Abstract
Background
Data are limited on marijuana use and its impact on liver transplant (LT) waitlist outcomes. We aimed to assess the risk of waitlist mortality/delisting and likelihood of LT among prior marijuana users, and to determine the prevalence and factors associated with marijuana use.
Methods
Retrospective cohort of adults evaluated for LT over 2 years at a large LT center. Marijuana use defined by self-report in psychosocial assessment and/or positive urine toxicology. Ongoing marijuana use was not permitted for LT listing during study period.
Results
884 adults were evaluated and 585 (66%) were listed for LT (median follow up 1.4 years, IQR 0.5–2.0). Prevalence of marijuana use was 48%, with 7% being recent users and 41% prior users. Marijuana use had statistically significant association with alcoholic cirrhosis (IRR=1.9) and hepatitis C (IRR=2.1) vs. hepatitis B, tobacco use (prior IRR=1.4; recent IRR=1.3 vs. never), alcohol use (never IRR 0.1; heavy use/abuse IRR 1.2 vs. social), and illicit drug use (prior IRR=2.3; recent =1.9 vs. never). In adjusted competing risk regression, marijuana use was not associated with the probability of LT (prior HR 0.9; recent HR=0.9 vs. never) or waitlist mortality/delisting (prior HR 1.0; recent HR 1.0 vs. never). However, recent illicit drug use was associated with higher risk of death or delisting (HR 1.8, p=0.004 vs. never).
Conclusions
Unlike illicit drug use, marijuana use was not associated with worse outcomes on the LT waitlist. Prospective studies are needed to assess ongoing marijuana use on the LT waitlist and post-LT outcomes.
Introduction
Medical marijuana has moderate-to-high-quality evidence to treat conditions including chronic pain, neuropathic pain, spasticity due to multiple sclerosis, and chemotherapy associated nausea and vomiting 1–3. There has been growing interest in standardized trials to determine efficacy and side effects using standardized dosing 4. Marijuana is also increasingly recognized as a promising therapeutic target in various digestive disorders including inflammatory bowel disease, irritable bowel syndrome, secretion and motility-related disorders 5.
Data on marijuana use and progression of liver disease are limited and have yielded conflicting results. Cross-sectional studies 6–8 have reported a correlation between daily marijuana use and increase in liver fibrosis and steatosis among hepatitis C (HCV) patients. However, several subsequent cohort studies 9–11 did not confirm the association between marijuana use and accelerated progression to fibrosis or cirrhosis in HCV or HIV/HCV co-infected patients.
Whether marijuana use should be a contraindication for liver transplant (LT) is unclear. In a recent survey of transplant physicians, 47% identified marijuana use as a “controversial characteristic”12. In fact, there is little consensus within the LT community whether marijuana users should be eligible for transplant listing at all 13–15. Despite this debate, there are few reports on overall survival (pre and posttransplant) among chronic liver disease patients who use marijuana. Consequently, marijuana use among LT candidates remains a controversial topic 12,13.
Yet, in July 2015, California adopted Assembly Bill 258, the Medical Cannabis Organ Transplant Act, which prohibits transplant institutions from denying transplantation to medical marijuana users based on their use of marijuana alone16. In fact, 6 other states have adopted similar measures protecting medical cannabis users: Arizona, Delaware, Illinois, Minnesota, New Hampshire and Washington15. In addition, 6 states passed legislation or ballot measures to legalize medical marijuana in 2016 alone, bringing the total number of states with legalization of marijuana to twenty-eight in addition to the District of Columbia. Given the increasing trend towards legalization and protection of medical marijuana, understanding the impact of marijuana use on LT outcomes is not only practical but also essential.
In the only prior study assessing LT-related outcomes among marijuana users, Ranney et al 17 found no survival difference among LT candidates whether they consumed marijuana or not. However, in this study, more than a third of eligible patients (n = 803) on the LT waitlist were excluded due to missing tobacco, toxicology or psychiatric history. This large proportion of patients with missing toxicology data is likely to include many substance users who might be reluctant to undergo drug screening for fear of delisting or had poor follow up. Despite exclusion of these potentially high-risk patients, marijuana users were significantly less likely to receive LT (21.8% vs. 14.8%). Given the proportion of missing data, it is plausible that this study may not have adequately captured adverse outcomes like death or delisting among marijuana users on the LT waitlist.
In light of the limited data on LT waitlist outcomes, in the present study, we aimed to assess several outcomes among historical marijuana users who were evaluated for LT at our institution, including death or delisting on the LT waiting list and probability of receiving LT. In addition, we also sought to evaluate the prevalence of and factors associated with marijuana use among all patients undergoing LT evaluation at our center to guide future studies among this population.
Methods
Study Population & Design
All adults (age ≥18 years) presenting for a LT evaluation at University of California, San Francisco (UCSF) over a 2-year period, from January 1, 2012 through December 31, 2013, were included in this retrospective cohort study. The study was reviewed and approved by the UCSF institutional review board.
During the study period, the UCSF LT program had a policy of not listing patients with active marijuana use. Prior to listing, patients were required to abstain from marijuana use and, therefore, all marijuana use among listed patients is likely to be historical. Marijuana use was defined as ‘recent’ if subjects self-reported ongoing marijuana use at the time of first LT evaluation and/or had positive drug toxicology on screening laboratory evaluation. These patients were generally asked to abstain from marijuana use before being listed for LT. ‘Prior’ use refers to self-reported historical use of marijuana. Similarly, tobacco, alcohol and illicit substance (heroin, cocaine, amphetamines, hallucinogens, stimulants, nonprescription opiate/BDZ etc.) use was defined by combination of self-report and urine toxicology and further categorized as ‘prior’ and ‘recent’.
Outcomes
For the primary outcome, we assessed (1) the risk of waitlist death or delisting and (2) the risk of transplant among historical marijuana users and nonusers who were listed for LT. We also report factors associated with death and/or delisting on the waitlist and receiving LT. Secondary outcomes include prevalence of marijuana use and factors associated with marijuana use.
Sample size
In this retrospective cohort study, the primary end point is risk of waitlist death or delisting among historical marijuana users and nonusers who were listed for transplant at UCSF. A sample size of 570 is obtained by setting the alpha (two-tailed) at 0.05, beta at 0.2, assuming a baseline event rate (delisting/death/transplant) of 50% among nonmarijuana users (based on historic data), over a median follow up of 2 years, estimating censoring at 15%, and assuming a relative hazard of 1.35. Since about 300 patients are listed for LT at UCSF each year, a study period of 2 years would provide sufficient data to reach the desired sample size.
Data Collection & Analysis
Patient demographic and clinical data were collected by individual health record review and/or programmed capture from electronic medical record databases (data was abstracted in December 2015). Substance use, including marijuana, information was obtained from review of detailed psychosocial assessment conducted by trained social workers at the time of first LT evaluation. Statistical analyses were performed using STATA versions 12 and 14 software (Stata Corporation, College Station, Texas).
Marijuana use was defined as combination of self-report on psychosocial assessment or positive urine toxicology during initial LT evaluation and work up. Urine drug screening was performed at the discretion of the LT team based on perceived risk of drug use on the LT waitlist. Our study includes the initial urine drug screen with further data captured at the end of the study period via final LT status (i.e. those with ongoing drug use were delisted and this was captured at the end of the study). Marijuana use was further categorized as ‘prior’ or ‘recent’ at the time of first LT evaluation, as described previously. Factors associated with marijuana use were analyzed using a multivariable log-link Poisson regression with robust standard errors to estimate adjusted incidence rate ratios (IRR). Using this method, the calculated IRR approximates the prevalence ratio 18. All risk factors with p-values of less than 0.05 were retained in the multivariable model.
Among those listed for LT, we calculated the cumulative incidence of death or delisting within strata of marijuana use. Similarly, we also calculated the cumulative incidence of receiving LT within strata of marijuana use. Observation time was measured from date of first LT evaluation to the first of dropout, waitlist death, or transplant. Cumulative incidence estimates accounted for competing events and patients remaining on the waiting list were censored at the last known date on the list. Using Fine and Gray competing risk regression 19 we estimated the hazard ratios (HR) and 95% CI for risk of the 2 outcomes of interest, (1) waitlist death or delisting and (2) receiving transplant on the waitlist. Factors with a univariate p<0.2 and the primary explanatory variable, marijuana use, were included in the multivariable modeling process. The final multivariable models were selected by backward elimination with p>0.05 for removal while retaining marijuana use.
Results
Demographics of study participants
884 adults (age ≥18 years) had an initial LT evaluation at UCSF over the 2-year study period and all patients were included in this analysis. The median age of the cohort was 58 years (IQR 51–63) with 37% women, 56% white, 25% Hispanic/Latino, and 64% with a college degree. The most common etiology of liver disease was HCV cirrhosis (49%), majority of patients had MELD <20 (71%) and 33% had hepatocellular carcinoma (HCC). 66% of evaluated patients (n = 585) were listed for liver transplant and had median follow up of 1.4 (IQR 0.5–2.0) years during the study. Demographic and clinical characteristics of study subjects are listed in Table 1.
Table 1.
Demographics and clinical characteristics of study participants
| N (%) | |||
|---|---|---|---|
| Not listed N=299 |
Listed N=585 |
Total N=884 |
|
| Age (years) | |||
| 18–29 | 10 (3) | 14 (2) | 24 (3) |
| 30–44 | 39 (13) | 47 (8) | 86 (10) |
| 45–59 | 142 (47) | 280 (48) | 422 (48) |
| ≥60 | 108 (36) | 244 (42) | 352 (40) |
| Gender | |||
| Women | 122 (41) | 202 (35) | 324 (37) |
| Men | 177 (59) | 383 (65) | 560 (63) |
| BMI | |||
| <25 | 72 (27) | 171 (29) | 243 (28) |
| 25–29.9 | 102 (38) | 200 (34) | 302 (35) |
| 30–34.9 | 52 (19) | 109 (19) | 161 (10) |
| ≥35 | 42 (16) | 105 (18) | 147 (17) |
| Race/Ethnicity | |||
| White | 159 (59) | 317 (54) | 476 (56) |
| African American | 13 (5) | 27 (5) | 40 (5) |
| Asian | 27 (10) | 72 (12) | 99 (12) |
| Native Hawaiian/Pacific Islander | 3 (1) | 9 (2) | 12 (1) |
| American Indian/Other | 7 (3) | 9 (2) | 16 (2) |
| Hispanic/Latino | 61 (23) | 151 (26) | 212 (25) |
| Education | |||
| Less than high school | 18 (10) | 33 (8) | 51 (9) |
| Finished high school | 62 (34) | 100 (25) | 162 (28) |
| College or beyond | 101 (56) | 270 (67) | 371 (64) |
| Etiology of liver disease | |||
| Alcoholic cirrhosis | 50 (18) | 86 (15) | 136 (16) |
| HCV cirrhosis | 137 (49) | 284 (49) | 421 (49) |
| HBV cirrhosis | 15 (5) | 43 (7) | 58 (7) |
| NAFLD | 32 (11) | 48 (8) | 80 (9) |
| Other | 48 (17) | 124 (21) | 172 (20) |
| MELD | |||
| <20 | 203 (68) | 429 (73) | 632 (71) |
| ≥20 | 96 (32) | 156 (27) | 252 (29) |
| HCC | |||
| No | 220 (78) | 358 (61) | 578 (67) |
| Yes | 62 (22) | 227 (39) | 289 (33) |
Marijuana and other substance use
The vast majority (89%) of the cohort (N = 788/884) underwent urine drug screening during initial LT evaluation while the remaining 96 subjects (11%) underwent psychosocial assessment alone or had missing toxicology data. Prevalence of marijuana use was 48% with 7% being recent users at the time of evaluation (Table 2). Among marijuana users, 13% had a self-reported history of weekly use while 16% had been daily users. History of tobacco use was comparable at 55% with 8% reporting recent use at the time of LT evaluation. History of alcohol use was higher at 89% among all candidates with 54% having a history of heavy use/abuse, while 5% had recent alcohol use. Notably, 46% had a history of illicit drug use with 14% being recent users. Further, 22% of candidates had recent opiate or benzodiazepine prescriptions. Figure 1 presents drug use within strata marijuana use – recent and prior marijuana users were was prevalent across all categories and types of substance use, except never users of alcohol had limited use of marijuana (3%).
Table 2.
Substance use among study subjects
| N (%) | |||
|---|---|---|---|
| Not listed N=299 |
Listed N=585 |
Total N=884 |
|
| Marijuana use* | |||
| Never | 141 (47) | 319 (55) | 460 (52) |
| Prior | 125 (42) | 234 (40) | 359 (41) |
| Recent | 33 (11) | 32 (5) | 65 (7) |
| Marijuana use frequency§ | |||
| Less than weekly | 55 (36) | 113 (43) | 168 (40) |
| Weekly | 21 (14) | 31 (12) | 52 (13) |
| Daily | 27 (18) | 40 (15) | 67 (16) |
| Unknown | 50 (33) | 80 (30) | 130 (31) |
| Tobacco use | |||
| Never | 131 (44) | 264 (45) | 395 (45) |
| Prior | 122 (41) | 289 (49) | 411 (47) |
| Recent | 42 (14) | 32 (5) | 74 (8) |
| Alcohol use | |||
| Never | 35 (12) | 66 (11) | 101 (11) |
| Prior | 245 (82) | 494 (84) | 739 (84) |
| Recent | 19 (6) | 25 (4) | 44 (5) |
| Alcohol use frequency¶ | |||
| Social use | 105 (40) | 259 (50) | 364 (46) |
| Heavy use/abuse | 159 (60) | 260 (50) | 419 (54) |
| Illicit drug use* | |||
| Never | 146 (49) | 328 (56) | 474 (54) |
| Prior | 103 (35) | 185 (32) | 288 (33) |
| Recent | 49 (16) | 72 (12) | 121 (14) |
| Prescription opiate/BDZ use§ | |||
| Never | 187 (63) | 419 (72) | 606 (69) |
| Prior | 22 (7) | 53 (9) | 75 (9) |
| Recent | 86 (29) | 109 (19) | 195 (22) |
Self-report and/or urine toxicology
Self-report
Social use: ≤7 drinks/week for women or ≤14 drinks/week for men.
Figure 1.
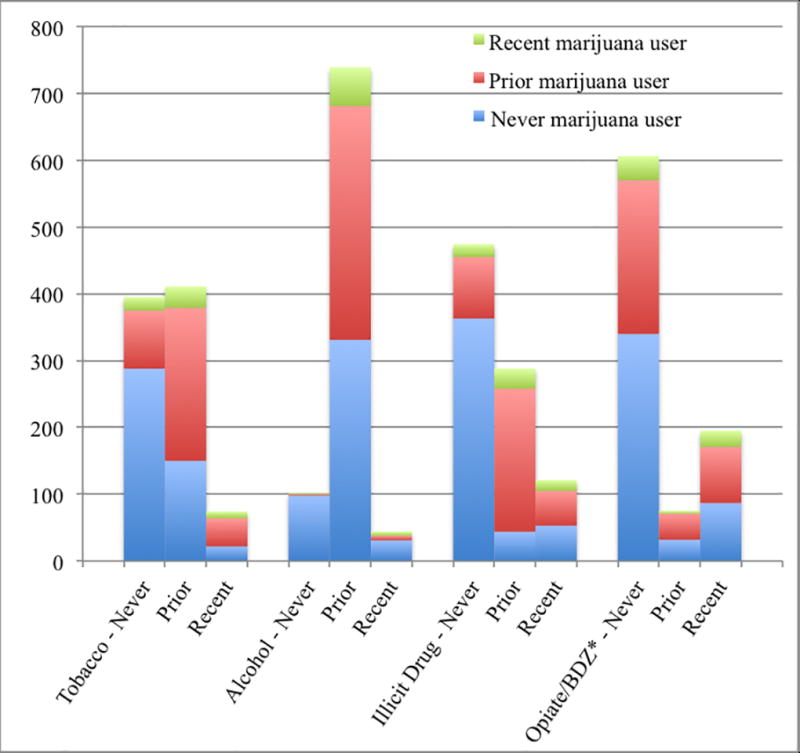
Drug use among all subjects in strata of marijuana use
*Prescription opiate and benzodiazepine use
Factors associated with marijuana use
After multivariable adjustment, history of marijuana use was associated with age 18–29 vs. 30–44 years (IRR 2.6, 95% CI 1.6–4.0), white vs. other race (IRR 1.2, 95% CI 1.1–1.4), alcoholic cirrhosis (IRR 1.9, 95% CI 1.0–3.7) and HCV (IRR 2.1, 95% CI 1.1–4.0) vs. HBV, MELD <20 (IRR 1.2, 95% CI 1.1–1.5), tobacco use (‘prior’ IRR 1.4, 95% CI 1.2–1.7 and ‘recent’ IRR 1.3, 95% CI 1.1–1.6 compared to ‘never’), alcohol use frequency (‘never’ IRR 0.1, 95% CI 0.04–0.3 and ‘heavy use/abuse’ IRR 1.2, 95% CI 1.0–1.3 compared to ‘social’) and illicit drug use (‘prior’ IRR 2.3, 95% CI 1.9–2.7 and ‘recent’ IRR 1.9, 95% CI 1.5–2.4 compared to ‘never’) (Table 3). Notably, male gender, BMI, HCC and prescription opiate/BDZ use were associated with marijuana use in univariate analysis but not after multivariable adjustment.
Table 3.
Poisson regression to determine factors associated with marijuana use (recent or prior)
| Univariable | Multivariable | |||
|---|---|---|---|---|
| IRR (95% CI) | p-value | IRR (95% CI) | p-value | |
| Age (years) | ||||
| 18–29 | 1.7 (1.1 – 2.6) | 0.02 | 2.6 (1.6 – 4.0) | <0.001 |
| 30–44 | 1 | 1 | ||
| 45–59 | 1.6 (1.1 – 2.1) | 0.005 | 1.0 (0.7 – 1.3) | 0.8 |
| >60 | 1.2 (0.9 – 1.7) | 0.2 | 0.9 (0.6 – 1.2) | 0.3 |
| Gender* | ||||
| Female | 1 | |||
| Male | 1.4 (1.2 – 1.6) | 0.0001 | ||
| BMI | ||||
| <25 | 1.0 (0.8 – 1.2) | 0.8 | ||
| 25–29.9 | 1 | |||
| 30–34.9 | 0.8 (0.6 – 1.0) | 0.02 | ||
| ≥35 | 0.9 (0.8 – 1.1) | 0.4 | ||
| Race/Ethnicity | ||||
| White | 1 | 1.2 (1.1 – 1.4) | 0.001 | |
| Non-white | 0.6 (0.5 – 0.7) | <0.0001 | 1 | |
| Education | ||||
| Did not finish high school | 1 | |||
| Finished high school | 1.4 (0.9 – 2.1) | 0.09 | ||
| College or beyond | 1.3 (0.9 – 1.9) | 0.2 | ||
| Etiology of liver disease | ||||
| Alcoholic cirrhosis | 3.6 (1.8 – 7.0) | <0.0001 | 1.9 (1.0 – 3.7) | 0.05 |
| HCV | 4.8 (2.5 – 9.2) | <0.0001 | 2.1 (1.1 – 4.0) | 0.02 |
| HBV | 1 | 1 | ||
| NAFLD | 1.4 (0.7 – 3.2) | 0.3 | 1.6 (0.8 – 3.2) | 0.2 |
| Other | 1.9 (1.0 – 3.9) | 0.06 | 1.6 (0.8 – 3.0) | 0.2 |
| MELD | ||||
| <20 | 1.2 (1.1 – 1.5) | 0.01 | 1.2 (1.1 – 1.5) | 0.005 |
| ≥20 | 1 | 1 | ||
| HCC* | ||||
| No | 1 | |||
| Yes | 1.2 (1.0 – 1.4) | 0.02 | ||
| Tobacco use | ||||
| Never | 1 | 1 | ||
| Prior | 2.3 (2.0 – 2.8) | <0.0001 | 1.4 (1.2 −1.7) | <0.001 |
| Recent | 2.6 (2.1 – 3.2) | <0.0001 | 1.3 (1.1 – 1.6) | 0.006 |
| Alcohol use frequency | ||||
| Never | 0.1 (0.02 – 0.2) | <0.0001 | 0.1 (0.04 – 0.3) | <0.001 |
| Social use | 1 | 1 | ||
| Heavy use/abuse | 1.7 (1.4 −1.9) | <0.0001 | 1.2 (1.0–1.3) | 0.03 |
| Illicit drug use | ||||
| Never | 1 | 1 | ||
| Prior | 3.6 (3.1 – 4.3) | <0.0001 | 2.3 (1.9 – 2.7) | <0.001 |
| Recent | 2.4 (1.9 – 3.0) | <0.0001 | 1.9 (1.5 – 2.4) | <0.001 |
| Prescription opiate/BDZ use* | ||||
| Never user | 1 | |||
| Prior user | 1.3 (1.1 – 1.6) | 0.02 | ||
| Recent user | 1.3 (1.1 – 1.5) | 0.003 | ||
Composite p-value <0.05 but not statistically significant in multivariable model.
Listing and waitlist outcomes
Of all 884 LT candidates, 585 (66%) were listed for LT. Among them, 205 (35%) died or were delisted while 287 (49%) received LT. Among never users of marijuana, 69% (319/460) were listed for LT. While, 65% (234/359) and 51% (33/65) of prior and recent users of marijuana were listed for LT, respectively. Listing and waitlist outcomes for all participants are outlined in Figure 2.
Figure 2.
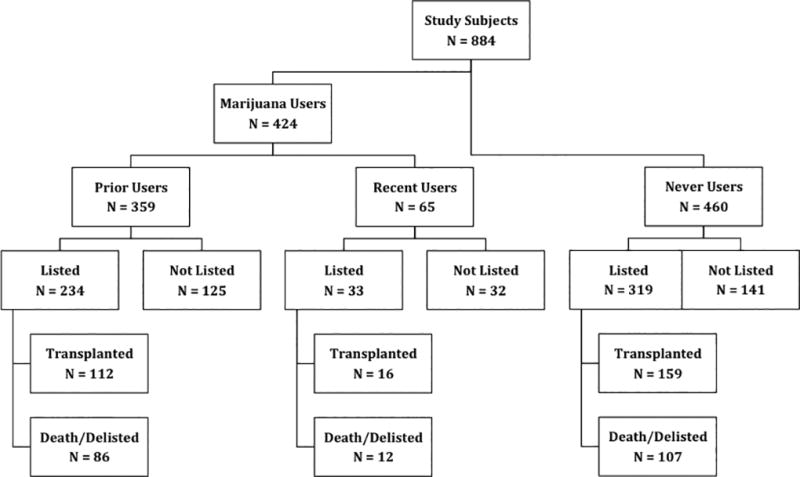
Listing and waitlist outcomes
Among those listed for LT, there was no statistically significant difference in the cumulative incidence of death or delisting on the LT waiting list within strata of marijuana use (Figure 3). Similarly, there was no statistically significant difference in the cumulative incidence of receiving LT within strata of marijuana use (Figure 4).
Figure 3.
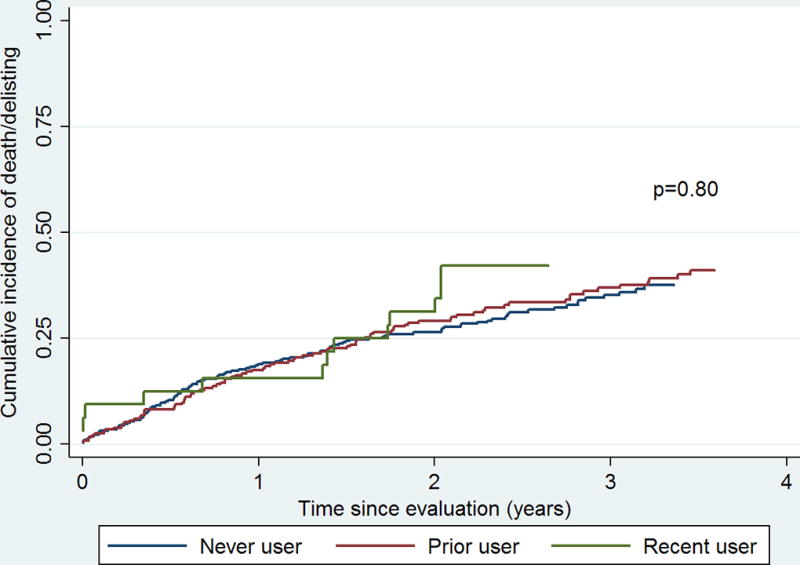
Cumulative incidence of death or delisting on the transplant waitlist by marijuana use
Figure 4.
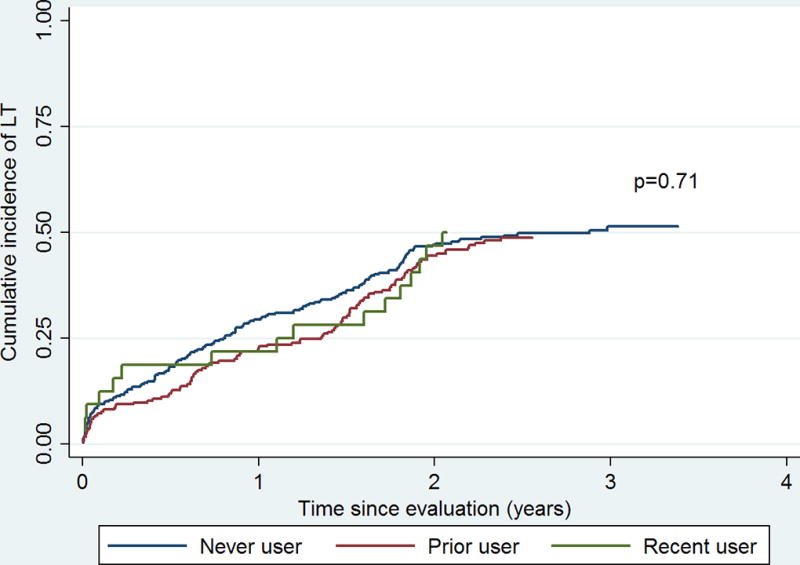
Cumulative incidence of receiving liver transplant (LT) on the transplant waitlist by marijuana use
Reasons for delisting from the LT waitlist are presented in Table 4. The most common reasons for delisting included ‘too sick for transplant’ (45%) and ‘death’ (31%). There were isolated cases of ‘substance abuse relapse’ (n = 8) with no significant differences between recent, prior and never users of marijuana (Pearson exact chi-square – recent vs. never, p=0.42 & prior vs. never, p=1.00).
Table 4.
Reasons for removal from the liver transplant waitlist by marijuana use (N = 205)
| Marijuana use N (%) |
|||
|---|---|---|---|
| Never user (N = 107) |
Prior user (N = 86) |
Recent user (N = 12) |
|
| Died | 51 (48) | 39 (45) | 3 (25) |
| Patient condition deteriorated, too sick for transplant | 35 (33) | 27 (31) | 2 (17) |
| Patient improved, transplant not needed | 4 (4) | 6 (7) | 2 (17) |
| Transferred to another center | 2 (2) | 3 (3) | 0 |
| Lack of social support | 0 | 2 (2) | 0 |
| Substance abuse relapse | 4 (4) | 3 (3) | 1 (8) |
| Refused transplant | 5 (5) | 1 (1) | 1 (8) |
| Other | 3 (3) | 3 (3) | 3 (25) |
Competing risk regression
Using competing risk regression, no statistically significant difference in risk of death or delisting was identified among patients with recent (HR 1.0, 95% CI 0.5–1.8, p=0.9) or prior (HR 1.0, 95% CI 0.7–1.4, p=0.9) marijuana use compared to never use in univariate or multivariable adjusted analysis (Table 5). In univariate analysis, alcohol use severity and illicit substance use had statistically significant associations with risk of death or delisting (Table 5). However, after multivariable adjustment, only recent use of illicit drugs (HR 1.8, 95% CI 1.2–2.8, p=0.004 vs. never) was statistically significantly associated with higher risk of death or delisting on the LT waiting list (Table 5).
Table 5.
Competing risk regression to determine factors associated with death/delisting on the liver transplant waitlist
| Univariable | Multivariable | |||
|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Marijuana use | ||||
| Never | 1.0 | 1.0 | ||
| Prior | 1.1 (0.8–1.4) | 0.54 | 1.0 (0.7–1.4) | 0.9 |
| Recent | 1.1 (0.6–2.0) | 0.70 | 1.0 (0.5–1.8) | 0.9 |
| Age | ||||
| 18–29 | 1.0 | |||
| 30–44 | 0.5 (0.2–1.5) | 0.22 | ||
| 45–59 | 0.7 (0.3–1.8) | 0.46 | ||
| >=60 | 0.7 (0.3–1.7) | 0.42 | ||
| Gender | ||||
| Female | 1.0 | |||
| Male | 1.1 (0.8–1.5) | 0.41 | ||
| Race | ||||
| White | 1.0 | |||
| Non-White | 1.0 (0.8–1.3) | 0.96 | ||
| MELD | ||||
| <20 | 1.0 | |||
| ≥20 | 1.3 (1.0–1.8) | 0.06 | ||
| HCC | ||||
| No | 1.0 | |||
| Yes | 1.2 (0.9–1.6) | 0.24 | ||
| Etiology of liver disease | ||||
| Alcoholic cirrhosis | 1.0 | |||
| HCV cirrhosis | 1.4 (0.9–2.0) | 0.14 | ||
| HBV cirrhosis | 1.1 (0.6–2.0) | 0.86 | ||
| NAFLD | 0.8 (0.4–1.6) | 0.60 | ||
| Other | 1.0 (0.6–1.7) | 0.90 | ||
| Education | ||||
| Did not finish high school | 1.0 | |||
| Finished high school | 1.8 (0.9–3.6) | 0.08 | ||
| College or beyond | 1.4 (0.7–2.6) | 0.33 | ||
| Unknown | 1.4 (0.8–2.8) | 0.26 | ||
| Tobacco use | ||||
| Never | 1.0 | |||
| Prior | 0.9 (0.7–1.2) | 0.72 | ||
| Recent | 1.3 (0.7–2.2) | 0.41 | ||
| Alcohol use severity | ||||
| Never | 1.1 (0.7–1.7) | 0.71 | ||
| Social | 1.0 | |||
| Heavy user/Abuse | 1.4 (1.0–1.8) | 0.03 | ||
| Illicit use | ||||
| Never | 1.0 | 1.0 | ||
| Prior | 1.2 (0.9–1.6) | 0.19 | 1.2 (0.9–1.8) | 0.2 |
| Recent | 1.8 (1.2–2.8) | 0.004 | 1.8 (1.2–2.8) | 0.004 |
| Prescription opiate/BDZ use | ||||
| Never | 1.0 | |||
| Prior | 0.9 (0.6–1.5) | 0.78 | ||
| Recent | 1.1 (0.8–1.5) | 0.65 | ||
Similarly, compared to never users, probability of receiving a LT was not statistically significantly decreased among patients with recent (HR 0.9, 95% CI 0.6–1.6, p=0.8) or prior (HR 0.9, 95% CI 0.7–1.2, p=0.4) marijuana use in univariate or multivariable adjusted analysis (Table 6). In univariate analysis, alcohol use severity and MELD ≥20 were statistically significantly associated with risk of receiving LT. However, after multivariable adjustment, only MELD ≥20 (HR 1.6, 95% CI 1.2–2.2, p=0.001) and HCC (HR 1.3, 95% CI 1.0–1.7, p=0.02) were statistically significantly associated with higher probability of receiving LT (Table 6).
Table 6.
Competing risk regression to determine factors associated with receiving liver transplant
| Univariable | Multivariable | |||
|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Marijuana use | ||||
| Never | 1.0 | 1.0 | ||
| Prior | 0.9 (0.7–1.1) | 0.41 | 0.9 (0.7–1.2) | 0.4 |
| Recent | 0.9 (0.6–1.5) | 0.77 | 0.9 (0.6–1.6) | 0.8 |
| Age | ||||
| 18–29 | 1.0 | |||
| 30–44 | 1.1 (0.5–2.4) | 0.86 | ||
| 45–59 | 0.8 (0.4–1.6) | 0.48 | ||
| >=60 | 0.8 (0.4–1.6) | 0.45 | ||
| Gender | ||||
| Female | 1.0 | |||
| Male | 1.0 (0.8–1.3) | 0.98 | ||
| Race | ||||
| White | 1.0 | |||
| Non-White | 1.1 (0.9–1.4) | 0.41 | ||
| MELD | ||||
| <20 | 1.0 | 1.0 | ||
| ≥20 | 1.5 (1.1–2.0) | 0.005 | 1.6 (1.2–2.2) | 0.001 |
| HCC | ||||
| No | 1.0 | 1.0 | ||
| Yes | 1.1 (0.9–1.4) | 0.24 | 1.3 (1.0–1.7) | 0.02 |
| Etiology of liver disease | ||||
| Alcoholic cirrhosis | 1.0 | |||
| HCV cirrhosis | 1.0 (0.7–1.4) | 0.86 | ||
| HBV cirrhosis | 1.5 (0.9–2.4) | 0.12 | ||
| NAFLD | 1.2 (0.7–1.9) | 0.58 | ||
| Other | 1.2 (0.8–1.8) | 0.30 | ||
| Education | ||||
| Did not finish high school | 1.0 | |||
| Finished high school | 0.6 (0.4–1.0) | 0.05 | ||
| College or beyond | 0.7 (0.5–1.2) | 0.20 | ||
| Unknown | 0.8 (0.5–1.3) | 0.40 | ||
| Tobacco use | ||||
| Never | 1.0 | |||
| Prior | 1.1 (0.9–1.4) | 0.41 | ||
| Recent | 0.8 (0.4–1.3) | 0.33 | ||
| Alcohol severity | ||||
| Never | 1.5 (1.0–2.1) | 0.04 | ||
| Social | 1.0 | |||
| Heavy use/Abuse | 0.9 (0.7–1.2) | 0.39 | ||
| Illicit use | ||||
| Never | 1.0 | |||
| Prior | 0.9 (0.7–1.1) | 0.30 | ||
| Recent | 0.8 (0.5–1.2) | 0.25 | ||
| Prescription opiate/BDZ use | ||||
| Never | 1.0 | |||
| Prior | 0.8 (0.5–1.2) | 0.30 | ||
| Recent | 0.8 (0.5–1.0) | 0.08 | ||
Discussion
Our study presents a comprehensive assessment of marijuana use among LT candidates. We found no statistically significant association between the risk of waitlist removal or death and historical marijuana use. On the other hand, notably, a history of recent illicit drug use was associated with higher risk of death or delisting. This finding could be related to a number of possibilities including recidivism to drug abuse which would prompt delisting from LT waitlist, or perhaps higher rate of medical illness from complications of drug use resulting in death or delisting. Illicit drug use may also reflect worse social circumstances and lack of support leading to delisting. On the other hand, a similar association with marijuana use was not found. This observation supports major differences in the impact of a history of marijuana use vs. illicit drug use among LT candidates. Similarly, in unadjusted and adjusted competing risk regression, we were unable to detect a statistically significant association between receiving LT and history of marijuana use. Factors associated with higher chance of receiving LT included MELD score ≥20 and HCC – both of which are consistent with and reflect current LT allocation practices (i.e. MELD exception points for HCC).
Marijuana use was highly prevalent among LT candidates at our institution. Almost half of all evaluated patients (48%) had a history of marijuana use and a considerable proportion (7%) were recent users at the time of evaluation. Among users, 13% had a self-reported history of weekly use while 16% had been daily users. Substance use, beyond marijuana, was a common feature among LT candidates – we found high prevalence of historical tobacco use (55%), alcohol use (89%), illicit drug use (47%) and prescription opiate/BDZ use (31%). More than half of all alcohol users (54%) had a history of heavy use/abuse, and a significant proportion (14%) of candidates were recent users of illicit substances. We also found that almost a quarter (22%) of evaluated patients had recent opiate/BDZ prescriptions. Though detailed and systematic data about substance abuse among all LT candidates are limited 20, our findings are similar to prior reports 20, including those assessing patients with alcoholic liver disease 21,22.
We also identify several factors associated with marijuana use, including younger age (18–29 years) and white race. Marijuana use was closely associated with other substance use – persons with alcoholic and HCV cirrhosis were more likely to have been marijuana users compared to those with HBV cirrhosis. Tobacco use, both prior and recent, was also associated with higher prevalence of marijuana use. Similarly, prior and recent illicit drug users had higher prevalence of marijuana use. Notably, never users of alcohol had much lower prevalence of marijuana use – this likely reflects a small proportion of LT candidates who have been abstinent or had very limited exposure to any substance use. There have been prior conflicting reports regarding an association between marijuana use and lower BMI 23–26. In univariate analysis, marijuana users were less likely to be obese (BMI 30–34.9, IRR 0.8) compared to overweight (BMI 25–29.9), though this association was not significant after multivariable adjustment (Table 3). This is the first study to present detailed data on prevalence and multivariable adjusted factors associated with marijuana use among LT candidates. Our findings are consistent with limited prior reports of marijuana use patterns among LT candidates 17. Recent national drug use surveys 27 have found that 6.5% of adults older than 25 had active marijuana use. These nationally representative estimates are in close agreement with our finding of 7% recent marijuana use among LT candidates. It is also important to note that marijuana use was not just limited to those with a history of substance abuse but was rather distributed across the spectrum of substance use, as demonstrated in Figure 1. Yet, in our study, despite noting a high prevalence of marijuana use and its associations with other substance use, we were unable to detect worse outcomes with historical marijuana use itself; whereas, illicit substance use did confer higher risk of death or delisting on the waitlist. In a recent study, Greenan et al 28 also found that isolated recreational marijuana was not associated with poorer outcomes among kidney transplant patients.
Though most patients (89%) underwent urine drug screening in addition to psychosocial evaluation to identify marijuana use in our cohort, we assessed for differences in sensitivity of marijuana use assessment between urine drug screening and psychosocial screening. Most marijuana users had positive urine toxicology – among ‘recent’ marijuana users 80% (N=52) had positive urine toxicology (of whom 52% also self-reported marijuana use) while an additional 20% (N=13) were identified based on self-report alone. Therefore, sensitivity of drug screening alone was 80% (N=52 of 65) while that of self-report alone was 62% (N=40 of 65).
We also assessed for differences in outcomes between those who tested negative for marijuana and those who were not tested with urine drug screening. A similar proportion of subjects with and without urine drug screen were positive for marijuana use – 48% (N=380 of 788) and 46% (N=44 of 96), respectively, with no statistical difference detected (chi-square p=0.66). When comparing subjects without marijuana use by presence or absence of the urine test, risk of death/delisting (univariate HR 0.69 urine test yes vs. no, 95% CI 0.36–1.32, p=0.26) and LT (univariate HR 0.92 urine test yes vs. no, 95% CI 0.52–1.62, p=0.77) failed to differ statistically. Regardless of screening method, a similar proportion of patients were positive for marijuana use and waitlist outcomes were similar.
Despite broad implications, there is limited data on clinical outcomes for patients who use marijuana before and after LT and no consensus within the transplant community surrounding marijuana use 12–14,29. Approximately 15,000 patients are currently listed for LT in the US according to the Organ Procurement and Transplantation Network (OPTN) 30. Therefore, given the rising prevalence of marijuana use, LT listing policies around marijuana use may affect several thousand patients in the US alone. Using psychosocial assessment and urine toxicology, our study is the first report on the prevalence and frequency of marijuana use and its effect on LT waitlist outcomes among a cohort of LT candidates in the Unites States. In the only prior study evaluating LT-related outcomes among marijuana users, Ranney et al 17 found that marijuana users were less likely to receive LT but had similar overall survival rates as nonusers. Their study, however, was limited by the exclusion of a large portion of LT waitlist candidates. They also did not assess waitlist outcomes like rate of delisting in this study and their use of urine toxicology alone to define marijuana led to a low prevalence estimate (∼10%) and may have led to misclassification of marijuana users. In contrast, we used a more robust definition of marijuana use based on psychosocial interviews combined with urine toxicology to describe the frequency and patterns of marijuana and other substance use among LT candidates. We also used a competing risk model to assess for rates of death or delisting in addition to receiving LT among marijuana users and nonusers.
Our study, and that of Ranney et al., did not find clear evidence of harm associated with historical marijuana use, and raises the question whether ongoing marijuana use could be considered safe on the LT waitlist. This question is especially relevant given recent passage of laws that protect medical marijuana users from transplant restrictions across several states in the United States. Further, could medical marijuana have a potential therapeutic role for LT candidates? A recent report documents successful use of prescription marijuana to decrease opiate use following liver transplantation 31. Perhaps marijuana could be effectively used for appetite stimulation, treating nausea, reducing opiate addiction, or postoperative pain relief. This is especially relevant considering that almost a quarter of LT candidates at our institution had recent opiate/BDZ prescriptions.
It is important to note that our understanding of the metabolism and effects of marijuana is still developing – marijuana use affects the endocannabinoid system, including the hepatic cannabinoid (CB) receptors, which are also modulated by chronic liver disease. Upregulation of the CB1 receptor in chronic liver disease has been implicated in progression of liver fibrosis 32,33. However, CB2 is also upregulated in liver disease and prevents fibrosis progression. It has been postulated that the balance between CB1 and CB2 receptor activation may modulate liver fibrosis – if both receptors are targeted equally then they may not be any net effect on liver fibrosis. However, there have been isolated cases of invasive aspergillosis related to marijuana use among posttransplant patients 34,35. A recent report also suggests potential for calcineurin inhibitor toxicity with heavy marijuana use 36.
Our study has several important limitations and should be interpreted with caution. We could not assess impact of ongoing marijuana use on waitlist outcomes because our institutional policy did not allow LT listing for active marijuana users. Those with active marijuana use, including heavy users, had to demonstrate abstinence prior to listing for LT. Therefore, based on our data we cannot comment on active marijuana use and our results should only be applied to historical marijuana use prior to LT listing. Those subjects who were able to satisfy the selection committee concerns and demonstrate abstinence from marijuana use were classified as ‘recent’ users in our study. All outcomes are presented in strata of ‘recent’ and ‘prior’ marijuana use to capture any differences between these 2 groups. Accordingly, we also cannot provide relevant data on the effects of ongoing marijuana use on post-LT outcomes. Though we attempt to adjust for confounding variables, given the limited prior work in this field there is potential for unmeasured confounding in our analysis. Further, our definition of marijuana use does not incorporate duration or method of marijuana use, as these data were not collected systematically at our institution. Finally, we defined marijuana use via combination of self-report in a psychosocial assessment and urine toxicology, which likely yields an underestimate of the true prevalence since patients had a conflict of interest in self-reporting marijuana use and urine toxicology to detect marijuana is an imperfect test.
In conclusion, we found a high prevalence of historical marijuana use that did not have clear adverse effects on LT waitlist outcomes. Recent use of illicit substances was, however, associated with higher risk of death or delisting from the LT waitlist. This suggests historical marijuana use alone may not be equivalent to use of other illicit drugs. Yet, this data should be interpreted with restraint as further research is needed to assess the impact of ongoing marijuana use among candidates on the LT waitlist. Further, posttransplant outcomes must also be followed in these patients to determine safety of continued marijuana use after LT. Recent passage of laws protecting medical marijuana users has created an urgent need to further study LT-related outcomes among this population.
Acknowledgments
Funding
This work was supported, in part, by the Biostatistics Core of the UCSF Liver Center (P30 DK026743).
Abbreviations
- BDZ
benzodiazepine
- HBV
hepatitis B virus
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- HIV
human immunodeficiency virus
- HR
hazard ratio
- IRR
incidence rate ratio
- LT
liver transplant
- MELD
model for end-stage liver disease
- NAFLD
nonalcoholic fatty liver disease
Footnotes
Authorship
PK - contributed to research design, data collection, data analysis, manuscript preparation
VS – contributed to research design, data analysis, manuscript preparation
JLD – contributed to data analysis, manuscript preparation
JR – contributed to research design, manuscript preparation
FY – contributed to research design, manuscript preparation
BH – contributed to research design, data analysis, manuscript preparation
Conflict of Interest
The authors declare no conflicts of interest
References
- 1.Hill KP. Medical Marijuana for Treatment of Chronic Pain and Other Medical and Psychiatric Problems: A Clinical Review. JAMA. 2015;313(24):2474–2483. doi: 10.1001/jama.2015.6199. [DOI] [PubMed] [Google Scholar]
- 2.Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA. 2015;313(24):2456–2473. doi: 10.1001/jama.2015.6358. [DOI] [PubMed] [Google Scholar]
- 3.Deshpande A, Mailis-Gagnon A, Zoheiry N, Lakha SF. Efficacy and adverse effects of medical marijuana for chronic noncancer pain: Systematic review of randomized controlled trials. Can Fam Physician. 2015;61(8):e372–381. [PMC free article] [PubMed] [Google Scholar]
- 4.Ware MA, Wang T, Shapiro S, Collet JP, team Cs. Cannabis for the Management of Pain: Assessment of Safety Study (COMPASS) J Pain. 2015;16(12):1233–1242. doi: 10.1016/j.jpain.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Goyal H, Singla U, Gupta U, May E. Role of cannabis in digestive disorders. Eur. J Gastroenterol Hepatol. 2017;29(2):135–143. doi: 10.1097/MEG.0000000000000779. [DOI] [PubMed] [Google Scholar]
- 6.Hezode C, Roudot-Thoraval F, Nguyen S, et al. Daily cannabis smoking as a risk factor for progression of fibrosis in chronic hepatitis C. Hepatology. 2005;42(1):63–71. doi: 10.1002/hep.20733. [DOI] [PubMed] [Google Scholar]
- 7.Hezode C, Zafrani ES, Roudot-Thoraval F, et al. Daily cannabis use: a novel risk factor of steatosis severity in patients with chronic hepatitis C. Gastroenterology. 2008;134(2):432–439. doi: 10.1053/j.gastro.2007.11.039. [DOI] [PubMed] [Google Scholar]
- 8.Ishida JH, Peters MG, Jin C, et al. Influence of cannabis use on severity of hepatitis C disease. Clin Gastroenterol Hepatol. 2008;6(1):69–75. doi: 10.1016/j.cgh.2007.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brunet L, Moodie EE, Rollet K, et al. Marijuana smoking does not accelerate progression of liver disease in HIV-hepatitis C coinfection: a longitudinal cohort analysis. Clin Infect Dis. 2013;57(5):663–670. doi: 10.1093/cid/cit378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu T, Howell GT, Turner L, Corace K, Garber G, Cooper C. Marijuana use in hepatitis C infection does not affect liver biopsy histology or treatment outcomes. Can J Gastroenterol Hepatol. 2014;28(7):381–384. doi: 10.1155/2014/804969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly EM, Dodge JL, Sarkar M, et al. Marijuana Use Is Not Associated With Progression to Advanced Liver Fibrosis in HIV/Hepatitis C Virus-coinfected Women. Clin Infect Dis. 2016;63(4):512–518. doi: 10.1093/cid/ciw350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Secunda K, Gordon EJ, Sohn MW, et al. National survey of provider opinions on controversial characteristics of liver transplant candidates. Liver Transpl. 2013;19(4):395–403. doi: 10.1002/lt.23581. [DOI] [PubMed] [Google Scholar]
- 13.Kroeker KI, Bain VG, Shaw-Stiffel T, Fong TL, Yoshida EM. Adult liver transplant survey: policies towards eligibility criteria in Canada and the United States 2007. Liver Int. 2008;28(9):1250–1255. doi: 10.1111/j.1478-3231.2008.01807.x. [DOI] [PubMed] [Google Scholar]
- 14.Coffman KL. The debate about marijuana usage in transplant candidates: recent medical evidence on marijuana health effects. Curr Opin Organ Transplant. 2008;13(2):189–195. doi: 10.1097/MOT.0b013e3282f56139. [DOI] [PubMed] [Google Scholar]
- 15.Pondrom S. Transplantation and Marijuana Use. Am J Transplant. 2016;16(1):1–2. doi: 10.1111/ajt.13679. [DOI] [PubMed] [Google Scholar]
- 16. [Accessed May 20, 2017];AB-258 Organ Transplants: medical marijuana: qualified patients. https://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=201520160AB258.
- 17.Ranney DN, Acker WB, Al-Holou SN, et al. Marijuana use in potential liver transplant candidates. Am J Transplant. 2009;9(2):280–285. doi: 10.1111/j.1600-6143.2008.02468.x. [DOI] [PubMed] [Google Scholar]
- 18.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 19.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;(94):496–509. [Google Scholar]
- 20.DiMartini A, Crone C, Dew MA. Alcohol and substance use in liver transplant patients. Clin Liver Dis. 2011;15(4):727–751. doi: 10.1016/j.cld.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 21.DiMartini A, Dew MA, Javed L, Fitzgerald MG, Jain A, Day N. Pretransplant psychiatric and medical comorbidity of alcoholic liver disease patients who received liver transplant. Psychosomatics. 2004;45(6):517–523. doi: 10.1176/appi.psy.45.6.517. [DOI] [PubMed] [Google Scholar]
- 22.Gedaly R, McHugh PP, Johnston TD, et al. Predictors of relapse to alcohol and illicit drugs after liver transplantation for alcoholic liver disease. Transplantation. 2008;86(8):1090–1095. doi: 10.1097/TP.0b013e3181872710. [DOI] [PubMed] [Google Scholar]
- 23.Rodondi N, Pletcher MJ, Liu K, Hulley SB, Sidney S. Marijuana use, diet, body mass index, and cardiovascular risk factors (from the CARDIA study) Am J Cardiol. 2006;98(4):478–484. doi: 10.1016/j.amjcard.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 24.Le Strat Y, Le Foll B. Obesity and cannabis use: results from 2 representative national surveys. Am J Epidemiol. 2011;174(8):929–933. doi: 10.1093/aje/kwr200. [DOI] [PubMed] [Google Scholar]
- 25.Thompson CA, Hay JW. Estimating the association between metabolic risk factors and marijuana use in U.S. adults using data from the continuous National Health and Nutrition Examination Survey. Ann Epidemiol. 2015;25(7):486–491. doi: 10.1016/j.annepidem.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 26.Hayatbakhsh MR, O’Callaghan MJ, Mamun AA, Williams GM, Clavarino A, Najman JM. Cannabis use and obesity and young adults. Am J Drug Alcohol Abuse. 2010;36(6):350–356. doi: 10.3109/00952990.2010.500438. [DOI] [PubMed] [Google Scholar]
- 27.Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality; 2016. Retrieved from http://www.samhsa.gov/data. [Google Scholar]
- 28.Greenan G, Ahmad SB, Anders MG, Leeser A, Bromberg JS, Niederhaus SV. Recreational marijuana use is not associated with worse outcomes after renal transplantation. Clin Transplant. 2016;30(10):1340–1346. doi: 10.1111/ctr.12828. [DOI] [PubMed] [Google Scholar]
- 29.Neyer J, Uberoi A, Hamilton M, Kobashigawa JA. Marijuana and Listing for Heart Transplant: A Survey of Transplant Providers. Circ Heart Fail. 2016;9(7) doi: 10.1161/CIRCHEARTFAILURE.115.002851. [DOI] [PubMed] [Google Scholar]
- 30.OPTN. Organ Procurement and Transplantation Network. [Accessed November 10, 2016];Liver Kaplan-Meier Patient Survival Rates For Transplants Performed : 1997 – 2004. https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/
- 31.Meng H, Hanlon JG, Katznelson R, Ghanekar A, McGilvray I, Clarke H. The prescription of medical cannabis by a transitional pain service to wean a patient with complex pain from opioid use following liver transplantation: a case report. Can J Anaesth. 2016;63(3):307–310. doi: 10.1007/s12630-015-0525-6. [DOI] [PubMed] [Google Scholar]
- 32.Basu PP, Aloysius MM, Shah NJ, Brown RS., Jr Review article: the endocannabinoid system in liver disease, a potential therapeutic target. Aliment Pharmacol Ther. 2014;39(8):790–801. doi: 10.1111/apt.12673. [DOI] [PubMed] [Google Scholar]
- 33.Tam J, Liu J, Mukhopadhyay B, Cinar R, Godlewski G, Kunos G. Endocannabinoids in liver disease. Hepatology. 2011;53(1):346–355. doi: 10.1002/hep.24077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hamadeh R, Ardehali A, Locksley RM, York MK. Fatal aspergillosis associated with smoking contaminated marijuana, in a marrow transplant recipient. Chest. 1988;94(2):432–433. doi: 10.1378/chest.94.2.432. [DOI] [PubMed] [Google Scholar]
- 35.Marks WH, Florence L, Lieberman J, et al. Successfully treated invasive pulmonary aspergillosis associated with smoking marijuana in a renal transplant recipient. Transplantation. 1996;61(12):1771–1774. doi: 10.1097/00007890-199606270-00018. [DOI] [PubMed] [Google Scholar]
- 36.Hauser N, Sahai T, Richards R, Roberts T. High on Cannabis and Calcineurin Inhibitors: A Word of Warning in an Era of Legalized Marijuana. Case Rep Transplant. 2016;2016:4028492. doi: 10.1155/2016/4028492. (2090–6943 (Print)) [DOI] [PMC free article] [PubMed] [Google Scholar]


