Abstract
Increased attention has highlighted the role of age and sexual development on HIV risk among Black MSM (BMSM); limited focus has been given to the relationship of sexual positioning to HIV risk along the life course. This study examined BMSM’s life course sexual positioning practices and accompanying HIV/STI risks. Twenty-six Black gay and bisexual men ages 24–61 completed life history interviews in Los Angeles, California, between September and November 2015. Thematic analysis evaluated domains including major life events, substance use, social support, and partner selection. Varying exposure to HIV treatment and prevention options and venues to meet male partners revealed generational differences in sexual risks. Childhood sexual abuse and internalized homonegativity impacted personal development, sexual positioning, and condom negotiation. BMSM also assumed sexual positioning using masculinity stereotypes and body language. Clarifying the sexual development and HIV/STI risk contexts among BMSM could better inform current treatment and prevention needs.
Keywords: Sexual positioning, Black MSM, HIV risk, STI risk, culture
Introduction
According to a 2016 report from the Centers for Disease Control and Prevention (CDC), Black gay, bisexual, and other men in the U.S. who have sex with men (MSM) have a 50% lifetime risk of HIV infection [1,2]. Despite having comparable or greater proportions of prevention behaviors—condom use, HIV testing, fewer sex partners—and less drug use before or during sex [3–5], Black MSM (BMSM) are still more likely to become HIV-positive and report a history of sexually transmitted infections (STIs) than other U.S. ethnic MSM groups [4,6]. The need to focus on efforts to protect young BMSM from HIV has been widely acknowledged [7–11]. The continued disparity in HIV and STI rates among young BMSM in particular has increased attention to the role of age and sexual identity development on the sexual risk among BMSM [12–15].
Due to the differing exposures to HIV risk, prevention messaging, and changing social environments surrounding same-sex relationships among those born before and after the onset of biomedical interventions and prevention options (i.e., highly active anti-retroviral treatment [HAART] and pre-exposure prophylaxis [PrEP]) [16–18], the lives and health outcomes of BMSM are affected in part by both generational differences and age-related developmental issues. Men born prior to the 1980s came of age during the first generation of the HIV/AIDS epidemic and witnessed the terminal consequences of infection, since most people came to medical attention in the later stages of disease and when effective treatments were unavailable. Comparatively, those born during and after that time witnessed a different epidemic in which the disease became increasingly treatable and subsequently more preventable. Regarding sexual identity development, younger cohorts of MSM are currently developing during a time in which social and structural changes such as legalization of same-sex marriage might reflect a more tolerant social climate regarding same-sex relationships [18,19], and could impact gay and bisexual identification. Given these generational differences, young MSM might be more likely to engage in risk behaviors due to feelings of HIV not being as lethal as it was initially, coupled with their increased ability to meet partners and develop relationships [18,20–22]. Younger age has also been associated with sexual risk taking [10,23–25]. Generational differences in exposure to risk, changing messages about HIV risk and same-sex relationships, and age-related sexual behaviors create differing sexual risk profiles among different cohorts of BMSM. It seems appropriate and timely, then, that we explore the social and sexual lives of BMSM with a life course lens.
Behavioral risks for acquiring or transmitting HIV and STIs via condomless sex vary by sexual positioning practices. Specifically, men who practice condomless receptive anal intercourse (RAI) with male partners are more likely to acquire HIV and rectal STIs than men who only participate in condomless insertive anal intercourse (IAI) with male partners [26–29]. Men who practice both “top” (i.e., insertive) and “bottom” (i.e., receptive) roles for anal sex (also referred to as “versatility”) are at high risk for HIV and STI infection via RAI and could also potentiate subsequent risk for HIV and STIs to male partners through IAI [30–33]. The range of contexts for versatility create ample opportunities for HIV and STI transmission. Some men might practice RAI and IAI within the same sexual encounter with the same partner, practice RAI and IAI in different sexual acts with the same partner, or practice RAI with certain types of male partners and IAI with other types of male partners [33]. Sexual positioning practices and versatility are therefore relative to contexts within individual sexual encounters. Within sexual encounters, sexual positioning practices are also influenced by a range of factors that potentially create power dynamics, including age, partner type, and masculinity stereotypes such as body and penis size and relative “femininity” (as described by MSM) [33–37]. Sexual positioning within some same-sex relationships is influenced by top and bottom relational dynamics [34,35,38]. Specifically, some MSM who were the receptive partner assumed risk during the sexual relationship and relinquished the responsibility of initiating condom use to their partners who “top” them [34,35]. Some MSM, who gave their partners the responsibility of initiating condom use, waived their negotiation ability in part for the pleasure of their partners, although other MSM who were the receptive partners managed their role as the “pleasure producer” to successfully negotiate condom use [34]. Versatility can lead to shared power between MSM [33,35,38,39]. Data also showed that some MSM changed sexual positioning preferences over the course of their lives due in part to time, personal growth, and relationship development, which has implications for sexual risk over the life course of BMSM [40].
Life Course Theory and the HIV Risk Environment
Little attention has been focused on how sexual positioning practices and sexual risk manifest along the life course of BMSM, given the varying generational exposures to HIV risk and prevention messaging. Life Course Theory (LCT) and Rhodes’ (2002) “risk environment” framework provide useful foundations for exploring sexual behaviors and outcomes as a result of a dynamic process involving historical, social, and environmental contexts, and individual behavior [17,41–44]. Both frameworks have been used to focus on how social, environmental, and structural factors increase HIV risk among drug users [44–49]. This has important theoretical implications for understanding the sexual risk of BMSM. LCT posits that behaviors and outcomes are the result of the individual, the environment, and time, and include key constructs of timing, trajectories, transitions, and critical periods [17,50]. The risk environment framework has been extended to consider the role of the environment for sexual risk for HIV [51–54]. For example, some of the discussion of the sexual ‘risk environment’ for MSM has noted the places where MSM meet and have sex, including bath houses [51], sex parties [55], and online (via the Internet or mobile social networking apps) [52,54]. However, there is a dearth of information related to how age-related differences in exposure to HIV and social climates regarding same-sex relationships might be useful in exploring sexual positioning practices and sexual risk for HIV and STIs among BMSM.
The present study is informed by the conceptual model posited by Dangerfield II et al. (2016) that described sexual positioning practices and HIV/STI risk as influenced by distal and proximal variables that create power dynamics within sexual encounters among MSM. Specifically, that model suggested that factors including age, masculinity stereotypes (e.g., penis size, relative body size), partner type, HIV status, and race/ethnicity could affect sexual positioning preferences and individual ability to negotiate sexual preferences and condom use with partners. The model also suggested how the interplay of those factors and the latitude an individual has to negotiate sexual positioning and condom use are related. This dynamic and cyclical relationship subsequently results in RAI or IAI practice, ultimately leading to varying HIV and STI risk [33]. The present study explored sexual risk among BMSM along the life course to identify developmental pathways of sexual risk and contexts for sexual positioning practices. Exploring the contexts of sexual positioning practices using a life course perspective is a timely and much needed approach to understanding and preventing the transmission of HIV and STIs among BMSM. Examining the contexts of sexual positioning practices with a life course perspective could also provide insights into ways sexual health interventions for BMSM should be enhanced.
Methods
In-depth qualitative interviews were conducted with 26 Black gay and bisexual men in Los Angeles, California, from September to November 2015. Individuals were recruited using active and passive recruitment methods. Active recruitment methods included targeting gay clubs and social support group meetings throughout Los Angeles where BMSM were known to frequent and providing study information at random. Passive recruitment included distributing fliers at similar venues and advertising the study on Craigslist. Interested individuals made an appointment with the principle investigator and study coordinator (i.e., the first author) and were screened for eligibility at the research study site, REACH LA, a community-based organization in downtown Los Angeles. Participants were eligible based on the following criteria: self-identifying as Black or African American, being ≥18 years of age, and reporting oral or anal sex practice in the previous six months with at least one male partner.
Participants were asked to provide government-issued identification to verify age. Eligible participants provided written informed consent and were interviewed at the study site. In-depth life history interviews were guided by LCT constructs. Interviews probed domains related to the participants’ personal development, sexual history, STI history, substance use, social and economic support, and knowledge and attitudes about HIV (Table 1). Questions related to personal identity development, social and economic support, and exposure to same-sex relationships and HIV prevention messaging were asked for each phase of life from birth to present day in five-year periods.
Table 1.
Domains covered under Life Course Theory (LCT) constructs for in-depth qualitative interviews
| LCT Constructs | Domains Covered |
|---|---|
| Timing-when behavior starts | When is oral/anal sex practice initiated? Under what contexts? If bisexual, are these practices different with women? What impacts (impacted) initiation of IAI and/or RAI practice? What role do drugs and alcohol play? |
| Time- behaviors over time | How does sexual positioning develop over time? |
| Trajectories-sequence of events behaviors and outcomes | How do goals and values influence decision-making around sex practice? How do life situations (e.g. outness, resource stability, age, partner type) influence decision-making around sexual practices? |
| Transitions-highlight key life events | What personal events trigger changes in sexual practice? |
| Critical periods-vulnerabilities that may be heightened | How did (does) independence (or lack thereof) affect sexual decision making? |
Interviews also assessed the timing of sexual debut, potential substance use debut, incarceration history, and potential housing instability. The events surrounding those incidents were explored and interviews inquired about repetitions in behaviors (i.e., sexual activities, substance use, incarceration, homelessness) over different five-year life phases.
To encourage participants to think critically about the events that could have influenced their life course trajectory, probes to capture key life events and explore risk outcomes included open-ended questions such as “What do you think led to that?’ and “How was the next phase of your life different from the one(s) we just discussed?” At the end of the interview, participants were asked “Is there anything else that we haven’t talked about that you think is important in understanding your life now?” Interviews ranged from 55 minutes to 2.5 hours. Study procedures were reviewed and approved by the University of Southern California Health Sciences Campus Institutional Review Board.
Qualitative Data Analysis
Interviews were audio-recorded and transcribed verbatim. Two coders (including the first author) read all transcripts to identify overarching themes, looking for repetitions across interviews; they developed a codebook listing each theme. Themes were identified by either patterns that were associated with specific questions, or expressions that provided examples of questions and concepts [56–58]. Transcript coding was conducted using Atlas.ti 7.1 (2016). Areas of text related to each theme for the first three interviews were coded independently by the two coders and inter-rater reliability was measured to ensure consistency between transcript coding (Kappa ≥ 0.70). Inter-rater reliability was measured twice to confirm coding consistency; inconsistencies were reviewed and showed minor differences in the lengths of quoted text but not overall quality of text. Team members then reviewed all coded text, examined the most frequently mentioned themes, and then selected those that were related to HIV, sexual positioning preferences, dynamics leading to sexual positioning practices, and condom use.
After collectively discussing this initial coding, the team created a code library and reviewed the remaining qualitative data, with new codes being created as needed. The team then identified key themes based on frequency and depth of discussion, presence across multiple formative research data sources, and interconnection to other themes. Data presented in this study represented the range of themes related to age-related differences in the factors that affected sexual positioning practices and HIV/STI risk along the life course of BMSM.
Timelines
After the in-depth interviews, a timeline diagram of life events was created for each participant detailing historical events related to HIV treatment and prevention options, major life events, changes in partner types, sexual positioning practices, and HIV/STI outcomes. The timeline diagrams provide a valuable resource in analysis that not only helps identify patterns in the life history data [47], but also highlight how a dynamic relationship between historical context, personal development, and individual sexual encounters might combine to facilitate sexual risk and HIV/STI outcomes among BMSM (Figure 1).
Figure 1.
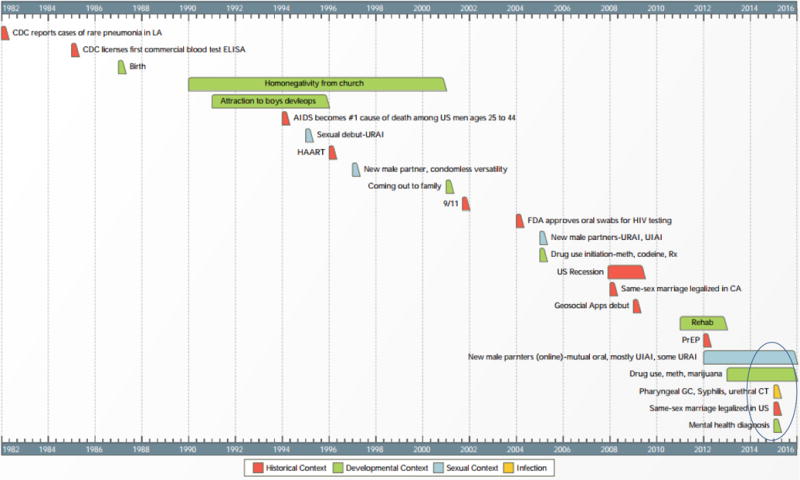
Example timeline of life events and developmental path of sexual risk using Life Course Theory and Risk Environment frameworks
Results
Demographic characteristics
The average age of participants was 40.7 years (range 24-61 years); 8 were age 30 or younger; 18 were over the age of 30. In the quantitative survey, the plurality (69.2%) of participants identified as gay; the remaining 30.8% identified as bisexual. Most participants were single or not in a committed relationship (19, 73.1%). Regarding sexual positioning preferences, 57.7% identified “top” as their preference, 1 (3.9%) preferred “bottom,” and four (15.4%) preferred “versatility.” Other participants identified “versatile bottom” (15.4%; someone who practices IAI most of the time and sometimes practices RAI, depending on the context) and “versatile top” (7.2%; someone who practices RAI most of the time and sometimes practices IAI, depending on the context) as their sexual role preference [33,59–61]. Regarding STI history, seven (26.9%) reported a history of gonorrhea infection and five (19.2%) reported a history of syphilis infection. Seven (26.9%) participants self-reported being HIV-positive (Table 2). Of note, 71.4% of the participants who self-reported being HIV-positive reported ever having a history of STI infection; seven (36.8%) who self-reported being HIV-negative or status unknown reported ever having a history of STI infection.
Table 2.
Demographic characteristics, STI history, and childhood sexual abuse history among Black gay and bisexual men in Los Angeles, CA 2015 (n=26)
| n (%) | |
|---|---|
| Age (years) | |
| Mean (Range) | 40.7 (24-61) |
| ≤ 30 | 8 (30.8) |
| > 30 | 18 (69.2) |
| Annual Income | |
| <$20,000 | 17 (65.4) |
| Between $20,000 and $30,000 | 4 (15.4) |
| Between $30,000 and $40,000 | 3 (11.5) |
| Over $40,000 | 2 (7.7) |
| Sexual Orientation | |
| Homosexual/gay/same gender loving | 18 (69.2) |
| Bisexual | 8 (30.8) |
| Partnership Status | |
| Single or not in a committed relationship | 19 (73.1) |
| In a committed relationship | 4 (15.4) |
| In an open relationship | 3 (11.5) |
| Sexual Role Preference | |
| Bottom | 1 (3.9) |
| Versatile Bottom | 4 (15.4) |
| Versatile | 4 (15.4) |
| Versatile Top | 2 (7.7) |
| Top | 15 (57.7) |
| STI History Ever | |
| Gonorrhea | 7 (26.9) |
| Chlamydia | 6 (23.1) |
| Syphilis | 5 (19.2) |
| Herpes | 1 (3.9) |
| STI History Previous Three Months | |
| Gonorrhea | 0(0.0) |
| Chlamydia | 1 (3.9) |
| Syphilis | 2 (7.7) |
| Self-reported HIV Status | |
| HIV-negative | 18(69.2) |
| HIV-positive | 7(26.9) |
| Don’t know/Not Sure | 1(3.9) |
| Reported History of Childhood Sexual Abuse | 11 (42.3) |
Emerging Themes
Overall, interviews yielded themes related to generational differences in HIV exposure, venues to meet partners, same-sex relationship exposure, developmental trajectories of risk, and factors within sexual encounters that impacted risk and HIV/STI outcomes between cohorts and along the life course of each group. Specifically, interviews showed how differences in exposures to HIV infections, treatment options, prevention information, and abilities to meet same-sex partners and develop relationships influenced varying risks between cohorts and along the life course.
For both cohorts, major life events such as childhood sexual abuse, battling homonegative messaging from churches in their youth, and age-related personal development influenced the participants’ ability to negotiate risk within same-sex sexual relationships. Additionally, dynamics within individual sexual encounters also created opportunities for risk because the men relied on body language and partner type to help inform sexual positioning practices. Participants also described how substance use and partner attraction impacted the relationship between their preferences for positioning and their ultimate sexual practices. Themes are reported in the following section with quotes that illustrate participants’ reflections on sexual positioning practices and sexual risk along the course of their lives.
Generational Differences: HIV Prevention Messaging, Same-Sex Relationship Development, and Venues to Meet Partners
HIV Prevention Messaging
Participants suggested that differences in exposure to community HIV infections and HIV prevention messaging contributed to their sexual risk-taking. Participants over the age of 30 mentioned that their patterns of condomless sex had begun during their teenage sexual debut. This was principally due to lack of knowledge regarding the full utility of condoms with male partners, as messages about condom use primarily targeted pregnancy prevention, not necessarily HIV prevention. When asked about the role of condoms in his sexual experiences as a teenager, one participant, aged 33, who reported condomless versatility practices and disclosed being HIV-positive, said:
Well, what’s interesting is, being that I didn’t ever heard nothing about HIV, I didn’t know what the point of condoms were. I know that you always hear, “Make sure you wear a condom,” dah, dah, dah, but then the only thing I ever heard about condoms in the past was it prevents pregnancy, you know what I mean, “Okay, make sure you put that on so you don’t get no babies,” and I’m like, “Well, two guys can’t have no babies,” so I didn’t think it was a big deal. I didn’t know anything about that, I didn’t know anything about STDs and stuff, I just wasn’t educated about that stuff.
Similarly, when asked about his early sexual experiences, another participant, age 60, who reported IAI preference and a history of gonorrhea infection, mentioned, “Condoms wasn’t a, [laughter] that wasn’t a household word back then [laughter]. That wasn’t, you know, it wasn’t like you can go now and you get condoms anywhere for free. None of that was going on.” Other participants also mentioned sociohistorical events such as Magic Johnson’s HIV disclosure as a turning point in their knowledge and awareness about their own HIV risk. One participant, age 51 mentioned:
People started using condoms when motherfuckers was catching AIDS, you know, like Magic, whenever that it got to that point, you know what I mean. Now it’s died down, not in the gay community but in other communities such as heterosexual and whatnot, it’s died down. I don’t know if you observed that but if you mention HIV right now to a heterosexual, he won’t give it the time of day to think about it compared to if you mention it to a person who’s gay.
Older participants in particular reflected on how generational differences in HIV prevention messaging impacted their condom use, and ultimately, their sexual risk.
Same-Sex Relationship Development
Younger participants (age 30 and under) mentioned that the pursuit of long-term relationship partners increased their willingness for condomless sex, regardless of sexual positioning preferences. When asked about his condomless versatility practices, one participant in particular (age 28) reported crystal meth use during sex and mentioned that he willingly participated in condomless sex while using drugs or drinking because of a personal desire to assess partners for long-term relationships. When asked if his condom use was related to his substance use, he said:
I’ve used condoms when I’ve been on crystal. I think that I wasn’t using condoms because I was trusting the other person. Because I wanted to [trust the other person], and then maybe I didn’t want to use condoms either, low key…
Following up with a question about whether attempts to establish trust through condomless sex was related to seeking a long-term romantic partner, he quickly responded, “Yes. Definitely. That’s really the main goal to all of this is to find a long-term partner…it’s the intimacy level, you know…”
Another mentioned, “I really am like a relationship person, like I don’t have too many crazy stories about like all these boys…so for me in a relationship, it’s like serious for me. So in a relationship you’re not using condoms.” Most of the commentary involving desire for long-term partnerships came from younger participants who mentioned sexual risk-taking in search of ideal sexual or romantic partners. Statements like this could be the result of generational differences in exposure to same-sex relationships that might impact sexual risk among the differing cohorts of BMSM.
Venues to Meet Partners
Older participants also suggested that having a limited range of places/venues that allowed them to meet other men socially or sexually when they were younger increased their sexual risk at that time. When asked about how he met potential sexual partners when he was younger, one participant, age 35, mentioned meeting sexual partners on the “party line,” an anonymous phone line
…where everybody come, it’s like, you know, like, like, you know, now they got sites and stuff you go to, yeah. Back then they didn’t have sites and computers, they, they had a party line phone number where you called the number and everybody in LA, you know, be on there and that’s how you meet and stuff… just judge, judge by people what you just talk to them on the phone and then you guys just meet up and then and it goes from there, so…
The men who described meeting people on the “party line” described how meeting potential partners was a risk due to the anonymous nature of meeting people over the phone. The oldest participants (age 56) also mentioned meeting male partners and having condomless sex with them in outdoor parks simply because in the past “that’s all we had.” While older participants suggested that the limited range of venues to meet partners increased their risk-taking, data did not clarify whether places such as parks were the only option for venues to have sex compared to someone’s home which could have been safer.
Developmental Trajectories: Childhood Sexual Abuse, Homonegative Messaging from Churches, and Age-Related Personal Development
Interviews also yielded themes related to how major events during childhood, sexual identity development, and personal identity development contributed to sexual risk across cohorts and along the course of men’s lives, regardless of sexual positioning preferences.
Childhood Sexual Abuse
Across cohorts, childhood sexual abuse was a salient theme that participants mentioned affected their ability to negotiate risk within sexual relationships; 11 (42%) participants mentioned childhood sexual abuse (i.e., a male or female fondling them or forcing them to engage in intercourse) prior to the age of 12. Some of these participants explicitly linked their willingness to participate in relationships in which they did not always practice their sexual positioning preference to their history of sexual abuse. One participant described a sexual relationship in which he was occasionally able to maintain his IAI preference; however, because of his financial dependence upon the partner, he was sometimes influenced to “bottom” and to forgo the use of condoms, even though he did not want to. He put it this way:
…I think it [referring to childhood sexual abuse] affected me…just to be able to accept and, and to, and to know that, just, just being open to tragedy, like tragedy is not really a tragedy, it happened because, it’s happening because there’s a reason. It’s a cause and an effect, you know…Yeah, it’s almost like déjà vu.
Reflections such as this showed how some participants were primed for sexual risk-taking due to childhood trauma.
Homonegative Messages from the Church
Another salient theme involving major events during childhood included a history of experiencing the church as homonegative, which led participants to have internal conflicts about their sexuality and subsequently use drugs as a coping strategy. When asked about his sexual history and drug use debut, one participant mentioned:
It had to do with the, you know, the church…so in return it just was causing me to be depressed and it caused me to use drugs even more to just not even want to feel the, the emotions and the feelings of that…drugs was really my own way to just not feel the effects that I was not moving forward because I was not keeping it real with myself.
Comments such as this suggested how exposures to social stigma from the church added to a foundation during development that might have influenced their sexual risk-taking.
Age-Related Personal Development
Across age cohorts, participants also mentioned that increasing age influenced their condom use, regardless of sexual positioning preferences. Specifically, participants stated that as they got older, they matured their perspective and increased attention to their sexual health. Some mentioned that their teenage sexual debut and sexual encounters thereafter were without condoms simply because
When you’re that young, you don’t see the point of condoms until you start getting older. I was 14, 13, or 14. You don’t start seeing the importance of condoms [until] when you get older you, you know, people catching AIDS and all these different diseases.
Participants also described how increasing age changed their perspective about their lives in general, not limited to their sexual health. When asked how they decided to increase their condom use as they got older, participants mention in a similar manner:
I mean, you get older, you think about things you don’t normally think about. I was more protective of myself in my 30s than I was in my 20s because I was older, I was, that’s the only thing I can say.
Interviews alluded to a developmental trajectory of sexual risk or safety that was linked to age and time, as participants mentioned being more mindful managing their sexual health as they got older.
Older participants explicitly described how attempts to connect with partners in their youth affected their sexual positioning practices. Some participants mentioned that while they were trying to develop relationships with male partners during their sexual debut and early sexual identity development, they attached emotional meaning to the sexual positioning preferences of their partners. When asked about his preference to “top” partners when he was younger, one participant mentioned:
I enjoyed it, but I felt that people wanted me more if they topped me, so that’s why I would let them do that more, because it felt like they were more connected to me in that way. You know what I mean, it’s like, it seemed like at that point, if, meaning I let most people dictate situations, it really more so was like this means that they want me more if I do this, so I started positioning my mindset and stuff to where that was more, I usually did more.
Participants who shared reflections about feeling more desirable if they engaged in partner preferences also shared details about histories of childhood sexual abuse, or feelings of abandonment from absent parents in their childhood. One participant described how this dynamic led him to condomless RAI practice with partners, ultimately leading to HIV infection. Participants also referenced how their level of empowerment in maintaining preferences for sexual positioning in sexual encounters and relationships increased as they got older, particularly with regard to “top” practices. They mentioned how as they got older:
I guess…just learning that I don’t have to do what somebody else wants me to do…and then, if I don’t like getting fucked, although I did do it, and as I got older it wasn’t even about top or bottom to me, it was about good sex.
Here, participants did not necessarily describe differences in “top” and “bottom” practices as their personal empowerment increased per se, although comments such as this particularly referenced maintaining preferences to “top” partners even if their partners wanted them to “bottom.” These comments could also reflect the effects of age on sexual practices, not necessarily cohort status.
Individual Sexual Encounters and Risk: Body Language, Masculinity Stereotypes, Partner Type, Substance Use, and Partner Attraction
Across cohorts, participants described how within sexual encounters along the course of their lives they relied on body language and masculinity stereotypes to help inform their sexual positioning practices. They suggested that these cues allowed them assume sexual positioning practices without necessarily verbally communicating or negotiating with partners. One put it this way:
Yeah, that was when I was like, okay, I kind of like verse, you know, versing, it was still more like on a vibe with a partner, you know, or how I was feeling at that time…and then feeling the vibe, “Okay, this person’s a bottom so I’m going to be a top, and I feel more comfortable being a top with them.” So, yeah, just basically the vibe with a partner still at that time or how I’m feeling, or the one of the two.
Comments about relying on body language or the “vibe” to assume their partners’ preferences and subsequent sexual positioning were salient among men in this sample. Regarding masculinity, participants across cohorts mentioned how they assumed the role of “the bottom” when they perceived their partner as “hood,” “thuggish,” or “muscular.” They assumed that these kinds of partners would not want to be the receptive partner, and thus assumed that role themselves.
Participants also described how partner type, substance use, and partner attraction also influenced their sexual positioning decision-making. They suggested that being in a romantic relationship or being very attracted to someone increased their willingness to practice their partner’s positioning preference. Additionally, they suggested that drug or alcohol use increased their willingness to practice their partner’s positioning preference and condomless sex for the sake of maintaining the flow of the sexual encounter. Participants described histories of condomless IAI and condomless RAI coupled with drug use during their sexual relationships, which facilitated lack of condom use regardless of sexual positioning preference. Participants did not describe how their personal or partners’ HIV status influenced their sexual positioning practices, regardless of whether or not they were using drugs or alcohol.
Conceptual Model of Study Results
A conceptual model is provided to highlight how the factors presented above would fit into the pre-existing model developed of sexual positioning and HIV/STI risk (Figure 2). As suggested in Figure 2, there are independent contexts that can combine to facilitate risk for HIV infection and STIs. Specifically, social and medical events in history (i.e., historical events: community HIV prevalence, HIV treatment and prevention options, same-sex stigma/acceptance), coupled with individual personal development (i.e., developmental context: age-related development, sexual development) and the dynamics within individual sexual encounters (i.e., sexual context: unspoken cues leading to RAI and IAI, condom/PrEP use) create a syndemic effect on HIV/STI risk and outcomes of BMSM.
Figure 2.
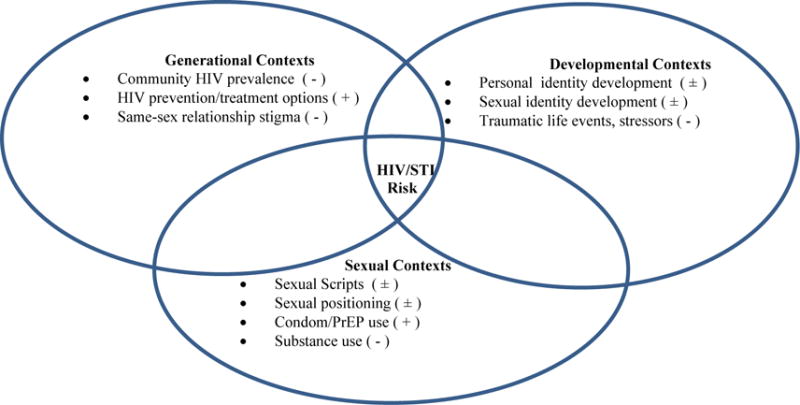
Conceptual model of the intersection of life course-related themes and the HIV risk environment framework on HIV and STI outcomes for Black MSM
(+) – indicates potentially protective contextual factors
(−) – indicates potentially risky contextual factors
(±) – indicates potentially both protective and risky factors
Discussion
This study explores how sexual positioning practices and sexual risk manifest using a life course perspective among BMSM. Our findings suggest that a combination of generational differences, traumatic childhood events, age-related identity development, and dynamics within individual encounters impact risk. Generational differences that impacted risk among older participants included varying HIV prevention information and limited availability of venues to meet partners. For the younger group, having the ability and desire to develop long-term relationships with male partners impacted condomless sex, which could be linked to the legalization of same-sex marriage in the U.S. and the changing social climate toward same-sex relationships. Across age cohorts, personal development accompanying age, childhood sexual abuse, and homonegative messaging from the church impacted men’s ability to negotiate and maintain sexual positioning preferences in sexual relationships with male partners.
Additionally, factors within sexual encounters—unspoken body language, partner type, substance use, and partner attraction—impacted the relationship between preferences and sexual positioning practices. Findings suggest that themes impacting the sexual risk behaviors and outcomes of BMSM could result from both cohort effects and age effects. Other research has also alluded to similar effects [18,62]. Specifically, younger cohorts of MSM had the highest prevalence of HIV testing, and the number of lifetime sexual partners decreased by birth cohort as well [18].
Results from the present study suggest that risk for HIV and STIs could be impacted by a syndemic effect from generational, social, developmental, and sexual contexts (Figure 2). Other research has found that early life events, developmental stages, and sociopolitical climate impact the trajectory of risk for BMSM [63–65]. Along with this effect, epidemiological risk also changes due to the different HIV prevalence among the two cohorts. Younger age among BMSM has been associated with condomless RAI [10,66] and HIV/STI infection [10,67]. The findings of the present study show how both generational and age differences relate to behavior, development, HIV prevalence, and impact risk for BMSM.
Given the historical relationship of medical mistrust and inequities in healthcare treatment among Black Americans, this research has important clinical implications for BMSM as well as medical healthcare providers [9,68,69]. Given the varying contexts for sexual positioning practices, providers should ensure that they inquire about RAI practices to ensure proper STI screening among BMSM.
The knowledge and comfort level of healthcare providers in evaluating same-sex sexual behaviors can be a barrier to STI screening [70,71] and ultimately to HIV/STI prevention. Moreover, many young BMSM do not always feel comfortable disclosing same-sex practices to providers [9,72,73]. Lack of disclosure of sexual behaviors could perpetuate an unproductive cycle of patients not engaging in health care, providers not asking appropriate questions, and discomfort among both parties. Findings would also be useful for psychologists and other mental health providers. The life course perspective aligns with standard intake procedures for psychotherapy [74–76], and the concepts in this study could guide therapists to the major domains and events that could be impacting clients in ways that are not yet obvious to the client themselves. Therapists could also potentially develop and utilize patient life course timelines as a tool in sessions or for clinical notes so that both parties could unpack the clients’ path to their current behaviors and health outcomes. The insight of men who were able to connect early life events to current behaviors suggests that addressing underlying traumatic stress and psychological constructs involving self-efficacy, coping, and decreasing dissociation during sex should be important interventions to implement for this group.
Introducing both patients and providers to the concepts that have been learned from this study provides an additional opportunity to optimize health outcomes among Black gay, bisexual, and other MSM through not only cultural but also structural competency [77]. Structural competency refers to recognizing how social and psychological factors such as same-sex marriage, gay identity development, and childhood trauma influence patient-clinical interactions and considering more systemic interventions [77,78]. Introducing and clarifying the wide range of contexts that inform HIV and STI risk among BMSM to patients and providers could have an important impact on the current treatment and prevention needs of BMSM.
The findings of this study also provide an opportunity to consider the role of sexual positioning practices in sexual communication interventions within same-sex dynamics to increase MSM’s ability to articulate preferences and negotiate risk. Communication of sexual role preferences could be nested within HIV-disclosure and/or PrEP disclosure skills, and sexual negotiation could be nested within condom use negotiation skills. Of note, the present study did not explicitly explore the influence of PrEP or condom use on sexual positioning practices. However, participants who expressed PrEP interest or uptake did not describe its influence on their decision-making. Currently, only one of the evidence-based behavioral interventions that have been identified by the CDC specifically addressed the role of “tops” and “bottoms” in same-sex dynamics for BMSM [79]. Behavioral interventions have not adequately explored the wide range of contexts for sexual positioning that lead some BMSM into occasionally unwanted and unconscious versatility practices. Data have shown that introducing concepts of self-efficacy, sexual communication, and risk negotiation might help BMSM manage risk related to sexual positioning [79]. Adding sexual preference topics could also complement trauma, coping, and empowerment interventions.
Of note, childhood sexual abuse was a salient theme in this sample, which participants often linked to their condomless sexual practices, compromise with partners, and substance use. Research has demonstrated that MSM who experienced childhood sexual abuse were more likely to engage in condomless anal intercourse [80–82]. The interplay of childhood sexual abuse with the other psychosocial forces that facilitate risk contributes to a syndemic for BMSM [82,83]. Given the salient nature of childhood sexual abuse in this and other studies of BMSM [4,82,84], interventions should target BMSM who have experienced childhood sexual abuse or similar childhood trauma. More focus on childhood trauma in the sexual risk of BMSM is needed.
Regarding the conceptual model from Dangerfield II et al. (2016), these data support that sexual positioning practices might be influenced by relative dynamics in individual encounters including masculinity stereotypes, partner type, and substance use. Participants in this study alluded to how dynamics within sexual encounters impacted their ability and willingness to communicate sexual role preferences and negotiate condom use, as the model suggests. Findings from the present study add to the concepts from the narrative review by including partner attraction, the impact of major life events, and personal development on ultimate “top” and “bottom” behaviors; however, more distal concepts of how individual and partner HIV status and partner race inform ability to negotiate sexual positioning preferences and condom use did not emerge as themes in this study.
There are limitations to consider with this study. The study sample size was small and was not representative of all BMSM; many were low-income and substance-involved, and all of the men in this study identified as either gay or bisexual. All data were self-reported. In addition, single interviews were conducted and some qualitative studies have suggested that multiple interviews with participants improve participant candor and disclosure [59–61].
Still, this research provides important insights into the lives and health trajectories of Black gay, bisexual, and other MSM. This study highlights the distinctions and interplay between differences related to generational cohort, the different societal contexts in which BMSM are engaging, versus individual-level changes related to age-related development. Future research might expand the findings of this study and utilize a life course framework to assess individuals’ access and relationship to healthcare along different phases of development, especially during vulnerable phases such as adolescence when their sexual debut occurs, housing transitioning (e.g., independent housing, homelessness), and substance use initiation. As seen in Figure 1, some BMSM might be more vulnerable to infections at different points of their lives. Unpacking their perceptions of and access to health care at different points of vulnerability might contribute to our understanding of how to address the changing needs of BMSM. Understanding BMSM’s relationship with healthcare environments at different points of development also enables healthcare providers to impact the sexual health trajectories of BMSM. Future efforts should consider both the independent and collective role of generational, developmental, and sexual contexts of risk on the lives and sexual health of BMSM. Effective HIV/STI prevention should not only include interventions that foster changes in individual behaviors, but also create environments conducive to individual and community level change [44].
Acknowledgments
We acknowledge and thank Greg Wilson and the staff at REACH LA for all their support as the research site for this study.
Complains With Ethical Standards: This research was funded by the National Science Foundation Graduate Research Fellowship Program (Award Year 2013). Additional support was also provided by NIDA grant K01 DA039767. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Centers for Disease Control and Prevention. Lifetime risk of HIV diagnosis in the United States [Internet] 2016 [cited 2016 Feb 28]. Available from: http://www.cdc.gov/nchhstp/newsroom/docs/factsheets/lifetime-risk-hiv-dx-us.pdf.
- 2.Hess KL, Hu X, Lansky A, Mermin J, Hall HI. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017 Apr;27(4):238–43. doi: 10.1016/j.annepidem.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flores SA, Bakeman R, Millett GA, Peterson JL. HIV risk among bisexually and homosexually active racially diverse young men. Sex Transm Dis. 2009 May;36(5):325–9. doi: 10.1097/OLQ.0b013e3181924201. [DOI] [PubMed] [Google Scholar]
- 4.Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, IV, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. The Lancet. 2012 Aug 3;380(9839):341–8. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 5.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007 Oct;21(15):2083–91. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 6.Mayer KH, Wang L, Koblin B, Mannheimer S, Magnus M, del Rio C, et al. Concomitant socioeconomic, behavioral, and biological factors associated with the disproportionate HIV infection burden among black men who have sex with men in 6 U.S. Cities. PLoS ONE. 2014 Jan 31;9(1):e87298. doi: 10.1371/journal.pone.0087298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arrington-Sanders R, Morgan A, Oidtman J, Qian I, Celentano D, Beyrer C. A medical care missed opportunity: Pre-exposure prophylaxis and young black men who have sex with men. J Adolesc Health. 2016 Dec 1;59(6):725–8. doi: 10.1016/j.jadohealth.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fields EL, Bogart LM, Smith KC, Malebranche DJ, Ellen J, Schuster MA. HIV risk and perceptions of masculinity among young black men who have sex with men. J Adolesc Health. 2012 Mar;50(3):296–303. doi: 10.1016/j.jadohealth.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arnold EA, Rebchook GM, Kegeles SM. ‘Triply cursed’: racism, homophobia and HIV-related stigma are barriers to regular HIV testing, treatment adherence and disclosure among young Black gay men. Cult Health Sex. 2014 Jul 3;16(6):710–22. doi: 10.1080/13691058.2014.905706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koblin BA, Mayer KH, Eshleman SH, Wang L, Mannheimer S, del Rio C, et al. Correlates of HIV acquisition in a cohort of black men who have sex with men in the United States: HIV Prevention Trials Network (HPTN) 061. PLoS ONE. 2013 Jul 26;8(7):e70413. doi: 10.1371/journal.pone.0070413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. CDC - HIV/AIDS - Gay and bisexual men’s health [Internet] 2014 [cited 2014 Dec 3]. Available from: http://www.cdc.gov/msmhealth/HIV.htm.
- 12.Arrington-Sanders R, Leonard L, Brooks D, Celentano D, Ellen J. Older partner selection in young African-American men who have sex with men. J Adolesc Health. 2013 Jun;52(6):682–8. doi: 10.1016/j.jadohealth.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bruce D, Harper GW, Fernández MI, Jamil OB, Adolescent Medicine Trials Network for HIV/AIDS Interventions Age-concordant and age-discordant sexual behavior among gay and bisexual male adolescents. Arch Sex Behav. 2011 Feb 3;41(2):441–8. doi: 10.1007/s10508-011-9730-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chamberlain N, Mena L, Geter A, Crosby RA. Does age matter among young black men who have sex with men? A comparison of risk behaviors stratified by age category. AIDS Educ Prev. 2016 May 31;28(3):246–51. doi: 10.1521/aeap.2016.28.3.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scott HM, Vittinghoff E, Irvin R, Sachdev D, Liu A, Gurwith M, et al. Age, race/ethnicity, and behavioral risk factors associated with per-contact risk of HIV infection among men who have sex with men in the United States. J Acquir Immune Defic Syndr 1999. 2014 Jan 1;65(1):115–21. doi: 10.1097/QAI.0b013e3182a98bae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Austin EL, Bozick R. Sexual orientation, partnership formation, and substance use in the transition to adulthood. J Youth Adolesc. 2011 Mar 16;41(2):167–78. doi: 10.1007/s10964-011-9653-7. [DOI] [PubMed] [Google Scholar]
- 17.Elder GH., Jr . Human lives in changing societies: Life course and developmental insights. In: Cairns RB, Elder GH Jr, Costello EJ, editors. Developmental science. New York, NY, US: Cambridge University Press; 1996. pp. 31–62. (Cambridge studies in social and emotional development). [Google Scholar]
- 18.Nelson KM, Gamarel KE, Pantalone DW, Carey MP, Simoni JM. Sexual debut and HIV-related sexual risk-taking by birth cohort among men who have sex with men in the United States. AIDS Behav. 2016 Feb;10:1–10. doi: 10.1007/s10461-016-1330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glick SN, Cleary SD, Golden MR. Increasing acceptance of homosexuality in the United States across racial and ethnic subgroups. J Acquir Immune Defic Syndr [Internet] 2015 Jun 26; doi: 10.1097/QAI.0000000000000740. [cited 2016 Dec 5]; Available from: https://iths.pure.elsevier.com/en/publications/increasing-acceptance-of-homosexuality-in-the-united-states-acros. [DOI] [PubMed]
- 20.Callander D, Senn C. Examining the role of relationships, body image, closeness to HIV/AIDS, and HIV optimism in the sexual risks of young men who have sex with men. J HIVAIDS Soc Serv. 2013 Apr 1;12(2):205–23. [Google Scholar]
- 21.Hammack PL, Cohler BJ. Narrative, identity, and the politics of exclusion: Social change and the gay and lesbian life course. Sex Res Soc Policy. 2011 Sep 1;8(3):162. [Google Scholar]
- 22.MacKellar DA, Hou S-I, Whalen CC, Samuelsen K, Valleroy LA, Secura GM, et al. A plausible causal model of HAART-efficacy beliefs, HIV/AIDS complacency, and HIV-acquisition risk behavior among young men who have sex with men. AIDS Behav. 2011 May 1;15(4):788–804. doi: 10.1007/s10461-010-9813-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mansergh G, Marks G. Age and risk of HIV infection in men who have sex with men. AIDS Lond Engl. 1998 Jul 9;12(10):1119–28. doi: 10.1097/00002030-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Mustanski B, Newcomb ME, Clerkin EM. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychol. 2011;30(5):597–605. doi: 10.1037/a0023858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osmond DH, Pollack LM, Paul JP, Catania JA. Changes in prevalence of HIV infection and sexual risk behavior in men who have sex with men in San Francisco: 1997 2002. Am J Public Health. 2007 Sep;97(9):1677–83. doi: 10.2105/AJPH.2005.062851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coates RA, Calzavara LM, Read SE, Fanning MM, Shepherd FA, Klein MH, et al. Risk factors for HIV infection in male sexual contacts of men with AIDS or an AIDS-related condition. Am J Epidemiol. 1988 Oct;128(4):729–39. doi: 10.1093/oxfordjournals.aje.a115026. [DOI] [PubMed] [Google Scholar]
- 27.Griensven GJPV, Tielman RaP, Goudsmit J, Noordaa JVD, Wolf FD, Vroome EMMD, et al. Risk Factors and Prevalence of HIV Antibodies in Homosexual Men in the Netherlands. Am J Epidemiol. 1987 Jun 1;125(6):1048–57. doi: 10.1093/oxfordjournals.aje.a114620. [DOI] [PubMed] [Google Scholar]
- 28.Kent CK, Chaw JK, Wong W, Liska S, Gibson S, Hubbard G, et al. Prevalence of rectal, urethral, and pharyngeal chlamydia and gonorrhea detected in 2 clinical settings among men who have sex with men: San Francisco, California, 2003. Clin Infect Dis. 2005 Jul 1;41(1):67–74. doi: 10.1086/430704. [DOI] [PubMed] [Google Scholar]
- 29.Schechter MT, Boyko WJ, Douglas B, Willoughby B, McLeod A, Maynard M, et al. The Vancouver Lymphadenopathy-AIDS Study: 6. HIV seroconversion in a cohort of homosexual men. CMAJ Can Med Assoc J J Assoc Medicale Can. 1986 Dec 15;135(12):1355–60. [PMC free article] [PubMed] [Google Scholar]
- 30.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. The Lancet. 2012 Aug 3;380(9839):367–77. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lyons A, Pitts M, Smith G, Grierson J, Smith A, McNally S, et al. Versatility and HIV vulnerability: investigating the proportion of Australian gay men having both insertive and receptive anal intercourse. J Sex Med. 2011 Aug;8(8):2164–71. doi: 10.1111/j.1743-6109.2010.02197.x. [DOI] [PubMed] [Google Scholar]
- 32.Wolitski RJ, Branson BM. “Gray area behaviors” and partner selection strategies. In: O’Leary A, editor. Beyond Condoms [Internet] Springer; US: 2002. pp. 173–98. cited 2015 Apr 21. Available from: http://link.springer.com/chapter/10.1007/0-306-47518-9_8. [Google Scholar]
- 33.Dangerfield DT, II, Smith LR, Williams J, Unger J, Bluthenthal R. Sexual positioning among men who have sex with men: A narrative review. Arch Sex Behav. 2016 May;13:1–16. doi: 10.1007/s10508-016-0738-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoppe T. Circuits of power, circuits of pleasure: Sexual scripting in gay men’s bottom narratives. Sexualities. 2011 Apr 1;14(2):193–217. [Google Scholar]
- 35.Johns MM, Pingel E, Eisenberg A, Santana ML, Bauermeister J. Butch tops and femme bottoms? Sexual positioning, sexual decision making, and gender roles among young gay men. Am J Mens Health. 2012 Nov 1;6(6):505–18. doi: 10.1177/1557988312455214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grov C, Parsons JT, Bimbi DS. The association between penis size and sexual health among men who have sex with men. Arch Sex Behav. 2009 Jan 13;39(3):788–97. doi: 10.1007/s10508-008-9439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carballo‐Diéguez A, Dolezal C, Nieves L, Díaz F, Decena C, Balan I. Looking for a tall, dark, macho man … sexual‐role behaviour variations in Latino gay and bisexual men. Cult Health Sex. 2004 Mar 1;6(2):159–71. [Google Scholar]
- 38.Dworkin SL, Zakaras JM, Campbell C, Wilson P, Grisham K, Chakravarty D, et al. Relationship power among same-sex male couples in New York and San Francisco: Laying the groundwork for sexual risk reduction interventions focused on interpersonal power. J Sex Res. 2017 Feb 16;0(0):1–13. doi: 10.1080/00224499.2017.1279258. [DOI] [PubMed] [Google Scholar]
- 39.Malebranche DJ, Fields EL, Bryant LO, Harper SR. Masculine socialization and sexual risk behaviors among black men who have sex with men: A qualitative exploration. Men Masculinities. 2009 Oct 1;12(1):90–112. [Google Scholar]
- 40.Pachankis JE, Buttenwieser IG, Bernstein LB, Bayles DO. A longitudinal, mixed methods study of sexual position identity, behavior, and fantasies among young sexual minority men. Arch Sex Behav. 2013 Oct;42(7):1241–53. doi: 10.1007/s10508-013-0090-4. [DOI] [PubMed] [Google Scholar]
- 41.Bronfenbrenner U. Contexts of child rearing: Problems and prospects. Am Psychol. 1979;34(10):844–50. [Google Scholar]
- 42.Friedman SR, Rossi D. Some Musings about big events and the past and future of drug use and of HIV and other epidemics. Subst Use Misuse. 2015 Jun 7;50(7):899–902. doi: 10.3109/10826084.2015.1018752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rhodes T. The ‘risk environment’: A framework for understanding and reducing drug-related harm. Int J Drug Policy. 2002 Jun 1;13(2):85–94. [Google Scholar]
- 44.Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005 Sep;61(5):1026–44. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 45.Arreola S, Bluthenthal RN, Wenger L, Chu D, Thing J, Kral AH. Characteristics of people who initiate injection drug use later in life. Drug Alcohol Depend. 2014 May 1;138:244. doi: 10.1016/j.drugalcdep.2014.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Friedman SR, Mateu-Gelabert P, Sandoval M. Group sex events amongst non-gay drug users: An understudied risk environment. Int J Drug Policy. 2011 Jan;22(1):1–8. doi: 10.1016/j.drugpo.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Friedman SR, Mateu-Gelabert P, Sandoval M, Hagan H, Jarlais DC. Positive deviance control-case life history: a method to develop grounded hypotheses about successful long-term avoidance of infection. BMC Public Health. 2008 Mar 20;8(1):94. doi: 10.1186/1471-2458-8-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hser Y-I, Longshore D, Anglin MD. The life course perspective on drug use: A conceptual framework for understanding drug use trajectories. Eval Rev. 2007 Dec 1;31(6):515–47. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- 49.Rhodes T. Risk environments and drug harms: A social science for harm reduction approach. Int J Drug Policy. 2009 May;20(3):193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 50.Elder GH. The life course as developmental theory. Child Dev. 1998 Feb 1;69(1):1–12. [PubMed] [Google Scholar]
- 51.Grov C. HIV risk and substance use in men who have sex with men surveyed in bathhouses, bars/Clubs, and on Craigslist.org: Venue of Recruitment Matters. AIDS Behav. 2011 Jul 12;16(4):807–17. doi: 10.1007/s10461-011-9999-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McFarlane M, Bull SS, Rietmeijer CA. The internet as a newly emerging risk environment for sexually transmitted diseases. JAMA J Am Med Assoc. 2000;284(4):443–6. doi: 10.1001/jama.284.4.443. [DOI] [PubMed] [Google Scholar]
- 53.Rice E. The positive role of social networks and social networking technology in the condom-using behaviors of homeless young people. Public Health Rep 1974. 2010;125(4):588–95. doi: 10.1177/003335491012500414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Young SD, Rice E. Online social networking technologies, HIV knowledge, and sexual risk and testing behaviors among homeless youth. AIDS Behav. 2010 Sep 17;15(2):253–60. doi: 10.1007/s10461-010-9810-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mimiaga MJ, Reisner SL, Bland S, Cranston K, Isenberg D, Driscoll MA, et al. “It’s a quick way to get what you want”: A formative exploration of HIV risk among urban Massachusetts men who have sex with men who attend sex parties. AIDS Patient Care STDs. 2010 Sep 16;24(10):659–74. doi: 10.1089/apc.2010.0071. [DOI] [PubMed] [Google Scholar]
- 56.Denzin NK, Lincoln YS. The SAGE Handbook of Qualitative Research. SAGE; 2011. p. 785. [Google Scholar]
- 57.Ober AJ, Dangerfield DT, II, Shoptaw S, Ryan G, Stucky B, Friedman SR. Using a “positive deviance” framework to discover adaptive risk reduction behaviors among high-risk HIV-negative black men who have sex with men. AIDS Behav. 2017:1–14. doi: 10.1007/s10461-017-1790-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ryan GW, Bernard HR. Techniques to identify themes. Field Methods. 2003 Feb 1;15(1):85–109. [Google Scholar]
- 59.Murray SA, Kendall M, Carduff E, Worth A, Harris FM, Lloyd A, et al. Use of serial qualitative interviews to understand patients’ evolving experiences and needs. BMJ. 2009 Sep 28;339:b3702. doi: 10.1136/bmj.b3702. [DOI] [PubMed] [Google Scholar]
- 60.Polkinghorne DE. Language and meaning: Data collection in qualitative research. J Couns Psychol. 2005;52(2):137–45. [Google Scholar]
- 61.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007 Dec 1;19(6):349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 62.Morgan EM. Outcomes of sexual behaviors among sexual minority youth. New Dir Child Adolesc Dev. 2014 Jun 1;2014(144):21–36. doi: 10.1002/cad.20058. [DOI] [PubMed] [Google Scholar]
- 63.Herrick AL, Stall R, Goldhammer H, Egan JE, Mayer KH. Resilience as a research framework and as a cornerstone of prevention research for gay and bisexual men: Theory and evidence. AIDS Behav. 2014 Jan 1;18(1):1–9. doi: 10.1007/s10461-012-0384-x. [DOI] [PubMed] [Google Scholar]
- 64.Dyer TP, Shoptaw S, Guadamuz TE, Plankey M, Kao U, Ostrow D, et al. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Health. 2012 Mar 2;89(4):697–708. doi: 10.1007/s11524-012-9674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Adam BD, Hart TA, Mohr J, Coleman T, Vernon J. HIV-related syndemic pathways and risk subjectivities among gay and bisexual men: a qualitative investigation. Cult Health Sex. 2017 Apr 10;0(0):1–14. doi: 10.1080/13691058.2017.1309461. [DOI] [PubMed] [Google Scholar]
- 66.Hart T, Peterson JL. Predictors of risky sexual behavior among young African American men who have sex with men. Am J Public Health. 2004 Jul 1;94(7):1122–4. doi: 10.2105/ajph.94.7.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sullivan PS, Peterson J, Rosenberg ES, Kelley CF, Cooper H, Vaughan A, et al. Understanding racial HIV/STI disparities in black and white men who have sex with men: A multilevel approach. PLoS ONE. 2014 Mar 7;9(3):e90514. doi: 10.1371/journal.pone.0090514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, Mayer KH. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS Care. 2017 Mar 12;0(0):1–8. doi: 10.1080/09540121.2017.1300633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc. 2005 Jul;97(7):951–6. [PMC free article] [PubMed] [Google Scholar]
- 70.Bernstein KT, Liu K-L, Begier EM, Koblin B, Karpati A, Murrill C. Same-sex attraction disclosure to health care providers among New York City men who have sex with men: Implications for HIV Ttesting approaches. Arch Intern Med. 2008 Jul 14;168(13):1458–64. doi: 10.1001/archinte.168.13.1458. [DOI] [PubMed] [Google Scholar]
- 71.Patton ME, Kidd S, Llata E, Stenger M, Braxton J, Asbel L, et al. Extragenital gonorrhea and chlamydia testing and infection among men who have sex with men—STD Surveillance Network, United States, 2010–2012. Clin Infect Dis. 2014 Mar 18; doi: 10.1093/cid/ciu184. ciu184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Konkle-Parker DJ, Amico KR, Henderson HM. Barriers and facilitators to engagement in HIV clinical care in the deep South: Results from semi-structured patient interviews. J Assoc Nurses AIDS Care. 2011 Mar;22(2):90–9. doi: 10.1016/j.jana.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Doshi RK, Malebranche D, Bowleg L, Sangaramoorthy T. Health care and HIV testing experiences among black men in the South: Implications for “seek, test, treat, and retain” HIV prevention strategies. AIDS Patient Care STDs. 2012 Dec 26;27(2):123–33. doi: 10.1089/apc.2012.0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Saunders BE, Kilpatrick DG, Resnick HS, Tidwell RP. Brief screening for lifetime history of criminal victimization at mental health intake: A preliminary study. J Interpers Violence. 1989 Sep 1;4(3):267–77. [Google Scholar]
- 75.Hales RE. The American Psychiatric Publishing Textbook of Psychiatry. American Psychiatric Pub; 2008. p. 1820. [DOI] [PubMed] [Google Scholar]
- 76.Kessler RC. The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Metzl JM, Hansen H. Structural competency: Theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014 Feb;103:126–33. doi: 10.1016/j.socscimed.2013.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Levy ME, Wilton L, Phillips G, Glick SN, Kuo I, Brewer RA, et al. Understanding structural barriers to accessing HIV testing and prevention services among black men who have sex with men (BMSM) in the United States. AIDS Behav. 2014 Feb 15;18(5):972–96. doi: 10.1007/s10461-014-0719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wilton L, Herbst JH, Coury-Doniger P, Painter TM, English G, Alvarez ME, et al. Efficacy of an HIV/STI prevention intervention for black men who have sex with men: Findings from the Many Men, Many Voices (3MV) project. AIDS Behav. 2009 Mar 9;13(3):532–44. doi: 10.1007/s10461-009-9529-y. [DOI] [PubMed] [Google Scholar]
- 80.Lloyd S, Operario D. HIV risk among men who have sex with men who have experienced childhood sexual abuse: Systematic review and meta-analysis. AIDS Educ Prev. 2012 Jun 1;24(3):228–41. doi: 10.1521/aeap.2012.24.3.228. [DOI] [PubMed] [Google Scholar]
- 81.Mimiaga MJ, Noonan E, Donnell D, Safren SA, Koenen KC, Gortmaker S, et al. Childhood sexual abuse is highly associated with HIV risk–taking behavior and infection among MSM in the EXPLORE study. J Acquir Immune Defic Syndr 1999. 2009 Jul 1;51(3):340–8. doi: 10.1097/QAI.0b013e3181a24b38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Phillips G, Magnus M, Kuo I, Rawls A, Peterson J, Montanez L, et al. Childhood sexual abuse and HIV-related risks among men who have sex with men in Washington, DC. Arch Sex Behav. 2014 May 1;43(4):771–8. doi: 10.1007/s10508-014-0267-5. [DOI] [PubMed] [Google Scholar]
- 83.Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of Co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003 Jun 1;93(6):939–42. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fields SD, Malebranche D, Feist-Price S. Childhood sexual abuse in black men who have sex with men: Results from three qualitative studies. Cultur Divers Ethnic Minor Psychol. 2008;14(4):385–90. doi: 10.1037/1099-9809.14.4.385. [DOI] [PubMed] [Google Scholar]


