Corrigendum
D'Arcy J, Myerson SG. Investigations in valvular heart disease. Clin Med 2010;10:172–6
Please note that Dr Myerson and Dr d'Arcy would like to acknowledge support from the Oxford NIHR Biomedical Research Centre programme in relation to this article.
Key points
The need for liver transplantation is increasing as mortality from liver disease is rising and outcomes after transplant are excellent
As a consequence of the shortage of donor livers, guidelines for selection and allocation have to be developed that are fair, just, equitable, transparent and, where possible, evidence-based
The traditional pool of donors is shrinking, so resources are prioritised to increasing awareness of organ donation, dispelling myths, and ensuring that all potential donors are identified and given the opportunity to donate their organs after death
The donor pool is being expanded by the use of donation after cardiac death, by using extended criteria donor grafts, by splitting livers to allow two recipients to receive organs from one donor, by increasing use of living donors and domino transplants
The success of liver transplantation in improving both the quality and length of life should not divert attention from the need to develop strategies for improving outcomes of those with acute and chronic liver disease
Over the last two decades, the cirrhosis mortality rates have almost doubled in men and increased by half in women with cirrhosis mortality rates in Scotland being among the highest in Europe (45.2 per 100 000 men and 19.9 per 100 000 women in 2002)1; this corresponds with a 45% in the incidence of cirrhosis and 69% in prevalence during the decade 1991–2001, with an estimated 30 000 people living with cirrhosis and at least 7,000 new cases being diagnosed each year.2
Despite the many advances made in the management of patients with cirrhosis, transplantation remains the only definitive treatment for those with end-stage disease.
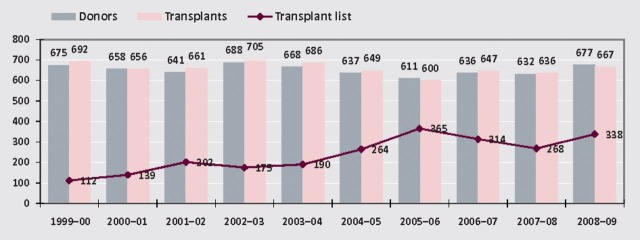
Liver transplantation (LT) is now a routine procedure with five-year survival of more than 70%.3 However, there is a shortage of grafts: 15% listed patients die while awaiting a graft.4 The number on the UK transplant list has trebled over the last 10 years while the availability of donor organs has increased only modestly (Fig 1).
Fig 1.
Deceased donor liver programme in the UK, 1 April 1999 to 31 March 2009 (adapted from NHS Blood and Transplant.5)
Current indications and contraindicatiotitles
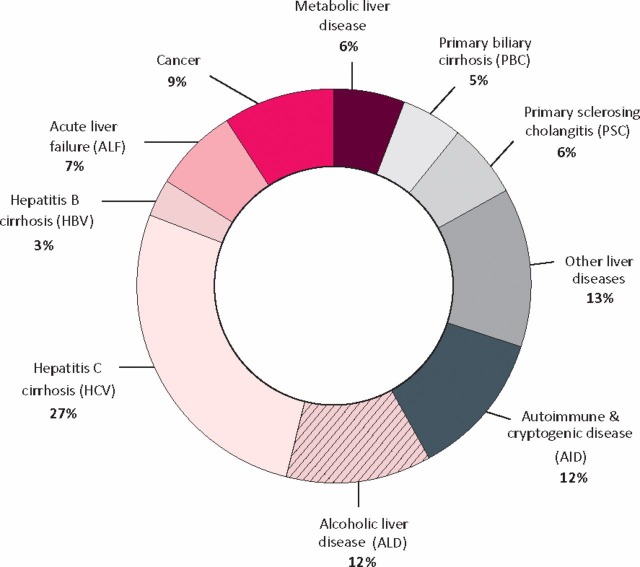
The proportion of patients grafted for alcohol-related liver disease (ALD) and viral hepatitis (especially hepatitis C (HCV)) (Fig 2) is rising while the proportion of patients grafted for malignancy and cholestatic diseases is falling. Alcohol remains a controversial indication, although these patients have similar long-term outcomes to patients grafted for other indications (indeed, better than those grafted for HCV). Non-alcoholic fatty liver disease is increasing and is an increasing indication for LT.7 Absolute contraindications are listed in Table 1.
Fig 2.
Indications for liver transplant (United Network for Organ Sharing (UNOS)).6
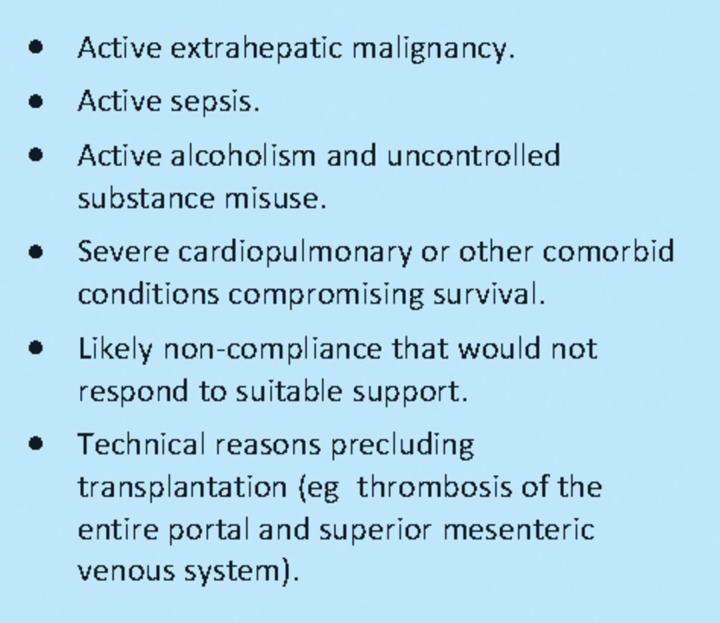
Table 1.
Absolute contraindications to liver transplantation.
Patient selectititlen
Patients should be considered for selection if:
the probability of survival without a transplant is less than survival with a transplant
they have a survival probability of more than 50% at five years with an acceptable quality of life
they have an unacceptable quality of life from the liver disease.
Criteria for selection are also designed to ensure that those patients who are listed will have a reasonable expectation of getting a graft – thus the size of the list does not reflect the need.
Assessment of prognosis
Several models have been developed to assess prognosis. The model for end-stage liver disease (MELD) score was initially developed to assess short-term prognosis following shunt procedures;8 it is based on serum creatinine, serum bilirubin and the international normalised ratio. Additional points are given for liver cell cancer (> 2cm in diameter). The model has been validated in many clinical situations and different populations. However, there are concerns over reproducibility of some analytes and gender effects of creatinine.
The United Kingdom model for end-stage liver disease (UKELD), developed and validated for patients awaiting liver transplantation in the UK, contains the same variables as the MELD (although with different strengths) and serum sodium. A MELD score greater than 16 or a UKELD score above 49 indicate a survival benefit from transplant.
Selection criteria
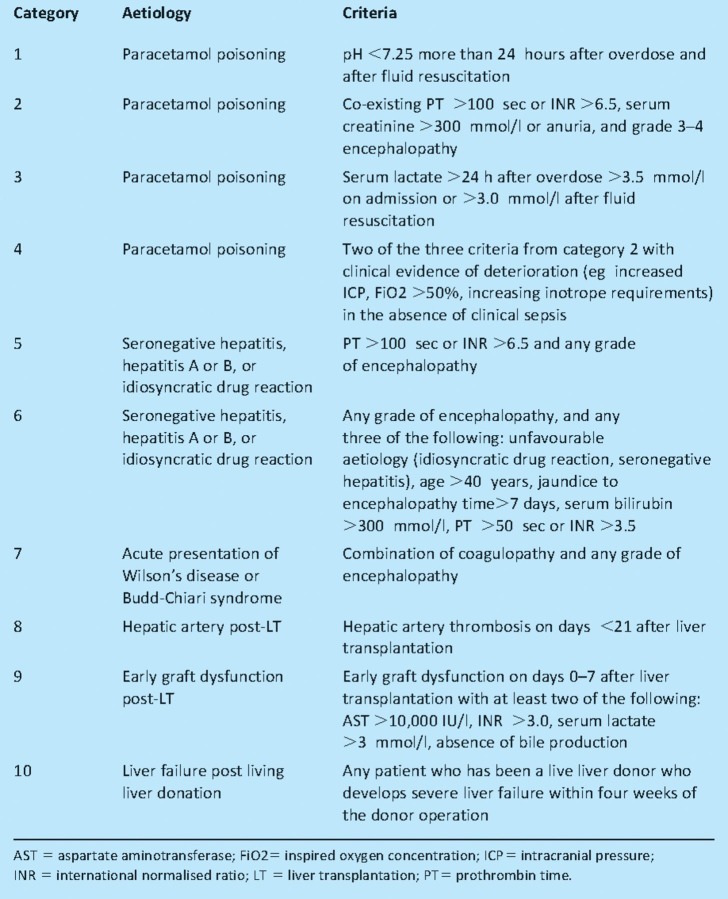
The selection criteria for those with acute liver failure are shown in Table 2. For those with chronic liver disease, there are three categories for listing:
projected one-year liver disease mortality without transplantation of over 9% (the current one-year survival after transplant is 91% in the UK)
hepatocellular carcinoma (HCC) within agreed criteria
Table 2.
Current UK blood and transplant criteria for registration as a super-urgent transplant: registered at UK Transplant, donor livers available from whole national pool. Adapted with permission from BMJ Publishing Group Ltd.9
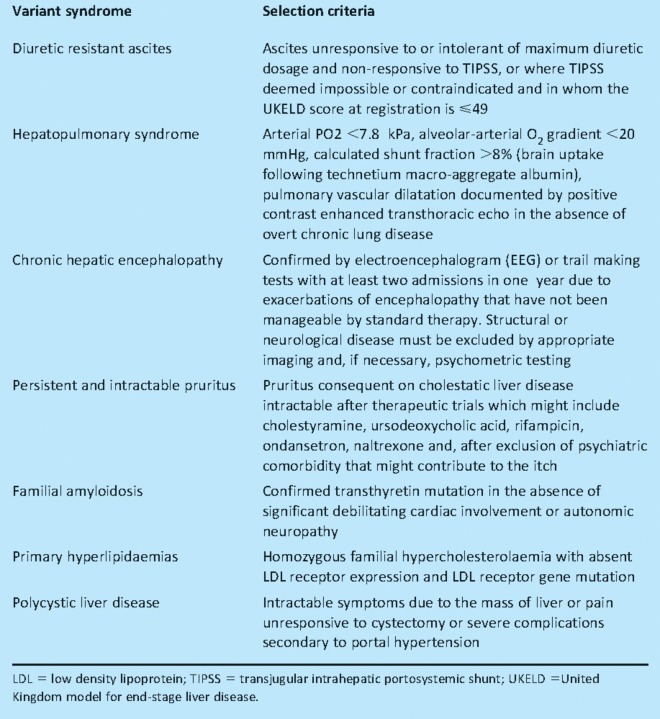
Table 3.
Variant syndromes and definitions for selection to the adult elective liver transplant waiting list. Adapted with permission from BMJ Publishing Group Ltd.9
Liver allocatititlen
At present, donated organs are allocated to one of the seven UK designated liver transplant centres. The centre's retrieval zone is adjusted to ensure equity of access. Allocation is determined by the centre, based primarily on ensuring optimal outcome rather than reducing mortality on the list. This policy is being reviewed. In the USA, minimal listing criteria were introduced, together with the creation of a ‘Status 1’ category (highest priority).10 The Child–Turcotte–Pugh (CTP) scoring system was introduced as a semi-objective measure of disease severity; patients required a CTP score above 7. Because of the huge number of patients on the waiting list and, to reduce the waiting list mortality, a new system was introduced so that grafts were offered to the sickest patient first (as assessed by the highest MELD score).
Alcohol-related liver disease
Transplantation for ALD has been subject to much controversy. The UK Liver Advisory Group recommendations for liver transplantation in patients with ALD11 include:
an assessment by alcohol specialist
signing an agreement indicating intention of abstinence before listing
regular follow-up by alcohol specialist and transplant clinician in the pre- and post-transplant period.
Significant improvement is seen with abstinence.12 Indeed with abstinence, many candidates referred for transplantation will improve to such an extent that transplantation is no longer indicated. There is no requirement for a fixed period of abstinence.
Current contraindications include:
alcoholic hepatitis
more than two episodes of medical non-adherence
return to drinking after full professional assessment
current illicit drug misuse.
The combination of ALD and HCV has a significant impact on the waiting list mortality as well as post- transplant mortality13 and all HCV recipients are advised to abstain from alcohol.
Increasing the donor potitlel
Resources have been invested in increasing public awareness and donor rates are increasing slowly. The traditional donor pool is shrinking, in part because public health measures have been successful in reducing premature death: for example, there are fewer deaths both from road accidents and from intracerebral trauma. Thus it is ever more important to encourage all potential donors to become actual donors.
Every allocation system has its own set of moral and ethical challenges. There is a need to balance the often conflicting demands of:
everyone has an equal opportunity of receiving a graft
utility: allocation is determined by the best outcome
where the survival benefits of transplant and non-transplant are compared
justice, which implies a variety of benefits.
Public opinion
Public opinion is important but does not always reflect medically acceptable values. Surveys of the general public indicate that there is little support for transplantation using scarce organs for those with liver failure from overdose, alcohol or drug misuse.14
Individuals offer a variety of reasons for unwillingness to donate organs, including:
lack of trust in the fairness of organ allocation
uncertainties about the success of transplantation
a belief that willingness to donate may affect their medical care
concern of religious or cultural values.
It is important to retain public confidence in how organs from deceased donors are used. The development of agreed guidelines and protocols will ensure that those transplanted for ALD have a fair and just access to transplant. It is essential to ensure that patients with ALD and substance misuse understand and adhere to their role in the process.
Organ donation rates
Organ donation rates vary between countries for various reasons including cultural, ethical and legal. Donation rates in the UK, although rising, continue to be lower than in Spain which has the highest donation rate. The Spanish model, introduced in 1989, is based on a decentralised network of specifically trained transplant coordinators (most of them physicians working in intensive care units) with organ procurement as the main goal.15
The Spanish model has been broadly adopted in the UK with a significant injection of resources and the introduction of several initiatives. These include the introduction of a national body of nearly 250 donor transplant coordinators (specialist nurses in organ donation), clinical leads in organ donation, donation committees in all acute hospitals and a national organ retrieval service. The main focus of the work is to ensure that all potential donors are identified, brain stem death testing applied where appropriate, and the individuals and the families of all those where donation is possible are given the opportunity to donate.
Consent
The laws governing consent (or authorisation) are clearly defined and regulated by professional bodies and the Human Tissue Authorities. The debate about the benefits of opt-in and opt-out systems continues. The UK has opted, for the present time, to remain with the opt-in process. Other health administrations have adopted different approaches, including giving priority for receipt of organs to those who have agreed to donate. There is now clarity over the diagnosis of death and the appropriateness of interventions to allow donation to proceed and fulfil the wishes of the individual to donate.
The Organ Donor Register (ODR) allows people to indicate their willingness to donate and indicate which organ or tissue they would wish to donate in the event of their death. There are currently over 17 million people registered on the ODR.
Expansion of the donor potitlel
Extended criteria donors (ECDs) are defined as those having characteristics that increase the probability of graft failure or disease transmission compared with the lower risk standard criteria donors. Characteristics of ECD liver grafts include increasing steatosis, donor age and length of intensive therapy unit (ITU) stay. Other factors that may make a graft at higher risk to the recipient include positive hepatitis, HIV serology and a history of malignancy. These factors will be exacerbated by prolonged cold ischaemia times.
Organs from patients with donation after cardiac death (DCD) (also known as non-heart beating donors) offer the potential to increase the donor pool to the conventional donation after brain death (DBD) (also known as brain-stem death donors). There are several classes of DCD patients. Those who are controlled donors (where death occurs after planned withdrawal of treatment) offer a significant increase of the donor pool. Such donors may come not only from the ITU but also from emergency medicine departments.
It is a tribute to surgical skills that outcomes are not deteriorating, even though the overall number of high-risk donors is increasing. In general, outcomes of organs from DCD donors are inferior to those of DBD donors, but this difference is being reduced with increasing experience. There still remain concerns about the longer-term outcomes, particularly with respect to ischaemic biliary strictures.
Surgical approaches to increase the donor potitlel
Living donation
Living donor transplantation can expand the donor pool, especially in those areas such as Asia where deceased donation rates are very low. The risks to the donor remain a concern, with reported mortality of up to one in 250 for adult-to-adult donation (the risks are less for left lobe donation).16
Split liver
Two grafts are generated from one donor liver. The most widely used technique is to split the graft into left lateral sectoral graft (segments 2 and 3) for a child and a right trisegmental graft (segments 1 and 4–8) for an adult. Various splitting techniques have been described. Irrespective of the technique used, outcomes seem to be comparable with deceased donor grafts.
Auxiliary transplants
Auxiliary liver transplantation is a technique in which all or part of the graft is placed in the abdomen and the native liver left in situ. This procedure will not increase the donor pool but is an option for those in whom there is a potential for recovery of the native liver. If the native liver recovers, immunosuppression may be withdrawn.17
Domino liver transplantation
In this technique the explanted liver is grafted to another. Livers from a handful of metabolic disorders (such as porphyria or amyloid), cured by liver transplantation, are used for domino transplantation. The genetic disorder either manifests later in life of the recipient or never manifests.
Xenotransplantation
Although xenotransplantation (animal to human) was performed initially in 1966, this remains, as it has always been, an option for the future. It is currently illegal.
New developmentitles
-
1
Machine-based liver preservation and newer perfusion fluids may allow greater use of marginal livers and improve their chance of good function.
-
2
Liver support devices have been developed which may bridge an ill patient in liver failure to transplant or allow time to spontaneous recovery.
-
3
Hepatocytes and stem cell transplantation are being intensively evaluated and offer some promise.
References
- 1.Leon DA, McCambridge J. Liver cirrhosis mortality rates in Britain from 1950 to 2002: an analysis of routine data. Lancet. 2006;367:52–6. doi: 10.1016/S0140-6736(06)67924-5. [DOI] [PubMed] [Google Scholar]
- 2.Fleming KM, Aithal GP, Solaymani-Dodaran M, Card TR, West J. Incidence and prevalence of cirrhosis in the United Kingdom, 1992–2001: a general population-based study. J Hepatol. 2008;49:732–8. doi: 10.1016/j.jhep.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 3.Dawwas MF, Gimson AE, Lewsey JD, Copley LP, van der Meulen JH. Survival after liver transplantation in the United Kingdom and Ireland compared with the United States. Gut. 2007;56:1606–13. doi: 10.1136/gut.2006.111369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van der Meulen JH, Lewsey JD, Dawwas MF, Copley LP. UK and Ireland Liver Transplant Audit Adult orthotopic liver transplantation in the United Kingdom and Ireland between 1994 and 2005. Transplantation. 2007;84:572–9. doi: 10.1097/01.tp.0000280540.76370.37. [DOI] [PubMed] [Google Scholar]
- 5. www.nhsbt.nhs.uk.
- 6. www.unos.org.
- 7.Hart CL, Morrison DS, Batty GD, Mitchell RJ, Davey Smith G. Effect of body mass index and alcohol consumption on liver disease: analysis of data from two prospective cohort studies. BMJ. 2010;340:c1240. doi: 10.1136/bmj.c1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malinchoc M, Kamath PS, Gordon FD, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864–71. doi: 10.1053/he.2000.5852. [DOI] [PubMed] [Google Scholar]
- 9.Neuberger J, Gimson A, Davies M, et al. Selection of patients for liver transplantation and allocation of donated livers in the UK. Gut. 2008;57:252–7. doi: 10.1136/gut.2007.131730. [DOI] [PubMed] [Google Scholar]
- 10.Lucey MR, Brown KA, Everson GT, et al. Minimal criteria for placement of adults on the liver transplant waiting list: a report of a national conference organized by the American Society of Transplant Physicians and the American Association for the Study of Liver Diseases. Liver Transpl Surg. 1997;3:628–37. doi: 10.1002/lt.500030613. [DOI] [PubMed] [Google Scholar]
- 11.Bathgate A. UK Liver Transplant Units Recommendations for alcohol-related liver disease. Lancet. 2006;367:2045–6. doi: 10.1016/S0140-6736(06)68904-6. [DOI] [PubMed] [Google Scholar]
- 12.Veldt BJ, Lainé F, Guillygomarc'h A, et al. Indication of liver transplantation in severe alcoholic liver cirrhosis: quantitative evaluation and optimal timing. J Hepatol. 2002;36:93–8. doi: 10.1016/S0168-8278(01)00228-8. [DOI] [PubMed] [Google Scholar]
- 13.Lucey MR, Schaubel DE, Guidinger MK, Tome S, Merion RM. Effect of alcoholic liver disease and hepatitis C infection on waiting list and posttransplant mortality and transplant survival benefit. Hepatology. 2009;50:400–6. doi: 10.1002/hep.23007. [DOI] [PubMed] [Google Scholar]
- 14.Neuberger J, Adams D, MacMaster P, Maidment A, Speed M. Assessing priorities for allocation of donor liver grafts: survey of public and clinicians. BMJ. 1998;317:172–5. doi: 10.1136/bmj.317.7152.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matesanz R. Organ procurement in Spain. Lancet. 1992;340:733. doi: 10.1016/0140-6736(92)92274-J. [DOI] [PubMed] [Google Scholar]
- 16.Middleton PF, Duffield M, Lynch SV, et al. Living donor liver transplantation – adult donor outcomes: a systematic review. Liver Transpl. 2006;12:24–30. doi: 10.1002/lt.20663. [DOI] [PubMed] [Google Scholar]
- 17.Azoulay D, Samuel D, Ichai P, et al. Auxiliary partial orthotopic versus standard orthotopic whole liver transplantation for acute liver failure: a reappraisal from a single centre by a case-control study. Ann Surg. 2001;234:723–31. doi: 10.1097/00000658-200112000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]