Abstract
Family-focused therapy (FFT) is an evidence-based intervention for adults and children with bipolar disorder (BD) and their caregivers, usually given in conjunction with pharmacotherapy after an illness episode. The treatment consists of conjoint sessions of psychoeducation regarding bipolar illness, communication enhancement training, and problem-solving skills training. This paper summarizes over 30 years of research on FFT and family processes in BD. Across eight randomized controlled trials with adults and adolescents with BD, FFT and mood-stabilizing medications have been found to hasten recovery from mood episodes, reduce recurrences, and reduce levels of symptom severity compared to briefer forms of psychoeducation and medications over 1–2 years. Several studies indicate that the effects of FFT on symptom improvement are greater among patients with high-expressed emotion relatives. New research focuses on FFT as an early intervention for youth at risk for BD, neuroimaging as a means of evaluating treatment mechanisms, and progress in implementing FFT in community mental health settings.
Keywords: Family-Focused Therapy, Expressed Emotion, Family Interaction, Bipolar Disorder, Psychosis, Functional Magnetic Resonance Imaging
OVERVIEW
Family-focused therapy (FFT) was developed in the mid-1980s as an intervention for patients with bipolar disorder (BD) who had just been in the hospital for an episode of mania or depression and were going home to live with parents, a spouse, or another set of familial caregivers. Over the last 30 years, we have learned a considerable amount about families coping with BD and how to treat the disorder within a familial context. This article reviews the format, key assumptions, clinical techniques, and empirical studies of FFT as an adjunct to pharmacotherapy for patients with BD. We review studies of variables that may moderate or mediate the effects of FFT on symptomatic outcomes, and recent work on implementing FFT in community mental health settings. Finally, we discuss a key direction for psychosocial research in BD: implementing family interventions to prevent the eventual onset of BD in high-risk youth.
HISTORICAL CONTEXT
Family-focused therapy emerged as a modification of behavioral family management (Falloon, Boyd, & McGill, 1984; Miklowitz & Goldstein, 1990), a 9-month treatment for schizophrenia patients and their families. Behavioral family management consists of sessions of psychoeducation, communication skills training, and problem-solving skills training for patients with schizophrenia and their parent(s) or, in rare cases, their spouse or adult siblings. Falloon et al. (1985) found that for schizophrenia patients who had just been discharged from hospital, the combination of 9 months of behavioral family management and neuroleptic medication was more effective in reducing rates of psychotic relapse and improving social functioning than 9 months of supportive individual therapy and neuroleptic medication. The extension of family psychoeducation to other recurrent, impairing psychiatric disorders—including BD—seemed promising.
The mid-1980s was an exciting time to be pursuing studies of families with major mental illnesses. The biological and genetic findings of the 1960s and 1970s led to a decisive shift in the overall framework for working with families. Patients with schizophrenia or BD were no longer viewed as victims of pathological family environments but rather, individuals with genetically based disorders who often lived in families that were distressed because of their lack of access to information on effective treatments. The double-bind hypothesis and the schizophrenogenic mother were no longer dominant paradigms; in fact, consumer groups like the National Alliance for the Mentally Ill were quite vocal about rejecting the blame of parents (and usually, mothers) inherent in these theories (Imber-Mintz, Liberman, Miklowitz, & Mintz, 1987). The countervailing hypothesis was that parents who expressed high levels of negative emotionality or unclear communication were reacting to the stresses and strains of living with a person with schizophrenia (Miklowitz, 1994).
Unfortunately, our current efforts to avoid blaming parents have led to a different problem: an exclusive focus on patients without consideration of their familial context. The position in the “Decade of the Brain” was that referring to psychiatric disorders as brain diseases would reduce stigma and place them among the larger spectrum of medical disorders. However, as articulated by Hinshaw and Cicchetti (2000) and others, the “brain disorders” movement has had the effect of further stigmatizing patients with mental illnesses. Patients complained bitterly about being told they had a brain disorder, along with the implication that they were crazy, could not be trusted, or were defective or developmentally disabled. To this day, those interested in family therapy struggle with finding a midpoint between avoiding blame or stigmatizing parents and patients and being able to help them restructure relationships, reduce conflict, and enhance communication in the aftermath of an illness episode.
Studies of Expressed Emotion
The literature on expressed emotion (EE) provided a road map for investigators who were interested in either treatment or basic familial processes in patients with severe psychiatric disorders. EE studies usually proceed as follows: An investigator interviews the parents or spouse of a concurrently ill patient using the 1- to 2-hour Camberwell Family Interview (Vaughn & Leff, 1976) that focuses on the 3 months leading up to the patient’s most recent period of illness. Later, a trained coder listens to tapes of these interviews and rates the number of critical comments voiced about the patient (e.g., “I don’t like it that he just sits and stares all day” with accompanying negative voice tone), level of expressed hostility (personalized or generalized criticism or rejection of the patient; e.g., “I hate him. … he’s a loser, he’s worthless”), and the level of emotional overinvolvement (i.e., statements indicating that the parent is unusually self-sacrificing, overconcerned, overprotective, or has exaggerated emotional responses to or unclear boundaries with the patient; e.g., “I have discontinued most of my friendships so that I can be there in case he ever needs me”). Parents—and by extension, families—are rated as high in EE if they express six or more critical comments, show evidence of hostility, or are rated high in emotional overinvolvement. If no parent has these attributes, the family is classified as low in EE. Across numerous studies of schizophrenia, major depression, BD, and other conditions, patients whose parental or spousal caregivers are high-EE are 2–3 times more likely to have an illness recurrence in the 9 months–1 year after an EE assessment than those whose caregivers are low-EE (for reviews, see Hooley, 2007; Peris & Miklowitz, 2015).
The dichotomous nature of the EE construct has been one of its limitations from the start, and has possibly affected its clinical utility. Knowing that a family is high- or low-EE does not in itself suggest an intervention. Nonetheless, EE research has spawned a series of process-oriented studies that have attempted to clarify the behavioral and interactional correlates of high- and low-EE attitudes among caregivers. For example, studies in the United Kingdom and United States found that patients with schizophrenia in high-EE families could be distinguished from those in low-EE families on their increased levels of physiological arousal (e.g., galvanic skin response) (Altorfer, Kasermann, & Hirsbrunner, 1998; Sturgeon, Turpin, Kuipers, Berkowitz, & Leff, 1984; Tarrier, Barrowclough, Porceddu, & Watts, 1988), especially when interacting with their relatives. High-EE parents of patients with schizophrenia are more likely than low-EE parents to criticize the patient during face-to-face interactions; those with high emotional overinvolvement make more “mind-reading” statements (Miklowitz, Goldstein, Falloon, & Doane, 1984; Strachan, Leff, Goldstein, Doane, & Burtt, 1986). High-EE parents also communicate with less clarity and higher levels of communication deviance when interacting with offspring with schizophrenia than low-EE parents (Miklowitz et al., 1986).
When we observed families in a laboratory-based problem-solving discussion in the 1–2 months after hospital discharge, patients with schizophrenia were more likely to express unusual thoughts or self-critical statements when interacting with high-EE parents than patients interacting with low-EE parents (Strachan, Feingold, Goldstein, Miklowitz, & Nuechterlein, 1989). In contrast, patients with BD were more likely to disagree with their parents, often becoming verbally confrontational and refusing to go along with the parents’ opinions or plans (Miklowitz, Goldstein, & Nuechterlein, 1995). Neither interaction pattern seemed productive to us in terms of the end goal of solving family problems. This process-oriented research led to the first behavioral target for family therapy in BD: altering the level of emotional negativity in bidirectional parent/offspring or couple interactions.
A different approach to EE was taken by Jill Hooley and colleagues (e.g., Hooley & Gotlib, 2000), who recognized that caregivers who held high-EE attitudes were more likely to attribute the causes of negative behavior in patients to internal, stable, and controllable factors (e.g., sullenness, laziness) than to uncontrollable factors (i.e., the presence of an illness). Attributions of controllability or intentionality (i.e., “he’s doing this on purpose”) understandably cause anger in caregivers, which may be expressed as critical comments or hostility toward the patient. A significant number of studies of depression and schizophrenia support Hooley’s attribution model (for review, see Hooley, 2007). For example, our group at the University of Colorado, Boulder, found that, when interacting with their bipolar family member, high-EE parents and spouses were more likely to attribute negative moods (e.g., irritability, depression) and associated behaviors of the patient to controllable factors (e.g., “if you would just slow down and focus, you might get something done”; Wendel, Miklowitz, Richards, & George, 2000). This research led to a second target for family intervention: increasing the degree to which caregivers attributed negative patient-related events or behaviors to an illness, as opposed to controllable causes. This is one of the reasons for beginning treatment with psychoeducation after an illness episode — to acquaint parents and other caregivers with the biological and genetic explanations for why the patient is underperforming or being aggressive or noncooperative during the postepisode period.
Observations of Families of Patients with BD
When we first began our studies of families with young adult bipolar patients (1983–88), it became clear to us from interviewing parents and spouses—whether high-EE or not — that most were seeking coping strategies for managing their relative’s BD. After observing one or more manic episodes, many parents/spouses became highly anxious that the illness could recur at any minute; that even minor changes in their offspring’s mood portended more serious illness episodes; and that patients should be held to their medication regimens at all costs. Some gave up their jobs or their focus on other children to advocate for the bipolar family member. In the eyes of mental health professionals, these caregivers resembled the emotionally overinvolved parents of schizophrenia patients described by Brown and colleagues (Brown, Birley, & Wing, 1972). Patients with BD, many clinicians believed, simply had an inborn metabolic error that was corrected by lithium, and with medications most if not all could lead happy and productive lives.
We felt that these explanations neglected the challenges that caregivers faced at a time when few mental health resources (other than medications) were available to patients. After a manic episode, most young adult patients were not ready to manage the disorder on their own; some abused substances or drank heavily, often driven by residual mood symptoms; a large proportion stopped taking medicines and relapsed. Despite their protestations about needing independence, many became highly dependent on their parents or spouses to provide the stability that their internal world did not provide.
These family processes became clearer to us when we observed the high rate of relapse of young adult patients with BD in high-EE homes (Miklowitz, Goldstein, Nuechterlein, Snyder, & Mintz, 1988). Patients who had parents with high-EE attitudes (expressed to an interviewer) or parents who were negative, critical, or guilt-inducing in direct interactions with the patient, had a 94% chance of having an illness recurrence in the 9 months after a hospitalization. The rate of relapse in patients whose parents were “benign” in both attitudes and interactional behavior was only 17%. Interestingly, EE attitudes and negative interactional behaviors were uncorrelated in the families of bipolar patients, possibly due to the verbal, assertive, and confrontational role taken by patients in these interactions. Some caregivers became docile with the patient and less negative; others who had expressed benign EE attitudes when with a clinician became angry, critical, and accusatory when with the patient (Miklowitz et al., 1995).
FAMILY-FOCUSED TREATMENT: DESCRIPTION AND EMPIRICAL STUDIES
In the late 1980s, we began piloting FFT with adults with BD. To examine whether we could engage families in treatment, we set out to extend Falloon et al.’s (1985) model, with 21 sessions over 9 months of psychoeducation (weekly sessions for 3 months), communication enhancement training (CET; weekly and then biweekly sessions for 3 months, up to months 5 or 6), and problem-solving skills training (biweekly and then monthly sessions, up to month 9). The majority of our pilot work was conducted in families’ homes, as Falloon et al. (1985) had done. Patients were recruited while they were in the hospital, usually (but not invariably) during a manic episode. Most would be considered bipolar I by today’s standards. In developing the treatment, we narrowed our goals to six objectives, as listed in Table 1.
TABLE 1.
Six Objectives of Family-Focused Therapy for Young Adults with Bipolar I Disorder
Assist the patient and caregivers in:
|
Psychoeducation Module
The first treatment module, psychoeducation, consists of didactically oriented sessions with patients, their parental or spousal caregivers, and any available siblings or extended relatives. Clinicians describe the patient as “expert” in explaining episodes of mania and depression: “we will be counting on you to share your experiences and educate us as well as your family about what you’ve gone through.” Symptom handouts help organize the patient’s recollections. Then, family members are encouraged to chime in with their own recollections of the patient’s most recent episode (e.g., “I don’t remember you being elated, but I sure do remember you being irritable”). The clinician encourages the family to agree on a timeline for the most recent episode: when the first symptoms began (either by the patient’s self-report or the caregivers’ observations), how and when they worsened over time, whether any stressors were associated with the most recent episode (even if not obviously causally related), and at what point the family members—or in rarer cases the patients themselves—called for help. In cases where the most recent mood episode was depressed and the patient expressed suicidal ideation or attempted suicide, the triggers for these ideas or actions are clarified. Suicidal thoughts or even attempts are “normalized” for the patient and family by pointing out their episodic nature, their biological correlates, and their co-occurrence with other symptoms of BD (e.g., insomnia or a decreased need to sleep).
As psychoeducation progresses, the family is acquainted with the role of stress (including persistent family conflicts) in eliciting symptoms. The notions of genetic or biological vulnerability are explained. Clinicians make it clear that, while we do not know the full nature of the biological predispositions associated with BD, we do know that the disorder runs in families; “moodiness” is often a precursor in childhood; the disorder is associated with (although not necessarily caused by) disturbances in neural transmission and abnormal functioning of brain circuitry; and medications are recommended to help stabilize these vulnerabilities (e.g., Manji, 2009). The influential role of stress is given equal weight through identifying contributory stressors from prior episodes (e.g., extended work hours, changing work shifts, conflicts in families, or romantic relationships). The clinician acknowledges that although the patient will be unable to avoid most forms of stress, learning to understand what experiences are stressful and to work around them (resilience) — with the help and support of family members—may do much to stave off the most severe episodes. For example, a patient recognized that at least one prior manic episode was associated with changes in her sleep/wake cycles as she transitioned from the end of summer to the beginning of a demanding semester of college. Learning to stabilize her sleep patterns in the weeks before the semester began helped minimize these disruptive effects.
Toward the end of psychoeducation, the family and patient develop a relapse prevention plan. This plan consists of three components: a list of likely prodromal symptoms of depressive or manic episodes, the stressors that have been associated with these symptoms in the past, and a list of preventative interventions to reduce the likelihood of full episodes in the future. These interventions may vary from medical (e.g., increasing one’s dose of antipsychotic medications when new manic symptoms appear) to psychosocial (e.g., keeping familial expectations of the patient to a minimum after an episode; avoiding chronic conflict areas) to practical (e.g., keeping track of one’s mood states from one day to the next).
CET and Problem-Solving Modules
Communication enhancement training may be introduced early in treatment, but typically is begun by sessions 6–7 of the 21-session protocol, by which time the patient has achieved more stability (as noted below, recent iterations of FFT for children at risk for BD are only 12 sessions, with CET beginning at session 4). The goals of CET are to improve family relationships through interrupting negative patterns of interaction, increasing active listening and statements of empathy, rebalancing the expression of praise versus criticism, and having a clear agenda when one is speaking. This part of FFT is similar to behavioral or cognitive-behavioral models of family or marital therapy (e.g., Baucom & Epstein, 1990; Falloon et al., 1984; Jacobson & Margolin, 1979). It also is influenced by strategic models of family therapy that encourage families to do “less of the same” and more of something different (Rohrbaugh & Shoham, 2001). The goal in FFT is not to get family members to talk in an artificial or overly scripted way, but to increase levels of collaboration and validation toward one another so that conflicts are more likely to be resolved. Later, when conflicts intensify, family members and patients are expected to draw on the reservoir of skills learned during less stressful exchanges.
The skills include expressing positive feelings, active listening, making positive requests for change in another’s behavior, communication clarity, and expressing negative feelings about specific behaviors. For each skill, a participant is named the speaker and another the listener. So, for example, a father may be instructed to listen actively as his son explains what a depressive episode feels like, paraphrase his son’s main points, and ask appropriate questions to clarify content. He is coached to avoid advice-giving or going beyond the content of what his son has said. In positive requests for changes, the speaker is asked to describe a behavior that he or she would like someone else to perform and clarify how it would make the speaker feel (e.g., “I’d really like for you to talk to me in a more respectful tone of voice. I’d feel more hopeful about us working together”).
The problem-solving module, typically conducted in the last 3–4 sessions, involves identifying specific family conflicts (e.g., eating habits, use of phones or computers, spending money, finding childcare, getting to appointments, doing household chores), “brainstorming” or generating solutions as a group, evaluating the advantages and disadvantages of each solution, choosing one or more solutions, and developing an implementation plan.
Of course, not every problem fits into this structure. For example, the clinician may learn well into the treatment that the patient has stopped taking medications or does not agree with the bipolar diagnosis. These problems are addressed in a nonthreatening way, with input from all family members. If the patient is an adult, the clinician makes clear that the patient has decision-making authority over whether to take medications or not. The therapist encourages the patient to clarify his viewpoint and the alternative explanation he has for the illness episode (e.g., “it never happened … it was all just sort of a story my parents made up”). The clinician offers her own beliefs about the likely course of the disorder without the protection afforded by medications, and reminds the family of the relapse prevention drill (e.g., “Let’s go back to what we decided you would each do if Brian were to become manic again. Brian, are you OK with us going in this direction? I think it would make your parents feel more comfortable with your decision”).
With younger patients, the decision to stop taking medications can often be traced to disagreements between the biological parents about whether the medications are necessary or effective. These disagreements need to be aired. Sometimes a separate session for the parents is necessary before they can present a united front for the child about expectations for medication use.
EMPIRICAL STUDIES OF FFT
Table S1 summarizes the results of the trials conducted with FFT. Rather than examine each study individually, we highlight some issues that have emerged in randomized controlled trials (RCTs) or open (nonrandomized) trials that have established the validity of FFT as adjunctive to pharmacotherapy. Figure 1 summarizes data aggregated from eight prior RCTs of FFT plus pharmacotherapy (n = 342) versus comparison treatments plus pharmacotherapy (n = 612) conducted in our labs at UCLA, University of Colorado, and collaborative sites. These trials included bipolar adults (three trials; N = 447), bipolar adolescents (two trials; N = 203), symptomatic youth at high risk for BD (two trials, n = 175), and adolescents/young adults at risk for psychosis (one trial, n = 129). The comparator conditions have typically been brief psychoeducation (e.g., 2–3 sessions for the individual or family) or equally intensive forms of individual therapy (e.g., CBT), with crisis management as needed (Table S1). Of 2,482 individuals screened for these trials, 954 (38.4%) were eligible and willing to be randomly assigned to treatments. The overall attrition rate in FFT (withdrawal prior to the end of treatment) was 16.4%; the rate was 24.5% in the various comparison conditions.
FIGURE 1. CONSORT Summary Diagram of Eight Randomized Trials of FFT for Adults and Children with Bipolar Disorder.
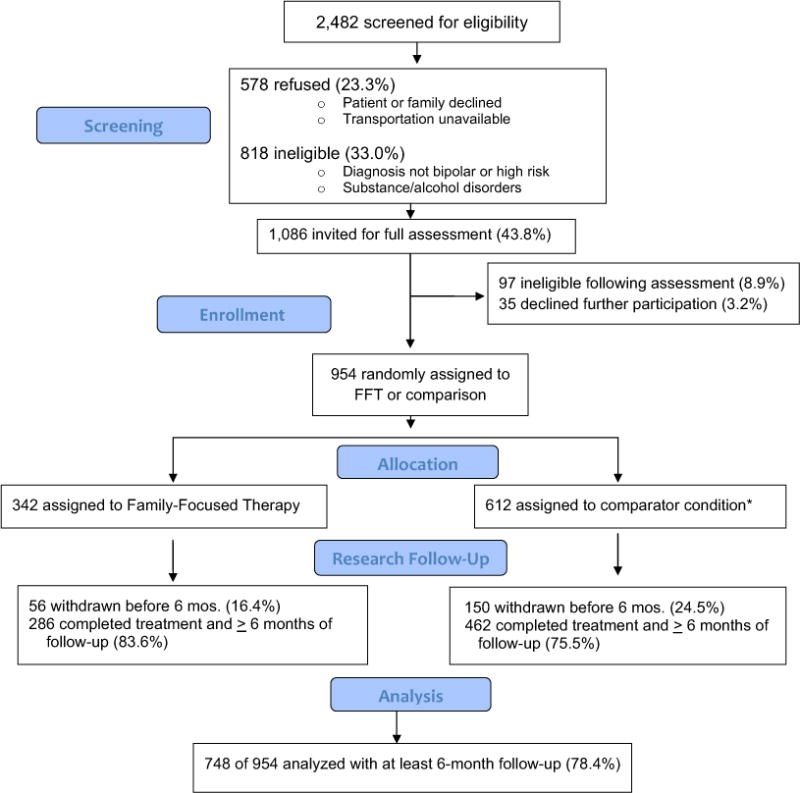
*Note. Includes STEP Bipolar Program that compared four psychotherapies (of which FFT was one) within different randomization strata.
As indicated in Table S1, patients who received FFT and pharmacotherapy had lower rates of relapse, more rapid episode recovery, and less severe symptoms over 1–2 years than patients who received brief psychoeducation or individual psychoeducation of equal duration (e.g., Rea et al., 2003) and pharmacotherapy. There were differences across trials in when treatment effects were observed and for what outcome variables (Table S1). Pharmacotherapy regimens did not explain treatment group differences in symptoms at baseline or at follow-up.
In most of the trials, FFT sessions lasted 9 months; in more recent trials with high-risk youth or young adults, treatment lasted 4–6 months. One of these trials concerned children and adolescents at high risk for BD (12 sessions over 4 months; Miklowitz et al., 2013) and one concerned adolescents and young adults at high risk for psychosis (18 sessions over 6 months; Miklowitz, O’Brien, et al., 2014). Youths at high risk for BD (mean age = 13 years) were defined as those with (a) a diagnosis of major depression, BD not elsewhere classified (i.e., subthreshold BD), or cyclothymic disorder, and (b) at least one first-degree relative with bipolar I or II disorder. Adolescents and young adults at risk for psychosis were those with attenuated positive symptoms, intermittent periods of psychosis, schizotypal personality disorder, and/or a family history of schizophrenia. In both studies, the short-term effects of FFT on subthreshold symptoms (depression, hypomania, or attenuated positive symptoms) were observed over 6 months–1 year, and were robust once the effects of concurrent medications were covaried. These studies raise the intriguing possibility that family intervention, if administered early in the high-risk period, may prevent, delay, or mitigate the onset or severity of major psychiatric disorders in children and adolescents.
There has been one nonreplication—a randomized trial of FFT and pharmacotherapy versus brief psychoeducation and pharmacotherapy for adolescents with bipolar I or II disorder (Miklowitz, Schneck, et al., 2014). In this study, conducted across three sites and involving 145 patients, no group differences were observed in time to recovery or time to recurrence over 2 years. There were secondary group differences in year 2 for manic/hypomanic symptoms, which improved more in the FFT than in brief psychoeducation. This result is similar to the result observed by Rea et al. (2003) in a comparison of FFT and equally intensive individual therapy for young adults with bipolar I disorder. In that study, no differences between groups were observed in year 1 (the interval during which the psychosocial treatments were being administered) but differences in time to relapse and rehospitalization emerged in the 1–2 years after FFT concluded. Theoretically, families may need time to “absorb” the FFT skills and implement them in day-to-day functioning. Once these skills are put into use, there is a greater chance for the familial context to be protective against a worsening of the disorder.
Studies of FFT Outside the United States
Led by Aysegul Ozerdem, M.D., a group in Izmir, Turkey, conducted the first open trial of FFT outside the United States. The 21-session protocol required few adaptations of format or content for Turkish patients or families. The 10 study patients showed improvements in global functioning and Clinical Global Impression scale ratings over 1 year (Ozerdem, Oguz, Miklowitz, & Cimilli, 2009). In a nonrandomized trial involving 137 patients with BD in Italy, Fiorillo et al. (2015) found that patients who were consecutively assigned to 4–6 months of family-focused psychoeducation had significant improvements in social functioning, and caregivers showed decreases in burden compared to a usual care group.
In a randomized trial in Egypt that was similar in design to Rea et al.’s (2003) study of FFT, Nagy et al. (2015) examined the effectiveness of “behavioral family psychoeducation” versus individual supportive therapy in 111 patients with BD. Patients had just been discharged from inpatient care. Like FFT, behavioral family psychoeducation consisted of 21 sessions of psychoeducation, communication training, and problem-solving skills training. All received mood-stabilizing medications as well. In the study year, patients in family psychoeducation had fewer relapses (25.4%) and rehospitalizations (1.5%) than patients in supportive psychotherapy (34.4% and 50%). Thus, there is reason to believe that the effects of FFT (or similarly constructed interventions) extend to non-U.S. populations.
Effectiveness Research
Few studies have undertaken comparisons of psychosocial treatments for BD in community settings. The Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) was a comparative effectiveness study of recovery in bipolar, depressed patients (Table S1). FFT and other treatments were compared to each other across multiple sites, with patients recruited from community or university-affiliated clinics and followed up for psychosocial and pharmacological treatments by personnel affiliated with those clinics. A total of 293 patients in a depressed phase of bipolar I or II disorder were drawn from 10 sites and randomly assigned to (1) one of three intensive psychosocial treatments (up to 30 sessions of FFT, interpersonal and social rhythm therapy [IPSRT], or cognitive-behavioral therapy [CBT] over 9 months); or (2) a 3-session individual educational treatment called collaborative care (CC). All patients received pharmacotherapy as operationalized by the study protocol.
Over 1 year, being in FFT, CBT, or IPSRT was associated with more frequent and more rapid recovery from bipolar depression than being in CC, but there were no statistical differences among the intensive therapies (Table S1) (Miklowitz, Otto, Frank, Reilly-Harrington, Wisniewski, et al., 2007). Patients in intensive treatment were 1.6 times more likely than patients in CC to be clinically well in any given study month. The greater benefits of intensive psychosocial intervention were evident for functional outcomes and life satisfaction as well (Miklowitz, Otto, Frank, Reilly-Harrington, Kogan, et al., 2007). Interestingly, in an overlapping randomized trial, STEP-BD investigators found no benefit of adding antidepressants to mood stabilizers in stabilizing patients with bipolar depression (Sachs et al., 2007). The STEP-BD study suggests that psychotherapy—including FFT, CBT, and IPSRT—is a vital part of the effort to stabilize episodes of depression in bipolar illness. Patients with acute depression may require more intensive family or individual therapy than is typically offered in community mental health centers.
Process Research
Process research in FFT has concerned three issues: (a) How is therapist fidelity measured, and what are its key elements? (b) What variables in the patient, family, or setting moderate the effects of FFT on the course of BD? (c) What person or family variables change as a result of FFT, and are changes in these variables associated with changes in patients’ outcomes (mediation)?
Treatment fidelity
The key measure of FFT fidelity is the Therapist Competence and Adherence Scale (TCAS) (Weisman et al., 1998). This 11-item scale measures therapist behaviors on 1 (non-adherent) to 7 (extremely adherent and competent) scales, including model-specific strategies (e.g., quality of psychoeducation or communication training) and nonspecific variables such as appropriate pacing, maintaining rapport with families, or taking command of sessions. Whenever possible, the TCAS is rated from audio- or videotapes from the beginning, middle, and end of each treatment.
We have conducted archival analyses of TCAS tape ratings from seven randomized trials to determine whether there are underlying factors (“fidelity components”) that distinguish FFT from other treatments and explain its association with improvements at the individual patient level. We examined 947 TCAS ratings of tapes obtained from 257 patients/families. Interrater reliabilities were as follows: overall fidelity (1–7 scale), .71; quality of psychoeducation, .73; quality of communication training, .70; quality of problem-solving, .69; homework assignments, .68; pacing, .68; session command, .82; family difficulty, problem specification, .57; and rapport/alliance, .52. The items with lower reliability also tended to have less variability. Using a cutoff of 5 (good adherence) or above on the overall adherence rating, 84.1% (796 of 947) of the sessions were rated above fidelity thresholds.
Discriminant validity of fidelity ratings
In the eight-site study of adolescents and young adults at high risk for psychosis (N = 129), we examined how TCAS raters (who were also the clinical supervisors) distinguished between fidelity to the FFT manual versus enhanced care (EC), consisting of three family psychoeducation sessions following the FFT protocol (Marvin, Miklowitz, O’Brien, & Cannon, 2014). Clinicians (n = 24) were equally skillful in administering psychoeducation in FFT and EC sessions, with no observed differences in quality of rapport with families, pacing of sessions, or session command. Not surprisingly, clinicians administering FFT were more likely to provide effective communication skills training, χ2(3, N = 172) = 17.36, p = .001, and problem-solving skills training, χ2(3, N = 172) = 7.27, p = .03, than those administering EC. Treatment fidelity was not related to the baseline severity of patients’ symptoms or the level of family conflict. The findings suggest that (a) FFT can be administered reliably by clinicians across sites and populations, (b) FFT can be distinguished from brief psychoeducation on the use of communication and problem-solving skills training; and (c) higher adherence/competence ratings do not simply reflect patients who are less severely ill or families that are more cooperative.
Factor Structure of TCAS
Four factors were identified in the 11-item TCAS scale (Table S2). The factor structure closely paralleled the modular structure of treatment, but it is worth noting the elements of each treatment component. The first factor, effective communication training, rests on the clinician’s ability to structure role-plays and direct family members to use active listening or positive requests for change when arguments become heated. The second factor, directive therapeutic style, includes keeping the session moving and discussions from drifting, and focusing the agenda so that the major didactic goals of treatment are met. The third component, psychoeducational stance, refers to the therapist’s ability to deliver accurate didactic information while maintaining a therapeutic alliance and clarifying/validating family members’ divergent opinions. The clinician engages in a Socratic give and take with patients and family members concerning their individual experiences, and addresses each person’s emotional reactions to the diagnosis or its treatments. Finally, an effective problem-solving orientation means that the clinician helps specify and define problems from multiple viewpoints. He or she also highlights the viability of different solutions based on the age of the patient, family structure, or limitations imposed by the illness.
Scores on these four factors are hypothesized to be fidelity components—markers of therapist skill that may activate mechanisms of change in the patient and family. In future studies, we will examine whether effective delivery of these components of FFT are associated with improvements in individual patients’ outcomes or family functioning in BD.
EE: Mediator or Moderator?
A key hypothesis of family intervention studies in the 1970s and 1980s was that high-EE families could be transformed via psychoeducation into low-EE families, and that patients would be less likely to relapse as a result. This hypothesis assumed that high levels of criticism or overprotectiveness among caregivers were due to a lack of understanding of the patient’s disorder and its biological/genetic underpinnings. Some hypothesized that low-EE parents could positively influence the attitudes of high-EE parents when participating together in multi-family psychoeducation groups. In a small (N = 24) randomized trial, Leff et al. (1990) showed that a protocol involving a psychoeducational workshop, caregiver groups, and relative/patient family sessions was associated with a relapse rate of 9% over 2 years, whereas routine care was associated with a rate of 50%. Furthermore, 73% of the high-EE families of patients with schizophrenia were low-EE when assessed after the protocol. No patient relapsed in families in which caregivers received psychoeducational treatment and changed from high-EE to low-EE.
Different results were observed in our first RCT examining bipolar adults and their caregivers (N = 101), in which levels of EE were measured at a pretreatment baseline and again at 9 months. Levels of EE (high vs. low) were stable over time in 70% of families and unstable in 30% (Miklowitz, George, Richards, Simoneau, & Suddath, 2003). Changing from low-EE to high-EE was as common (12%) as changing from high-EE to low-EE (17%), and these patterns were unrelated to whether the patient/family received FFT or brief family psychoeducation. They were also unrelated to patients’ symptomatic outcomes (Simoneau, Miklowitz, Richards, Saleem, & George, 1999). Thus, changes in EE did not appear to mediate the effects of FFT in bipolar illness.
In our work, the real value of EE appears to be its moderation of responses to psychosocial treatments. In the 2003 trial described above, the largest reductions in depression symptoms over 1 year occurred among patients with BD whose families were highly critical at baseline and who received pharmacotherapy and FFT, compared to those whose families were low in criticism (Kim & Miklowitz, 2004). The emotional overinvolvement component of relatives’ EE also moderated the responses of patients to FFT. When relatives showed low levels of inappropriate self-sacrifice (i.e., giving up valued personal goals to take care of the patient), both FFT and brief psychoeducation were associated with improvements in patients’ manic symptoms over 2 years. When relatives showed high levels of inappropriate self-sacrifice, patients in brief psychoeducation became more manic over time, whereas patients in FFT became less manic (Fredman, Baucom, Boeding, & Miklowitz, 2015).
In our first adolescent BD trial, patients from high-EE families who received FFT showed greater reductions in depression scores over 2 years than patients from high-EE families who received brief psychoeducation (Miklowitz et al., 2008; Miklowitz et al., 2009). Similarly, children and adolescents at high risk for BD (mean age = 13 years) who had high-EE parents recovered from depression more rapidly in FFT than high-risk youths with high-EE parents who received a one- to two-session educational control treatment (Miklowitz et al., 2013). Possibly, high-EE families display more of the behaviors that are the targets of FFT: attributing patients’ negative behaviors to controllable, internal, or personal factors; getting into frequent arguments that escalate and become hostile and critical; and difficulty solving problems because of uncontrolled affective expression. Assessment of EE prior to treatment may help identify patients and families who are most likely to benefit from FFT.
An interesting footnote to the EE/moderation question comes from a small study of neuroimaging in youth at high risk for BD. These 12 youth completed 1-hour fMRI scans before and after 4 months of FFT or before/after 4 months of the educational control treatment. At baseline, the degree of amygdala hyperactivity shown by the child during an emotion processing (face-rating) task was associated with a better response over 4 months to psychosocial treatments in general, and FFT in particular (Garrett et al., 2015). Because the amygdala is central to circuits that involve emotion processing and regulation, we would expect it to be highly active when a child is interacting with high-EE parents. We would also expect level of amygdala activation to decrease as patients improve or families became less conflictual. Indeed, levels of amygdala activity decreased from pre- to posttreatment in both treatment groups. In contrast, levels of dorsolateral prefrontal cortical (DLPFC) activity, thought to be associated with response inhibition, planning, and emotional control, increased over time. The degree of increase in DLPFC activity was associated with improvement in hypomania and mania symptoms over this same 4-month pre/posttreatment interval.
In this small study, we were unable to derive causal pathways between amygdala activity, family EE, and clinical improvements associated with FFT. The study does, however, point to a methodology that has been under-used in family interaction and treatment studies—examination of neural activation during emotion processing or problem-solving tasks as proxies for the behavior of patients when negotiating with highly critical parents. Identifying the neural correlates of response to family interventions will almost certainly contribute to our knowledge of how these treatments work, for whom they will be most effective, and whether more powerful and cost-effective treatments can be developed to achieve these aims. These are central goals of “personalized medicine” approaches to psychiatric care.
Family Interactions: Targets for Change?
Changes in family interactional behavior (i.e., the frequency of positively or negatively valenced communication) are often more salient targets for the family clinician than parental EE. Dyadic pairings of high-EE parents and offspring who have BD are often characterized by repetitive, reciprocally negative exchanges, and self-reinforcing behavioral chains in family discussions. In fact, high-EE relative/bipolar patient dyads are statistically distinguishable from low-EE relative/patient dyads by behavioral chains that last for at least three “volleys” of negative behavior (e.g., criticism from a parent followed by counter-criticism from the offspring and more criticism from the parent; Simoneau, Miklowitz, & Saleem, 1998). Negative parent/offspring interactional behavior is associated with relapsing outcomes and psychosocial impairment in young adults with BD and schizophrenia (Miklowitz et al., 1988; Rosenfarb et al., 2001).
Adult patients with BD and adolescents or young adults at risk for psychosis both showed greater improvements in family communication during interaction tasks conducted before and after FFT than adolescents/young adults in a brief psychoeducational treatment (O’Brien, Miklowitz, & Cannon, 2014; Simoneau et al., 1999). In the Simoneau et al. (1999) study of bipolar adults, most of whom were paired with parents or a spouse, improvements in positive interactional behavior partially mediated the association between treatment condition (FFT vs. brief psychoeducation) and reductions in mood symptoms over 1 year. Thus, FFT may have enhanced symptom outcomes by helping families and patients develop resilience (i.e., more productive and collaborative communication) in dealing with the stress of mood or psychosis symptoms.
In the study of youth and young adults at risk for psychosis (O’Brien et al., 2014), families in FFT demonstrated greater improvement from baseline to 6 months in positive communication (e.g., praise, constructive feedback), and greater decreases in conflict behaviors (e.g., criticisms, irritability, off-task comments) during family interactions than families in brief psychoeducation. Both treatments were associated with reductions in adolescents’ perceptions of amount of criticism from mothers, which in turn were associated with lower symptom severity ratings over 12 months (O’Brien, Miklowitz, & Cannon, 2015). In adolescents with BD, high-conflict families (by parent-report) who received FFT reported greater reductions in conflict over time than high-conflict families who received brief psychoeducation. Moreover, treatment-related decreases in parent-reported conflict predicted decreases in adolescents’ manic symptoms over 2 years (Sullivan, Judd, Axelson, & Miklowitz, 2012). Thus, FFT has a record of improving positive and decreasing negative family communication, although the degree to which these changes in communication precede or succeed changes in symptom functioning has not been determined.
Dissemination and Implementation of FFT in Community Mental Health Clinics
A significant barrier to the uptake of evidence-based practices—including FFT—is the skepticism of community providers about the relevance of these practices for lower income, under-resourced populations. In one community study, we conducted focus groups with administrators and providers within publicly funded Community Mental Health Clinics (CMHCs) in Los Angeles before and after day-long trainings in FFT. The focus groups ascertained providers’ perceived barriers to implementation of evidence-based practices (Chung, Mikesell, & Miklowitz, 2014). Unique in California during the time period of this study, FFT was one of the evidence-based practices funded by the California Mental Health Services Act for implementation by County of Los Angeles Department of Mental Health funded CMHCs. Training in cognitive-behavioral therapy, mindfulness, dialectical behavioral therapy, and parent–child interaction therapy was also being conducted concurrently, making mastery of any one practice challenging. Prior to FFT training, the focus group participants perceived evidence-based practices to be rigid and inflexible, as well as less relevant for patients with medication nonadherence, with comorbid disorders (e.g., alcohol or substance abuse), or other features technically outside the scope of evidence-based practice. Similarly, they perceived evidence-based practices as limiting their ability to incorporate their clinical experience in therapy, particularly when developing a therapeutic alliance with patients and families.
After attending the day-long training, providers noted two seemingly contradictory sentiments regarding FFT’s structured approach. First, they appreciated the supervisory feedback offered to clinicians implementing the treatment, as well as example videos of an expert conducting FFT sessions. In the words of one clinician, treating patients with BD can be “chaotic and derailing, so this helps at least give you a roadmap.” The participants expressed appreciation for FFT’s nonlinearity and flexibility. Specifically, clinicians appreciated bring able to implement psychoeducation, communication training, and problem-solving skills training in a different sequence, based on their own assessment. For example, a couple that is knowledgeable about mood disorders but presents with relationship problems may benefit most from starting with (and mastering) the CET. The providers did express concerns, however, that the time and effort required to learn FFT and to implement the full protocol (i.e., minimum 12 sessions) may be incompatible with productivity requirements for “billable” services of many CMHCs, and the barriers (e.g., family transportation costs, parent’s rigid work schedules) to participation for low-income families.
In the implementation study of Fiorillo et al. (2015, 2016), 11 Italian mental health centers were recruited, with two clinicians (total N = 22) from each center offered training in psychoeducational family therapy [as per the FFT and Falloon et al. (1985) manuals]. Of the 22, 16 agreed to participate in a fairly intensive training course (3 monthly sessions of 2.5 days each, followed by 1 week of assessment training and five supervision sessions of 1.5 days each). When implementing the intervention in an experimental sample of 60 patients, the clinicians cited organizational difficulties as the largest hurdle (e.g., integrating the intervention with other workload demands, providing the intervention beyond usual working hours). Clinicians also reported a “low level of collaboration” from their colleagues in identifying suitable families for the study.
The clinicians in the Italian study reported some difficulties with learning family-focused interventions, mainly in conducting communication training role-plays or assigning homework, but these difficulties diminished over time. Clinicians rated the intervention as high in benefits for patients, families, and clinicians; these scores increased with time.
In summary, across international settings, clinicians have had a positive response to FFT. Organizational requirements regarding time management for clinicians and travel costs for families appear to be the most significant barriers to implementation. However, clinicians and administrators appreciate that FFT has both the flexibility to address barriers to implementation in CMHCs while having sufficient structure to address the chaos associated with episodes of bipolar illness (Chung et al., 2014). We are currently evaluating whether clinicians who learn FFT in a 6-hour online training course followed by low intensity telephone supervision (i.e., one-half hour per month) maintain fidelity scores that are comparable to those achieved by clinicians who attend a live workshop followed by high intensity (i.e., weekly) supervision.
CONCLUSIONS AND FUTURE DIRECTIONS
Studies of family process and interventions in major psychiatric disorders are often written off as “old hat,” the residue of outmoded theories involving schizophrenogenic mothers and double-bind communications. As we have hopefully illustrated, the study of family processes in BD is challenging and can be a lifelong pursuit, especially when the end goal is developing effective treatments. Although we have traveled part way to our destination, multiple challenges remain.
First, we do not know what factors predict the long-term sustainability of usage of FFT or other psychoeducational treatments. Will FFT ever become a staple of care in community health settings? CMHCs are more interested than ever in evidence-based care. Although we are optimistic that more and more facilities will adopt family skill-based treatments, many systems do not prioritize working with family members, or have patient populations that are disconnected from their relatives. Some caregivers refuse to involve themselves in the patient’s treatment, having felt burned by the mental health system before. Others do not live nearby or are unable to afford mental health care. Solutions to problems of access to care are beginning to emerge in the form of electronic mail, telehealth (e.g., skype), and smartphone-based interventions. Eventually, these approaches may supplement or even replace face-to-face psychosocial treatments, although the potential for loss of efficacy or longevity of effects when relying on less personalized approaches needs to be explored.
Can FFT or other family interventions serve a preventative function? When are the “critical periods” in development when these interventions will have maximal effects? As described earlier, we are examining a briefer form of FFT (12 sessions) as an early intervention for youths (age 9 years–17 years) at high risk for BD, with follow-up into the age of risk—early adulthood. In conducting this study, we have noted the concern on the part of mental health administrators that preventative programs can be quite costly to administer, and need to be balanced against the costs of treatments for persons who have already developed debilitating disorders. Our view is that taking part in 12 sessions of family education and skills training may reduce the odds that a high-risk person develops BD, or at minimum may reduce the level of symptom severity or functional impairment associated with its onset. If these goals are achieved, the program will have more than paid for itself.
Supplementary Material
Table S1. Randomized and nonrandomized trials of family-focused treatment: recovery, relapse, and symptom severity in child and adult patients with bipolar and related disorders.
Table S2. Family-focused therapy competence and adherence scale: factor analytic solution.
Acknowledgments
Dr. Miklowitz receives research funding from the National Institute of Mental Health, the Carl and Roberta Deutsch Foundation, the Kayne Family Foundation, Danny Alberts Foundation, Attias Family Foundation, and the American Foundation for Suicide Prevention. He has received book royalties from Guilford Press and John Wiley and Sons. Dr. Chung receives research funding from the National Institute of Mental Health, National Institute of Minority Health and Health Disparities, the UCLA Clinical and Translational Science Institute/National Center for Advancing Translational Research, Centers for Medicare and Medicaid Innovations, and the Patient-Centered Outcomes Research Institute.
Footnotes
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article:
References
- Altorfer A, Kasermann ML, Hirsbrunner H. Arousal and communication: 1. The relationship between nonverbal, behavioral, and psychophysiological indices of the stress response. Journal of Psychophysiology. 1998;12:40–59. [Google Scholar]
- Baucom DH, Epstein N. Cognitive behavioral marital therapy. New York: Brunner/Mazel; 1990. [Google Scholar]
- Brown GW, Birley JLT, Wing JK. Influence of family life on the course of schizophrenic disorder. British Journal of Psychiatry. 1972;121:241–258. doi: 10.1192/bjp.121.3.241. [DOI] [PubMed] [Google Scholar]
- Chung BD, Mikesell L, Miklowitz DJ. Flexibility and structure: Characteristics of family-focused therapy perceived to enhance implementation in community settings. Community Mental Health Journal. 2014;50(7):787–791. doi: 10.1007/s10597-014-9733-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falloon IRH, Boyd JL, McGill CW. Family care of schizophrenia: A problem-solving approach to the treatment of mental illness. New York: Guilford Press; 1984. [Google Scholar]
- Falloon IRH, Boyd JL, McGill CW, Williamson M, Razani J, Moss HB, et al. Family management in the prevention of morbidity of schizophrenia. Archives of General Psychiatry. 1985;42:887–896. doi: 10.1001/archpsyc.1985.01790320059008. [DOI] [PubMed] [Google Scholar]
- Fiorillo A, Del Vecchio V, Luciano M, Sampogna G, De Rosa C, Malangone C, et al. Efficacy of psychoeducational family intervention for bipolar I disorder: A controlled, multicentric, real-world study. Journal of Affective Disorders. 2015;172C:291–299. doi: 10.1016/j.jad.2014.10.021. [DOI] [PubMed] [Google Scholar]
- Fiorillo A, Del Vecchio V, Luciano M, Sampogna G, Sbordone D, Catapano F, et al. Feasibility of a psychoeducational family intervention for people with bipolar I disorder and their relatives: Results from an Italian real-world multicentre study. Journal of Affective Disorders. 2016;190:657–662. doi: 10.1016/j.jad.2015.10.060. [DOI] [PubMed] [Google Scholar]
- Fredman SJ, Baucom DH, Boeding S, Miklowitz DJ. Relatives’ emotional involvement moderates the effects of family therapy for bipolar disorder. Journal of Consulting and Clinical Psychology. 2015;83(1):81–91. doi: 10.1037/a0037713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett AS, Miklowitz DJ, Howe ME, Singh MK, Acquaye TK, Hawkey CG, et al. Changes in brain function associated with family focused therapy for youth at high risk for bipolar disorder. Progress in Neuropsychopharmalogical and Biological Psychiatry. 2015;56C:215–220. [Google Scholar]
- Hinshaw SP, Cicchetti D. Stigma and mental disorder: Conceptions of illness, public attitudes, personal disclosure, and social policy. Development and Psychopathology. 2000;12(4):555–598. doi: 10.1017/s0954579400004028. [DOI] [PubMed] [Google Scholar]
- Hooley JM. Expressed emotion and relapse of psychopathology. Annual Review of Clinical Psychology. 2007;3:329–352. doi: 10.1146/annurev.clinpsy.2.022305.095236. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Gotlib IH. A diathesis-stress conceptualization of expressed emotion and clinical outcome. Applied and Preventive Psychology. 2000;9:131–151. [Google Scholar]
- Imber-Mintz L, Liberman RP, Miklowitz DJ, Mintz J. Expressed emotion: A call for partnership among relatives, patients, and professionals. Schizophrenia Bulletin. 1987;13:227–235. doi: 10.1093/schbul/13.2.227. [DOI] [PubMed] [Google Scholar]
- Jacobson N, Margolin G. Marital therapy. New York: Brunner/Mazel; 1979. [Google Scholar]
- Kim EY, Miklowitz DJ. Expressed emotion as a predictor of outcome among bipolar patients undergoing family therapy. Journal of Affective Disorders. 2004;82:343–352. doi: 10.1016/j.jad.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Leff J, Berkowitz R, Shavit N, Strachan A, Glass I, Vaughn C. A trial of family therapy versus a relatives’ group for schizophrenia: Two-year follow-up. British Journal of Psychiatry. 1990;157:571–577. doi: 10.1192/bjp.157.4.571. [DOI] [PubMed] [Google Scholar]
- Manji H. The role of synaptic and cellular plasticity cascades in the pathophysiology and treatment of mood and psychotic disorders. Bipolar Disorders. 2009;11(suppl 1):2–3. [Google Scholar]
- Marvin SE, Miklowitz DJ, O’Brien MP, Cannon TD. Family-focused therapy for youth at clinical high risk of psychosis: Treatment fidelity within a multisite randomized trial. Early Intervention in Psychiatry. 2014;10:137–143. doi: 10.1111/eip.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ. Family risk indicators in schizophrenia. Schizophrenia Bulletin. 1994;20:137–149. doi: 10.1093/schbul/20.1.137. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Axelson DA, Birmaher B, George EL, Taylor DO, Schneck CD, et al. Family-focused treatment for adolescents with bipolar disorder: Results of a 2-year randomized trial. Archives of General Psychiatry. 2008;65(9):1053–1061. doi: 10.1001/archpsyc.65.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Axelson DA, George EL, Taylor DO, Schneck CD, Sullivan AE, et al. Expressed emotion moderates the effects of family-focused treatment for bipolar adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:643–651. doi: 10.1097/CHI.0b013e3181a0ab9d. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, George EL, Richards JA, Simoneau TL, Suddath RL. A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. Archives of General Psychiatry. 2003;60:904–912. doi: 10.1001/archpsyc.60.9.904. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ. Behavioral family treatment for patients with bipolar affective disorder. Behavior Modification. 1990;14:457–489. doi: 10.1177/01454455900144005. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Falloon IRH, Doane JA. Interactional correlates of expressed emotion in the families of schizophrenics. British Journal of Psychiatry. 1984;144:482–487. doi: 10.1192/bjp.144.5.482. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Nuechterlein KH. Verbal interactions in the families of schizophrenic and bipolar affective patients. Journal of Abnormal Psychology. 1995;104:268–276. doi: 10.1037//0021-843x.104.2.268. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Nuechterlein KH, Snyder KS, Mintz J. Family factors and the course of bipolar affective disorder. Archives of General Psychiatry. 1988;45:225–231. doi: 10.1001/archpsyc.1988.01800270033004. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, O’Brien MP, Schlosser DA, Addington J, Candan KA, Marshall C, et al. Family-focused treatment for adolescents and young adults at high risk for psychosis: Results of a randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53(8):848–858. doi: 10.1016/j.jaac.2014.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Kogan JN, Sachs GS, et al. Intensive psychosocial intervention enhances functioning in patients with bipolar depression: Results from a 9-month randomized controlled trial. American Journal of Psychiatry. 2007;164:1340–1347. doi: 10.1176/appi.ajp.2007.07020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Wisniewski SR, Kogan JN, et al. Psychosocial treatments for bipolar depression: A 1-year randomized trial from the Systematic Treatment Enhancement Program. Archives of General Psychiatry. 2007;64:419–427. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Schneck CD, George EL, Taylor DO, Sugar CA, Birmaher B, et al. Pharmacotherapy and family-focused treatment for adolescents with bipolar I and II disorders: A 2-year randomized trial. American Journal of Psychiatry. 2014;171(6):658–667. doi: 10.1176/appi.ajp.2014.13081130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Schneck CD, Singh MK, Taylor DO, George EL, Cosgrove VE, et al. Early intervention for symptomatic youth at risk for bipolar disorder: A randomized trial of family-focused therapy. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(2):121–131. doi: 10.1016/j.jaac.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Strachan AM, Goldstein MJ, Doane JA, Snyder KS, Hogarty GE, et al. Expressed emotion and communication deviance in the families of schizophrenics. Journal of Abnormal Psychology. 1986;95(1):60–66. doi: 10.1037//0021-843x.95.1.60. [DOI] [PubMed] [Google Scholar]
- Nagy N, Sabry W, Khalifa D, Hashem R, Zahran N, Khalil AH. Relapse rate and outcome correlates in Egyptian patients with bipolar disorder treated with behavioural family psychoeducation. Middle East Current Psychiatry. 2015;22:121–131. [Google Scholar]
- O’Brien MP, Miklowitz DJ, Cannon TD. A randomized trial of family focused therapy with youth at clinical high risk for psychosis: Effects on interactional behavior. Journal of Consulting and Clinical Psychology. 2014;82(1):90–101. doi: 10.1037/a0034667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MP, Miklowitz DJ, Cannon TD. Decreases in perceived maternal criticism predict improvement in sub-threshold psychotic symptoms in a randomized trial of family-focused therapy for individuals at clinical high risk for psychosis. Journal of Family Psychology. 2015;29(6):945–951. doi: 10.1037/fam0000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozerdem A, Oguz M, Miklowitz DJ, Cimilli C. Family-focused treatment for patients with bipolar disorder in Turkey: A case series. Family Process. 2009;48(3):417–428. doi: 10.1111/j.1545-5300.2009.01292.x. [DOI] [PubMed] [Google Scholar]
- Peris TS, Miklowitz DJ. Parental expressed emotion and youth psychopathology: New directions for an old construct. Child Psychiatry and Human Development. 2015;46(6):863–873. doi: 10.1007/s10578-014-0526-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rea MM, Tompson M, Miklowitz DJ, Goldstein MJ, Hwang S, Mintz J. Family focused treatment vs. individual treatment for bipolar disorder: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2003;71:482–492. doi: 10.1037/0022-006x.71.3.482. [DOI] [PubMed] [Google Scholar]
- Rohrbaugh MJ, Shoham V. Brief therapy based on interrupting ironic processes: The Palo Alto model. Clinical Psychology: Science and Practice. 2001;8(1):66–81. doi: 10.1093/clipsy.8.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfarb IS, Miklowitz DJ, Goldstein MJ, Harmon L, Nuechterlein KH, Rea MM. Family transactions and relapse in bipolar disorder. Family Process. 2001;40(1):5–14. doi: 10.1111/j.1545-5300.2001.4010100005.x. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Nierenberg AA, Calabrese JR, Marangell LB, Wisniewski SR, Gyulai L, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. New England Journal of Medicine. 2007;356(17):1711–1722. doi: 10.1056/NEJMoa064135. [DOI] [PubMed] [Google Scholar]
- Simoneau TL, Miklowitz DJ, Richards JA, Saleem R, George EL. Bipolar disorder and family communication: Effects of a psychoeducational treatment program. Journal of Abnormal Psychology. 1999;108:588–597. doi: 10.1037//0021-843x.108.4.588. [DOI] [PubMed] [Google Scholar]
- Simoneau TL, Miklowitz DJ, Saleem R. Expressed emotion and interactional patterns in the families of bipolar patients. Journal of Abnormal Psychology. 1998;107:497–507. doi: 10.1037//0021-843x.107.3.497. [DOI] [PubMed] [Google Scholar]
- Strachan AM, Feingold D, Goldstein MJ, Miklowitz DJ, Nuechterlein KH. Is expressed emotion an index of a transactional process? II. Patient’s coping style. Family Process. 1989;28:169–181. doi: 10.1111/j.1545-5300.1989.00169.x. [DOI] [PubMed] [Google Scholar]
- Strachan AM, Leff JP, Goldstein MJ, Doane JA, Burtt C. Emotional attitudes and direct communication in the families of schizophrenics: A cross-national replication. British Journal of Psychiatry. 1986;149:279–287. doi: 10.1192/bjp.149.3.279. [DOI] [PubMed] [Google Scholar]
- Sturgeon D, Turpin G, Kuipers L, Berkowitz R, Leff J. Psychophysiological responses of schizophrenic patients to high and low expressed emotion relatives: A follow-up study. British Journal of Psychiatry. 1984;145:62–69. doi: 10.1192/bjp.145.1.62. [DOI] [PubMed] [Google Scholar]
- Sullivan AE, Judd CM, Axelson DA, Miklowitz DJ. Family functioning and the course of adolescent bipolar disorder. Behavior Therapy. 2012;43:837–847. doi: 10.1016/j.beth.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarrier N, Barrowclough C, Porceddu K, Watts S. The assessment of psychophysiological reactivity to the expressed emotion of the relatives of schizophrenic patients. British Journal of Psychiatry. 1988;152:618–624. doi: 10.1192/bjp.152.5.618. [DOI] [PubMed] [Google Scholar]
- Vaughn CE, Leff JP. The influence of family and social factors on the course of psychiatric illness: A comparison of schizophrenia and depressed neurotic patients. British Journal of Psychiatry. 1976;129:125–137. doi: 10.1192/bjp.129.2.125. [DOI] [PubMed] [Google Scholar]
- Weisman AG, Okazaki S, Gregory J, Goldstein MJ, Tompson MC, Rea M, et al. Evaluating therapist competency and adherence to behavioral family management with bipolar patients. Family Process. 1998;37:107–121. doi: 10.1111/j.1545-5300.1998.00107.x. [DOI] [PubMed] [Google Scholar]
- Wendel JS, Miklowitz DJ, Richards JA, George EL. Expressed emotion and attributions in the relatives of bipolar patients: An analysis of problem-solving interactions. Journal of Abnormal Psychology. 2000;109:792–796. doi: 10.1037//0021-843x.109.4.792. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Randomized and nonrandomized trials of family-focused treatment: recovery, relapse, and symptom severity in child and adult patients with bipolar and related disorders.
Table S2. Family-focused therapy competence and adherence scale: factor analytic solution.


