensive guidance from the National Institute for Health and Clinical Excellence (NICE),3–5 parliamentary committees6,7 and non-governmental organisations – but to whom does this advice apply?
The sobering factitles
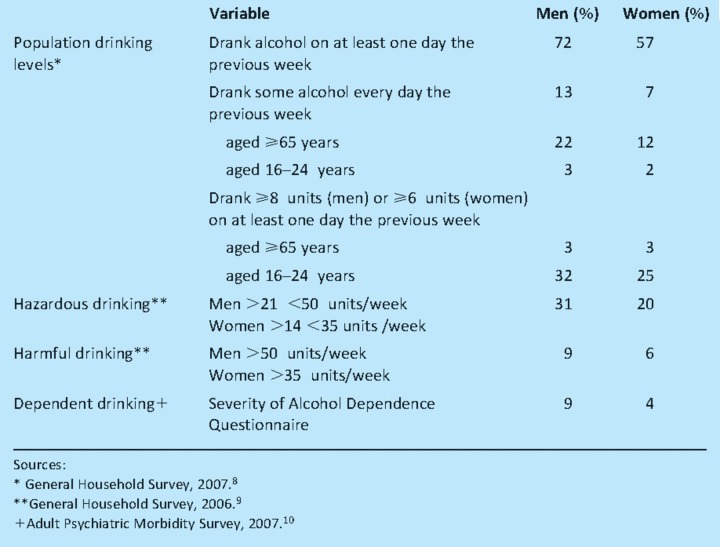
Most adults in Britain drink alcohol and do so responsibly.1 However, some 33% of men and 16% of women drink hazardously – that is, at a level which increases their risk of alcohol-related harm, while 6% of men and 4% of women drink to an extent that is mentally or physically harmful.8,9 In 2007, 9% of men and 4% of women in England were dependent on alcohol (Table 1).10
Table 1.
Adult drinking behaviour by gender (individuals in England aged ≥16 years).1
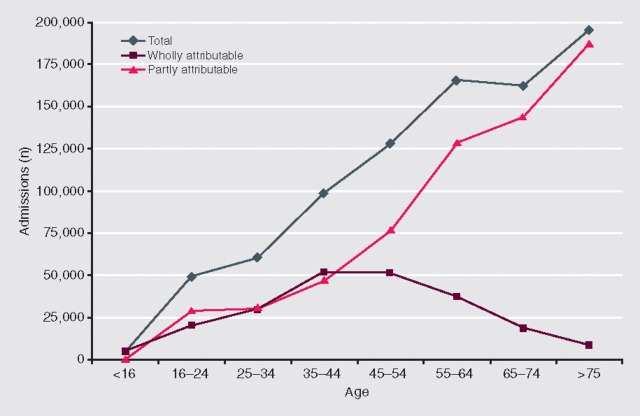
Alcohol misuse is associated with a wide variety of physical health problems and is also causally linked to accidents, injuries and poisoning. There was a total of 863,300 alcohol-related hospital admissions in England in 2007–8, of which 222,600 were for diseases wholly attributable to alcohol. Two-thirds of these admissions were for mental/behavioural disorders due to alcohol use, while 30,100 were for alcohol-related liver injury.11,12 Men make up almost two-thirds of the admissions. There are significant differences in admission ages for conditions that are wholly or partly alcohol-related (Fig 1).11,12
Fig 1.
Alcohol-related hospital admissions in England, by age, 2007–8. Activity in NHS hospitals and commissioned activity in the independent sector. Finished activity episodes are identified when an alcohol-related diagnosis is recorded in any of the 20 primary and secondary fields in a Hospital Episode Statistics record. Wholly attributable conditions are alcohol-specific (eg alcohol dependence, alcoholic cirrhosis of the liver), peak age for admission 35–54 years. Partly attributable conditions such as accidents, injuries and some cancers where varying proportions are alcohol-attributable; total figures adjusted accordingly, highest number of admissions aged >75 years.11,12
In 2007, 6,541 deaths in England were directly attributable to alcohol, 4,249 11,12 If account is taken of attributable fractions, the number of overall deaths increases substantially, with an estimated figure for 2005 of 14,982.11,12 The cost of alcohol-related harm to the NHS is £2.7 billion a year at 2006–7 prices.13
Management of alcohol dependentitlee
Alcohol withdrawal
Approximately 6% of adults in Britain are dependent on alcohol.8–10 Management of these individuals centres initially on their safe withdrawal from alcohol.4,5 The withdrawal may be planned as part of a package of care, and can often be managed safely and effectively in an outpatient setting or at home supervised by a specialist community nurse. However, certain patients are best withdrawn from alcohol in hospital, including those who have experienced severe withdrawal symptoms in the past, have a history of fitting, significant physical and mental comorbidities or complex social needs, and those aged 18 or younger.
Frequently, however, the withdrawal is unplanned, perhaps in the context of an intercurrent illness or accident. In these instances the decision to hospitalise is determined by the severity of the withdrawal, concomitant illness and any comorbidities. However, there are no hard or fast rules.
Patients with moderate or severe alcohol withdrawal symptoms should be sedated. The drug most commonly used is chlordiazepoxide, given in a standard dose reducing steadily over several days.4,5 Severe established withdrawal, or delirium tremens, is best treated initially with a quick-acting benzodiazepine such as lorazepam, given orally or parenterally, or with haloperidol. Withdrawal seizures should be treated with parenteral lorazepam. Drug dosages should be reduced in patients with cirrhosis and those with respiratory disease because of the risk of respiratory depression. Prophylactic parenteral thiamine should be given to individuals withdrawing from alcohol if they are malnourished, have decompensated liver disease or an acute illness or injury. Otherwise, oral supplements should be used.4
Relapse prevention
Once patients have been successfully withdrawn from alcohol they need support to maintain abstinence in the longer term.5 The level and type of support needed varies considerably.
There are a variety of treatment options although the most successful are psycho- social therapies5 including cognitive behavioural therapies, counselling, solution focused relapse prevention, and family/couples therapy.
Pharmacotherapy is a useful adjunct to treatment but is currently underutilised.1,5
Acamprosate has a significant, albeit modest, effect on drinking behaviour. It is usually prescribed in a daily divided dose of 2 g and given for 12–18 months. It has an excellent safety profile. Greatest benefit is seen if treatment is started just before the patient is withdrawn from alcohol.
Naltrexone also has a significant but modest effect on drinking behaviour. It is prescribed in a dose of 50 mg daily for up to 12 months. It interacts with opioid drugs and hepatotoxicity has been observed with high doses. It is not currently licensed for use in the UK.
There is no real evidence base for the use of disulfiram, although it is still popular in some centres.
Treatment can be delivered within the community or by specialist addiction services. However, as the range of therapies provided in both settings is similar, the boundaries between them are noticeably blurred. GPs now play a more active and important role in the management of these patients. Self-help groups such as Alcoholic Anonymous provide a valuable service. Despite the guidance provided by the Department of Health in 2007,14 alcohol services are still poorly developed: only one in 18 alcohol-dependent individuals in the UK accesses treatment each year.15
Management of alcohol-related liver diseatitlee
Although alcohol produces a spectrum of liver injury ranging from fatty liver to alcoholic hepatitis, cirrhosis and hepatocellular carcinoma, only a minority of individuals (perhaps <20%) develop significant liver injury. These lesions do not occur in isolation and may coexist.
Over the past 30 years, mortality from alcohol-related liver disease has increased by over 450% and deaths in young people are rising sharply.16 Admissions to intensive care units in England and Wales for alcohol-related liver disease tripled between 1996 and 2005.17
Few specific management issues arise in these patients. The most important is to secure long-term abstinence from alcohol. In the majority of individuals it is all that is required.
A minority of patients with alcoholic hepatitis present with features of severe hepatic dysfunction, many on a background of already established cirrhosis. The mortality rate in these individuals may be as high as 40%. However, the outcome can be significantly improved by treatment with corticosteroids, typically prednisolone 40 mg daily reducing over six weeks.5 A discriminant function (DF) of above 32 identifies patients who will benefit from treatment:
DF = 4.6 × (prothrombin time [patient–control]) + bilirubin/17
The diagnosis of severe alcoholic hepatitis should be biopsy-proven, but this need not delay the start of treatment.4 Patients should also receive vigorous nutritional support. A small number of patients do not respond to steroids and the treatment options for them are limited. Transplantation has been used in some centres but its use is contentious.
Patients with decompensated alcohol-related cirrhosis who have not improved despite optimal management and abstinence from alcohol for at least three months should be considered for transplantation.5 At present, patients with alcohol-related liver disease are underrepresented on the majority of transplant waiting lists in the UK.
Prevention: the bigger pictutitlee
Population approach
Guidance produced by both the House of Commons Health Select Committee6 and the Public Accounts Committee7 suggests that changes in government policy are likely to be highly effective – and cost-effective – in reducing alcohol-related harm, and that national level action is needed to reduce alcohol consumption in the population as a whole.
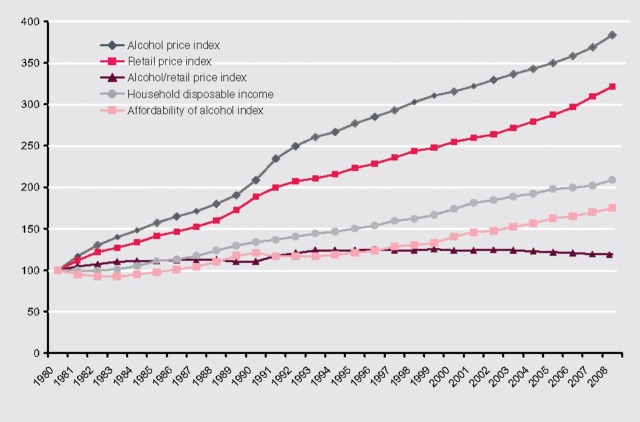
Between 1980 and 2008 alcohol became 75% more affordable as incomes increased faster than the price of alcohol (Fig 2).1,18,19 Today, 80% of alcohol consumed in the UK is purchased by less than 30% of the population, suggesting that low pricing is encouraging consumption in those who already drink more heavily.3 Making alcohol less affordable is the most effective way of reducing alcohol-related harm.3,20 A review of pricing policies is urgently needed. Current excise duty regimens, for example, are anomalous and should be altered to link alcohol duty to the strength of each product. Likewise, the introduction of minimum pricing has long been mooted.
Fig 2.
Affordability of alcohol, 1980–2008: indices of alcohol price, retail price for all items, real household disposable income and the consequent affordability of alcohol (indices: 1980 = 100).18,19
Stricter licensing laws would reduce the consumption of alcohol by making it less available. Stricter marketing laws would work as effectively. Changes in advertising standards are likely to be crucial in any coordinated effort to reduce alcohol-related harm, particularly in young people.3 Government expenditure on promoting alcohol awareness in 2009–10 was £17.6 million whereas the drinks industry spent £600–800 million on promoting consumption.3
Individual approach
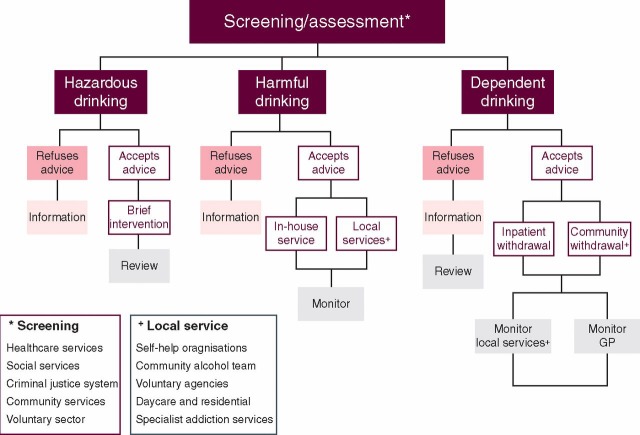
Early detection and intervention are key to the prevention of alcohol dependence and harm. NICE guidance recommends that all NHS and other professionals in the public, private, community and voluntary sector should carry out alcohol screening as an integral part of practice,3 using a validated, screening questionnaire such as the Alcohol Use Disorders Identification Test (AUDIT).21 Where impractical, screening could be targeted at high-risk groups.
Patients identified as drinking hazardously should be offered either immediate or scheduled motivational advice in the form of a brief intervention (Fig 3). A more prolonged, extended brief intervention may be necessary for some. For many patients, these brief interventions are sufficient to induce lifestyle changes, but they should be reviewed regularly.
Fig 3.
Screening for alcohol use disorders and subsequent proposed care pathways (GP = general practitioner).
Additional help may be required for those drinking in a harmful way or with alcohol dependence and in those who do not respond to brief intervention. Patients who are severely dependent or have coexistent psychiatric and/or physical morbidity should be referred to specialist services (Fig 3).
Conclusiotitles
The hepatologist has a clear role in the management of individuals with significant alcohol-related liver injury, the psychiatrist in managing the patient at the more severe end of the dependence spectrum, and the economist in informing fiscal policy. However, the effective management of the social, health and economic problems caused by alcohol misuse requires a much broader collaborative and multidisciplinary approach led ultimately by government.
References
- 1.The NHS Information Centre . Statistics on alcohol: England. Leeds: The Health and Social Care Information Centre; 2009. [Google Scholar]
- 2. Strategies to reduce the harmful use of alcohol. Report submitted to the 61st World Health Assembly. Geneva: World Health Organization, 2008.
- 3. Centre for Public Health at the National Institute for Health and Clinical Excellence. Alcohol-use disorders: preventing the development of hazardous and harmful drinking. Public Health guidance PH24. London: NICE, 2010.
- 4. National Institute for Health and Clinical Excellence. Alcohol-use disorders: diagnosis and clinical management of alcohol-related physical complications. Clinical Guideline CG100. London: NICE, 2010.
- 5. National Institute for Health and Clinical Excellence. Alcohol-use disorders: diagnosis, assessment and management of harmful drinking and alcohol dependence. Clinical Guideline. London: NICE, 2011. [PubMed]
- 6. House of Commons Public Accounts Committee. Reducing alcohol harm: health services in England for alcohol misuse. London: The Stationery Office, 2009.
- 7. House of Commons Health Select Committee. Alcohol first report of session 2009–10. London: The Stationery Office, 2010.
- 8. General Household Survey, 2007. London: The Office for National Statistics, 2007.
- 9. General Household Survey, 2006. London: The Office for National Statistics, 2006.
- 10. The Adult Psychiatric Morbidity Survey, 2007. The NHS Information Centre, 2008. www.ic.uk/pubs/psychiatricmorbidity07.
- 11. Hospital Episode Statistics. The NHS Information Centre, 2008. www.hesonline.org.uk.
- 12.Jones L, Bellis M, Dedham D, Sumnall H, Tocque K. Alcohol attributable fractions for England: alcohol attributable mortality and hospital admissions. Liverpool: North West Public Health Observatory; 2008. [Google Scholar]
- 13.Department of Health . The cost of alcohol harm to the NHS in England: An update to the Cabinet Office (2003) study. London: DH; 2008. [Google Scholar]
- 14.Department of Health . Models of care for alcohol misusers (MoCAM) London: DH; 2006. [Google Scholar]
- 15.Drummond DC, Oyefeso N, Phillips T, et al. Alcohol Needs Assessment Research Project: the 2004 National Alcohol Needs Assessment for England. London: Department of Health; 2005. [Google Scholar]
- 16.Prime Minister's Strategy Unit . Strategy Unit Alcohol Harm Reduction Project: Interim Analytical Report. London: Cabinet Office; 2003. [Google Scholar]
- 17.Welch C, Harrison D, Short A, Rowan K. The increasing burden of alcoholic liver disease on United Kingdom critical care units: secondary analysis of a high quality clinical database. J Health Serv Res Policy. 2008;3((Suppl 2)):40–4. doi: 10.1258/jhsrp.2007.007101. [DOI] [PubMed] [Google Scholar]
- 18.Focus on Consumer Price Indices. London: The Office for National Statistics; 2010. [Google Scholar]
- 19.Real Households Disposable Income: Economic Trends. London: The Office for National Statistics; 2008. [Google Scholar]
- 20.Chisholm D, Rehm J, Van Ommeren M, Monteiro M. Reducing the global burden of hazardous alcohol use: a comparative cost-effectiveness analysis. J Stud Alcohol. 2004;65:782–93. doi: 10.15288/jsa.2004.65.782. [DOI] [PubMed] [Google Scholar]
- 21.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]