Abstract
Research has shown that family functioning has been positively associated with physical activity and dietary intake, both of which are obesity-related risk factors. The most widely practiced methodological approach to assessing this construct in empirical studies relies on either parent or adolescent report. Yet, discrepancy in parent and adolescent report of family functioning may provide a fuller understanding of the effects of this construct on obesity-related health outcomes. This is especially important among Hispanics, a population that suffers from disproportionately high rates of obesity and its health-related consequences. The purpose of this study was to examine whether, and to what extent, parent-adolescent discrepancies in family functioning are associated with physical activity, and fruit and vegetable and added sugar intake. We estimated discrepancy scores between parents and adolescents (n=280 dyads) in family functioning. Then, using structural equation modeling, we tested the effect of family functioning discrepancy on adolescent reports of physical activity, fruits and vegetables intake, and added sugar intake. After controlling for adolescent’s gender and BMI, family functioning discrepancy was significantly associated with reduced physical activity (β= −.14*, 95% CI (−.26, −.05)) and fruits and vegetables intake (β= −.22*, 95% CI (−.38, −.09)) such that the larger the discrepancy between parent and youth reported family functioning, the fewer days of adolescent physical activity and the poorer the fruits and vegetables intake. Our findings provide insight for the role of the family in Hispanic adolescent health outcomes and rationale for capturing rich data to better understand that role.
Keywords: Family functioning, obesity, overweight, Hispanic, adolescent
INTRODUCTION
Childhood overweight and obesity continue to be major clinical and public health challenges in the United States. While trends for childhood obesity have leveled-off in some groups, ethnic and racial disparities are still a growing public health concern. The prevalence of obesity (body mass index [BMI] at or above the 95th percentile adjusted for age and sex) is highest among Hispanics ages 12–19 than in any other major ethnic group (22.8% versus 22.6 % for non-Hispanic black, 19.6 % for non-Hispanic white, 9.4% for Asians; Ogden et al., 2016). Sequelae associated with overweight and obesity are also disproportionately affecting Hispanic children and adolescents. Most notably, the prevalence per 1000 of type 2 diabetes in 10-to 19-year-olds is 0.79 for Hispanics versus 0.17 for non-Hispanic whites (Dabelea et al., 2014). Additionally, Hispanics ages 2–19 have the highest rates of non-alcoholic fatty liver disease compared to non-Hispanic whites, non-Hispanic blacks, and Asians (Schwimmer et al., 2006). Moreover, Hispanic adolescents are less likely to engage in healthy behaviors. For example, according to the Youth Risk Behavior Surveillance System (Kann et al., 2016), the prevalence of not having eaten vegetables was higher among Hispanic (8.5%) than white (4.9%) students and the prevalence of not having participated in at least 60 minutes of physical activity on at least 1 day of the last seven days was higher among Hispanic (15.6%) than white (11.6%) students. As the Hispanic population continues to grow in the US to a projected 28.1% by 2060 (U.S. Census Bureau, 2014), addressing these disparities needs to continue to be a national public health priority.
Etiology of Obesity Related Risk Factors: Family Functioning
The family system has been found to be among the most influential social system impacting health related behaviors. Family functioning has been linked to physical, mental, emotional, and behavioral health outcomes as well as developmental and academic outcomes (Zubrick, Williams, Silburn, Vimpani, 2000;. Renzaho, Kumanyika, & Tucker, 2011; Kim, Viner-Brown, Garcia, 2007; Annunziata, Hogue, Faw, & Liddle, 2006). For example, research has found that higher levels of family functioning (i.e., positive parenting, parental involvement, family communication, parental monitoring of peers, and parent–adolescent communication) prevent and reduce substance use and sexual risk behaviors in Hispanic youth (Cordova, Huang, Pantin, & Prado, 2012; Prado et al., 2012a; Prado et al., 2012b). Similarly, there is growing evidence documenting the family’s impact on obesity-related risk and protective factors, specifically the parenting style. Studies have shown that children from homes with an authoritative parenting style, that is one that respects the child’s opinion but sets clear boundaries, are more likely to eat healthy, be physically active, and have a lower BMI (Sleddens, Gerards, Thijs, de Vries, & Kremers, 2011). However, parenting style is one aspect of family functioning (Rhee, 2008), and for adolescents who are gaining more independence in terms of their health choices (Basset, Chapman, & Beagan, 2008), the general family functioning may be more impactful.
Although there are far fewer studies evaluating the family’s impact on obesity related outcomes than other health outcomes, a systematic review concluded that children and adolescents who are overweight or obese are more likely to come from families with poor family functioning (Halliday, Palma, Mellor, Green &, Renzaho, 2014). Studies indicate that families with overweight or obese children and/or adolescents report higher family conflict (Zeller et al., 2007) and lower family cohesion (Kitzmann et al., 2008). Another study examining the association of adolescent girls’ perception of family cohesion on healthy eating behaviors found that greater family cohesion predicted more days of eating breakfast and consuming less soda (Franko et al., 2008). It is notable that of the 21 studies included in the previously mentioned systematic review (Halliday et al., 2014), only two included Hispanics in their study population creating an important gap in this literature (Zeller et al., 2007; McConley et al., 2011).
Reports of Family Functioning
To date the most widely practiced methodological approach to assessing family functioning in empirical studies uses only parent or adolescent report of this contstruct (e.g., Hooper, Burnham, & Richey, 2009; Haines et al., 2016). The parent’s report has been traditionally used to measure family functioning since in many family-based preventive interventions parents are seen as the change agents and the majority of intervention activities are directed towards parents (Prado et al., 2007). However, when both parents and adolescents have completed measures of family functioning, parents have reported more favorable levels of this construct than have adolescents (Ohannessian, Lerner, Lerner, & von Eye, 1995; Schwartz, Mason, Pantin, & Szapocznik, 2008; Stuart & Jose, 2012).
Significant parent-adolescent incongruence is common even when informants complete identical or valid parrallel measures (Laird & De los Reyes, 2013; Pasch, Stigler, Perry, & Komro, 2010). Yet, research examining the congruence between parent and adolescent report have historically concluded inconsistent findings (De los Reyes, 2011). Recently, clinicians and researchers have come to find that there is value in this informant discrepancy and its impact on health behaviors. The primary understanding of this discrepancy is that reports from different informants (e.g., parent and adolescent) reflect their individual perspective of the construct (Taber, 2010). Regarding perceived family behaviors, the literature reveals that parent-youth agreement to be small to moderate. For example, studies have shown parent-adolescent discrepancies in reports of parenting (Guion, Mrug, & Windle, 2009) and, specifically, parental monitoring (Han et al, 2012). These discrepancies have been investigated as risk factors following the logic that if parents and adolescents disagree on family behaviors, family functioning, and/or parenting, it would result in adverse health outcomes (De los Reyes, 2015; Cordova et al., 2014; Maurizi, Gershoff, & Aber, 2012; Abar, Jackson, Colby, & Barnett, 2015). For example, one study found that parent–adolescent family functioning discrepancies are associated with an increased HIV risk behaviors in Hispanic adolescents (Cordova et al., 2014). To date, no studies have examined the impact of family functioning discrepancy in relation to obesity related outcomes. Furthermore, discrepancy in parent and adolescent report of family functioning may provide a fuller understanding of the effects of this construct on obesity related health outcomes especially in Hispanic families who are traditionally strongly family centric (Toro-Morn, 2015).
The purpose of this study was to examine whether, and to what extent parent–adolescent discrepancies in family functioning are associated with lack of physical activity and poor dietary intake. Given the previous literature of parent-adolescent incongruence as a risk factor, we hypothesize that greater parent–adolescent discrepancies in family functioning will be related to poor dietary intake and lack of physical activity.
METHODS
This study utilized data from the baseline assessment of a randomized controlled trial conducted in collaboration with the Miami Dade County Public School system (MDCP-S). The larger trial evaluated the efficacy of a family-based obesity preventive intervention. Inclusion criteria specified that participants had to be Hispanic, have a BMI > 85%-ile for age and sex, and be in 7th or 8th grades. This study was approved by both the University of Miami and MDCP-S Institutional Review Boards.
Participants
The study sample consisted of 280 Hispanic overweight and obese 7th and 8th grade youth and their primary caregivers recruited from middle schools in MDCP-S. Participant demographics are presented on Table 1. The majority of the adolescents were female (52%). The range of adolescents’ age was 11–15 and the mean age was 13.01. Most of the adolescent with were born in US (64%). The majority of adolescents born outside of the US were native to Cuba (19.3%). The majority of adolescents reported living in the US more than 10 years (66.1%). For parents, 88.2% were female and 11.8% were male. The range of parents’ age was 24–59 and the mean age was 41.88. The majority (97.9%) of parents were the primary caregiver with 87.5% of parents being the mother and 11.8% being the father. The majority of parents were born outside of the US (91.1%), were married (57.9%), and had an annual income less than $30,000 (65.4%).
Table 1.
Participant Demographics (N= 280 dyads)
| Variable | Mean (SD) or % |
|---|---|
| Adolescent | |
| Female | 52% |
| Age | 13.01 (0.83) |
| Country of Origin | |
| US | 64% |
| Cuba | 19.3% |
| Honduras | 4.3% |
| Venezuela | 3.6% |
| BMI | 28.06 (6.07) |
| Obesity (> 30 BMI) | 23.8% |
| Parent | |
| Female | 88.2% |
| Age | 44.88 (6.5) |
| Country of Origin | |
| US | 8.9% |
| Cuba | 34.3% |
| Nicaragua | 15% |
| Honduras | 11.4% |
| Marital Status | |
| Married | 57.9% |
| Divorced | 12.9% |
| Living with someone | 10% |
| Separated | 10% |
| Never married & not living with someone | 8.6% |
| Widowed | 0.7% |
| Full-time employment | 50.7% |
| Annual Income | |
| Less than $30,000 | 65.4% |
| Greater than $30,000 | 20.7% |
| Greater than $50,000 | 13.9% |
Measures
The measures used in this study have been used by our research team and others with Hispanic populations for over 15 years (e.g., Estrada et al., 2017; Pantin et al., 2003; Prado et al., 2007; Prado et al., 2012a; Santisteban et al., 2003). They were originally translated by our research team using back translation and committee approaches recommended by Kurtines & Szapocznik (1995) and have been found to be valid and reliable in our studies.
Family functioning
Family functioning was assessed using adolescent and parent reports of five indicators: positive parenting, parental involvement, family communication, parental monitoring of peers, and parent–adolescent communication. Each of the scales used to assess the indicators of family functioning were developed for diverse ethnic youth and have been used in various all-Hispanic youth trials (Pantin et al., 2003; Prado et al., 2012b; Estrada et al. 2017).
Corresponding subscales from the Parenting Practices Scale (Gorman-Smith, Tolan, Zelli, & Huesmann, 1996) were used to assess positive parenting and parental involvement. The positive parenting subscale (9 items, adolescent report α = .79, parent report α =.68) measures parent responses to good behaviors. Sample items for the adolescent include “When you have done something that your parent likes or approve of, how often does she/he give you something like a hug, kiss, or pat on the back for it?”, and for the parent, “When your child has done something that you like or approve of, how often do you give you child something like a hug, kiss, or pat on the back for it?” The response choices ranged from “0 = never” to “4 = often.” The parental involvement subscale (16 items, adolescent report α = .84, parent report α = .73) measures the degree to which the parent is involved in the child’s life. Sample items for the adolescent include “How often do you have a friendly talk with your parent?”, and for the parent, “How often do you have a friendly talk with your youth?” with a response range of “0 = never to “4 = always.”
The communication subscale from the Family Relations Scale (Tolan, Gorman-Smith, Huesmann, & Zelli, 1997) was used to assess family communication (3 items, adolescent report α = .68, parent report α = .79). Sample questions included “My family and I have the same views about what is right and wrong” and “My family knows what I mean when I say something.” Response choices ranged from “1 = not true at all” to “3 = true a lot.”
The Parent Relationship with Peer Group Scale (Pantin, 1996) was used to assess parental monitoring of peers (5 items, adolescent report α = .84, parent report α = .80). This measure asks parents to indicate the extent to which they supervise adolescents’ friends, activities, and whereabouts on a five-point Likert-type scale, ranging from “0 = not at all” to “5 = extremely well (often).” Sample items for the adolescent include “How well do your parents know your best friends?”, and for parents, “How well do you personally know your child’s best friends?”
The Parent–Adolescent Communication Scale (Barnes & Olson, 1985) was used to assess parent-adolescent communication (20 items, adolescent report α = .86, parent report α = .84). A sample adolescent question included “When I ask questions, I get honest answers from my mother/father” and for parent, “When I ask questions I get honest answers from my child.” Response choices ranged from “1 = strongly disagree” to “5 = strongly agree.”
Dietary Intake
Dietary intake was assessed using the Dietary Screener Questionnaire (DSQ) in the National Health and Nutrition Examination Survey (NHANES) (Block, Dresser, Hartman, & Caroll, 1985). The questionnaire asks participants how much of 22 specific foods or beverages they have had to eat on average in the past month. Items reflect both good (fruit, vegetable, whole grains) and poor (doughnuts, candy) dietary choices. There are eight responses choices ranging from “Never” to “2 or more times per day”. The fruit and vegetable dietary factor consists of the following food items: fruit, fruit juice, salad, fried potatoes, other potatoes, dried beans, other vegetables, tomato sauce, salsa, and pizza. The added sugars dietary factor consists of the following food items: soda, fruit drinks, cookies, cake and pie, doughnuts, ice cream, sugar/honey in coffee/tea, candy, and cereal and cereal type. For the current analyses, we used algorithms developed by the National Cancer Institute (NCI) for use with the DSQ (available at https://epi.grants.cancer.gov/nhanes/dietscreen/scoring/current#scoring) to calculate daily fruit and vegetable consumption (unit: a cup; Mean [SD] = 3.38 [2.53]; skewness = 1.67) and daily added sugar consumption (unit: tsp; Mean [SD] = 17.80 [17.00]; skewness = 2.78). Following George and Mallery (2010), daily sugar intake was positively skewed, and was log-transformed for analyses.
Physical Activity
Moderate-to-vigorous physical activity was assessed by asking youth the following questions: “During the past 7 days, on how many days were you physically active for a total of at least 60 minutes per day? Add up all the time you spend in any kind of physical activity that increase your heart rate and make you breathe hard some of the time” as is asked in the NHANES Physical Activity and Physical Fitness Questionnaire (2012; Mean [SD]= 3.64 [2.34], Skewness = −.02).
Analytical Strategy
The purpose of the study was to investigate discrepancy scores between parent-reported scores and adolescent-reported scores in family functioning and to examine the association between discrepancy scores and healthy-related behaviors (i.e., dietary intake and physical activity). To address these issues, the analytic plan consisted of several analytical steps.
First, we conducted a series of paired sample t-tests to investigate the mean difference between parent-reported scores and adolescent-reported scores across multiple family functioning indicators. Second, to examine the associations between parent-reported and adolescent-reported scores across the five family function indicators, we estimated a series of bivariate correlations coefficients between parent-reported and adolescent-reported scores across the five family function indicators. Pruchno (1989) suggested that high correlations imply low discrepancy (high congruence between parents and adolescents), and low correlations imply high discrepancy (low congruence between parents and adolescents).
Third, we estimated standardized different scores (Shishido & Latzman, 2017) between parent-reported and adolescent-reported scores across the five family function indicators. In the standardized difference scores approach, parent and adolescent’s raw scores are first converted to standardized scores (z-scores). Discrepancy scores are then calculated by subtracting adolescent’s z-scores from parent’s z scores on each of five family function indicators (positive parenting, parental involvement, family communication, parental monitoring of peer, and parent-adolescent communication). The use of z scores has been shown to equalize the influence from the differential distribution of parent and adolescent’s raw scores as well as to adjust for potential systematic bias (De Los Reyes & Kazdin, 2004). Then, using a confirmatory factor analysis, the shared variance for common discrepancy scores across multiple discrepancies in family function was estimated. The model fit was evaluated using the Comparative Fit Index (CFI; >.90 acceptable fit), Tucker-Lewis Index (TLI; >.90 acceptable fit), and the Root mean square error of approximation (RMSEA; < .08 acceptable fit; Little, 2013).
Fourth, structural equation modeling (SEM) was estimated to examine whether, and the extent to which, the parent-adolescent family functioning discrepancy scores were associated with obesity-related behaviors (i.e., physically active days, fruit and vegetable- and sugar intakes). To estimate more unique associations between discrepancy scores of family functioning and obesity-related behaviors, we controlled for potential covariates (youth’s gender and BMI) to estimate path coefficients. For all analyses, we used a full-information maximum likelihood (FIML) estimator with robust standard errors, implemented as MLR in Mplus (Version 7.2; Muthén & Muthén, 1998–2012) statistical software to estimate the parameters.
Results
Descriptive analyses for each indicator of parent and adolescent reports of family functioning (i.e., positive parenting, parental involvement, family communication, parental monitoring of peers, and parent-adolescence communication) and correlations between parent and adolescent reports of each of the indicators are reported in Table 2. The result of the paired t-tests show that parents’ scores were statistically higher across most of the family functioning variables compared to the adolescents’ scores (t-values = 31.36 (p < .001), 37.05 (p < .001), 11.79 (p < .01), and 15.56 (p < .001) for positive parenting, family communication, peer monitoring, and parent-adolescent communication, respectively), except for parental involvement (t-value=.03, p = .86). In addition, as can be seen from Table 2, the correlations among family functioning indicators were low (correlations ranged from .04 to .28), implying the existence of discrepancy scores between parents and adolescents in family functioning.
Table 2.
Descriptive statistics among study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parent reports | |||||||||||||||
| 1. Positive parenting | - | ||||||||||||||
| 2. Parental Involvement | .37 | - | |||||||||||||
| 3. Family communication | .13 | .31 | - | ||||||||||||
| 4. Peer monitoring | .23 | .49 | .22 | - | |||||||||||
| 5. P-A communication | .11 | .48 | .37 | .37 | - | ||||||||||
| Adolescent reports | |||||||||||||||
| 6. Positive parenting | .04 | .07 | -.01 | .05 | .09 | - | |||||||||
| 7. Parental Involvement | .05 | .21 | .01 | .20 | .19 | .55 | - | ||||||||
| 8. Family communication | −.07 | .18 | .19 | .22 | .24 | .32 | .45 | - | |||||||
| 9. Peer monitoring | .11 | .09 | .03 | .28 | .09 | .27 | .48 | .27 | - | ||||||
| 10. P-A communication | .01 | .17 | -.04 | .17 | .21 | .39 | .62 | .50 | .37 | - | |||||
| Obesity-related behaviors | |||||||||||||||
| 11. Physically active days | .07 | .04 | .05 | .07 | .07 | .13 | .19 | .08 | .15 | .06 | - | ||||
| 12. Fruit and vegetable intake | .12 | −.03 | −.09 | −.01 | −.09 | .21 | .12 | −.02 | .08 | .07 | .14 | - | |||
| 13. Added sugar intake | .05 | −.03 | −.05 | −.05 | −.06 | .10 | .01 | .02 | −.05 | −.08 | .11 | .51 | - | ||
| Control variables | |||||||||||||||
| Youth related factors | |||||||||||||||
| 14. Female (vs. Male) | −.15 | −.01 | −.05 | −.03 | −.05 | −.07 | .01 | −.08 | .04 | −.10 | −.15 | −.19 | −.24 | - | |
| 15. Youth’s BMIa | .10 | −.05 | .05 | .02 | −.10 | .18 | .07 | .02 | .08 | .13 | −.13 | .13 | .05 | −.07 | - |
|
| |||||||||||||||
| Mean (or Proportion) | 23.2 | 43.4 | 7.3 | 10.6 | 77.0 | 20.8 | 43.2 | 6.5 | 9.4 | 73.5 | 3.6 | 3.3 | 17.8 | 52% | 0.0 |
| Standard deviation | 4.1 | 6.4 | 1.7 | 4.7 | 10.7 | 6.0 | 9.0 | 1.7 | 4.9 | 13.2 | 2.3 | 2.5 | 17.0 | - | 1.0 |
| Range (Observed) | |||||||||||||||
| Min | 12.0 | 18.1 | 0.0 | 0.0 | 42.0 | 0.0 | 12.0 | 1.0 | 0.0 | 34.0 | - | - | - | - | - |
| Max | 32.0 | 58.0 | 9.0 | 20.0 | 100.0 | 32.0 | 60.0 | 9.0 | 20.0 | 98.0 | - | - | - | - | - |
| Range (Possible) | |||||||||||||||
| Min | 0.0 | 0.0 | 0.0 | 0.0 | 20.0 | 0.0 | 0.0 | 0.0 | 0.0 | 20.0 | - | - | - | - | - |
| Max | 36.0 | 64.0 | 9.0 | 20.0 | 100.0 | 36.0 | 64.0 | 9.0 | 20.0 | 100.0 | - | - | - | - | - |
Note. P-A communication = Parent-Adolescent communication. Bold and italic coefficients represent significant correlations at p < .05.
Standardized scores.
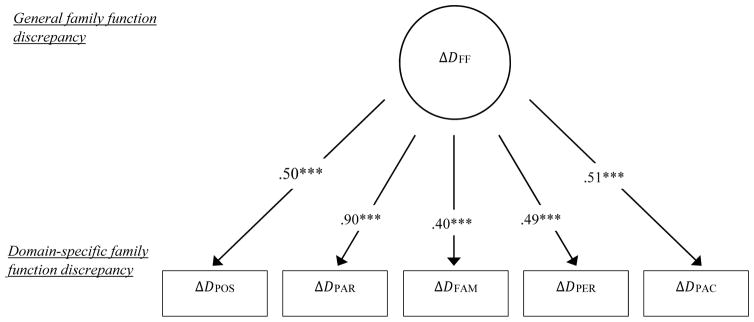
Next, using standardized discrepancy scores of five family function indicators, we estimated the common factor of family functioning discrepancy. The results are shown in Figure 1. The model fit were acceptable (χ2(df)= 9.56 (4); CFI/TLI = .98/.94; SRMR= .03). Also, the standardized loadings ranged from .40 (between latent discrepancy factor and Δ family communication) to .90 (between latent discrepancy factor and Δparental involvement), indicating that discrepancy scores of domain-specific family functioning indicators contributed to produce the latent discrepancies of common discrepancy of family functioning.
Figure 1.
A multivariate latent discrepancy score model for family functioning between parents rating and adolescents rating
Note. D= Discrepancy score. FF= Family functioning. POS=Positive parenting. PAR=Parental involvement. FAM= Family communication. PER= Peer monitoring. PAC=Parent-Adolescent communication. χ2 (df)= 9.56 (4); CFI/TLI = .98/.94; RMSEA=.07; SRMR= .03. ***p < .001.
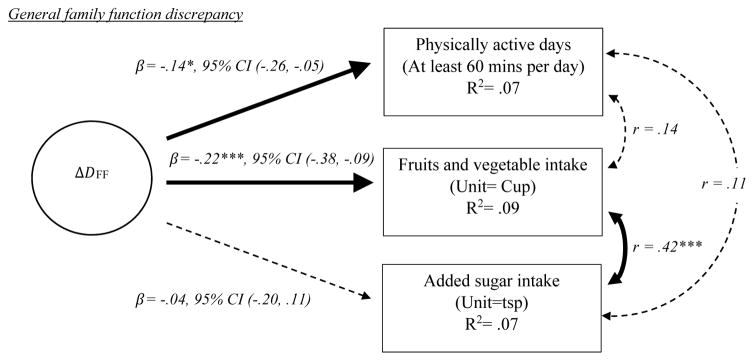
Finally, we investigated associations between latent discrepancy of family functioning and obesity-related behaviors (i.e., physically active days, fruit and vegetable intake, and sugar intake; see figure 2). The model fit was acceptable (χ2(df) = 45.28 (37), p < .001, CFI/TLI = .98/.96, RMSEA=.03, SRMR=.03). The results showed that the discrepancy scores of family functioning were negatively linked to both physically active days (β= −.14, p < .05, 95% CI (−.26, −.05)) and fruit and vegetable intake (β= −.22, p < .001, 95% CI (−.38, −.09)).
Figure 2.
The effect of discrepancy in parent-adolescent family functioning ratings on obesity-related behaviors
Notes. D= Discrepancy score. FF= Family functioning. CI= Confidence Interval. Standardized coefficients are shown. Dotted lines indicate non-significant paths. All path coefficients were estimated after adjusting covariate effects (i.e., adolescent’s gender and BMI). χ2 (df) =45.28(37), p < .001, CFI/TLI = .98/.96, RMSEA=.03, SRMR=.03.
*p < .05. ***p < .001.
After controlling for the associations between discrepancy scores in family functioning and obesity-related behaviors, we also found gender difference on obesity-related behaviors (see table 2). For example, females showed lower levels of physical activity (β= −.17, p < .01, 95% CI (−.28, −.05)), fruits and vegetable intake (β= −.20, p < .01, 95% CI (−.44, −.12)), and sugar intake (β= −.23, p < .01, 95% CI (−.56, −.19)). In addition, BMI was negatively associated to physically active days (β= −.16, p < .01, 95% CI (−.28, −.05)).
DISCUSSION
The purpose of this study was to examine whether, and to what extent, parent–adolescent discrepancies in family functioning are associated with lack of physical activity and poor dietary intake (i.e. fruit and vegetable intake and added sugar intake). To the best of our knowledge, this is the first study to examine the effects of parent–adolescent discrepancies in family functioning on obesity risk behaviors in a sample of overweight/obese Hispanic youth.
Study findings indicate that parent–adolescent discrepancies in family functioning are associated with Hispanic youth obesity risk behaviors such that greater discrepancies are related to poorer fruit and vegetable intake and less physical activity. This finding did not hold true for added sugar intake. The addition of covariates (adolescent’s gender and BMI z scores) resulted in gender differences detected across all three obesity-related outcomes (i.e., physically active days, fruits and vegetable intake, and added sugar intake) after adjusting for other covariate effects. There was also a significant association between adolescent’s BMI and physical active days.
As expected, our findings indicate that the family functioning scores by parents for each functioning indicator except parental involvement were significantly higher than that of adolescents. This further strengthens the notion that studies assessing family functioning should collect data from both parents and youth. Our study suggests that parents and adolescents differ with respect to how they perceive family functioning. De los Reyes and colleagues (2013) argue that too often researchers address informant discrepancies by treating them as measurement error. However, those discrepancies give important contextual clues and may profoundly impact the interpretation of empirical findings and their clinical implications (De los Reyes et al., 2013). Furthermore, Hunsley and Mash contend that informant ratings are not interchangeable and the use and interpretation of multiple informants are necessary components of best practice in evidence based assessment (2007). In fact, a recent meta-analysis of parent-adolescent congruence on three different constructs of parenting (acceptance, behavioral control, and psychological control) concluded that those discrepancies are significant and vary systematically (Korelitz, & Garber, 2016).
Informant discrepancies in families have typically been used to examine psychopathologies (De los Reyes & Kazdin, 2005). This study is the first to apply parent-adolescent discrepancies of family functioning to examine its relationship to the obesogenic environment. Better family functioning has long been known to be a protective factor that cuts across multiple health outcomes (Bernard, 1991). Yet, there have only been a few studies that investigated the effects of family functioning on the obesogenic environment of youth (Halliday et al., 2014), and none that focus on discrepancies in family functioning reports from two members of the same family. Additionally, those studies have examined study populations that have mostly non-Hispanic white participants, higher-income populations, and younger children. Cordova et al. (2014) suggest that discrepancies may be more pronounced in Hispanic families where they also face the challenges of acculturation discrepancies. Similar to previous research examining informant congruence (Han et al., 2012), our study provides provocative preliminary data that parent-adolescent discrepancies of family functioning reveal important information on Hispanic adolescent obesity related behaviors. However, since this was a cross-sectional study and the variance accounted for was small, better understanding of the way parent-adolescent discrepancies in family functioning impact health outcomes would be gained if future researchers incorporated both reports in their design and analyses.
Our results are consistent with prior findings that a more disjointed family leads to poorer obesity-related behaviors for adolescents (Zeller et al., 2007; Haines et al., 2016; Berge et al., 2013). For example, Haines and colleagues (2016) found that family functioning is protective for adolescent weight and weight-related health behaviors (such as disordered eating behaviors and physical activity). Similarly, Berge and colleagues (2013) found that higher family functioning was associated with greater meal participation, more frequent breakfast consumption, and less sedentary activity in adolescents. Notably, family functioning in these studies was determined by either the parent or the adolescent but not both. From an intervention science perspective, the findings from this study demonstrate that family-based obesity prevention interventions should focus on reducing family functioning discrepancies. If the intervention reduces the discrepancy, it may be able to change the behavior. Future studies need to be conducted to examine if reductions in family functioning discrepancies over time is related to changes in behavior over time.
Although the finding is novel, it is unsurprising that gender serves as a meaningful covariate to adjust the discrepancy effects of family functioning on obesity-related outcomes. In a review of family correlates of child and adolescent obesity, Berge (2009) describes gender differences across several family domains and the impact it has on obesity related factors. For example, studies have found that maternal food restriction is associated with increased energy intake and ultimately weight in girls (Birch, Fisher, & Davison, 2003; Fisher & Birch, 2002). Additionally, parental involvement has been reported to be an important determinant in the physical activity of young girls (Davison, Cutting, Birch, 2003; Thompson et al., 2003). In the case of Hispanic girls, findings have demonstrated that girls have engaged in more unhealthy eating when their parents use a controlling style to monitor their diet (Arredondo et al., 2006) and that Latino mothers are more restrictive with the diet of their daughters than with the diet of their sons (Olverra, Power, & Cousins, 1990). One study found that Hispanic girls get teased by their family about their weight more than their white counterparts (but not boys) which has been associated with BMI and disordered eating behaviors (Berg, Neumark-Sztainer, Eisenberg, & Haines, 2008). Our study demonstrates that not only is low family functioning a risk factor for obesity related factors, but that discrepancies between Hispanic parent and adolescent girls can also be impactful.
The study has important implications for clinical interventions. Discrepancies in family functioning between parent and adolescent indicate that focusing just on parenting or other family domains may not be enough to impact obesity-related behaviors; we need to focus on both reducing family function and addressing compromised family functioning. Study findings indicate that parents report higher in almost every family functioning indicator. However, to maximize the influence of the intervention, clinicians/researchers should focus on how the adolescent perceives the parent behavior. Interventionists may find it helpful to measure the incongruence between parent and adolescent and, when substantial discrepancies are found, explore the reasons for differences (Korelitz et al., 2016) with the goal being to foster family cohesion and improve functioning. As described, poor family functioning is a risk factor for obesity and obesity-related health factors; using discrepancies to further inform and personalize the intervention to the family may result in positive family functioning which in turn may impact the obesogenic environment.
Strengths of our study include that we utilized multi reporter as well as the multiple indicators to assess family functioning. Additionally, we collected data on an ethnic group facing a strong health disparity. The study also had several potential limitations. Although parents participating in this study were mostly biological parents (only 2 cases [.8%] were step-parents), results may have been different depending on which parent participated. The parent views captured in the current study represent only one person’s perspective, and it is possible that there are disagreements between parents/partners on family functioning. Another limitation is the use of self-reported data which allow for social desirability. This means that the prevalence of specific behaviors, like dietary intake and physical activity, may be underestimated. Also, this was a cross-sectional study and thus causality with respect to the impact of parent- adolescent discrepancies on adolescent obesity risk behaviors cannot be inferred. Lastly, the study sample is not representative of the U.S. overweight/obese Hispanic adolescent population and thus findings are not generalizable to all U.S. Hispanic youth in the same weight categories.
CONCLUSION
We found that parent adolescent discrepancies in family functioning are associated with an increase in Hispanic youth obesity risk behaviors such that greater discrepancies are related to poorer fruit and vegetable intake and lower levels of physical activity. Our findings add to conceptual models of health disparity research and the obesogenic environment. Findings are suggestive that family-based preventive interventions aimed at narrowing parent–adolescent family functioning discrepancies may aid in preventing and reducing Hispanic adolescent obesity related factors. Although further longitudinal studies are needed to understand the underpinnings for the development of these disparities, our findings provide insight for the role of the family in Hispanic adolescent health outcomes and rationale for capturing rich data to better understand that role.
Acknowledgments
This research was supported by a grant funded by the National Institute on Minority Health and Health Disparities (R01 MD007724) to Guillermo Prado, PhD (contact PI) and Sarah Messiah, PhD, MPH (Co-PI). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Contributor Information
Cynthia N. Lebron, PhD Student, Prevention Science and Community Health, Department of Public Health, University of Miami Miller School of Medicine.
Tae Kyoung Lee, Sr. Research Associate III, Department of Public Health Sciences, University of Miami Miller School of Medicine.
Sung Eun Park, PhD student, Research, Measurement, and Evaluation, School of Education and Human Development, University of Miami
Sara M. St George, Assistant Professor, Department of Public Health Sciences, University of Miami Miller School of Medicine.
Sarah E. Messiah, Research Associate Professor of Pediatrics and Public Health Sciences, Co-Director, Division of Community-Based Research and Training, Mailman Center for Child Development, The University of Miami Leonard M. Miller School of Medicine.
Guillermo Prado, Dean, Graduate School, Miller Professor of Public Health Sciences, Director, Division of Prevention Science and Community Health, University of Miami
References
- Abar CC, Jackson KM, Colby SM, Barnett NP. Parent–child discrepancies in reports of parental monitoring and their relationship to adolescent alcohol-related behaviors. Journal of youth and adolescence. 2015;44(9):1688–1701. doi: 10.1007/s10964-014-0143-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annunziata D, Hogue A, Faw L, Liddle HA. Family functioning and school success in at-risk, inner-city adolescents. J Youth Adolesc. 2006;35:105–13. doi: 10.1007/s10964-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arredondo EM, Elder JP, Ayala GX, Campbell N, Baquero B, Duerksen S. Is parenting style related to children’s healthy eating and physical activity in Latino families? Health education research. 2006;21(6):862–871. doi: 10.1093/her/cyl110. [DOI] [PubMed] [Google Scholar]
- Barnes HL, Olson DH. Parent–adolescent communication and the circumplex model. Child Development. 1985;56:438–447. doi: 10.2307/1129732. [DOI] [Google Scholar]
- Berg P, Neumark-Sztainer D, Eisenberg ME, Haines J. Racial/ethnic differences in weight-related teasing in adolescents. Obesity. 2008;16(S2) doi: 10.1038/oby.2008.445. [DOI] [PubMed] [Google Scholar]
- Berge JM. A review of familial correlates of child and adolescent obesity: what has the 21st century taught us so far? International journal of adolescent medicine and health. 2009;21(4):457–484. doi: 10.1515/IJAMH.2009.21.4.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Wall M, Larson N, Loth KA, Neumark-Sztainer D. Family Functioning: Associations With Weight Status, Eating Behaviors, and Physical Activity in Adolescents. Journal of Adolescent Health. 2013;52(3):351–357. doi: 10.1016/j.jadohealth.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard B. Fostering resiliency in kids: Protective factors in the family, school, and community. 1991. [Google Scholar]
- Birch LL, Fisher JO, Davison KK. Learning to overeat: maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. The American journal of clinical nutrition. 2003;78(2):215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block G, Dresser CM, Hartman AM, Carroll MD. Nutrient Sources In The American Diet: Quantitative Data From the NHANES II Survey: I. Vitamins And Minerals. Am J Epidemiol. 1985;122(1):13–26. doi: 10.1093/oxfordjournals.aje.a114072. [DOI] [PubMed] [Google Scholar]
- Cordova D, Huang S, Lally M, Estrada Y, Prado G. Do Parent-Adolescent Discrepancies in Family Functioning Increase the Risk of Hispanic Adolescent HIV Risk Behaviors? Fam Process. 2014;53(2):348–363. doi: 10.1111/famp.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordova D, Huang S, Pantin H, Prado G. Do the effects of a family intervention on alcohol and drug use vary by nativity status? Psychology of Addictive Behaviors. 2012;26:655–660. doi: 10.1037/a0026438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, … Hamman RF for the SEARCH for Diabetes in Youth Study. Prevalence of Type 1 and Type 2 Diabetes Among Children and Adolescents From 2001 to 2009. JAMA. 2014;311(17):1778–1786. doi: 10.1001/jama.2014.3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison KK, Cutting TM, Birch LL. Parents’ activity-related parenting practices predict girls’ physical activity. Medicine and science in sports and exercise. 2003;35(9):1589. doi: 10.1249/01.MSS.0000084524.19408.0C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A. Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2011;40(1):1–9. doi: 10.1080/15374416.2011.533405. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Measuring informant discrepancies in clinical child research. Psychological Assessment. 2004;16:330–334. doi: 10.1037/1040-3590.16.3.330. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological bulletin. 2005;131(4):483. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Thomas SA, Goodman KL, Kundey SM. Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology. 2013;9:123–149. doi: 10.1146/annurev-clinpsy-050212-185617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada Y, Lee TK, Huang S, Tapia MI, Velázquez MR, Martinez MJ, … Villamar J. Parent-centered prevention of risky behaviors among Hispanic youths in Florida. American journal of public health. 2017;107(4):607–613. doi: 10.2105/AJPH.2017.303653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. The American journal of clinical nutrition. 2002;76(1):226–231. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franko DL, Thompson D, Bauserman R, Affenito SG, Striegel-Moore RH. What’s Love Got to Do with It? Family Cohesion and Healthy Eating Behaviors in Adolescent Girls. Int J Eat Disord. 2008;41:360–367. doi: 10.1002/eat.20517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George D, Mallery M. SPSS for Windows Step by Step: A Simple Guide and Reference, 17.0 update. 10. Boston: Pearson; 2010. [Google Scholar]
- Gorman-Smith D, Tolan PH, Zelli A, Huesmann LR. The relation of family functioning to violence among inner-city minority youths. Journal of Family Psychology. 1996;10:115–129. doi: 10.1037//0893-3200.10.2.115. [DOI] [Google Scholar]
- Guion K, Mrug S, Windle M. Predictive value of informant discrepancies in reports of parenting: Relations to early adolescents’ adjustment. Journal of abnormal child psychology. 2009;37(1):17–30. doi: 10.1007/s10802-008-9253-5. [DOI] [PubMed] [Google Scholar]
- Haines J, Rifas-Shiman SL, Horton NJ, Kleinman K, Bauer KW, Davison KK, Walton K, Austin SB, Field AE, Gillman MW. Family functioning and quality of parent-adolescent relationship: cross-sectional associations with adolescent weight-related behaviors and weight status. Int J Behav Nutr Phys Act. 2016;13:68. doi: 10.1186/s12966-016-0393-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliday JA, Palma CL, Mellor D, Green J, Renzaho AMN. The relationship between family functioning and child and adolescent overweight and obesity: a systematic review. International journal of obesity. 2014;38(4):480–493. doi: 10.1038/ijo.2013.213. [DOI] [PubMed] [Google Scholar]
- Han Y, Grogan-Kaylor A, Bares C, Ma J, Castillo M, Delva J. Relationship between discordance in parental monitoring and behavioral problems among Chilean adolescents. Children and youth services review. 2012;34(4):783–789. doi: 10.1016/j.childyouth.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper LM, Burnham JJ, Richey R. Select parent and family system correlates of adolescent current weight status: a pilot study. Fam J. 2009;17:14–21. doi: 10.1177/1066480708328460. [DOI] [Google Scholar]
- Hunsley J, Mash EJ. Evidence-based assessment. Annu Rev Clin Psychol. 2007;3:29–51. doi: 10.1146/annurev.clinpsy.3.022806.091419. [DOI] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Hawkins J, … Zaza S. Youth Risk Behavior Surveillance — United States, 2015. MMWR Surveill Summ. 2016;65(6):1–174. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- Kim HH, Viner-Brown SI, Garcia J. Children’s mental health and family functioning in Rhode Island. Pediatrics. 2007;119(Suppl 1):S22–8. doi: 10.1542/peds.2006-2089E. [DOI] [PubMed] [Google Scholar]
- Kitzmann KM, Dalton WT, Buscemi J. Beyond Parenting Practices: Family Context and the Treatment of Pediatric Obesity. Family Relations. 2008;57:13–23. doi: 10.1111/j.1741-3729.2007.00479.x. [DOI] [Google Scholar]
- Korelitz KE, Garber J. Congruence of parents’ and children’s perceptions of parenting: A meta-analysis. Journal of youth and adolescence. 2016;45(10):1973–1995. doi: 10.1007/s10964-016-0524-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird RD, De Los Reyes A. Testing informant discrepancies as predictors of early adolescent psychopathology: Why difference scores cannot tell you what you want to know and how polynomial regression may. Journal of Abnormal Child Psychology. 2013;41(1):1–14. doi: 10.1007/s10802-012-9659-y. [DOI] [PubMed] [Google Scholar]
- Little T. Longitudinal Structural Equation Modeling. Guilford Press; 2013. [Google Scholar]
- Maurizi L, Gershoff ET, Aber JL. Item-level discordance in parent and adolescent reports of parenting behavior and its implications for adolescents’ mental health and relationships with parents. Journal of Youth and Adolescence. 2012;41:1035–1052. doi: 10.1007/s10964-011-9741-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConley RL, Mrug S, Gilliland MJ, Lowry R, Elliott MN, Schuster MA, et al. Mediators of maternal depression and family structure on child BMI: parenting quality and risk factors for child overweight. Obesity. 2011;19:345–352. doi: 10.1038/oby.2010.177. [DOI] [PubMed] [Google Scholar]
- NHANES. 2011–2012 National Health and Nutrition Examination Survey- Physical Activity and Physical Fitness Questionnaire. 2012 Available from https://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/paq.pdf.
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran Deanna, Kit BK, Flegal KM. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohannessian CM, Lerner RM, Lerner JV, von Eye A. Discrepancies in adolescents’ and parents’ perceptions of family functioning and adolescent emotional adjustment. Journal of Early Adolescence. 1995;15:490–516. doi: 10.1177/0272431695015004006. [DOI] [Google Scholar]
- Olvera-Ezzell N, Power TG, Cousins JH. Maternal Socialization of Children’s Eating Habits: Strategies Used by Obese Mexican-American Mothers. Child Development. 1990;61(2):395–400. doi: 10.1111/j.1467-8624. [DOI] [PubMed] [Google Scholar]
- Pantin H. Ecodevelopmental measures of support and conflict for Hispanic youth and families. University of Miami School of Medicine; Miami, FL: 1996. [Google Scholar]
- Pantin H, Coatsworth JD, Feaster DJ, Newman FL, Briones E, Prado G, … Szapocznik J. Familias Unidas: The efficacy of an intervention to promote parental investment in Hispanic immigrant families. Prevention Science. 2003;4(3):189–201. doi: 10.1023/a:1024601906942. [DOI] [PubMed] [Google Scholar]
- Pasch KE, Stigler MH, Perry CL, Komro KA. Parents’ and children’s self-report of parenting factors: How much do they agree and which is more strongly associated with early adolescent alcohol use? Health Education Journal. 2010;69(1):31–42. doi: 10.1177/0017896910363325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prado G, Cordova D, Huang S, Estrada Y, Bacio GA, Leon Jimenez G, et al. The efficacy of Familias Unidas on drug and alcohol use for Hispanic delinquent youth: Main effects and effects by environmental context. Drug and Alcohol Dependence. 2012a;125:S18–S25. doi: 10.1016/j.drugalcdep.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prado G, Pantin H, Briones E, Schwartz SJ, Feaster D, Huang S, … Szapocznik J. A randomized controlled trial of a parent-centered intervention in preventing substance use and HIV risk behaviors in Hispanic adolescents. Journal of consulting and clinical psychology. 2007;75(6):914. doi: 10.1037/0022-006X.75.6.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prado G, Pantin H, Huang S, Cordova D, Tapia M, Velazquez MR, et al. Effects of a family intervention in reducing HIV risk behaviors among high-risk Hispanic adolescents: A randomized controlled trial. Archives of Pediatrics and Adolescent Medicine. 2012b;166:127–133. doi: 10.1001/archpediatrics.2011.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruchno RA. Alzheimer’s disease and families: methodological advances. In: Light E, Lebowitz B, editors. Alzheimer’s disease treatment and family stress: Directions for research. Washington, D.C: NIMH, Government Printing Office; 1989. pp. 174–195. [Google Scholar]
- Renzaho A, Kumanyika S, Tucker K. Family functioning, parental psychological distress, child behavioral problems, socio-economic disadvantage and fruit and vegetable consumption among 4–12 year-old Victorians, Australia. Health Promot Int. 2011;26:263–275. doi: 10.1093/heapro/daq054. [DOI] [PubMed] [Google Scholar]
- Rhee K. Childhood Overweight and the Relationship between Parent Behaviors, Parenting Style, and Family Functioning. American Academy of Political and Social Sciences. 2008;615:12–37. doi: 10.1177/0002716207308400. [DOI] [Google Scholar]
- Santisteban DA, Coatsworth JD, Perez-Vidal A, Kurtines WM, Schwartz SJ, LaPerriere A, Szapocznik J. Efficacy of brief strategic family therapy in modifying Hispanic adolescent behavior problems and substance use. Journal of Family Psychology. 2003;17(1):121–133. doi: 10.1037/0893-3200.17.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ, Mason CA, Pantin H, Szapocznik J. Effects of family functioning and identity confusion on substance use and sexual behavior in Hispanic immigrant early adolescents. Identity. 2008;8:107–124. doi: 10.1080/15283480801938440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118(4):1388–1393. doi: 10.1542/peds.2006-1212. [DOI] [PubMed] [Google Scholar]
- Shishido Y, Latzman RD. Mother-son discrepant reporting on parenting practices: The contribution of temperament and depression. Journal of Family Psychology. 2017;31:398–408. doi: 10.1037/fam0000284. [DOI] [PubMed] [Google Scholar]
- Sleddens EFC, Gerards SMPL, Thijs C, De Vries NK, Kremers SPJ. General parenting, childhood overweight and obesity-inducing behaviors: A review. International Journal of Pediatric Obesity. 2011;6:e12–e27. doi: 10.3109/17477166.2011.566339. [DOI] [PubMed] [Google Scholar]
- Stuart J, Jose PE. The influence of discrepancies between adolescent and parent ratings of family dynamics on the well-being of adolescents. Journal of Family Psychology. 2012;26:858–868. doi: 10.1037/a0030056. [DOI] [PubMed] [Google Scholar]
- Taber SM. The veridicality of children’s reports of parenting: A review of factors contributing to parent–child discrepancies. Clinical Psychology Review. 2010;30(8):999–1010. doi: 10.1016/j.cpr.2010.06.014. [DOI] [PubMed] [Google Scholar]
- Thompson VJ, Baranowski T, Cullen KW, Rittenberry L, Baranowski J, Taylor WC, Nicklas T. Influences on diet and physical activity among middle-class African American 8-to 10-year-old girls at risk of becoming obese. Journal of nutrition education and behavior. 2003;35(3):115–123. doi: 10.1016/s1499-4046(06)60195-4. [DOI] [PubMed] [Google Scholar]
- Tolan PH, Gorman-Smith D, Huesmann LR, Zelli A. Assessment of family relationship characteristics: A measure to explain risk for antisocial behavior and depression among urban youth. Psychological Assessment. 1997;9:212–223. doi: 10.1037/1040-3590.9.3.21. [DOI] [Google Scholar]
- Toro-Morn MI. Familismo. In: Sajatovic SLM, editor. Encyclopedia of Immigrant Health. New York: Springer; 2015. pp. 672–674. [Google Scholar]
- U.S. Census Bureau. 2014 National Population Projections. 2014 Retrieved from http://www.census.gov/population/projections/data/national/2012.html.
- Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, Davies WH. Controlled study of critical parent and family factors in the obesogenic environment. Obesity (Silver Spring) 2007;15(1):126–36. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]
- Zubrick S, Williams A, Silburn S, Vimpani G. Indicators of Social and Family Functioning. Department of Family and Community Services; Canberra, Australia: 2000. [Google Scholar]