Abstract
RATIONALE
Abstinence-based approaches to treating alcohol use disorder (AUD) are highly prevalent, but abstinence from chronic drinking may exacerbate subsequent levels of alcohol intake in relapse.
OBJECTIVE
Use a non-human primate model that encompasses a range of chronic voluntary ethanol drinking to isolate biological responses to repeated cycles of imposed abstinence as a function of baseline voluntary alcohol drinking levels.
METHODS
Over a 26-month protocol, young adult male rhesus macaques were first induced to drink alcohol and then given continuous access to 4% (w/v) ethanol (n=8) or water (n=4) for approximately 14 months, followed by three 28–35 day abstinence phases, with 3 months of ethanol access in between. Ethanol intake and BEC were the primary dependent variables. Observational signs of physical dependence and circulating ACTH and cortisol were monitored.
RESULTS
Prior to abstinence, stable, categorical, individual differences in voluntary ethanol intake under chronic access conditions were found. Following abstinence, categorical “non-heavy” drinking subjects increased drinking transiently (increased between 0.7–1.4 g/kg/day in first month after abstinence), but returned to baseline after three months. Categorical “heavy” drinkers, however maintained drinking 1.0–2.6 g/kg above baseline for over 3 months following abstinence. Signs of physical dependence were rare, although huddling and social withdrawal increased in ethanol and control subjects. The most prominent effect on hormonal measures was heightened cortisol during abstinence that increased to a greater extent in ethanol subjects.
CONCLUSION
Involuntary abstinence increases drinking in the absence of overt physical withdrawal symptoms, and heavy drinkers are more robustly affected compared to non-heavy drinkers.
Keywords: forced abstinence, ethanol, monkey, HPA axis, self-administration, relapse, macaque, cortisol, extinction
Introduction
Alcohol use disorder (AUD) is a chronic, progressive disease that is often characterized by cycles of heavy drinking, remission and relapse (American Psychological Association, 2013). A primary approach to treatment of AUD across all modalities is a period of imposed abstinence, from rehabilitation clinics to outpatient support groups (e.g., alcoholics anonymous). Abstinence is also the benchmark for success in many new clinical trials aimed to develop therapeutics for AUD (Food and Drug Administration, 2006). Despite the prevalence of forced abstinence in therapeutic approaches, data are accumulating that involuntary treatment (i.e., medical, family or court ordered abstinence) results in lower remittance of problem drinking compared to voluntary treatment (Matzger et al., 2005; Witkiewitz and Marlatt, 2006; Delucchi and Kaskuras, 2010).
The probability of relapse following treatment is determined by a complex interaction between internal and external variables that are difficult to disentangle or predict (Marlatt and Gordon, 1985; Larimer et al., 1999). Following alcohol-dependent patients over many years shows that the individual’s choice to enter treatment voluntarily is critical to longer-term success (Polich et al., 1981; Delucchi and Kaskuras, 2010). However, for many AUD patients, achieving abstinence does not necessarily mean successful remission. For example, after short-term abstinence (1–5 months), patients were just as likely to relapse as those that never abstained (Polich et al., 1981). Further, in some cases a month of complete abstinence is immediately followed by a month of no abstinent days (Witkiewitz, 2005). Thus, the efficacy of abstinence-based treatment is questionable, and utilizing animal models can isolate the response to abstinence separate from behavioral therapies and variance in environmental factors (family life, job security, etc.).
Specifically, translational studies in robust animal models have been used to better understand the mechanisms underlying excessive alcohol intake, the role of abstinence, and drinking trajectories post-remittance. Many rodent animal models utilize repeated periods of chronic ethanol exposure interspersed with periods of complete abstinence to increase alcohol self-administration (Becker and Lopez, 2004; Griffin et al., 2009; Anderson et al., 2014). However, the most significant increases in drinking in rodents are reported after involuntary (i.e. passive vapor chamber) ethanol exposure, a period of alcohol withdrawal (1–3 days), followed by very limited ethanol access (<2 hrs). These pre-clinical models initially emphasized an exacerbation of physiological withdrawal symptoms over repeated withdrawal periods, such as handling-induced convulsions (Becker and Hale, 1993; Becker 1998). However, the emphasis in pre-clinical studies on physiological withdrawal symptoms are not well matched to the abstinence syndromes noted in human subjects (Holleran and Winder, 2017), which emphasize psychological features such as negative affect, lower coping and risk of relapse (Witkiewitz, 2005, Witkiewitz and Masyn, 2008). An alternate approach has been using deprivation periods to produce an alcohol deprivation effect (ADE), in which drinking is transiently increased following drug removal (Sinclair and Senter, 1968; Spanagel and Holter, 1999; Sanchis-Segura and Spanagel, 2006). However, the magnitude of the escalation in drinking is modest, though it appears under conditions of brief or extended abstinence (3 to 60 days, Spanagel and Holter, 1999). Additionally, many animal models measure alcohol relapse under extinction conditions in which alcohol is not actually consumed, which is not well-matched in the clinical literature (Hauser et al., 2016). Finally, the common use of inbred rodent strains inherently limits the individual variability in ethanol drinking before abstinence, as well as the behavioral response to alcohol withdrawal.
To address some of these issues, we utilized an monkey model of alcohol self-administration that captures individual differences in voluntarily drinking to excessive levels associated with phenotypic alcoholic intakes (Grant et al., 2008; Baker et al, 2014) prior to imposed abstinence and observed the effects on subsequent alcohol self-administration. This model has helped unravel the biological contribution to individual variability in voluntary daily ethanol drinking (Cervera-Juanes et al., 2016, 2017; Nimitvilai et al., 2017; Pleil et al., 2016; Siciliano et al., 2016a,b), including endocrine measures of stress response as predictors (Helms et al., 2014) and consequences (Jimenez and Grant, 2017; Jimenez et al., 2017a,b) of ethanol self-administration. Thus, the current study sought to characterize the response to repeated cycles of abstinence on voluntary drinking, associated blood ethanol concentrations and HPA activity, due to the translational potential to human studies of abstinence (Sinha et al., 2009).
Materials and methods
Animals
Twelve experimentally-naïve young adult male rhesus macaques (Macaca mullatta; 4.0–5.5 years at assignment) were selected for this study from a pedigreed population at the Oregon National Primate Research Center (Beaverton, OR) and did not have common parents or grandparents. This study was an extension of a previous experiment examining the effect of repeated abstinence in male cynomolgus monkeys (Cuzon Carlson et al., 2011). Since a cohort design was used, this study was populated with only young adult males males to address species differences prior to addressing other important organismal variables such as sex or age. Co-housed controls were also added to the original design that had only experimental subjects. All monkeys were housed individually within the same room, allowing visual, auditory, and olfactory contact with conspecifics. The housing room was maintained at a constant temperature (20–22°C) and humidity (65%) with an 11-hour light/dark cycle (lights on at 7:00AM). Animals were housed in either a single (0.8×0.8×0.8 m) or double (1.6×0.8×0.8 m) wide cage within a quadrant rack, depending on body weight. All monkeys were trained to present their legs through an opening in the front of the cage for awake blood collection and to operate a panel located on a side wall of the housing cage. Each panel was equipped with two drinking spouts, stimulus lights, food pellet receptacle, and a device that measures discrete light beam breaks scheduled for food delivery (further details in Grant et al., 2008; Baker et al., 2014). Fluid reservoirs resting on digital scales (Ohaus Corporation, Parsnippany, NJ) and pellet dispensers were located outside of the housing cage. Fluid was recorded with an accuracy of 0.1ml and 1sec.
After training, animals were assigned to either an ethanol group (n=8) or yoked control group (n=4). The experimental procedures were identical for ethanol and control groups, except that the control group had water available though both spouts. In addition, at the start of the experiment, yoked controls were assigned to a specific ethanol subject. Every morning, each control was given a specific volume of maltodextrin solution (10% w/v in water) calculated weekly to match the average daily calories consumed in the form of ethanol (calories/kg/day) of the assigned ethanol subject over the past week. Maltodextrin volumes were administered in a separate bottle hung on the outside of the cage at the session start. All solutions were made fresh daily.
Ethanol-self administration
All monkeys were induced to drink either ethanol or water using a schedule induced polydipsia (SIP) procedure, which has been described in detail (Grant et al., 2008; Baker et al., 2014, 2017). The key feature of this procedure is that 1-gram banana-flavored food pellets are delivered under a fixed time (FT) schedule (typically FT 300sec) until a specified dose of ethanol is consumed. Induction began with water (volume equivalent to 1.5 g/kg from 4% (w/v) ethanol) and then escalated to 0.5 g/kg, 1.0 g/kg, and 1.5 g/kg ethanol, with each condition given in at least 30 session increments. The induction of water was 56 sessions to allow the adjunctive drinking patterns to stabilize in al individuals prior to ethanol induction. The 1.5 g/kg induction was 67 sessions to allow for an extensive examination of adrenal hormonal response (Jimenez et al. 2017a). Control monkeys were induced to drink an equivalent volume of water in each phase of the schedule induction procedure. At the end of induction (183 consecutive sessions, Table 1), the FT pellet delivery was discontinued, both ethanol and water spouts were operative for 22 hours/day, and, the total daily food allotment available as three meals at 0, 2, and 4 hours into the self-administration session. All monkeys were weighed weekly without sedation to calculate g/kg ethanol intakes.
Table 1.
Behavioral ethogram
| Behavior | Description |
|---|---|
| Signs of physical alcohol dependence | |
| Piloerection | Raised body hair |
| Intentional Tremor | Spontaneous shake of hand when reaching or extending arm |
| Tremor | Spontaneous shake of any body part |
| Vomiting | Any vomiting or gagging |
|
| |
| Huddling/Social withdrawal | |
| Huddling | Hugging self with head between knees |
| Social withdrawal | Sitting at back of cage, unresponsive to any cage noise or objects being moved by other monkeys in the room |
|
| |
| Normal (or species-typical) behaviors | |
| Cage exploration | Tactile or oral exploration of their environment |
| Dowel pull | Pulling the dowel at the center of the panel |
| Left spout | Drinking from the left spout |
| Right spout | Drinking from the right spout |
| Masturbation | Tactile contact with genitals |
| Self-grooming | Picking, scraping, or spreading of animal’s own hair |
| Vocalizing | Any vocalization originating in the throat, most commonly cooing and grunting |
Abstinence
After 425 sessions of daily access to ethanol (~14 months), the first abstinence phase began (Table 1). All independent variables remained constant except the ethanol bottle was replaced with a second water bottle. Yoked controls no longer received daily maltodextrin during the abstinence phase. Abstinence 1 lasted for a total of 35 days (sessions 426–460), which included an additional week for magnetic resonance imaging (MRI) as part of a larger study. Days 1–28 were used in data analysis, and MRIs were conducted over days 29–35. On session 461, the ethanol bottle was replaced for ~3 months and yoked maltodextrin was reinstated. Abstinence 2 was 28 days in total, and Abstinence 3 was 35 days (28 days of abstinence, with MRIs on days 29–35). These abstinence periods were otherwise identical to abstinence 1, with a final ethanol access phase between them (Table 1). The final ethanol access phase was also extended due to MRI imaging on days 63–74 post-abstinence 2 (Table 1).
Behavioral observations
Live behavioral observations were conducted by trained staff as previously reported (Cuzon Carlson et al., 2011). Pre-abstinence observations occurred typically 3–5 days before abstinence, following 2 baseline sessions to habituate subjects to the observers. All observers were involved in animal husbandry and familiar to the subjects. Abstinence observations (Abstinence 1–3) took place 1–3 days after ethanol was removed at 8AM and 4PM (time points: 24hr, 32hr, 48hr, 56hr, and 72hr post-ethanol). Time of day was matched in the Pre-abstinence observations for 3 morning observations and 2 evening observations in each experimental phase. Morning and afternoon observation sessions were conducted to capture spontaneous behavior before and after daily meals (daily 22-hour sessions ran from 10AM–8AM).
Prior to observations, training video recordings were used to establish consistent criteria based on the ethogram (Table 2; adapted from Cuzon Carlson et al., 2011 and Ruedi-Bettschen et al., 2012). Each monkey was observed for a total of 20 minutes, the first 10 minutes by one observer, and the second 10 minutes by a second observer. Six observers were present for approximately 45 minutes (4 monkeys/observer, 12 monkeys). The order of the observations was rotated and counterbalanced. All behaviors were recorded on a binary scale (0 = did not occur, 1 = did occur) to weight each behavior equally and minimize the between-rater variability. Behaviors within three categories (physical signs of dependence, huddling/social withdrawal, and normal behaviors; Table 2) were summed for each monkey by observation session (i.e., 24 hours abstinence) and then by Pre-abstinence or Abstinence period. This approach increased statistical power with the small number of subjects and extensive ethogram.
Table 2.
Behavioral observations during alcohol abstinence.
| Number of observed behaviors collapsed across experimental phase and group (Mean±SD)
| ||||||
|---|---|---|---|---|---|---|
| Signs of physical alcohol dependence (max score = 40) | Pre-abs 1 | Abs 1 | Pre-abs 2 | Abs 2 | Pre-abs 3 | Abs 3 |
| Control (n=4) | 0.0±0.0 | 0.8±1.0 | 0.8±0.5 | 0.3±0.5 | 0.3±0.5 | 0.3±0.5 |
| Non-heavy drinkers (n=5) | 0.0±0.0 | 0.0±0.0 | 0.2±0.4 | 0.2±0.4 | 0.4±0.9 | 0.6±0.9 |
| Heavy drinkers (n=3) | 0.0±0.0 | 0.0±0.0 | 0.3±0.6 | 0.0±0.0 | 0.7±0.6 | 0.7±0.6 |
|
| ||||||
| All subjects (n=12) | 0.0±0.0 | 0.3±0.4 | 0.4±0.3 | 0.2±0.1 | 0.4±0.2 | 0.5±0.2 |
|
| ||||||
| Huddling/Social withdrawal (max score = 20) | Pre-abs 1 | Abs 1 | Pre-abs 2 | Abs 2 | Pre-abs 3 | Abs 3 |
|
| ||||||
| Control (n=4) | 1.0±1.2 | 3.5±2.5 | 3.3±2.1 | 3.8±4.2 | 3.8±1.3 | 5.2±2.6 |
| Non-heavy drinkers (n=5) | 0.6±0.9 | 4.4±1.1 | 4.8±2.8 | 4.6±2.9 | 2.0±2.6 | 5.8±3.0 |
| Heavy drinkers (n=3) | 0.0±0.0 | 3.7±3.6 | 2.3±2.5 | 4.0±1.7 | 1.0±0.0 | 4.3±0.6 |
|
| ||||||
| All subjects (n=12) | 0.5±0.5 | 3.9±0.5*** | 3.5±1.2 | 4.1±0.4 | 2.3±1.4 | 5.1±0.7*** |
|
| ||||||
| Normal (or species-typical) behaviors (max score = 80) | Pre-abs 1 | Abs 1 | Pre-abs 2 | Abs 2 | Pre-abs 3 | Abs 3 |
|
| ||||||
| Control (n=4) | 41.3±13.4 | 36.8±5.9 | 33.3±2.6 | 33.3±9.9 | 34.3±10.0 | 32.5±9.7 |
| Non-heavy drinkers (n=5) | 40.0±6.9 | 31.4±8.2 | 35.0±5.0 | 31.8±6.8 | 39.6±10.2 | 27.4±6.3## |
| Heavy drinkers (n=3) | 34.7±7.0 | 39.7±5.5 | 31.3±13.1 | 34.7±11.0 | 38.7±11.0 | 29.7±10.7# |
|
| ||||||
| All subjects (n=12) | 38.6±3.5 | 35.9±4.2 | 33.2±1.8 | 33.2±1.4 | 37.5±2.9 | 29.9±2.6*** |
p<0.001, indicating a significant difference between abstinence and the preceding Pre-abstinence measure.
p<0.05;
p<0.01, indicating a significant difference compared to controls during abstinence
Blood sampling
All blood samples for hormone analysis (3ml) were collected from the femoral vein during routine weekly morning blood draws (7-9AM) from the home cage without sedation. Samples were kept on ice until centrifuged (15min, 5°C, 3000rpm) and then stored at −80°C until assayed on an automatic Roche platform by the Endocrine Core at Oregon National Primate Research Center (Beaverton, OR).
Blood samples for blood ethanol concentration (BEC) analysis (20μl) were collected 7 hours into the drinking session from the medial saphenous vein and diluted in 500μl sterile water, placed in airtight containers and stored at −4°C until assayed using headspace gas chromatography (Agilent Technologies, Santa Clara, CA). Samples were analyzed using linear regression against a standard curve that included 25, 50, 100, 200, and 400 mg/dl.
Drinking categories
Drinking categories for each ethanol monkey were established using drinking and BEC data from the first 22-hour open access period (425 sessions, Table 1), as previously described (Grant et al., 2008; Baker et al., 2014). Very Heavy Drinkers (VHD) have a daily ethanol intake average ≥ 3 g/kg, with ≥ 10% of drinking days exceeding 4 g/kg. Heavy Drinkers (HD) are monkeys that reach 3 g/kg for ≥ 20% of open access days. Binge Drinkers (BD) have ethanol intakes of ≥2 g/kg for ≥ 55% of drinking days, and have a BEC ≥ 80mg/dl at least once per year. Low Drinkers (LD) are all monkeys that do not meet the criteria for any of the previous categories (Baker et al., 2014).
Data analysis
All analyses were conducted using GraphPad Prism 6. Drinking data were collapsed into Non-heavy (Low and Binge drinkers) and Heavy (Heavy and Very Heavy drinkers) groups for all analyses (Baker et al., 2017). Drinking and BEC data were confirmed for normality and then entered into a one-way repeated measures ANOVA with experimental phase as the independent variable. To emphasize the transitory nature of drinking post-abstinence, we analyzed 28 sessions immediately prior to abstinence (Pre-abstinence), the first 28 sessions after abstinence ended (days 1–28), and the final 28 sessions of the open access period (Post abstinence 1: days 56–84; Post-abstinence 2: days 76–104). Post-hoc comparisons were made using Dunnett’s test. For intakes under extinction conditions (Figure 3), the first 28-sesssions of abstinence were used in paired t-tests within each abstinence phase, excluding days 29–35 in Abstinence 1 and 3 when MRIs were occurring.
Fig. 3.
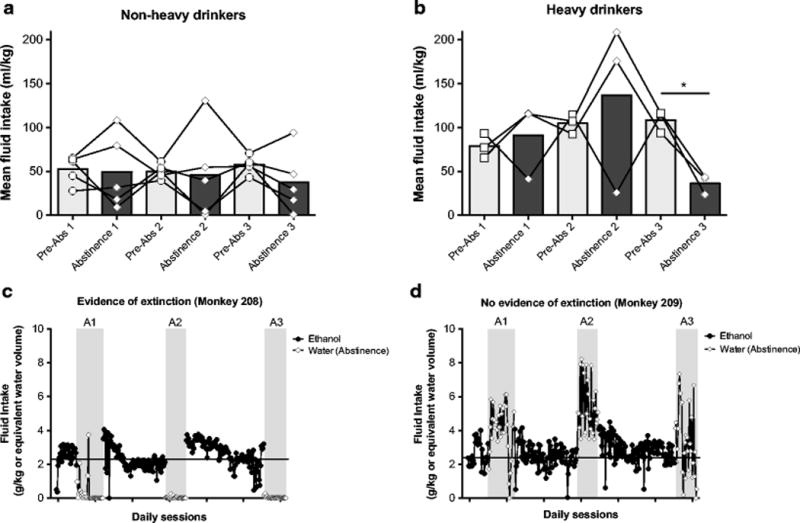
Water intake on ethanol spout during abstinence. a,b) Total fluid intake (ml/kg) before (Pre-abstinence) and during abstinence for each of the three abstinence periods for a) non-heavy and b) heavy drinkers. Each data point represents a 28-day mean for each monkey and the bars represent a group mean ± SEM. Asterisks represent significant changes from pre-abstinence (Pre-abs), *p<0.05. c,d) Representative drinking patterns are shown for two monkeys: one that had evidence of extinction during abstinence (c, Monkey 209) and another that had no evidence of extinction (d, Monkey 208). Solid horizontal lines in both panels represent each monkey’s 12-month average ethanol intake prior to abstinence.
Behavioral observations were confirmed for normality and then analyzed as separate two-way repeated measures ANOVAs for each abstinence period (Abstinence 1, 2 and 3) with group (Heavy drinkers, Non-heavy drinkers, Controls) and experimental phase (Pre-abstinence and Abstinence) as factors within each category. Post-hoc comparisons were made with the control group as appropriate (Sidak’s).
For ACTH and cortisol analyses, blood samples were taken 3 days before abstinence (Pre-abstinence), 24 hours into abstinence, 21–22 days into abstinence, and within one week of ethanol being reintroduced (Post-abstinence) (Figure 5A–B). There are no post-abstinence samples for Abstinence 3 since the experiment had ended (Table 1). All samples were log transformed for normality and then analyzed as a two-way repeated measures ANOVA with group (Heavy, Non-heavy, and Control) and experimental phase as factors within each abstinence (Abstinence 1–3). Post-hoc comparisons were made with Pre-abstinence or the control group (Sidak’s).
Results
Baseline ethanol drinking
Prior to the first abstinence, individual daily ethanol intakes (g/kg/day) were measured during the first open access period (425 consecutive sessions), and 66–70 blood samples/monkey were taken over this period for BEC analysis. These data were used to assign each monkey to a drinking category (see Methods). There were 2 VHD, 1 HD, 3 BD, and 2 LD (Figure 1). To accommodate statistical analysis, the four categories were collapsed into two: Heavy (VHD and HD) and Non-heavy (BD and LD), consistent with previous publications (Beattie et al., 2015; Baker et al., 2014, 2017; Cervera-Juanes et al., 2016a, 2016b, 2017). The summary drinking and BEC data are shown in Figure 1A and 1B respectively. Figure 1C depicts the percent of total drinking days at each categorical drinking level.
Fig. 1.
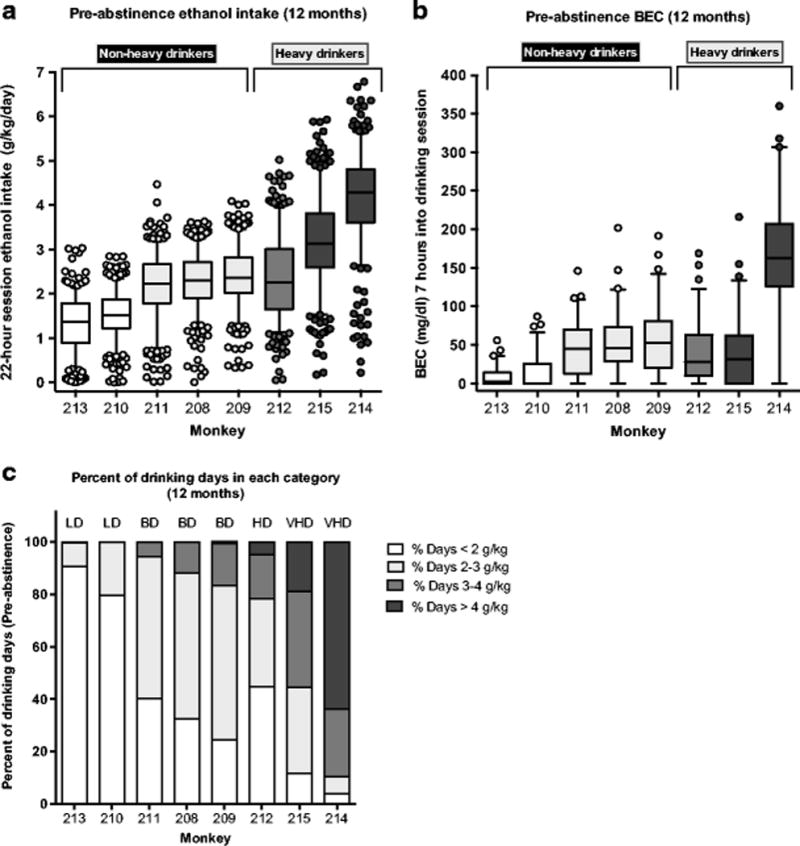
Boxplots of ethanol intake and BEC during the 12 months before abstinence. a) Boxplot of 425 sessions prior to abstinence for each monkey colored by drinking category (each plot includes between 410–415 drinking sessions excluding days where sedation occurred or there was a computer/technical error in data collection). b) Boxplot of 66–70 blood samples assayed for BEC over 425 sessions before abstinence. Whiskers in both graphs represent 5–95% of sessions/samples, with the outliers as individual data points. The monkeys that were collapsed into Non-heavy and Heavy categories are indicated above the graphs. Low drinkers (LD) are in white, Binge drinkers (BD) are in light gray, Heavy drinkers (HD) are in dark gray, and Very heavy drinkers (VHD) are in black. c) Percentage of drinking sessions at each categorical drinking level for each monkey, as indicated by color (legend at right).
Effect of abstinence on ethanol drinking and blood ethanol concentrations
To determine the effect of abstinence on subsequent ethanol drinking and BEC, 28-day epochs before and after each abstinence phase were analyzed in heavy and non-heavy drinkers (timeline in Figure 2A). Pre-abstinence drinking (28 days) was not different from the 12-month averages, demonstrating the stability of each monkey’s drinking category prior to abstinence (p>0.05, Figure 2B,C). Overall, both abstinence 1 and abstinence 2 initially increased drinking in both non-heavy and heavy drinkers (Figure 2B,C; Main effect of abstinence, Non-heavy: F(4,16)=14.19, p<0.0001; Heavy: F(4,8)=47.87, p<0.0001). In non-heavy drinkers, this effect is only observed in early post-abstinence (Figure 2C; Post-abs 1 (days 1–28): p<0.05; Post-abs 2 (days 1–28): p<0.001). Drinking returned to pre-abstinence levels at the end of the post-abstinence ethanol access periods (days 56–84 (Abs 1) and 76–104 (Abs 2): p>0.05). Heavy drinkers, however, had elevated drinking that remained elevated over the entire post-abstinence ethanol access (Figure 2B; Post-abs 1 (days 1–28): p<0.001; Post-abs 1 (days 56–84): p<0.01; Post-abs 2 (days 1–28): p<0.001; Post-abs 2 (days 76–104): p<0.01). Water intake was not different between heavy and non-heavy drinkers, and was unchanged following abstinence (Figure 2F). Additionally, there was no effect of abstinence on water intake in the control group (Figure 2G).
Fig. 2.
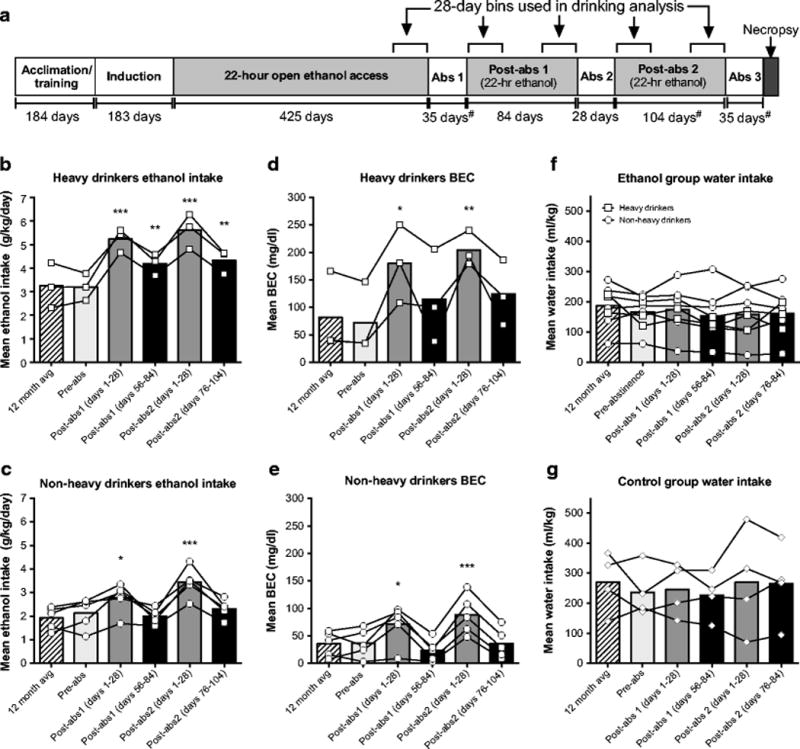
Effect of abstinence on ethanol intake and blood ethanol concentration (BEC) in heavy and non-heavy drinkers. a) Experimental timeline. The number of days of each phase of the experiment is indicated below each section. Additionally, the 28-day epochs used in current analysis are highlighted. #Hash symbol indicates that these periods were extended to allow for MRI brain imaging. MRIs took place on days 29–35 in Abstinence 1 and 3, and on days 63–74 in the final ethanol open access period, and these days were excluded from the analysis. b,c) Ethanol intake in heavy (b; n=3) and non-heavy drinkers (c; n=5) before and after each abstinence period. The post-abstinence period is separated into two phases: the first 28-days following abstinence (Post-abs days 1–28) and the last 28-days of the open access period (Post-abs days 56–84 (Abs 1) and 76–104 (Abs 2)). Each data point represents a 28-day mean for each monkey and the bars represent a group mean ± SEM. d,e) BEC in d) heavy and e) non-heavy drinkers before and after abstinence (Pre-abs, Early Post-abs, and Late Post-abs). Each data point represents a mean of 4–6 samples per monkey collected 7 hours into the drinking session. f) Water intake before and after abstinence for heavy and non-heavy drinkers. g) Total water intake (ml/kg) for control subjects (n=4) from both spouts before and after each abstinence. Asterisks represent significant changes from pre-abstinence (Pre-abs), *p<0.05; **p<0.01, ***p<0.001.
In general the effect of abstinence on BEC reflected the ethanol intake results. Both abstinence periods increased BEC in non-heavy and heavy drinkers (Figure 2D,E; Main effect of abstinence, Non-heavy: F(4,16)=14.54, p<0.0001; Heavy: F(4,8)=7.985, p<0.01). In non-heavy drinkers, this effect is observed in the first 28 days following abstinence (Figure 2E; Post-abs 1 (days 1–28): p<0.05; Post-abs 2 (days 1–28): p<0.001), while BECs in the last month of ethanol access returned to pre-abstinence levels. A similar effect is found with the heavy drinkers, where the average BEC is only statistically increased in the early post-abstinence period (Figure 2D; Post-abs 1 (days 1–28): p<0.05; Post-abs 2 (days 1–28): p<0.01).
Extinction conditions: Water drinking on ethanol spout during abstinence
Extinction conditions were imposed on the ethanol animals during the abstinence periods such that ethanol was removed from its vehicle (i.e., water), therefore both spouts supplied only water. Intake (ml/kg) on the former ethanol spout during the 28-day abstinence was compared to ethanol intake (ml/kg) 28 days prior to water substitution (Figure 3). As a group, non-heavy drinkers did not significantly decrease intake on the ethanol spout during any of the abstinence periods (Figure 3A; p>0.05), and individually, only 2 monkeys showed any evidence of extinction (Figure 3A). Heavy drinkers as a group showed significant decrease on the ethanol spout only in the third abstinence phase (t(2)=6.39, p<0.05), but one subject significantly decreased drinking on the ethanol spout during all three abstinences. Representative graphs of different drinking patterns during abstinence are shown in Figure 3C–D. There were no changes in drinking on the previous water spout in either ethanol drinking group (Figure S2A).
Control subjects did not demonstrate any extinction on either water spout during abstinence (Figure S2B–C). However, during the first abstinence, control monkeys increased their water intake on the ‘ethanol’ spout (Figure S2B). These monkeys no longer received maltodextrin on the outside of their cage, and this increased water intake may correspond to the loss of additional fluid each morning.
Behavioral observations
Behavioral observations took place immediately prior to abstinence (Pre-abstinence) and during abstinence. There was a near absence of any physical signs of alcohol dependence (Table 2; tremor, intentional tremor, piloerection, or vomiting) during any observation period (Figure 4A). The main observation was an increase in huddling/social withdrawal during both abstinence 1 (F(1,9)=24.56, p<0.001) and abstinence 3 (F(1,9)=10.64, p<0.01), but not abstinence 2 (p>0.3) (Figure 4B). There was no effect of group on huddling/social withdrawal in any of the abstinence periods (p>0.3), indicating that this effect is not specific to ethanol subjects (Figure 4B).
Fig. 4.
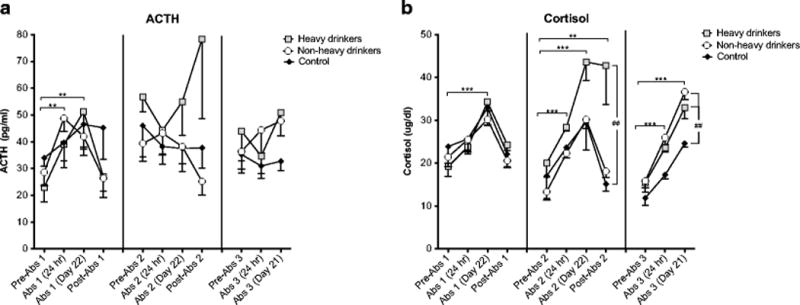
Pituitary and adrenal hormone response to repeated abstinence during morning blood draws. a) ACTH and b) cortisol before abstinence (Pre-abs), 24 hours into abstinence, 21–22 days into abstinence, and within 1 week of resumed ethanol access (Post-abs). Each of these time points was matched for all abstinence phases (Abstinence 1–3). All data are presented as mean ± SEM. Asterisks indicate a significant change from Pre-abstinence. *p<0.05; **p<0.01; ***p<0.001. Hashes represent a significant group difference compared to the control group; ##p<0.01.
Normal, or species-typical, behaviors (Table 2) appeared stable across pre-abstinence and abstinence periods (Figure 4C), except for a decrease in normal behaviors during abstinence 3 (F(1,9)=25.69, p<0.001). A significant group interaction (F(2,9)=4.73, p<0.05), indicated that only the ethanol subjects decreased normal behaviors during abstinence 3 (Heavy drinkers: p<0.05; Non-heavy drinkers: p<0.01) (Figure 4C).
Hormonal response to repeated abstinence
In general, ACTH and cortisol were differentially responsive to ethanol consumption and abstinence (Figure 5). Specifically, ACTH was altered during abstinence 1 in all subjects (F(3,27)=9.82, p<0.001) with a significant increase at 24 hours into abstinence (Abstinence 1 (24 hr): p<0.01) that persisted through day 21 (p<0.01; Figure 5B). However, when ethanol was reintroduced, ACTH returned to pre-abstinence levels (Post-abstinence 1: p>0.05). This effect is driven primarily by the ethanol group, though only a trend level interaction was found so no post-hoc comparisons were made (F(6,27)=2.27, p=0.066). During abstinence 2, there was an interaction between group and phase (F(6,27)=3.818, p<0.01), but post-hoc tests between ethanol and control groups were not significant (p>0.05).
Cortisol, however, was highly reactive to abstinence throughout all three abstinence phases (Figure 5B; (Abstinence 1: F(3,27)=16.42, p<0.0001; Abstinence 2: F(3,27)=28.16, p<0.0001; Abstinence 3: F(2,18)=97.09, p<0.0001). During each abstinence phase a similar pattern was found: cortisol increased at 24 hours of abstinence, continued to rise in week 3, and then fell post-abstinence. However, over repeated abstinence cycles, morning cortisol patterns begin to diverge between ethanol and control groups, particularly in heavy drinkers. Specifically, during abstinence 1, the three groups are tightly matched (p=0.89). In abstinence 2, there is an interaction between experimental group and abstinence (F(6,27)=3.32, p<0.05). During the second abstinence, control monkeys and non-heavy drinkers remain matched, but heavy drinkers have higher cortisol (p<0.001). In abstinence 3, cortisol rose in all groups (F(2,18)=97.09, p<0.0001), and was significantly higher than pre-abstinence cortisol at both 24 hour (p<0.001), and 21–22 days (p<0.001) into abstinence. Additionally, there was a group difference (F(2,9)=8.45, p<0.01), such that heavy drinkers (p<0.05) and non-heavy drinkers (p<0.01) had higher cortisol during abstinence compared to controls.
Discussion
The examination of repeated cycles of abstinence on drinking and stress hormones in this study represents an extension of previous work from our laboratory establishing a nonhuman primate model of chronic ethanol self-administration (Grant et al., 2008). Over replicate cohorts, the individual differences in daily ethanol intakes in our monkey population represent statistically-defined, stable categories of ethanol drinking phenotypes under continuous access conditions of 22 hours/day (Grant et al., 2008; Baker et al., 2014, 2017). These studies have reliably and repeatedly produced cohorts of monkeys with a predictable range of drinking (Baker et al., 2014; 2017), including the present cohort with a consistent distribution of heavy and non-heavy drinkers. Average ethanol intakes in this cohort range from 1.3 to 4.2 g/kg/day, which are approximately equivalent to 5–17 drinks/day in humans. This range extends from binge drinking to clinically problematic drinking, which averages approximately 15 drinks per day (Kwako et al., 2014). The between-subject variance prior to abstinence represents a critical strength of the current study, allowing us to examine the effects of prolonged, repeated cycles of abstinence on both non-heavy and heavy drinkers within the same experiment.
The most prominent effect of abstinence was the robust increase in ethanol intake and BEC in the 28 days following abstinence (Figure 2B–C). The increase in ethanol intake resulted in 6 out of 8 monkeys having mean BECs consistently above 80 mg/dl, compared to only one monkey at this mean level before abstinence (Figure 2C). The final post-abstinence drinking phase resulted in a range of mean BECs from 48 – 240 mg/dl. Human data show BECs from 50 mg/dl to over 150 mg/dl are associated with impairments in memory, attention and motor coordination, increasing the risk of injury to self and others up to and including severe impairments in judgment, amnesia (blackouts) and loss of consciousness (National Institute on Alcohol Abuse and Alcoholism, 2015). Thus, the increased mean BECs seen here and documented over the first 28-day period following abstinence are highly relevant. A similar self-administration protocol in cynomolgus monkeys also found that repeated abstinence resulted in higher BECs in relapse (Cuzon Carlson et al., 2011). Under a different protocol and laboratory, 8 male rhesus monkeys were provided prolonged (i.e., over 1 year) concurrent access to 16% or 32% (v/v) ethanol and water (Kornet et al., 1990). In this study, short alcohol deprivation periods (1, 2 and 7 days) increased post-abstinent ethanol intake proportional to the number of days abstinent. Overall, macaque monkeys robustly display individual differences in voluntary ethanol intakes, and the present study also demonstrates increased alcohol drinking following abstinence. Importantly, however, the effect of repeated abstinence on drinking has not yet been characterized in female macaques, indicating a critical future direction for these findings.
In contrast to the few reports in non-human primates, rodent models have a long history of investigating repeated alcohol deprivations (i.e., alcohol deprivation effect, ADE) following chronic daily drinking (Sinclair and Senter 1968; Spanagel and Holter, 1999; Spanagel 2000). In general, ADE is classically associated with a transient increase in ethanol intake that slowly recovers over up to 4 weeks of resumed ethanol access (Spanagel and Holter, 1999), which is notably similar to the effect observed here. However, ADE using rodent models has not been applied to between-subjects variability in drinking. The current data with macaques suggest that an alcohol deprivation effect is prominent following abstinence across all drinking levels, including low-to-moderate drinkers. While the initial increase in drinking eventually resolves in most subjects, the heaviest drinkers demonstrated sustained (over 3 months) increases in ethanol intake and resultant BECs that rose after each subsequent abstinence (Figure 2). The heavy drinkers all had average BECs exceeding 100 mg/dl in the one month after abstinence 1, and exceeding 175 mg/dl following abstinence 2. This sustained effect of abstinence on heavy drinkers indicates a marked divergence from the traditional ADE effect and was not found in non-heavy drinkers. The differential sensitivity to increased drinking following repeated involuntary abstinence between heavy and non-heavy drinkers provides additional validation of the drinking categories developed using our macaque model (Baker et al., 2014; Cervera-Juanes et al., 2016a,b).
The sustained escalation of ethanol intake post-abstinence in heavy drinkers resembles rodent alcohol dependence models of involuntary ethanol exposure, such as CIE (chronic intermittent ethanol). In this design, alcohol dependence is experimentally induced through passive ethanol exposure via inhalation chambers to maintain blood ethanol concentrations above 250mg% for 24–72 hours (Becker 1998; Becker and Lopez, 2004). This procedure can produce elevations in self-administration 72 hours after removal from the inhalation chambers (Becker and Lopez, 2004; Griffin et al., 2009). Importantly, the current protocol of self-administration in macaques demonstrates a similar robust escalation in drinking, induced exclusively through voluntary ethanol intake. In addition, there are minimal overt signs of physical dependence in this model, which deviates from the rodent dependence studies. These data provide a translational link between rodent models of alcohol dependence that emphasize physical dependence and studies of AUD in humans that emphasize signs of negative affect during abstinence (Holleran and Winder, 2017). A primary emphasis of the macaque model is the self-selection into heavy and non-heavy categorical drinking emerging from a heterogeneous population that reflects human populations of moderate to heavy drinkers.
Interestingly, there was minimal evidence of extinction across the first two abstinence phases, based on similar (or greater) average fluid intakes through the ethanol spout before and during abstinence. In abstinence 3, water intake on the ethanol spout decreased selectively in heavy drinkers, suggesting that extinction was learned in this group by the third abstinence cycle (Figure 3B). The initial resistance to extinction is consistent with the development of inflexible (or habitual) behavior over the course of prolonged ethanol intake. There is evidence that chronic ethanol drinking produces a shift from flexible, easily adjusted behavior to habitual highly patterned behavior that is less modifiable in response to changes in reinforcement contingencies (Gerdeman et al., 2003; Everitt and Robbins, 2005; Corbit et al., 2012; O’Tousa and Grahame, 2014). In addition, research in baboons has shown that alcohol-associated cues can maintain responding at levels above cues associated with other reinforcers (i.e., Tang solution) and this behavior is highly resistant to change (Holtyn et al., 2014). Thus, the prolonged daily ethanol paired with the complex cues in the home cage associated with ethanol availability likely contributed to the resistance to extinction reported here. Resistance to extinction in abstinence may be mediated by synaptic changes within the striatum to favor habitual, inflexible behavior (Yin et al., 2007; Cuzon Carlson et al., 2011). Specifically, chronic ethanol and abstinence in monkeys is associated with increased synaptic firing within the putamen (rodent dorsolateral striatum) but not the caudate (rodent dorsomedial striatum), representing a shift toward habitual striatal circuitry (Cuzon Carlson et al., 2011). Thus, resistance to extinction may reflect the state of the primate brain once ethanol is made available (e.g., relapse conditions) that leads to a rapid return to excessive ethanol consumption.
Signs of overt physical dependence were minimal in this cohort, similar to a previous report on the absence of withdrawal signs in rhesus monkeys given over 1 year ethanol access (Kornet et al., 1990, 1991). The most notable change in behavior was an increase huddling and social withdrawal, which were also seen in control subjects. These data suggest that the conditions of co-housing ethanol and control subjects were not optimal for detecting changes in behavior due specifically to ethanol abstinence. Recent work in mice has demonstrated transfer of alcohol withdrawal states between experimental and control groups within the same housing environment (Smith et al., 2016). Additionally, control subjects had their daily yoked-ration of highly palatable maltodextrin removed during abstinence, and this removal of a valued commodity may have contributed to the control monkeys also showing increased huddling/social withdrawal in the abstinence periods (Lemolo et al., 2012).
Lastly, the effects of abstinence on circulating ACTH and cortisol were variable and wide-ranging in both drinkers and controls. Overall, ACTH was more variable compared to cortisol, and ACTH levels were not consistently related to the experimental phases. In general, these data support a common finding of dissociation between ACTH and cortisol over chronic ethanol drinking in the macaque model (Helms et al., 2012; Helms et al., 2014). The results are also consistent with clinical alcohol-dependent populations that have elevated cortisol during acute abstinence from ethanol (Iranmanesh et al., 1989; Adinoff et al., 1991, 2003), as well previous work in cynomolgus monkeys (Cuzon Carlson et al., 2011). In alcohol-dependent patients, cortisol often falls from acute to protracted abstinence (Adinoff et al., 2003). However, other studies demonstrated that abstinent AUD patients maintain higher basal cortisol relative to controls a month after their last drink, even if some recovery within subjects is observed (Sinha et al., 2009), consistent with the elevation in cortisol levels across the course of 28 days of abstinence seen here in the monkey. Interestingly, the cortisol response of the control monkeys tightly match the ethanol subjects during the first abstinence, perhaps due to heightened stress though the entire housing room that extends beyond ethanol subjects alone (Smith et al., 2016). However, by the third experience of abstinence, ethanol monkeys continue to show heightened cortisol response during abstinence in contrast to controls. This group difference is primarily due to ethanol monkeys showing a nearly doubled range of morning cortisol levels between ethanol access periods and abstinence. These findings indicate that repeated abstinence periods with interspersed daily alcohol drinking may be necessary to show ethanol-specific activation of the HPA axis and circulating cortisol as opposed to stress due to the loss of any important commodity. This finding as implications for the clinical literature because nearly all AUD patients have undergone several relapse cycles throughout the course of their disease progression superimposed upon multiple commodity losses (e.g., employment, significant relationships, health) as a consequence of their alcohol drinking.
In conclusion, we have presented data from heterogeneous sample of male rhesus monkeys demonstrating that repeated 28–35 day abstinences following daily access to ethanol for over one year produced consistently elevated drinking in all monkeys, independent of intake level before abstinence. Importantly, abstinence did not result in a decrease in drinking in any subject, a result that is consistent with longitudinal analysis of human AUD patients (over 11 years) indicating that involuntary abstinence was a consistent predictor of increased drinking (Delucchi and Kaskuras, 2010). Further, significant changes in drinking were present despite the absence of spontaneous signs of physical alcohol dependence. Lastly, morning cortisol did not differentiate drinkers from control subject until the third abstinence experience, highlighting the importance of repeated abstinences in animal models of AUD. In conclusion, these data provide evidence that abstinence, as a target for treatment, can exacerbate reinstated drinking particularly in the heaviest drinking subjects. Instead, treatment approaches that emphasize harm reduction rather than complete abstinence may improve treatment outcomes and decrease risk of relapse behavior.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Andrew Woodall, Molly McGinnis, and Devin Owen who provided essential technical assistance in carrying out these experiments. These studies were funded by grants from the US National Institutes of Health F31 AA024660, AA019431, AA013641 and U01 AA013510.
Footnotes
Authors contribution
K.A.G designed the experiment. D.C.A. conducted the experiment and analyzed the data. S.W.G conducted preliminary data processing and analysis. D.C.A and K.A.G. wrote the paper. All authors critically reviewed the paper and approved the final version for publication.
Supplementary Figure Legends
Figure S1. Water intake (ml/kg) during abstinence. A,B) Water intake on the ‘water’ spout (i.e., spout that was never associated with ethanol) in A) non-heavy and B) heavy drinkers before (Pre-abs) and during abstinence. C) Water intake in control subjects on the ‘ethanol’ spout (i.e., spout associated with the schedule induction procedure) before and during abstinence. D) Water intake in control subjects on the ‘water’ spout (i.e., spout that was not associated with the schedule induction procedure) before and during abstinence. Each data point represents a 28-day mean for each monkey and the bars represent a group mean ± SD. Asterisks represent significant changes from pre-abstinence (Pre-abs), *p<0.05; **p<0.01.
References
- Adinoff B, Risher-Flowers D, De Jong J, Ravitz B, Bone GH, Nutt DJ, Roehrich L, Martin PR, Linnoila M. Disturbances of hypothalamic-pituitary-adrenal axis functioning during ethanol withdrawal in six men. Am J Psychiatry. 1991;148:1023–1025. doi: 10.1176/ajp.148.8.1023. [DOI] [PubMed] [Google Scholar]
- Adinoff B, Ruether K, Krebaum S, Iranmanesh A, Williams MJ. Increased salivary cortisol concentrations during chronic alcohol intoxication in a naturalistic clinical sample of men. Alcohol Clin Exp Res. 2003;27:1420–1427. doi: 10.1097/01.ALC.0000087581.13912.64. [DOI] [PubMed] [Google Scholar]
- American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. American Psychiatric Association; Washington DC: 2013. p. 493. [Google Scholar]
- Anderson RI, Lopez MF, Becker HC. Forced swim stress increases ethanol consumption in C57BL/6J mice with a history of chronic intermittent ethanol exposure. Psychopharmacology (Berl) 2016;233:2035–2043. doi: 10.1007/s00213-016-4257-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker EJ, Farro J, Gonzales S, Helms C, Grant KA. Chronic alcohol self-administration in monkeys shows long-term quantity/frequency categorical stability. Alcohol Clin Exp Res. 2014;38:2835–2843. doi: 10.1111/acer.12547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker EJ, Walter NA, Salo A, Rivas Perea P, Moore S, Gonzales S, Grant KA. Identifying future drinkers: Behavioral analysis of monkeys initiating drinking to intoxication is predictive of future drinking classification. Alcohol Clin Exp Res. 2017 doi: 10.1111/acer.13327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beattie MC, Maldonado-Devincci AM, Porcu P, O’Buckley TK, Daunais JB, Grant KA, Morrow AL. Voluntary ethanol consumption reduces GABAergic neuroactive steroid (3α,5α)3-hydroxypregnan-20-one (3α,5α-THP) in the amygdala of the cynomolgus monkey. Addict Biol. 2015 doi: 10.1111/adb.12326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker HC. Kindling in alcohol withdrawal. Alcohol Health Res World. 1998;22:25–33. [PMC free article] [PubMed] [Google Scholar]
- Becker HC, Hale RL. Repeated episodes of ethanol withdrawal potentiate the severity of subsequent withdrawal seizures: an animal model of alcohol withdrawal “kindling”. Alcohol Clin Exp Res. 1993;17:94–98. doi: 10.1111/j.1530-0277.1993.tb00731.x. [DOI] [PubMed] [Google Scholar]
- Becker HC, Lopez MF. Increased ethanol drinking after repeated chronic ethanol exposure and withdrawal experience in C57BL/6 mice. Alcohol Clin Exp Res. 2004;28:1829–1838. doi: 10.1097/01.alc.0000149977.95306.3a. [DOI] [PubMed] [Google Scholar]
- Cervera-Juanes R, Wilhem LJ, Park B, Lee R, Locke J, Helms C, Gonzales S, Wand G, Jones SR, Grant KA, Ferguson B. MAOA expression predicts vulnerability for alcohol use. Mol Psychiatry. 2016;21:472–479. doi: 10.1038/mp.2015.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervera-Juanes R, Wilhelm LJ, Park B, Grant KA, Ferguson B. Genome-wide analysis of the nucleus accumbens identifies DNA methylation signals differentiating low/binge from heavy alcohol drinking. Alcohol. 2016 doi: 10.1016/j.alcohol.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervera-Juanes R, Wilhelm LJ, Park B, Grant KA, Ferguson B. Alcohol-dose-dependent DNA methylation and expression in the nucleus accumbens identifies coordinated regulation of synaptic genes. Transl Psychiatry. 2017;7:e994. doi: 10.1038/tp.2016.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbit LH, Nie H, Janak PH. Habitual alcohol seeking: time course and the contribution of subregions of the dorsal striatum. Biol Psychiatry. 2012;72:389–395. doi: 10.1016/j.biopsych.2012.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuzon Carlson VC, Seabold GK, Helms CM, Garg N, Odagiri M, Rau AR, Daunais J, Alvarez VA, Lovinger DM, Grant KA. Synaptic and morphological neuroadaptations in the putamen associated with long-term, relapsing alcohol drinking in primates. Neuropsychopharmacology. 2011;36:2513–2528. doi: 10.1038/npp.2011.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delucchi KL, Kaskutas LA. Following problem drinkers over eleven years: understanding changes in alcohol consumption. J Stud Alcohol Drugs. 2010;71:831–836. doi: 10.15288/jsad.2010.71.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–1489. doi: 10.1038/nn1579. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration. Medical review of Vivitrol. Rockville, MD: 2006. Food and drug administration; pp. 21–897. [Google Scholar]
- Gerdeman GL, Partridge JG, Lupica CR, Lovinger DM. It could be habit forming: drugs of abuse and striatal synaptic plasticity. Trends Neurosci. 2003;26:184–192. doi: 10.1016/S0166-2236(03)00065-1. [DOI] [PubMed] [Google Scholar]
- Grant KA, Leng X, Green HL, Szeliga KT, Rogers LS, Gonzales SW. Drinking typography established by scheduled induction predicts chronic heavy drinking in a monkey model of ethanol self-administration. Alcohol Clin Exp Res. 2008;32:1824–1838. doi: 10.1111/j.1530-0277.2008.00765.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin WC, 3rd, Lopez MF, Becker HC. Intensity and duration of chronic ethanol exposure is critical for subsequent escalation of voluntary ethanol drinking in mice. Alcohol Clin Exp Res. 2009;33:1893–1900. doi: 10.1111/j.1530-0277.2009.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser SR, Deehan GA, Jr, Knight CP, Toalston JE, McBride WJ, Rodd ZA. Parameters of context-induced ethanol (EtOH)-seeking in alcohol-preferring (P) rats: temporal analysis, effects of repeated deprivation, and EtOH priming injections. Alcohol Clin Exp Res. 2016;40:2229–2239. doi: 10.1111/acer.13205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms CM, McClintick MN, Grant KA. Social rank, chronic ethanol self-administration, and diurnal pituitary-adrenal activity in cynomolgus monkeys. Psychopharmacology (Berl) 2012;224:133–143. doi: 10.1007/s00213-012-2707-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms CM, Park B, Grant KA. Adrenal steroid hormones and ethanol self-administration in male rhesus macaques. Psychopharmacology (Berl) 2014;231:3425–3436. doi: 10.1007/s00213-014-3590-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holleran KM, Winder DG. Preclinical voluntary drinking models for alcohol abstinence-induced affective disturbances in mice. Genes, Brain and Behavior. 2017;16:8–14. doi: 10.1111/gbb.12338. [DOI] [PubMed] [Google Scholar]
- Holtyn AF, Kaminski BJ, Wand GS, Weerts EM. Differences in extinction of cue-maintained conditioned responses associated with self-administration: Alcohol versus a nonalcoholic reinforcer. Alcohol Clin Exp Res. 2014;38:2639–2646. doi: 10.1111/acer.12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iranmanesh A, Veldhuis JD, Johnson ML, Lizarralde G. 24-hour pulsatile and circadian patterns of cortisol secretion in alcoholic men. J Androl. 1989;10:54–63. doi: 10.1002/j.1939-4640.1989.tb00062.x. [DOI] [PubMed] [Google Scholar]
- Jimenez VA, Porcu P, Morrow AL, Grant KA. Adaptations in Basal and Hypothalamic-Pituitary-Adrenal-Activated Deoxycorticosterone Responses Following Ethanol Self-administration in Cynomolgus Monkeys. Front Endocrinol. 2017a;8:19. doi: 10.3389/fendo.2017.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez VA, Allen DC, McClintick MN, Grant KA. Social setting, social rank and HPA axis response in cynomolgus monkeys. Psychopharmacology. 2017b doi: 10.1007/s00213-017-4596-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez VA, Grant KA. Studies using macaque monkeys to address excessive alcohol drinking and stress interactions. Neuropharmacology. 2017 doi: 10.1016/j.neuropharm.2017.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwako LE, Schwandt ML, Sells JR, Ramchandani VA, Hommer DW, George DT, Sinha R, Heilig M. Methods for inducing alcohol craving in individuals with co-morbid alcohol dependence and posttraumatic stress disorder: behavioral and physiological outcomes. Addict Biol. 2015;20:733–746. doi: 10.1111/adb.12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornet M, Goosen C, Van Ree JM. The effect of interrupted alcohol supply on spontaneous alcohol consumption by rhesus monkeys. Alcohol Alcohol. 1990;25:407–412. [PubMed] [Google Scholar]
- Kornet M, Goosen C, Van Ree JM. Effect of naltrexone on alcohol consumption during chronic alcohol drinking and after a period of imposed abstinence in free-choice drinking rhesus monkeys. Psychopharmacology (Berl) 1991;104:367–376. doi: 10.1007/BF02246038. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Palmer RS, Marlatt GA. Relapse prevention. An overview of Marlatt’s cognitive-behavioral model. Alcohol Res Health. 1999;23:151–160. [PMC free article] [PubMed] [Google Scholar]
- Lemolo A, Valenza M, Tozier L, Knapp CM, Kornetsky C, Steardo L, Sabino V, Cottone P. Withdrawal from chronic, intermittent access to a highly palatable food induces depressive-like behavior in compulvive eating rats. Behav Pharmacol. 2012;23:593–602. doi: 10.1097/FBP.0b013e328357697f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt G, Gordon J. Relapse prevention: A self-control strategy for the maintenance of behavior change. New York: Guilford; 1985. pp. 85–101. [Google Scholar]
- Matzger H, Kaskutas LA, Weisner C. Reasons for drinking less and their relationship to sustained remission from problem drinking. Addiction. 2005;100:1637–1646. doi: 10.1111/j.1360-0443.2005.01203.x. [DOI] [PubMed] [Google Scholar]
- Nimitvilai S, Uys JD, Woodward JJ, Randall PK, Ball LE, Williams RW, Jones BC, Lu L, Grant KA, Mulholland PJ. Orbitofrontal neuroadaptations and cross-species synaptic biomarkers in heavy-drinking macaques. J Neurosci. 2017;37:3646–3660. doi: 10.1523/JNEUROSCI.0133-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol Overdose: The Dangers of Drinking Too Much. Brochures and Fact Sheets. 2015 Available via NIAAA https://pubs.niaaa.nih.gov/publications/alcoholoverdosefactsheet/overdoseFact.pdf Accessed 20 November 2016.
- O’Tousa D, Grahame N. Habit formation: implications for alcoholism research. Alcohol. 2014;48:327–335. doi: 10.1016/j.alcohol.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pleil KE, Helms CM, Sobus JR, Daunais JB, Grant KA, Kash TL. Effects of chronic alcohol consumption on neuronal function in the non-human primate BNST. Addict Biol. 2016;21:1151–1167. doi: 10.1111/adb.12289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polich JM, Armor DJ, Braiker HB. The Course of Alcoholism: Four Years After Treatment. Vol. 1981. New York: John Wiley & Sons; 1981. Stability and change in drinking patterns; pp. 159–200. [Google Scholar]
- Ruedi-Bettschen D, Rowlett JK, Rallapalli S, Clayton T, Cook JM, Platt DM. Modulation of alpha5 subunit-containing GABAA receptors alters alcohol drinking by rhesus monkeys. Alcohol Clin Exp Res. 2013;37:624–634. doi: 10.1111/acer.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siciliano CA, Calipari ES, Yorgason JT, Mateo Y, Helms CM, Lovinger DM, Grant KA, Jones SR. Chronic ethanol self-administration in macaques shifts dopamine feedback inhibition to predominantly D2 receptors in nucleus accumbens core. Drug Alcohol Depend. 2016a;158:159–163. doi: 10.1016/j.drugalcdep.2015.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siciliano CA, Calipari ES, Yorgason JT, Lovinger DM, Mateo Y, Jimenez VA, Helms CM, Grant KA, Jones SR. Increased presynaptic regulation of dopamine neurotransmission in the nucleus accumbens core following chronic ethanol self-administration in female macaques. Psychopharmacology (Berl) 2016b;233:1435–1443. doi: 10.1007/s00213-016-4239-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair JD, Senter RJ. Development of an alcohol-deprivation effect in rats. Q J Stud Alcohol. 1968;29:863–867. [PubMed] [Google Scholar]
- Sinha R, Fox HC, Hong KA, Bergquist K, Bhagwagar Z, Siedlarz KM. Enhanced negative emotion and alcohol craving, and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology. 2009;34:1198–1208. doi: 10.1038/npp.2008.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ML, Hostetler CM, Heinricher MM, Ryabinin AE. Social transfer of pain in mice. Sci Adv. 2016;2:e1600855. doi: 10.1126/sciadv.1600855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanagel R. Recent animal models of alcoholism. Alcohol Res Health. 2000;24:124–131. [PMC free article] [PubMed] [Google Scholar]
- Spanagel R, Holter SM. Long-term alcohol self-administration with repeated alcohol deprivation phases: an animal model of alcoholism? Alcohol Alcohol. 1999;34:231–243. doi: 10.1093/alcalc/34.2.231. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K. Defining relapse from a harm reduction perspective. Journal of Evidence-Based Social Work. 2005;2:191–206. [Google Scholar]
- Witkiewitz K, Marlatt AG. Overview of harm reduction treatments for alcohol problems. International Journal of Drug Policy. 2006;17:285–294. [Google Scholar]
- Witkiewitz K, Masyn KE. Drinking trajectories following an initial lapse. Psychol Addict Behav. 2008;22:157–167. doi: 10.1037/0893-164X.22.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vivian JA, Green HL, Young JE, Majerksy LS, Thomas BW, Shively CA, Tobin JR, Nader MA, Grant KA. Induction and maintenance of ethanol self-administration in cynomolgus monkeys (Macaca fascicularis): long-term characterization of sex and individual differences. Alcohol Clin Exp Res. 2001;25:1087–1097. [PubMed] [Google Scholar]
- Yin HH, Park BS, Adermark L, Lovinger DM. Ethanol reverses the direction of long-term synaptic plasticity in the dorsomedial striatum. Eur J Neurosci. 2007;25:3226–3232. doi: 10.1111/j.1460-9568.2007.05606.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


