Abstract
Introduction
Immediate postpartum long-acting, reversible contraception (LARC)—providing intrauterine devices (IUD) and contraceptive implants immediately following birth—is an effective strategy to prevent unintended pregnancies and improve birth spacing. We measured US certified nurse-midwives’ (CNM) and certified midwives’ (CM) knowledge, training needs, current practice, and perceived barriers to providing immediate postpartum LARC.
Methods
We invited currently practicing CNM and CM members of the American College of Nurse-Midwives to complete an online survey about their knowledge and experience with the use of LARC, then analyzed eligible questionnaires using descriptive statistics.
Results
Of 4609 eligible midwives, 794 responded (17% response rate). Most were female (99.5%) and non-Hispanic white (92.1%), with 45.0% attending births in urban settings. Responses revealed multiple knowledge gaps related to IUD expulsion rates and appropriateness of immediate postpartum LARC in certain clinical scenarios. Only 10.1% of respondents reported feeling confident to insert an immediate postpartum IUD and 43.3% an implant. Many reported desiring additional training in immediate postpartum IUD (63.5%) and implant (22.8%) insertion; few reported access to such training (IUD 19.9%, implant 15.2%). Most respondents had never inserted an immediate postpartum IUD (90.7%) or implant (86.8%). The most commonly cited barriers to immediate postpartum LARC provision were that it is not standard practice (IUD 40.9%, implant 39.0%) or is not available (IUD 27.8%, implant 34.8%) at one’s institution and feeling inadequately trained (IUD 26.5%, implant 10.7%).
Discussion
Nine in 10 midwife respondents have never inserted an IUD or implant immediately postpartum, but more than half indicated they would like the opportunity to provide these services. Our findings highlight opportunities to enhance the immediate postpartum LARC-related knowledge and skills of the midwife workforce. They also suggest that logistical and institutional barriers to immediate postpartum LARC access must be removed in order to make this evidence-based reproductive health service available to all women who desire it.
Keywords: immediate postpartum contraception, midwife, intrauterine device, contraceptive implant, long-acting reversible contraception
INTRODUCTION
Seventy percent of pregnancies that occur in the first year after childbirth are unintended in the US.1 Such pregnancies are at increased risk for obstetric complications like preterm birth, stillbirth, and low birthweight.2–4 Unintended, short-interval pregnancies are directly related to contraceptive non-use or ineffective use.5 Women using highly effective, long-acting, reversible contraception (LARC) have approximately 4 times the odds of achieving an optimal birth interval than women using a barrier or no method.5 Although women using LARC methods enjoy the highest satisfaction and continuation rates of all reversible methods,6 only 6% of postpartum women use LARC.1 This scarce utilization does not seem to reflect patient demand, but rather, barriers to LARC access.7–9
Immediate postpartum LARC is proposed as a promising strategy to increase LARC utilization and offer postpartum women another opportunity to meet their family planning goals. Having LARC devices accessible for placement in the immediate postpartum period is safe and effective, is associated with high contraceptive continuation rates (>80% at 6 months), and reduces rapid repeat pregnancy rates.10–13 Furthermore, immediate postpartum LARC is cost-effective for payers and healthcare systems.14–16 The American College of Obstetricians and Gynecologists (ACOG) and the Centers for Disease Control and Prevention (CDC) support immediate postpartum LARC given its safety, effectiveness, and unique advantages compared to the outpatient setting.17,18
In recognition of these advantages, 21 state Medicaid agencies have initiated specific reimbursement for immediate postpartum LARC (outside the global payment for birth-related care) since 2012.19,20 This has created increased opportunities for women to gain access to immediate postpartum LARC. Yet increased reimbursement alone will not be sufficient to promote increased adoption if maternity care providers remain unprepared to offer immediate postpartum LARC.21–23 Midwives provide a substantial proportion of perinatal care in the United States,24 caring for 100% of women giving birth in some geographic areas.25 Women in these regions are more likely to be poor, rely heavily on Medicaid, travel longer distances to see a health care provider, report the highest rates of delayed or no medical care due to cost, and have a higher unintended pregnancy rate compared to women in more urban areas.25 Midwives thus represent a critically important group of maternity care providers who can offer increased immediate postpartum LARC access. Yet very little is currently known about the immediate postpartum LARC knowledge and practices of midwives who provide inpatient or hospital-based maternity care. Accordingly, the objective of this study was to identify immediate postpartum LARC knowledge and experiences, training needs, and perceived barriers among a national sample of midwives certified by the American Midwifery Certification Board (AMCB) as certified nurse-midwives (CNMs) or certified midwives (CMs) who are providing inpatient maternity care.
METHODS
We conducted an online survey of a national sample of midwives who were members of the American College of Nurse-Midwives (ACNM) and certified by AMCB as CNMs and CMs. This research was conducted in accordance with ACNM’s policy regarding soliciting its members for research purposes.
Sample Recruitment
Over 4 weeks in June and July 2016, we invited participation of all active members of ACNM with working e-mail addresses via e-mail. Active members include CNMs and CMs. We sent an introductory e-mail describing the study, followed by a primary invitation e-mail a week later, and finally 2 follow-up e-mails a week apart to encourage participation. All e-mails contained the ACNM logo, the subject heading “Approved ACNM Research Survey,” and a personalized greeting. Invitation e-mails contained a link to our online survey website. The survey was also publicized on various national midwife forums and networks. We offered a respondent reward (raffle prize for a $100 gift card) to incentivize responses.
Survey Administration
Recruitment e-mails to midwives provided a link to our study’s Qualtrics survey website. An introduction page explained the study’s purpose, its anonymous nature, the expected survey completion time (15 minutes), potential risks of participation, the option to quit at any time, and the raffle prize for survey completion. Participants consented to participation by clicking the “Enter Study” button on the page. Eligibility was determined by an affirmative response to the question “Do you currently provide unsupervised inpatient labor and delivery-related care?”
Survey Instrument
The survey instrument was developed by our research team based on a comprehensive literature review and our prior work. In our prior work, we have qualitatively interviewed Medicaid administrators about barriers to immediate postpartum LARC implementation.20,22 Key findings from prior work suggest that immediate postpartum LARC capacity will be influenced by general LARC knowledge, both LARC and immediate postpartum LARC training, and current levels of LARC and immediate postpartum LARC provision. Our survey included items assessing all of these domains.
We assessed knowledge about the relative risk of intrauterine device (IUD) expulsion with immediate versus interval insertion and the appropriateness of immediate postpartum LARC in specific clinical scenarios. The US Medical Eligibility Criteria for Contraceptive Use (USMEC) is a publicly-available guide published by the CDC for clinicians providing family planning services. The USMEC provides evidence-based guidance about the use of various contraceptive methods under specific clinical circumstances. Conditions are classified into 4 categories: USMEC 1, no restriction, method can be used; USMEC 2, advantages generally outweigh theoretical or proven risks; USMEC 3, theoretical or proven risks generally outweigh advantages; USMEC 4, unacceptable health risk, method not to be used. Immediate postpartum LARC appropriateness is classified as USMEC 1 or 2.17
We assessed perceived importance of contraceptive counseling and provision (with responses on a 5-item Likert scale, “strongly agree” to “strongly disagree”). We then asked about frequency of provision of immediate postpartum LARC (“I have placed an immediate postpartum IUD at time of vaginal delivery,” “I have placed an immediate postpartum implant”). Respondents could answer “Never”, “1-2 times,” “3-5 times,” “6-10 times,” or “>10 times.” We included one item assessing confidence to counsel about and insert LARC devices in the outpatient setting and immediate postpartum setting (with responses on a 6-item Likert scale, “extremely confident” to “not at all confident”). We also included items assessing whether respondents had received prior training in LARC device insertion, whether additional training was desired, and whether training opportunities were accessible (response options were yes or no).
Finally, recognizing that multiple clinical barriers may exist to immediate postpartum LARC, we also asked about perceived barriers to immediate postpartum LARC provision. A range of barriers were provided as potential answer choices, including: feel inadequately trained, device not available at institution, not institution’s standard practice, risks of placement (and a request to specify with free text), lack of institutional policy for informed consent, reimbursement concern, not enough time, and patients decline. Respondents were also allowed to provide free text responses to this question. Prior to fielding, the survey was pilot tested with midwives (n=12) at our home institution.
Data Analysis
The analytic sample included only those submitting the last online questionnaire page. The Internet Protocol (IP) address of the respondent’s computer was reviewed; no duplicate respondents were identified. Descriptive statistics were used to calculate frequencies, proportions, 95% confidence intervals, means, and standard deviations for all responses. Reponses to Likert Scale or ranked-response questions were dichotomized into appropriate categories. Responses to open-ended questions in the survey were manually reviewed and summarized. All analyses were conducted using SAS version 9.4 (SAS Institute Inc, Cary, NC), and effects were considered significant at an alpha level of .05. This project was approved by the University of Michigan Institutional Review Board.
RESULTS
Of 4609 individuals invited to participate, 794 (17%) completed the survey. Overall, participants (N=794) were predominantly female (99.5%) and non-Hispanic white (92.1%; Table 1). Significant proportions reported practicing midwifery for more than 10 years (67.0%) and in urban settings (45.0%). The sample was evenly distributed across major regions of the United States, with respondents practicing in 47 states.
Table 1.
Demographic and practice characteristics of midwives currently attending births in the United States (N=794)
| Characteristics | Respondents n (%) |
|---|---|
| Sex | |
| Female | 785 (99.5) |
| Male | 4 (0.5) |
| Race | |
| Non-Hispanic white | 721 (92.1) |
| Non-Hispanic black | 17 (2.2) |
| Other | 45 (5.7) |
| Years in Practice | |
| 1 - 10 years | 261 (33.0) |
| 11 - 20 years | 215 (27.2) |
| > 20 years | 314 (39.8) |
| Regiona | |
| Northeast | 188 (25.0) |
| Midwest | 190 (25.2) |
| South | 193 (25.6) |
| West | 183 (24.2) |
| Practice Location | |
| Urban | 355 (45.0) |
| Suburban | 251 (31.8) |
| Town (5000 - 50,000) | 146 (18.5) |
| Rural or town < 5000 | 37 (4.7) |
| Births attended in last 12 months | |
| 0 – 10 | 26 (3.4) |
| 11 - 50 | 240 (31.5) |
| 51 - 100 | 318 (41.7) |
| > 100 | 178 (23.4) |
| Proportion of patients covered by Medicaid | |
| < 25% | 130 (18.4) |
| 25 - 49% | 189 (26.7) |
| 50 - 75% | 190 (26.8) |
| >75% | 199 (28.1) |
| Location of attended birthsb | |
| Hospitals | 748 (94.2) |
| Birthing centers | 80 (10.1) |
| Women’s centers | 48 (6.1) |
Based on US Census Bureau designations for region
Column does not equal 100% due to multiple responses
LARC Knowledge and Attitudes
Overall, there were notable knowledge gaps among the respondents about immediate postpartum LARC. When asked about IUD expulsion, 40.5% did not identify expulsion rates as higher with immediate postpartum compared to interval IUD placement. Similarly, 46.4% did not identify that expulsion rates with insertion at 6 weeks postpartum are similar to insertion in women who are not postpartum. When asked about the appropriateness of immediate postpartum LARC during clinical scenarios (Figure 1), 25.3% incorrectly reported that no immediate postpartum LARC method is acceptable in women with chorioamnionitis; IUDs are contraindicated with this condition (USMEC 4), but the contraceptive implant is appropriate (USMEC 1). More than 7 in 10 respondents correctly identified the levonorgestrel IUDs, copper IUD, and contraceptive implant as appropriate for breastfeeding women. However, fewer respondents perceived the levonorgestrel IUDs (68.6%) and contraceptive implant (59.2%) as appropriate for women with a history of postpartum depression (although the USMEC rates these devices as category 1 in the setting of depressive disorders). Most respondents correctly identified immediate postpartum LARC as appropriate in adolescents (USMEC 1 or 2). Only half of respondents (52.1% hormonal IUD; 50.3% non-hormonal IUD) felt IUDs were appropriate in women with a history of pelvic inflammatory disease (PID), despite USMEC category 1 ratings for LARC devices in this setting (assuming the absence of acute PID or puerperal infection). Most respondents strongly agreed or somewhat agreed that counseling about postpartum contraception (92.1%) and providing the full range of contraceptive methods (94.4%) are each important parts of their role as a midwife.
Figure 1. Perceived appropriateness of immediate postpartum hormonal IUD, non-hormonal IUD, and implant insertion in specific clinical scenarios.
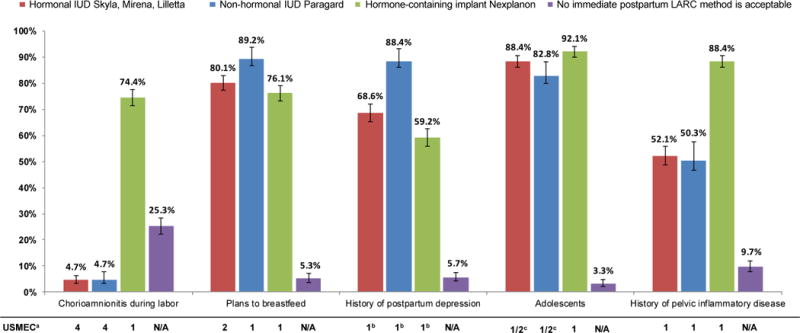
<<TYPESETTER, THE FOLLOWING TEXT GOES BELOW THE BLUE BOX WITH THE FIGURE TITLE>>
Abbreviation: USMEC, United States Medical Eligibility Criteria.
aThe USCMEC categories are 1 – no restriction for use, 2 – advantages of method generally outweigh risks, 3 – theoretical or proven risks generally outweigh advantages, and 4 – unacceptable health risk with method use.
bSee USMEC ratings for depressive disorders.
cCategory 2 for women aged <20 years and category 1 for women aged 20 years and older.
LARC and Immediate Postpartum LARC Training Needs
A majority of respondents reported feeling confident, very confident, or completely confident to counsel about LARC (96.7%) and insert IUDs (87.5%) or implants (67.4%) in the outpatient office setting. In contrast, fewer felt confident, very confident, or completely confident performing these tasks immediately postpartum (counsel on IUD, 40.3%; insert an IUD, 10.1%; counsel on implants, 53.2%; insert an implant, 43.3%).
A majority of respondents reported having previously received training to insert at least one of the levonorgestrel IUDs (Skyla, Liletta, Mirena; 94.0%) or the contraceptive implant (Nexplanon; 76.4%). Many respondents reported desire for additional training in IUD insertion at the outpatient postpartum visit (10.3%), IUD insertion immediately following a vaginal birth (63.5%), and contraceptive implant insertion (22.8%), yet far fewer respondents reported having access to training at their institution, national meetings, or other continuing education opportunities (outpatient IUD insertion, 6.6%; immediate postpartum IUD insertion, 19.9%; implant insertion, 15.2%).
Immediate Postpartum LARC Provision
Overall, respondents rarely performed immediate postpartum LARC insertions, with the vast majority of midwives having never placed an immediate postpartum IUD (90.7%) or implant (86.8%) during their career. Among those who have never inserted an IUD immediately postpartum (90.7%), 52.5% desire the opportunity to do so. Among those who have inserted an immediate postpartum IUD during their career (9.3%), 51.4% would like to do so more often. Among those who have never inserted an implant immediately postpartum (86.6%), 52.6% desire the opportunity to do so. Among those who have inserted an immediate postpartum implant during their career (13.2%), 59.1% would like to do so more often.
Perceived Barriers to Immediate Postpartum Contraception
Respondents identified multiple barriers to immediate postpartum LARC placement (Figure 2). The most commonly cited barriers were that postpartum LARC insertion was not standard practice or not available at one’s institution. Feeling inadequately trained was more often cited as a barrier to immediate postpartum IUD (26.5%) compared to implant (10.7%) insertion. Reimbursement concerns were cited as barriers to both device types (16.4%), and some respondents (8.4%) also harbored concerns about IUD expulsion or perforation. Uncommonly cited barriers included one’s patients decline immediate postpartum LARC, religious institutional policy, one’s personal objections to immediate postpartum LARC, and perceived risks for breastfeeding.
Figure 2.
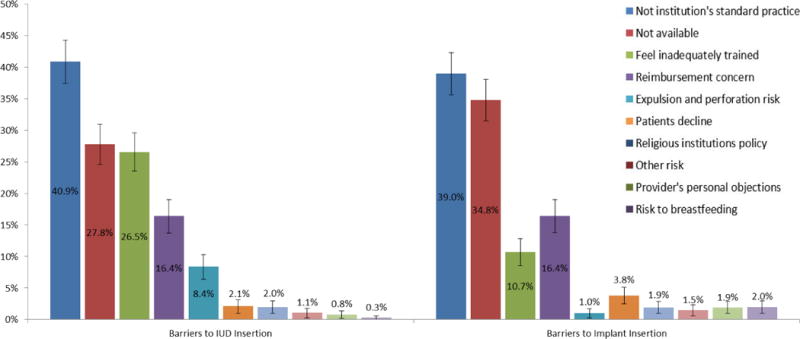
Perceived barriers to immediate postpartum intrauterine device and implant insertion among a national sample of midwives in the United States
DISCUSSION
In this national, cross-sectional survey of ACMB-certified midwives who are members of ACNM, most reported never inserting an IUD or implant in the immediate postpartum setting, but more than half would like the opportunity to offer these services. Our findings highlight opportunities to enhance the immediate postpartum LARC-related knowledge and skills of the midwife maternity care workforce. They also suggest that midwives perceive logistic and institutional barriers to this service, indicating that addressing training needs alone will be insufficient to enhance access to immediate postpartum LARC.
Approximately 9 in 10 respondents had never placed an IUD or implant in the immediate postpartum setting. Given that midwives are the primary maternity care provider in many regions of the country,25 this suggests a concerning barrier for women hoping to initiate a LARC method during hospitalization for childbirth. Both ACOG and the CDC have emphasized the safety and effectiveness of immediate postpartum LARC.17,26 While ACNM does not have its own statement specific to the use of LARC or immediate postpartum LARC, ACNM does have a position statement supporting access to evidence-based options to support women’s reproductive health choices, which would include LARC.27 However, women will not be able to access immediate postpartum LARC if maternity care providers do not or cannot offer it. A recent ACOG Committee Opinion endorsed by ACNM states that “immediate postpartum LARC should be offered as an effective option for postpartum contraception” and “maternity care providers should incorporate immediate postpartum LARC into their practices.”26 Encouragingly, more than half of respondents expressed a desire to perform immediate postpartum LARC device insertions more frequently.
One critical step in building workforce capacity for immediate postpartum LARC is addressing knowledge gaps. In our survey, only 6 in 10 respondents correctly identified IUD expulsion rates as higher in the immediate versus delayed postpartum setting. The estimated risk of IUD expulsion is as high as 10% to 27% immediately postpartum, compared to approximately 4% when placed at greater than 4 weeks postpartum.28–33 In a meta-analysis of 4 randomized controlled trials of immediate postpartum IUD insertion, the likelihood of IUD expulsion was higher for immediate versus interval insertion (odds ratio, 4.89; 95% confidence interval, 1.47-16.32), but IUD use at 6 months was twice as likely in the immediate insertion group, likely due to low rates of follow-up for outpatient insertion.33 For women who face barriers to outpatient follow-up, the advantages of immediate postpartum IUD insertion may outweigh the potential drawbacks of a higher expulsion rate. ACOG recommends that maternity care providers counsel women about the risk of expulsion in the context of informed decision-making about postpartum contraception.26
Our survey also documented knowledge gaps related to appropriateness of immediate postpartum LARC under certain clinical circumstances. The CDC recently released the USMEC, 2016, which can assist maternity care providers in offering women evidence-based guidance about postpartum contraceptive options.17
Our findings suggest the importance of connecting midwives with skills-based training opportunities. For midwives already trained to insert the contraceptive implant, reassurance may be the only intervention needed, as the immediate postpartum insertion technique is identical to the routine outpatient insertion technique. For immediate postpartum IUD placement, insertion technique is different from insertion in a non-gravid uterus. Six in 10 respondents in our survey desired additional training in immediate postpartum IUD insertion, but only 2 in 10 respondents reported having access to such training. Our findings corroborate a recent study of attending-level maternity care providers (obstetricians, midwives, and family physicians) at 7 academic hospitals in Massachusetts that also documented low levels of immediate postpartum LARC knowledge and experience.23 Among midwives and family physicians, only 2 in 10 offered immediate postpartum IUDs, and only 4 in 10 obstetricians provided this service. The most frequently cited reason for never having placed a postpartum IUD was inadequate training. Multiple tools are publicly available to assist providers wanting to build a skill set for immediate postpartum IUD insertion;34 however, additional formal training opportunities, including simulation-based training and supervised insertion in one’s primary clinical setting, as well as provisions for training student midwives, will likely be necessary to ensure that the full midwife workforce is trained to offer this service.
In addition to training needs, midwives in our survey identified multiple other barriers to provision of immediate postpartum LARC services, including institutional norms, device unavailability, and concerns about reimbursement. In many institutions, the primary barrier to immediate postpartum LARC services has been non-reimbursement for inpatient LARC provision. Labor and birth care has traditionally been reimbursed with one global, bundled payment. Recognizing that this may act as a financial disincentive to the provision of inpatient LARC services, 26 state Medicaid agencies to date have begun providing specific payment for immediate postpartum contraception in addition to the global fee.20,35 The Center for Medicaid and Children’s Health Insurance Program (CHIP) Services has encouraged all state agencies to adopt reimbursement approaches that promote the availability of LARC, including “unbundling payment for LARC from other labor and birth services.”36 Eliminating reimbursement policies that deny postpartum women access to LARC prior to hospital discharge is an essential step in ensuring access to highly effective methods and reducing unintended and short-interval pregnancies.37 As reimbursement becomes more commonplace, it may create an environment conducive to addressing other barriers, such as provider training.
Notably, midwife respondents to this survey did not report concerns about potential adverse effects of immediate postpartum LARC on breastfeeding. Immediate postpartum insertion of IUDs and the contraceptive implant is considered safe (USMEC 1 for implant and copper IUD, USMEC 2 for levonorgestrel IUD for women who are breastfeeding, USMEC 1 for levonorgestrel IUD for women who are not breastfeeding). A recent study of lactation consultants documented misinformation regarding the safety of immediate postpartum LARC.38 Maternity care providers should be aware of potential knowledge gaps and work to ensure that women receive consistent and evidence-based guidance about immediate postpartum LARC.
Our findings should be interpreted within the context of our study’s limitations. Cross-sectional surveys will not capture changes over time in knowledge, attitudes, and expertise. Our response rate was suboptimal, despite our using best practices for clinician recruitment for survey research (eg, using multiple personalized e-mail invitations endorsed by ACNM, providing a monetary raffle incentive). While maintaining high response rates is always desirable, clinician surveys may be more resilient to non-response bias, particularly when they involve a larger sample size as in our survey.39 Findings may not generalize to non-members of ACNM or to midwives certified by other organizations. There may be important clinician-level barriers not assessed in our surveys, although our team’s prior work investigating immediate postpartum LARC provision mitigates this risk. While the study’s anonymous, online design reduces the risk of social desirability bias, all self-report measures are subject to this concern.
This national survey of midwives constitutes a large-scale assessment of potential barriers faced by midwives wanting to provide immediate postpartum LARC services. The knowledge and training gaps documented here suggest a need for didactic and skills-based training opportunities directed towards midwife clinicians, a critical portion of the maternity care workforce. Our findings also suggest the need to remove institutional and policy-level barriers to immediate postpartum LARC services, including social norms that may prevent service provision, as well as to remove technical barriers to stocking LARC devices in the inpatient setting. Our study and other work suggest that multi-component strategies will be needed in order to integrate immediate postpartum LARC into routine postpartum care.21,22 Such efforts will help make this evidence-based reproductive health service available to all women who desire it.
QUICK POINTS.
Approximately 9 in 10 midwife respondents to this national survey of American College of Nurse-Midwives members have never inserted an IUD or implant in the immediate postpartum setting.
Midwives identified training needs and multiple logistical and institutional barriers to immediate postpartum LARC provision.
More than half of respondents would like the opportunity to provide these services.
Findings suggest a need for didactic and skills-based training opportunities directed towards midwives, as well as institutional interventions to enhance LARC availability in the inpatient postpartum setting.
Acknowledgments
This study was funded by the Department of Obstetrics and Gynecology at the University of Michigan.
Grant: NIH/NIDDK grant #P30 DK092926.
Footnotes
Conflict of Interest: Vanessa Dalton is a paid expert witness for Bayer Corporation. All other authors have no conflicts of interest to disclose.
Contributor Information
Michelle H. Moniz, Clinical practice and an Assistant Professor in the University of Michigan’s Department of Obstetrics and Gynecology and Institute for Healthcare Policy and Innovation.
Lee Roosevelt, Clinical Assistant Professor at the University of Michigan School of Nursing.
Halley P. Crissman, House Officer in the Department of Obstetrics and Gynecology at the University of Michigan.
Emily K. Kobernik, Biostatistician in the Department of Obstetrics and Gynecology at the University of Michigan.
Vanessa K. Dalton, Practicing clinician, Associate Professor, and Associate Chair for Research in the Department of Obstetrics and Gynecology at the University of MichiganMember of the Institute for Healthcare Policy and Innovation.
Michele H. Heisler, Professor of Internal Medicine at the University of Michigan Medical School and Professor of Health Behavior and Health Education at the University of Michigan School of Public HealthMember of the Institute for Healthcare Policy and Innovation.
Lisa Kane Low, Clinical practice at the University of Michigan Von Voigtlander Women’s Hospital, an Associate Professor and Associate Dean for Practice and Professional Graduate Studies at the University of Michigan School of Nursing, and Associate Professor in the Department of Obstetrics and Gynecology.
References
- 1.White K, Teal SB, Potter JE. Contraception after delivery and short interpregnancy intervals among women in the United States. Obstet Gynecol. 2015 Jun;125(6):1471–1477. doi: 10.1097/AOG.0000000000000841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conde-Agudelo A, Rosas-Bermudez A, Castano F, Norton MH. Effects of birth spacing on maternal, perinatal, infant, and child health: a systematic review of causal mechanisms. Stud Fam Plann. 2012 Jun;43(2):93–114. doi: 10.1111/j.1728-4465.2012.00308.x. [DOI] [PubMed] [Google Scholar]
- 3.Conde-Agudelo A, Rosas-Bermudez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006 Apr 19;295(15):1809–1823. doi: 10.1001/jama.295.15.1809. [DOI] [PubMed] [Google Scholar]
- 4.Rigsby DC, Macones GA, Driscoll DA. Risk factors for rapid repeat pregnancy among adolescent mothers: a review of the literature. J Pediatr Adolesc Gynecol. 1998 Aug;11(3):115–126. doi: 10.1016/s1083-3188(98)70130-5. [DOI] [PubMed] [Google Scholar]
- 5.Thiel de Bocanegra H, Chang R, Howell M, Darney P. Interpregnancy intervals: impact of postpartum contraceptive effectiveness and coverage. Am J Obstet Gynecol. 2014 Apr;210(4):311 e311–318. doi: 10.1016/j.ajog.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 6.Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011 May;117(5):1105–1113. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogburn JA, Espey E, Stonehocker J. Barriers to intrauterine device insertion in postpartum women. Contraception. 2005 Dec;72(6):426–429. doi: 10.1016/j.contraception.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 8.Potter JE, Hopkins K, Aiken AR, et al. Unmet demand for highly effective postpartum contraception in Texas. Contraception. 2014 Nov;90(5):488–495. doi: 10.1016/j.contraception.2014.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zerden ML, Tang JH, Stuart GS, Norton DR, Verbiest SB, Brody S. Barriers to Receiving Long-acting Reversible Contraception in the Postpartum Period. Womens Health Issues. 2015 Jul 23; doi: 10.1016/j.whi.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Tocce KM, Sheeder JL, Teal SB. Rapid repeat pregnancy in adolescents: do immediate postpartum contraceptive implants make a difference. Am J Obstet Gynecol. 2012 Jun;206(6):481 e481–487. doi: 10.1016/j.ajog.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 11.Grimes DA, Lopez LM, Schulz KF, Van Vliet HA, Stanwood NL. Immediate post-partum insertion of intrauterine devices. Cochrane Database Syst Rev. 2010;5:CD003036. doi: 10.1002/14651858.CD003036.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Kapp N, Curtis KM. Intrauterine device insertion during the postpartum period: a systematic review. Contraception. 2009 Oct-/80(4):327–336. doi: 10.1016/j.contraception.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 13.Whitaker AK, Endres LK, Mistretta SQ, Gilliam ML. Postplacental insertion of the levonorgestrel intrauterine device after cesarean delivery vs. delayed insertion: a randomized controlled trial. Contraception. 2014 Jun;89(6):534–539. doi: 10.1016/j.contraception.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Gariepy AM, Duffy JY, Xu X. Cost-Effectiveness of Immediate Compared With Delayed Postpartum Etonogestrel Implant Insertion. Obstet Gynecol. 2015 Jul;126(1):47–55. doi: 10.1097/AOG.0000000000000907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodriguez MI, Caughey AB, Edelman A, Darney PD, Foster DG. Cost-benefit analysis of state- and hospital-funded postpartum intrauterine contraception at a university hospital for recent immigrants to the United States. Contraception. 2010 Apr;81(4):304–308. doi: 10.1016/j.contraception.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Washington CI, Jamshidi R, Thung SF, Nayeri UA, Caughey AB, Werner EF. Timing of postpartum intrauterine device placement: a cost-effectiveness analysis. Fertil Steril. 2015 Jan;103(1):131–137. doi: 10.1016/j.fertnstert.2014.09.032. [DOI] [PubMed] [Google Scholar]
- 17.Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65(RR-3):1–104. doi: 10.15585/mmwr.rr6503a1. [DOI] [PubMed] [Google Scholar]
- 18.Long-acting reversible contraception: implants and intrauterine devices. Practice Bulletin No. 121. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2011;118:184–96. doi: 10.1097/AOG.0b013e318227f05e. [DOI] [PubMed] [Google Scholar]
- 19.Immediate Postpartum LARC. Available at: http://www.acog.org/About-ACOG/ACOG-Departments/Long-Acting-Reversible-Contraception/Coding-and-Reimbursement-for-LARC/Reimbursement-Resources-for-Postpartum-LARC-Initiation. Accessed on 7/15/2016.
- 20.Moniz MH, Dalton VK, Davis MM, et al. Characterization of Medicaid policy for immediate postpartum contraception. Contraception. 2015 Dec;92(6):523–531. doi: 10.1016/j.contraception.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 21.Kroelinger CD, Waddell LF, Goodman DA, et al. Working with State Health Departments on Emerging Issues in Maternal and Child Health: Immediate Postpartum Long-Acting Reversible Contraceptives. J Womens Health (Larchmt) 2015 Sep;24(9):693–701. doi: 10.1089/jwh.2015.5401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moniz MH, Chang T, Davis MM, Forman J, Landgraf J, Dalton VK. Medicaid Administrator Experiences with the Implementation of Immediate Postpartum Long-Acting Reversible Contraception. Womens Health Issues. 2016 Feb 26; doi: 10.1016/j.whi.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 23.Holland E, Michelis LD, Sonalkar S, Curry CL. Barriers to Immediate Post-placental Intrauterine Devices among Attending Level Educators. Womens Health Issues. 2015 Jul-Aug;25(4):355–358. doi: 10.1016/j.whi.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 24.Births: Final Data for 2013. National Vital Statistics Reports. 64(1) Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_01.pdf. Accessed on August 24, 2015. [PubMed] [Google Scholar]
- 25.The American College of Obstetricians anf Gynecologists. Committee Opinion Number 586. Health Disparities in Rural Women. http://www.acog.org/-/media/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/co586.pdf?dmc=1&ts=20150824T0825590493. Accessed on August 24, 2015.
- 26.Immediate postpartum long-acting reversible contraception. Committee Opinion No. 670. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2016;128:e32–7. doi: 10.1097/AOG.0000000000001587. [DOI] [PubMed] [Google Scholar]
- 27.Position Statement. American College of Nurse-Midwives; Reproductive Choices. Available for download at: http://midwife.org/index.asp?bid=59&cat=3&button=Search. Accessed on October 12, 2016. [Google Scholar]
- 28.Chen BA, Reeves MF, Creinin MD, Schwarz EB. Postplacental or delayed levonorgestrel intrauterine device insertion and breast-feeding duration. Contraception. 2011 Nov;84(5):499–504. doi: 10.1016/j.contraception.2011.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dahlke JD, Terpstra ER, Ramseyer AM, Busch JM, Rieg T, Magann EF. Postpartum insertion of levonorgestrel–intrauterine system at three time periods: a prospective randomized pilot study. Contraception. 2011 Sep;84(3):244–248. doi: 10.1016/j.contraception.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 30.Hayes JL, Cwiak C, Goedken P, Zieman M. A pilot clinical trial of ultrasound-guided postplacental insertion of a levonorgestrel intrauterine device. Contraception. 2007 Oct;76(4):292–296. doi: 10.1016/j.contraception.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 31.Çelen Ş, Möröy P, Sucak A, Aktulay A, Danışman N. Clinical outcomes of early postplacental insertion of intrauterine contraceptive devices. Contraception. 2004;69(4):279–282. doi: 10.1016/j.contraception.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 32.Levi E, Cantillo E, Ades V, Banks E, Murthy A. Immediate postplacental IUD insertion at cesarean delivery: a prospective cohort study. Contraception. 2012 Aug;86(2):102–105. doi: 10.1016/j.contraception.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 33.Lopez LM, Bernholc A, Hubacher D, Stuart G, Van Vliet HA. Immediate postpartum insertion of intrauterine device for contraception. Cochrane Database Syst Rev. 2015;6:CD003036. doi: 10.1002/14651858.CD003036.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The LARC Program. American College of Obstetricians and Gynecologists; Immediate Postpartum LARC Resource Digest. Available at: https://www.acog.org/-/media/Departments/LARC/IPPLARCResourceDigestReplaceable.pdf?dmc=1&ts=20160819T1326385264. Accessed on 8/19/2016. [Google Scholar]
- 35.Medicaid reimbursement for postpartum LARC by state. Available at: http://www.acog.org/About-ACOG/ACOG-Departments/Long-Acting-Reversible-Contraception/Coding-and-Reimbursement-for-LARC/Reimbursement-Resources-for-Postpartum-LARC-Initiation/Medicaid-Reimbursement-for-Postpartum-LARC-by-State. Accessed on 8/13/2016.
- 36.Center for Medicaid and CHIP Service. CMCS Informational Bulletin: State Medicaid Payment Approaches to Improve Access to Long-Acting Reversible Contraception. Available at https://www.medicaid.gov/federal-policy-guidance/downloads/cib040816.pdf. Accessed on August 13, 2016.
- 37.Aiken AR, Creinin MD, Kaunitz AM, Nelson AL, Trussell J. Global fee prohibits postpartum provision of the most effective reversible contraceptives. Contraception. 2014 Nov;90(5):466–467. doi: 10.1016/j.contraception.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dunn K, Bayer LL, Mody SK. Postpartum contraception: An exploratory study of lactation consultants’ knowledge and practices. Contraception. 2016 Jul;94(1):87–92. doi: 10.1016/j.contraception.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flanigan TS, McFarlane E, Cook S. Section of Survey Research Methods. American Association for Public Opinion Research; 2008. Conducting Survey Research among Physicians and other Medical Professionals – A Review of the Literature. Available at: https://www.amstat.org/sections/srms/proceedings/y2008/Files/flanigan.pdf. Accessed on 8/19/2016. [Google Scholar]


