Abstract
Purpose
Prostate cancer patients who have undergone androgen deprivation therapy (ADT) may experience cognitive impairment, yet there is an unmet need for nonpharmacological interventions to address cognitive impairment in this population. This study examines the feasibility, acceptability, and preliminary efficacy of a home-based computerized cognitive training (CCT) program to treat cancer-related cognitive impairment.
Methods
Sixty men who had received ≥3 months of ADT were screened for at least mild cognitive or neurobehavioral impairment and randomized to 8 weeks of CCT or usual care. Follow-up assessments occurred immediately post-intervention or equivalent (T2) and 8 weeks later (T3). The acceptability of CCT was also assessed.
Results
Feasibility
A priori feasibility thresholds were partially met (i.e., randomization rate >50%, retention rate>70% excluding CCT drop-outs, but <70% for intent-to-treat).
Acceptability
Participants were mostly satisfied with CCT and found it somewhat enjoyable, though barriers to uptake existed.
Preliminary efficacy
Linear mixed models indicated significant time by group effects favorable to CCT in reaction time (p=.01), but unfavorable to CCT in verbal and visual memory (ps<.05). Memory was temporarily suppressed in the CCT group at T2, but normalized by T3. There was no effect of CCT on self-reported cognitive functioning, neurobehavioral functioning, nor quality of life.
Conclusions
This study provides tentative support for the feasibility and acceptability of CCT to treat mild cognitive impairment in ADT patients. CCT had a beneficial effect on reaction time, but temporarily suppressed memory. CCT’s benefits may be limited to a narrow area of functioning. Larger-scale studies are needed.
Keywords: oncology, hormone therapy, cancer-related cognitive impairment, cognition, computers, antiandrogens
BACKGROUND
Androgen deprivation therapy (ADT) is a treatment for prostate-specific antigen recurrence following prostate cancer treatment [1, 2] associated with side-effects, including cognitive impairment [3, 4]. ADT patients are twice as likely to exhibit impaired cognition than non-ADT patients and healthy controls [3]. A recent conflicting reports exists, though different tests were used than earlier reports [5]. Neurobehavioral symptoms (i.e., behavioral signs and symptoms of neurological impairment) that can underlie cognitive problems may also affect ADT patients [6].
Few nonpharmacologic approaches exist to treat cancer-related cognitive impairment. To the best of the authors’ knowledge, no known studies have focused specifically on treating cognitive dysfunction in ADT patients. Although a recent study in ADT patients showed that engaging in aerobic exercise was associated with better cognitive change scores than usual care [7], participants were not screened for cognitive impairment as it was not the primary outcome, and cognition was assessed with only two items from a quality of life questionnaire. In a recent Cochrane review of non-pharmacologic approaches to treat cancer-related cognitive impairment [8], only five studies were eligible for inclusion, and all were in breast cancer. The studies focused on computerized cognitive training (CCT; involving repetitive practice of cognitive skills), compensatory strategy training (involving learning strategies to manage cognitive impairments), meditation, and exercise. Findings suggested that CCT and compensatory strategy training showed promise. A more recent study tested a 15-week CCT program in a mixed group of non-central nervous system cancer survivors [9]. CCT led to improvements in self-reported cognitive symptoms compared with standard care, but not on neuropsychological outcomes.
Should the findings of the aforementioned studies translate to ADT patients [8, 9], then CCT could be a promising intervention for them, because it is easily disseminable and requires little clinical oversight [10]. BrainHQ (Posit Science) is one such program. It is informed by brain plasticity research that suggests that behavioral experiences can change cortical representations. Such changes are said to underlie basic-level perceptual, cognitive and motor skill learning which, in turn, underlies higher-level cognitive and behavioral functions [10]. The foundational importance of basic-level skills is also supported by cognitive aging research [11]. BrainHQ trains basic-level functions in order to also support higher-level functions. In two breast cancer CCT trials – one that targeted speed of processing (using BrainHQ) and memory, and the other that targeted executive functioning – CCT led to domain-specific cognitive improvements that transferred to higher-level cognitive functions, symptom distress and quality of life in the former, and self-reported cognitive function in both studies [12, 13].
The purpose of the present study was to examine the feasibility, acceptability, and preliminary efficacy of home-based CCT (BrainHQ) to improve cognitive functioning in ADT patients with cognitive or neurobehavioral impairment. We hypothesized that 1) >50% of eligible participants would agree to be randomized and >70% would complete the study [14–16]; 2) CCT participants would be satisfied with and enjoy CCT; and 3) CCT would improve basic-level cognitive performance more than usual care (UC). Effects on secondary outcomes (i.e., higher-level cognitive performance, self-reported cognitive functioning, neurobehavioral functioning, and quality of life) were also explored.
METHODS
Study Design
This pilot study consisted of a two-group randomized controlled trial comparing CCT with UC in prostate cancer patients who had been on ADT for ≥3 months. Patients were screened and outcomes assessed at baseline, immediately after the 8-week intervention or equivalent time point (T2), and 8 weeks later (T3). The planned sample size for the study was 40 in the CCT group and 20 in the UC group which i) was based on an established rule of thumb for pilot trials of at least 12 per group [17]; ii) facilitated the estimation of a 25% drop-out rate to within a 95% confidence interval of ±11% approximately, accounting for the difference in sample sizes between groups; and iii) ensured that available study resources were not exceeded during the planned data collection time frame of 2 years.
Recruitment and Procedures
Study approval was obtained by Mount Sinai’s Program for the Protection of Human Subjects. ADT patients were recruited between November 2012 and June 2014 from the following: a) Mount Sinai Hospital, New York; and b) listservs and online advocacy groups. Patients were informed that we were evaluating a program to help with concentration, thinking, or memory problems reported by some people who had undergone ADT. Informed consent was obtained from all participants. All remaining aspects of the study were conducted by phone and internet.
Screening baseline assessment
Interviews established that participants 1) had completed primary prostate cancer treatment, 2) had received ADT for ≥3 months, 3) could speak and read English, and 4) had access to a telephone and computer with internet access; but were excluded if screening indicated the following: 1) neurological history likely to impair cognition; 2) active psychosis, clinically significant depression, or substance abuse; 3) visual, hearing, or physical impairment; or 4) other previous cancer, secondary tumor, or metastasis. Baseline assessment consisted of an interview to gather demographic and medical information, computerized neuropsychological assessment (i.e., CNS Vital Signs; [18]), and completion of questionnaires on PsychData.com. Participants were actively guided by research staff to ensure accurate comprehension of instructions. Participants were eligible if they had mild cognitive or neurobehavioral impairment indicated either by 1) a score of ≥1 SD below the normative mean on any CNS Vital Signs subtest, 2) a score of ≥8 on the Patient Assessment of Own Functioning Inventory (i.e., ≥1 SD above mean endorsements from a non-clinical sample [19, 20]), or 3) a T-score ≥60 on any Frontal Systems Behavior Scale subscale [21]. Prior cognitive intervention studies in cancer survivors have generally relied on self-reported cognitive impairment as the primary inclusion criteria. However, due to the known discrepancy between self-reported and objective cognitive impairment, we included individuals who met criteria for either [22]. Eligible participants were randomized to CCT or UC in a 2-to-1 ratio ensuring sufficient collection of feasibility and acceptability data, while minimizing reduction in power. The approach of block randomization was used in order to ensure balance between groups in a 2-to-1 ratio of sample sizes in each group throughout the study [23].
Intervention
Within 3 days of Baseline, CCT participants were instructed to use BrainHQ (www.brainhq.com), which consisted of five visual attention and information processing exercises. Adaptive Bayesian algorithms ensure that virtually any participant can perform them and is optimally challenged. Exercises follow a defined order optimizing fidelity to the intervention. The “dose” was 1 h/day, 5 days/week for 8 weeks [24]. Adherence was promoted through daily email reminders and weekly phone calls. UC participants were permitted to try CCT for 8 weeks at the end of their participation. Although random assignment was completed by someone unconnected with the study, research staff were not blinded to study condition in order to facilitate contact with participants. Potential biases were minimized through computerized administration of outcome measures.
T2 and T3 assessment
These assessments replicated baseline except CCT participants completed additional questionnaires assessing CCT’s helpfulness and acceptability. All participants were offered a stress management/relaxation CD to thank them for their participation.
Participants who withdrew from the study
Participants who chose to withdraw from the study were asked about their reasons for dropping out. Their feedback was important for evaluating the acceptability of the study protocol and program. Participants who could not be reached were sent a thank you letter.
Measures
Feasibility
The percentage of eligible participants who agreed to randomization, retention rates, and completion rates was calculated. Guided by previous research [14–16], a priori thresholds for feasibility were as follows: percentage of eligible participants who agreed to be randomized >50% and percentage of participants who completed the study >70%. Measures of participation were based on time spent on CCT measured by BrainHQ’s tracking software. Participants were also asked to complete participation logs noting when they started and ended training each day. Since BrainHQ cannot track training pauses, or if non-participants use the program, the logs were used to edit the tracked times. Completers were operationalized as participants who trained for ≥10 h in total which, although low, ensured that a sufficient number of participants would complete the training, thus permitting an evaluation of preliminary efficacy as well. Furthermore, this approximated the dose found in other studies to be efficacious (i.e., between 8 and 10 h) [25–27]. CCT participants also reported their experiences in the participation logs and weekly phone calls.
Acceptability
The 8-item Client Satisfaction Questionnaire [28] measured satisfaction with CCT using a 4-point Likert scale from 1 to 4 where a higher total score indicated greater satisfaction. Cronbach’s α was .88. The 7-item interest/enjoyment subscale of the Intrinsic Motivation Inventory [29] measured enjoyment of CCT using a 3-point Likert scale (1= ‘Not at all true,’ 4= ‘Somewhat true,’ and 7= ‘Very true’); a higher total score indicated greater interest/enjoyment. Cronbach’s α was .94. Content analysis of participation log comments and clinical notes from phone calls was undertaken to characterize participant experiences with CCT.
Objective cognitive functioning
CNS Vital Signs [18], a 30-min computer-administered neuropsychological assessment tool, consists of seven cognitive tests that assess basic-level functions (reaction time, simple attention, processing speed, and motor speed) and higher-level functions (verbal memory, visual memory, and cognitive flexibility). CNS Vital Signs is sensitive to mild cognitive dysfunction and has psychometric characteristics (i.e., concurrent and discriminant validity) similar to that of conventional neuropsychological tests, and the ability to generate multiple forms, thus minimizing practice effects [18]. Using CNS Vital Signs’ embedded validity indicators, invalid scores were excluded from analyses and extreme low outliers were truncated to 3 SDs below the mean to reduce skewness.
Self-reported cognitive functioning
The 33-item Patient Assessment of Own Functioning Inventory (PAOFI) measures patient perceptions regarding the “adequacy of their [cognitive] functioning in various everyday tasks and activities” using a Likert scale from 1 (Almost Always) to 6 (Almost Never) [20]. Likert ratings of 1–3 were scored ‘1’ indicating impairment, and ratings from 4–6 were scored ‘0’ indicating no impairment. A total impairment score was calculated by summing the impaired items. Cronbach’s α was .91.
Neurobehavioral functioning
The 46-item Frontal Systems Behavior Scale (FrSBe [21]) measures neurobehavioral difficulties (i.e., apathy, disinhibition, and executive dysfunction) using a 5-point Likert scale. Each total score was converted to a T-score. A higher T-score indicated greater dysfunction. Cronbach’s α was .90.
Quality of life
The 39-item Functional Assessment of Cancer Therapy–Prostate [30] measures quality of life using a 5-point Likert scale. Total scores range from 0 to 156 with a higher score indicating better quality of life. Cronbach’s α was .93.
Sociodemographic and medical information
This data was captured by self-report. The Self-Administered Comorbidity Questionnaire assessed the presence of 13 comorbid conditions and their impact on functioning (range 0–39) [31].
Data Analyses
Descriptive statistics were used to characterize sociodemographic, clinical, and neuropsychological variables and to calculate feasibility and acceptability outcomes. Group differences were analyzed with independent t-tests. Preliminary efficacy was assessed using repeated measures linear mixed models (LMMs) using V.9.4 of SAS procedure MIXED. A dummy-coded group variable (CCT vs. UC) was entered as the independent variable to test main effects and a time by group variable to test interaction effects for each outcome. Effect sizes for each significant model and individual effect sizes for baseline-T2 and baseline-T3 were calculated. For these exploratory analyses, a significance level of p<.05 was used.
RESULTS
Participant characteristics
Table 1 summarizes participant characteristics. Participants were predominantly White, married, college educated, and had high incomes. Groups did not differ significantly on sociodemographic characteristics (i.e., age, race/ethnicity [White vs. other], marital status [married/marriage-like relationship vs. other], years of education, and annual household income [<$95,000 vs. ≥$95,000]), nor on medical characteristics (i.e., medical comorbidities, primary treatment [surgery vs. other], time since diagnosis, and duration of ADT). Groups did not differ in cognitive functions (i.e., CNS Vital Signs cognitive domain scores, and PAOFI self-reported cognitive impairment) nor in neurobehavioral functions (i.e., FrSBe total T-score), except processing speed where the standard score for CCT (M=104.76, SD=19.11) was higher than that for UC (M=95.74, SD=9.97; t(50.86)=−2.26, p=.03) where equal variances were not assumed.
Table 1.
Participant characteristics
| Variable | Usual Care | Computerized cognitive training | All participants | |||
|---|---|---|---|---|---|---|
| (n=20) | (n=40) | (n=60) | ||||
|
| ||||||
| M (SD) | n (%) | M (SD) | n (%) | M (SD) | n (%) | |
| Age (years) | 66.70 (7.81) | 66.5 (8.9) | 66.6 (8.5) | |||
| Race/ethnicity | ||||||
| White | 19 (95.0) | 36 (90.0) | 55 (91.7) | |||
| African American/Black | 1 (5.0) | 2 (5.0) | 3 (5.0) | |||
| Other | 0 (0.0) | 2 (5.0) | 2 (3.3) | |||
| Marital status | ||||||
| Married/partnered | 16 (80.0) | 36 (90.0) | 52 (86.7) | |||
| Single/never married | 2 (10.0) | 2 (5.0) | 4 (6.7) | |||
| Divorced/separated | 2 (10.0) | 2 (5.0) | 4 (6.7) | |||
| Years of education | 16.20 (2.71) | 16.7 (2.9) | 16.5 (2.8) | |||
| Annual household income | ||||||
| ≥$110,000 | 9 (45.0) | 14 (37.5) | 24 (40.0) | |||
| $95,000–109,999 | 1 (5.0) | 6 (15.0) | 7 (11.7) | |||
| $80,000–94,999 | 1 (5.0) | 1 (2.5) | 2 (3.3) | |||
| $65,000–79,999 | 4 (20.0) | 5 (12.5) | 9 (15.0) | |||
| $50,000–64,999 | 3 (15.0) | 1 (2.5) | 4 (6.7) | |||
| $35,000–49,999 | 1 (5.0) | 5 (12.5) | 6 (10.0) | |||
| $20,000–34,999 | 0 (0.0) | 3 (7.5) | 3 (5.2) | |||
| <$20,000 | 1 (5.0) | 1 (2.5) | 2 (5.0) | |||
| Did not report | 0 (0.0) | 3 (7.5) | 3 (5.2) | |||
| Medical comorbidities | 3.80 (3.37) | 6.6 (13.9) | 5.7 (11.6) | |||
| Primary Treatment | ||||||
| Surgery | 6 (30.0) | 5 (12.5) | 11 (18.3) | |||
| Surgery and radiation therapy | 4 (20.0) | 6 (15.0) | 11 (18.3) | |||
| Other combination including surgery | -- | 7 (17.5) | 7 (11.7) | |||
| External beam radiation therapy | 6 (30.0) | 3 (7.5) | 9 (15.0) | |||
| Radioactive seed implantation | 2 (3.3) | 2 (3.3) | ||||
| Radiation therapy and seed implantation | 1 (5.0) | 4 (10.0) | 5 (8.3) | |||
| Androgen deprivation therapy (ADT) | 1 (5.0) | 6 (15.0) | 8 (13.3) | |||
| Other combination not including surgery | 2 (10.0) | 5 (12.5) | 7 (11.7) | |||
| Time since diagnosis (years) | 7.3 (4.6) | 6.6 (5.9) | 6.9 (5.5) | |||
| Duration of ADT (months) | 45.4 (31.5) | 45.8 (57.3) | 45.7 (49.7) | |||
Feasibility
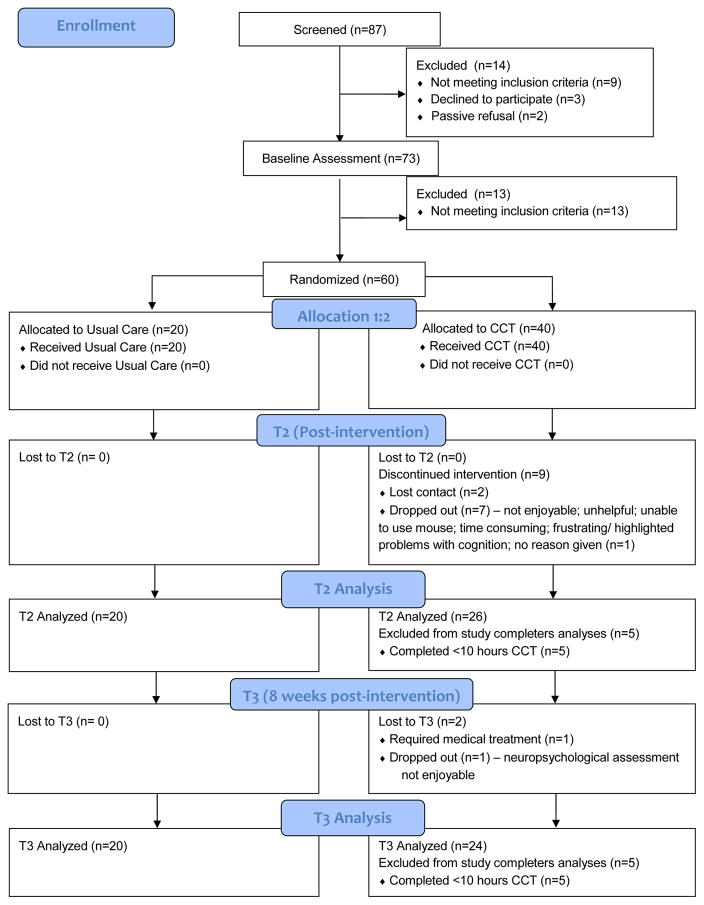
Enrollment and participation are illustrated in Figure 1. There were 174 patients approached – 156 through community recruitment and 18 at Mount Sinai. Eighty-seven were consented and screened (50% enrollment rate). Primary refusal reasons were lack of interest or lack of time. Seventy-three completed baseline, and 60 met randomization criteria. Retention was 77.5% for CCT and 100% for UC at T2, and 72.5% for CCT and 100% for UC at T3. When we examined “completers” only, i.e., participants who trained ≥10 total hours in total, retention at T2 dropped to 65% and at T3 to 60%. Multiple reasons were reported for dropping out of CCT including the following: the program was not enjoyable, not helpful, time consuming, frustrating/highlighted problems with cognition, or unable to use the mouse. Completers trained on average 30.25 h (SD=8.35; range 14.55–46.05).
Fig. 1.
Consort diagram
Overall, feasibility thresholds were partially met (i.e., >50% randomization rate, but <70% completed the study). However, when all CCT participants were included, whether or not they were “completers,” it was deemed to be feasible (>70% retention).
Acceptability
Thirty-one CCT participants completed T2. Participants were mostly satisfied with CCT (mean=2.96, SD=.53) and found the program somewhat enjoyable (mean=4.40, SD=1.59). Content analysis of participation logs and clinical notes indicated that participants found CCT lengthy and challenging but were willing to keep training. Sixteen participants (52%) had difficulty finding time to train (“hard to get 1 hour in per day”) or had trouble completing the full hour. Other interfering factors included the following: tiredness (39%) (“I got sleepy in the middle of it”), health problems (35%) (“medical tests wore me out”), boredom (32%) (“boring after a while”), or being distracted (16%) (“after you’ve been at it… concentration goes down”). A majority mentioned that the exercises were challenging (68%) (“hard time especially with the birds”). Other obstacles included technical problems (58%) such as the computer freezing, and a few noted side effects such as hand pain or eye strain (19%).
Participants were motivated to address barriers by taking breaks (39%) (“30 minute chunks helped me to sustain concentrating”) or training during optimal times (29%) (“did better at night”). A majority of participants (77%) reported that training was “going fine, ok, or well,” some noting that they felt stimulated (16%) (“they are interesting tests for my brain”) or enjoyed CCT (13%) (“I am enjoying doing the training”). Some noticed general improvement (23%) (“I think I’ve made progress”) or improvement on specific skills (“my range of vision is increasing”). Hence, despite obstacles to participation, most participants completed the minimally acceptable amount of training.
Preliminary efficacy
Primary outcomes
In all repeated measures LMMs, years of education was entered as a covariate because it is often associated with cognition [32] and was significantly associated with two of the 4 primary outcomes (i.e., reaction time and processing speed). Table 2 contains between-within effect sizes based on least squares means for all outcomes for baseline-T2 and baseline-T3.
Table 2.
Least squares means and between-within effect sizes by group from Baseline to T2 and Baseline to T3.
| Completers
|
Intent-to-treat group
|
||||||
|---|---|---|---|---|---|---|---|
| Variable | Time point | UCa Mean (SD) | CCTb Mean (SD) | Cohen’s d* | UC Mean (SD) | CCT Mean (SD) | Cohen’s d* |
| Primary outcomes | |||||||
| Reaction time | Baseline | 94.74 | 93.18 | 94.73 | 93.79 | ||
| (10.57) | (10.46) | (10.97) | (10.88) | ||||
| T2 | 95.72 | 99.98 | 0.58 | 95.73 | 99.29 | 0.43 | |
| (10.20) | (9.78) | (10.60) | (10.29) | ||||
| T3 | 95.63 | 99.91 | 0.58 | 95.63 | 99.61 | 0.47 | |
| (10.57) | (9.53) | (10.97) | (10.08) | ||||
| Processing speed | Baseline | 95.34 | 104.32 | 95.37 | 103.60 | ||
| (14.67) | (14.75) | (14.56) | (14.65) | ||||
| T2 | 101.55 | 108.61 | 0.14 | 101.57 | 106.61 | 0.23 | |
| (14.67) | (13.74) | (14.57) | (13.81) | ||||
| T3 | 103.17 | 109.25 | 0.20 | 103.20 | 109.14 | 0.16 | |
| (14.91) | (13.56) | (14.80) | (13.42) | ||||
| Simple attention | Baseline | 96.25 | 100.18 | 96.21 | 100.66 | ||
| (12.94) | (12.97) | (12.73) | (12.76) | ||||
| T2 | 100.65 | 99.44 | 0.40 | 100.62 | 98.73 | 0.50 | |
| (13.01) | (12.78) | (12.80) | (12.61) | ||||
| T3 | 99.29 | 103.11 | 0.01 | 99.28 | 102.42 | 0.10 | |
| (12.89) | (12.42) | (12.69) | (12.55) | ||||
| Motor speed | Baseline | 94.03 | 98.49 | 93.99 | 98.34 | ||
| (14.04) | (14.02) | (14.11) | (14.09) | ||||
| T2 | 96.64 | 102.31 | 0.09 | 96.60 | 102.00 | 0.08 | |
| (13.80) | (12.77) | (13.87) | (12.97) | ||||
| T3 | 99.80 | 101.15 | 0.24 | 99.76 | 101.35 | 0.21 | |
| (13.80) | (12.27) | (13.87) | (12.53) | ||||
| Secondary outcomes | |||||||
| Verbal memory | Baseline | 93.91 | 98.65 | 93.88 | 98.34 | ||
| (13.53) | (13.53) | (13.22) | (13.21) | ||||
| T2 | 103.11 | 96.62 | 0.85 | 103.08 | 95.78 | 0.90 | |
| (13.53) | (13.12) | (13.22) | (12.88) | ||||
| T3 | 98.91 | 101.58 | 0.15 | 98.88 | 100.51 | 0.22 | |
| (13.53) | (12.98) | (13.22) | (12.76) | ||||
| Visual memory | Baseline | 95.32 | 103.53 | 95.22 | 102.20 | ||
| (13.77) | (13.77) | (14.68) | (14.67) | ||||
| T2 | 97.32 | 95.92 | 0.71 | 97.22 | 95.68 | 0.60 | |
| (13.77) | (13.26) | (14.68) | (14.10) | ||||
| T3 | 96.20 | 103.52 | 0.07 | 96.09 | 101.60 | 0.10 | |
| (13.77) | (13.09) | (14.68) | (13.92 | ||||
| Cognitive flexibility | Baseline | 98.20 | 98.93 | 98.17 | 98.65 | ||
| (10.58) | (10.43) | (11.59) | (11.40) | ||||
| T2 | 102.55 | 104.29 | 0.10 | 102.45 | 103.28 | 0.03 | |
| (10.02) | (9.92) | (10.84) | (10.80) | ||||
| T3 | 100.35 | 105.21 | 0.41 | 100.32 | 103.77 | 0.27 | |
| (10.58) | (9.82) | (11.59) | (10.69) | ||||
| Self-reported cognitive | Baseline | 5.99 | 4.78 | 5.98 | 4.59 | ||
| (4.91) | (4.91) | (4.73) | (4.73) | ||||
| impairment (PAOFI)c,d | T2 | 3.24 | 2.47 | 0.09 | 3.23 | 2.40 | 0.12 |
| (4.91) | (4.61) | (4.73) | (4.41) | ||||
| T3 | 4.94 | 2.83 | 0.19 | 4.93 | 2.78 | 0.17 | |
| (4.91) | (4.48) | (4.73) | (4.38) | ||||
| Neurobehavioral | Baseline | 61.61 | 64.14 | 61.59 | 63.65 | ||
| (15.45) | (15.46) | (15.00) | (15.01) | ||||
| symptoms (FrSBe)d,e | T2 | 55.76 | 55.98 | 0.16 | 55.74 | 56.31 | 0.11 |
| (15.45) | (14.12) | (15.00) | (13.58) | ||||
| T3 | 57.76 | 54.70 | 0.39 | 57.74 | 55.19 | 0.33 | |
| (15.45) | (13.57) | (15.00) | (13.42) | ||||
| Quality of life (FACT-P)f | Baseline | 102.56 | 106.32 | 102.61 | 106.68 | ||
| (21.44) | (21.44) | (21.28) | (21.30) | ||||
| T2 | 104.37 | 107.38 | 0.04 | 104.42 | 106.80 | 0.09 | |
| (21.44) | (19.19) | (21.28) | (18.59) | ||||
| T3 | 101.51 | 105.39 | 0.01 | 101.56 | 104.65 | 0.05 | |
| (21.44) | (18.30) | (21.28) | (18.59) | ||||
Non-italicized effect sizes favor CCT over UC, italicized effect sizes favor UC over CCT.
UC=Usual Care;
CCT=Computerized Cognitive Training;
PAOFI=Patient Assessment of Own Functioning Inventory;
Higher score indicates worse function;
Frontal Systems Behavior Scale;
FACT-P=Functional Assessment of Cancer Therapy-Prostate
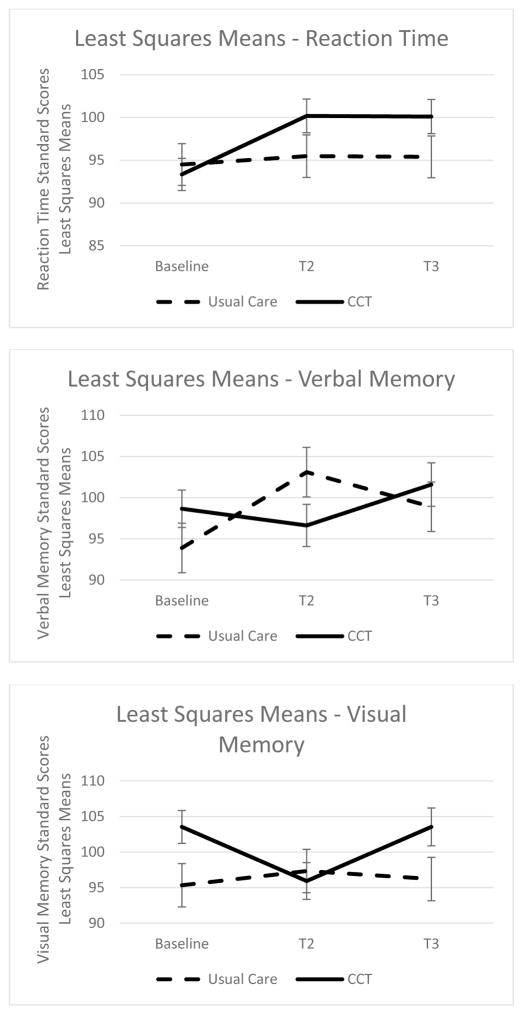
Among study completers, the LMM analysis showed that years of education was positively associated with reaction time performance. A significant time effect (F[2,83]=9.15; p=<.001) indicated that reaction time improved over time. A significant time by group effect (F[2,83]=5.22; p=.007) indicated that groups differed with respect to change in reaction time over time. The CCT group’s reaction time improved significantly from baseline to T2 then remained stable to T3, while the UC group’s reaction time remained stable over time (see Figure 2). There was a medium effect size for the model (d=.70) [33] indicating that reaction time improved more in the CCT group over time than in the UC group. No other statistically significant interaction effects were found among study completers on the other primary outcome variables (i.e., simple attention, processing speed, motor speed).
Fig. 2.
Least squares means and standard error bars for outcomes with significant interaction effects – completer analyses.
Among the intent-to-treat group, LMM results followed the same patterns as for study completers indicating a significant time effect (F[2,93]=6.22; p=.003) and a significant time by group effect (F[2,93]=3.18; p=.046) for reaction time with a medium effect size (d=.50). No other statistically significant interaction effects were found among intent-to-treat participants on the other primary outcome variables.
Secondary outcomes
Among study completers, the LMM for verbal memory indicated a significant time by group effect (F[2,86]=4.32; p=.02). UC’s verbal memory improved compared with the CCT group’s from baseline to T2, but by T3, verbal memory in the UC group had declined so that there was no longer a favorable effect from being in the UC group compared with the CCT group. There was a medium effect size for the overall model (d=.63). The LMM for visual memory indicated a significant time by group effect (F[2,86]=3.61; p=.03). The CCT group’s visual memory declined from baseline to T2 compared with UC, but returned to baseline levels by T3. There was a medium effect size for the overall model (d=.59). No other statistically significant interaction effects were found among study completers on the other secondary outcome variables (i.e., cognitive flexibility, self-reported cognitive functioning, neurobehavioral functioning, or quality of life).
Among the intent-to-treat group, LMMs indicated a significant time by group effect (F[2,96]=5.04; p=.008) for verbal memory with a medium effect size (d=.67). No other statistically significant interaction effects were found among intent-to-treat participants on the remaining secondary outcome variables.
DISCUSSION
This is the first study to examine CCT in ADT patients. Preliminary efficacy was demonstrated for reaction time, but not other cognitive functions. Many BrainHQ tasks require rapid responses to visual stimuli so it is not surprising that reaction time improved. However, there was an unexpected temporary suppression of two higher-level functions – verbal and visual memory – that was not sustained 8 weeks post-CCT. These results contradict findings that do show transfer from basic-level to higher-level abilities (including memory) following CCT [12, 34]. It is possible that improvements in reaction time may be insufficient for transfer to higher-level functions and that improvements in other basic functions, such as processing speed, may be necessary for such a transfer to occur [11]. Furthermore, a study by van der Linden and colleagues [35] provides another possible explanation for these results. When cognitive fatigue was induced in healthy participants using a 2-h cognitively demanding task, fatigued participants performed worse on higher level (executive functioning) tasks than controls, but basic attention was unaffected. Consistent with this work, neuroimaging studies indicate that there are significant associations between mental fatigue and brain activity during more complex and fatiguing cognitive tasks, but not during less demanding cognitive tasks [36]. Given that the trainees in the current study trained on average 2 h per week more than what has been prescribed in other studies focused on visual speed of processing training (when averaged by number of weeks of training), this explanation seems possible. In other words, our trainees may have experienced cognitive fatigue associated with computer use that suppressed memory performance temporarily, but recovered after 8 weeks of rest, leaving reaction time improvements intact. It is also possible that repetitive practice on the largely visual-motor and reaction time tasks were rehearsed more than, or even interfered with, verbal and visual learning processes. There was no effect of CCT on self-reported cognitive functioning, neurobehavioral functioning, nor quality of life suggesting that its potential may be limited to a narrow area of functioning, at least in the short-term.
Results provide tentative support for CCT’s feasibility and acceptability. The 50% enrollment rate reflects a common challenge in this population, possibly relating to gender. A psychosocial intervention study that examined accrual challenges in prostate cancer patients and their spouses found that refusals were greater among the male patients than their female spouses [37]. However, our enrollment was higher than that of a technology-assisted psychosocial intervention study for prostate cancer patients [38] possibly because our participants could train in their own time, or maybe our study’s focus felt less threatening.
Retention rates were good (>70%), but lower when participants who completed less than 10 h of training were excluded (≥60%). Numerous reasons were cited for terminating CCT such as finding it unenjoyable or time consuming. Shorter training times, as in other studies [12, 13], may have been more palatable for these participants. Participants who did complete the minimally acceptable amount of training trained for 75% of the prescribed duration (i.e., ~45 min/weekday).
Most CCT studies in cancer patients have focused on efficacy [12, 13]. Although our CCT participants were mostly satisfied with the program, challenges to CCT uptake can reduce its utility if not addressed. About 40% of participants found CCT lengthy or difficult to fit into their schedule. One third found it boring or had trouble staying focused, often due to health problems or tiredness. Two-thirds found the exercises challenging. Sixty percent experienced technical problems. A few noted side effects such as hand pain or eye strain. Despite these challenges, participants were generally motivated to overcome them using various strategies. The most popular strategy (40%) was to take breaks or break up training into chunks. Almost a third indicated that training during alert times of the day was helpful. Based on this data, certain elements are necessary to optimize CCT’s utility: 1) basic computer skills are a necessity; 2) patients should be told that training may be more challenging to stick to than expected, and given strategies, such as breaking up training into chunks, to optimize adherence; and 3) detailed technical guidance should be provided at the beginning of training.
Findings need to be understood in the context of some limitations. First, our sample was predominantly white, married, college educated, with high incomes, and diagnosed relatively young (mean age at diagnosis was 59), thus limiting its generalizability. Second, because CCT was compared to UC rather than an attention control condition, improvements (and declines) may have been due to nonspecific effects. An attention control condition involving participation in nonadaptive computer activities may have been a more appropriate or important additional condition, especially since computer use may be cognitively fatiguing. Third, although BrainHQ targets visual attention and processing skills that may contribute to the visuomotor skills most vulnerable to impairment in ADT patients, it does not train them directly. Fourth, our ability to detect effects was likely limited by the small sample size and the mild severity of participants’ cognitive impairment.
In conclusion, this study provides information about the feasibility, acceptability and preliminary efficacy of CCT to treat cognitive impairment in ADT patients. We have demonstrated that BrainHQ [4] may be a promising tool for patients with cognitive difficulties that affect reaction time, but transfer to higher level abilities found in other studies did not occur [34]. Future studies are necessary to determine whether these results hold in a larger sample, to determine whether a shorter prescribed dose may be more efficacious for improving cognitive functions, and to clarify whether cognitive fatigue was responsible for the unexpected memory findings. Given that few approaches to treat cancer-related cognitive impairment have been tested adequately and even fewer in ADT patients [8], the development and assessment of tools to treat cognitive impairment in ADT patients becomes all the more important.
Acknowledgments
This work was supported by the American Cancer Society (L.W., grant #PF-12-041-01-CPPB); and the National Cancer Institute of the National Institutes of Health (L.W., grant #5K07CA184145-03). Content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health. We thank Posit Science and CNS Vital Signs for providing their programs to this study at no cost.
Footnotes
CONFLICTS OF INTEREST
Wu and Amidi report personal fees from Bayer Pharmaceutical outside the submitted work. The other authors have no conflicts of interest to declare. Wu has full control of all primary data and agrees to allow the journal to review this data if requested.
References
- 1.Han M, Partin AW, Pound CR, Epstein JI, Walsh PC. Long-term biochemical disease-free and cancer-specific survival following anatomic radical retropubic prostatectomy. The 15-year Johns Hopkins experience. Urol Clin North Am. 2001;28:555–565. doi: 10.1016/s0094-0143(05)70163-4. [DOI] [PubMed] [Google Scholar]
- 2.Singh J, Trabulsi EJ, Gomella LG. Is there an optimal management for localized prostate cancer? Clin Interv Aging. 2010;5:187–197. doi: 10.2147/cia.s6555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gonzalez BD, Jim HS, Booth-Jones M, Small BJ, Sutton SK, Lin HY, Park JY, Spiess PE, Fishman MN, Jacobsen PB. Course and Predictors of Cognitive Function in Patients With Prostate Cancer Receiving Androgen-Deprivation Therapy: A Controlled Comparison. J Clin Oncol. 2015 doi: 10.1200/JCO.2014.60.1963. JCO.2014.60.1963 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGinty HL, Phillips KM, Jim HS, Cessna JM, Asvat Y, Cases MG, Small BJ, Jacobsen PB. Cognitive functioning in men receiving androgen deprivation therapy for prostate cancer: a systematic review and meta-analysis. Support Care Cancer. 2014;22:2271–2280. doi: 10.1007/s00520-014-2285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alibhai SMH, Timilshina N, Duff-Canning S, et al. Effects of long-term androgen deprivation therapy on cognitive function over 36 months in men with prostate cancer. Cancer. 2016:1–8. doi: 10.1002/cncr.30320. [DOI] [PubMed] [Google Scholar]
- 6.Wu LM, Tanenbaum ML, Dijkers MPJM, Amidi A, Hall SJ, Penedo FJ, Diefenbach MA. Cognitive and neurobehavioral symptoms in patients with non-metastatic prostate cancer treated with androgen deprivation therapy or observation: A mixed methods study. Soc Sci Med. 2016;156:80–9. doi: 10.1016/j.socscimed.2016.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galvão DA, Taaffe DR, Spry N, Joseph D, Newton RU. Combined Resistance and Aerobic Exercise Program Reverses Muscle Loss in Men Undergoing Androgen Suppression Therapy for Prostate Cancer Without Bone Metastases: A Randomized Controlled Trial. J Clin Oncol. 2010;28:340–347. doi: 10.1200/JCO.2009.23.2488. [DOI] [PubMed] [Google Scholar]
- 8.Treanor CJ, Mcmenamin UC, O’Neill RF, Cardwell CR, Clarke MJ, Cantwell M, Donnelly M. Non-pharmacological interventions for cognitive impairment due to systemic cancer treatment. Cochrane Database Syst Rev. 2016;2016:CD011325. doi: 10.1002/14651858.CD011325.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bray VJ, Dhillon HM, Bell ML, Kabourakis M, Fiero MH, Yip D, Boyle F, Price MA, Vardy JL. Evaluation of a Web-Based Cognitive Rehabilitation Program in Cancer Survivors Reporting Cognitive Symptoms After Chemotherapy. J Clin Oncol. 2017;35:217–225. doi: 10.1200/JCO.2016.67.8201. [DOI] [PubMed] [Google Scholar]
- 10.Mahncke HW, Bronstone A, Merzenich MM. Brain plasticity and functional losses in the aged: scientific bases for a novel intervention. Prog Brain Res. 2006;157:81–109. doi: 10.1016/S0079-6123(06)57006-2. [DOI] [PubMed] [Google Scholar]
- 11.Salthouse TA, AT The processing-speed theory of adult age differences in cognition. Psychol Rev. 1996;103:403–428. doi: 10.1037/0033-295x.103.3.403. [DOI] [PubMed] [Google Scholar]
- 12.Von Ah D, Carpenter JS, Saykin A, et al. Advanced cognitive training for breast cancer survivors: a randomized controlled trial. Breast Cancer Res Treat. 2012;135:799–809. doi: 10.1007/s10549-012-2210-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kesler S, Hadi Hosseini SM, Heckler C, Janelsins M, Palesh O, Mustian K, Morrow G. Cognitive training for improving executive function in chemotherapy-treated breast cancer survivors. Clin Breast Cancer. 2013;13:299–306. doi: 10.1016/j.clbc.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lebowitz MS, Dams-O’Connor K, Cantor JB. Feasibility of computerized brain plasticity-based cognitive training after traumatic brain injury. J Rehabil Res Dev. 2012;49:1547–56. doi: 10.1682/jrrd.2011.07.0133. [DOI] [PubMed] [Google Scholar]
- 15.Boivin MJ, Busman RA, Parikh SM, Bangirana P, Page CF, Opoka RO, Giordani B. A pilot study of the neuropsychological benefits of computerized cognitive rehabilitation in Ugandan children with HIV. Neuropsychology. 2010;24:667–673. doi: 10.1037/a0019312. [DOI] [PubMed] [Google Scholar]
- 16.Morgan NP, Graves KD, Poggi EA, Cheson BD. Implementing an expressive writing study in a cancer clinic. Oncologist. 2008;13:196–204. doi: 10.1634/theoncologist.2007-0147. [DOI] [PubMed] [Google Scholar]
- 17.Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat. 2005;4:287–291. [Google Scholar]
- 18.Gualtieri CT, Johnson LG. Reliability and validity of a computerized neurocognitive test battery, CNS Vital Signs. Arch Clin Neuropsychol. 2006;21:623–643. doi: 10.1016/j.acn.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 19.Richardson-Vejlgaard R, Dawes S, Heaton RK, Bell MD. Validity of cognitive complaints in substance-abusing patients and non-clinical controls: the Patient’s Assessment of Own Functioning Inventory (PAOFI) Psychiatry Res. 2009;169:70–4. doi: 10.1016/j.psychres.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chelune GJ, Heaton RK, Lehman RAW. Neuropsychological and personality correlates of patients’ complaints of disability. In: Tarter RE, Goldstein G, editors. Adv Clin Neuropsychol. Vol. 3. Plenum Press; New York: 1986. pp. 95–126. [Google Scholar]
- 21.Grace J, Malloy PF. Psychological Assessment Resources. Lutz, FL: 2001. Frontal Systems Behavior Scale (FrSBe): Professional Manual. [Google Scholar]
- 22.Hutchinson AD, Hosking JR, Kichenadasse G, Mattiske JK, Wilson C. Objective and subjective cognitive impairment following chemotherapy for cancer: a systematic review. Cancer Treat Rev. 2012;38:926–934. doi: 10.1016/j.ctrv.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Suresh K. An overview of randomization techniques: An unbiased assessment of outcome in clinical research. J Hum Reprod Sci. 2011;4:8–11. doi: 10.4103/0974-1208.82352. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Smith GE, Housen P, Yaffe K, Ruff R, Kennison RF, Mahncke HW, Zelinski EM. A cognitive training program based on principles of brain plasticity: results from the Improvement in Memory with Plasticity-based Adaptive Cognitive Training (IMPACT) study. J Am Geriatr Soc. 2009;57:594–603. doi: 10.1111/j.1532-5415.2008.02167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ball K, Berch DB, Helmers KF, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA. 2002;288:2271–2281. doi: 10.1001/jama.288.18.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rebok GW, Ball K, Guey LT, et al. Ten-year effects of the advanced cognitive training for independent and vital elderly cognitive training trial on cognition and everyday functioning in older adults. J Am Geriatr Soc. 2014;62:16–24. doi: 10.1111/jgs.12607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolinsky FD, Vander Weg MW, Howren MB, Jones MP, Dotson MM. A randomized controlled trial of cognitive training using a visual speed of processing intervention in middle aged and older adults. PLoS One. 2013;8:e61624. doi: 10.1371/journal.pone.0061624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 29.Choi J, Mogami T, Medalia A. Intrinsic motivation inventory: an adapted measure for schizophrenia research. Schizophr Bull. 2010;36:966–976. doi: 10.1093/schbul/sbp030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Esper P, Mo F, Chodak G, Sinner M, Cella D, Pienta KJ. Measuring quality of life in men with prostate cancer using the functional assessment of cancer therapy-prostate instrument. Urology. 1997;50:920–928. doi: 10.1016/S0090-4295(97)00459-7. [DOI] [PubMed] [Google Scholar]
- 31.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 32.Farmer ME, Kittner SJ, Rae DS, Bartko JJ, Regier DA. Education and change in cognitive function. The Epidemiologic Catchment Area Study. Ann Epidemiol. 1995;5:1–7. doi: 10.1016/1047-2797(94)00047-w. [DOI] [PubMed] [Google Scholar]
- 33.Cohen J. Statistical power analysis for the behavioural sciences. 2. Lawrence Erlbaum Associates; New York, NY: 1988. [Google Scholar]
- 34.Mahncke HW, Connor BB, Appelman J, Ahsanuddin ON, Hardy JL, Wood RA, Joyce NM, Boniske T, Atkins SM, Merzenich MM. Memory enhancement in healthy older adults using a brain plasticity-based training program: a randomized, controlled study. Proc Natl Acad Sci U S A. 2006;103:12523–12528. doi: 10.1073/pnas.0605194103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van der Linden D, Frese M, Meijman TF. Mental fatigue and the control of cognitive processes: effects on perseveration and planning. Acta Psychol (Amst) 2003;113:45–65. doi: 10.1016/s0001-6918(02)00150-6. [DOI] [PubMed] [Google Scholar]
- 36.Cook DB, O’Connor PJ, Lange G, Steffener J. Functional neuroimaging correlates of mental fatigue induced by cognition among chronic fatigue syndrome patients and controls. Neuroimage. 2007;36:108–122. doi: 10.1016/j.neuroimage.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 37.Northouse LL, Rosset T, Phillips L, Mood D, Schafenacker A, Kershaw T. Research with families facing cancer: The challenges of accrual and retention. Res Nurs Heal. 2006 doi: 10.1002/nur.20128. [DOI] [PubMed] [Google Scholar]
- 38.Yanez B, McGinty HL, Mohr DC, Begale MJ, Dahn JR, Flury SC, Perry KT, Penedo FJ. Feasibility, acceptability, and preliminary efficacy of a technology-assisted psychosocial intervention for racially diverse men with advanced prostate cancer. Cancer. 2015;121:4407–4415. doi: 10.1002/cncr.29658. [DOI] [PMC free article] [PubMed] [Google Scholar]