Abstract
BACKGROUND
Despite the availability of a safe and efficacious vaccine against human papillomavirus, uptake of the vaccine in the United States is low. Missed clinical opportunities to recommend and to administer human papillomavirus vaccine are considered one of the most important reasons for its low uptake in adolescents; however, little is known about the frequency or characteristics of missed opportunities in the young adult (18–26 years of age) population.
OBJECTIVE
The objective of the study was to assess both the rates of and the factors associated with missed opportunities for human papillomavirus immunization among young adult women who attended an urban obstetrics and gynecology clinic.
STUDY DESIGN
In this cross-sectional study, medical records were reviewed for all women 18–26 years of age who were underimmunized (<3 doses) and who sought care from Feb. 1, 2013, to January 31, 2014, at an urban, hospital-based obstetrics and gynecology clinic. A missed opportunity for human papillomavirus immunization was defined as a clinic visit at which the patient was eligible to receive the vaccine and a dose was due but not administered. Multivariable logistic regression was used to test associations between sociodemographic variables and missed opportunities.
RESULTS
There were 1670 vaccine-eligible visits by 1241 underimmunized women, with a mean of 1.3 missed opportunities/person. During the study period, 833 of the vaccine eligible women (67.1%) had at least 1 missed opportunity. Overall, the most common types of visits during which a missed opportunity occurred were postpartum visits (17%) or visits for either sexually transmitted disease screening (21%) or contraception (33%). Of the patients with a missed opportunity, 26.5% had a visit at which an injectable medication or a different vaccine was administered. Women who identified their race as black had higher adjusted odds of having a missed opportunity compared with white women (adjusted odds ratio, 1.61 [95% confidence interval, 1.08–2.41], P < .02). Women who reported a non-English- or non-Spanish-preferred language had lower adjusted odds of having a missed opportunity (adjusted odds ratio, 0.25 [95% confidence interval, 0.07–0.87], P = .03). No other patient characteristics assessed in this study were significantly associated with having a missed opportunity.
CONCLUSION
A majority of young-adult women in this study had missed opportunities for human papillomavirus immunization, and significant racial disparity was observed. The greatest frequency of missed opportunities occurred with visits for either contraception or for sexually transmitted disease screening.
Keywords: cervical cancer prevention, human papillomavirus, preventative medicine, vaccination
Human papillomavirus (HPV) causes the majority of cervical, oropharyngeal, and anogenital cancers.1,2 The Centers for Disease Control and Prevention (CDC) estimates that every year there are 330,000 new cases of precancerous cervical lesions and 30,000 new cases of HPV-attributable cancers in the United States.3
The total economic burden of preventing and treating HPV-related disease is estimated to be about $8 billion per year.4 Immunization against HPV has been shown to be safe and effective at preventing HPV-attributable precancerous lesions,5 which has led the CDC Advisory Committee on Immunization Practices to recommend that HPV immunization be administered routinely to females at 11–12 years of age with a catch-up immunization through 26 years of age.6
Despite these recommendations, HPV immunization rates remain low. In 2016, the CDC reported that the 3-dose HPV vaccine completion rate among adolescent girls 13–17 years of age in the state of Connecticut was 55.2%. This is in contrast to the 93.5% vaccine uptake for the quadrivalent meningococcal conjugate vaccine and 93.7% for the tetanus, diphtheria, and acellular pertussis vaccine in both male and female adolescents of the same age group.7
Several studies in the United States have demonstrated that most young adult women 19–26 years of age do not have antibodies to the high-risk HPV types most commonly associated with cancer and included in the vaccines and therefore will also benefit from immunization.8–10 Moreover, in one report, the HPV vaccine was at least 30% efficacious at preventing HPV 16/18–positive precancerous cervical lesions of moderate grade or worse in women 15–26 years of age, irrespective of their HPV infection status prior to immunization.11 However, the uptake of the HPV vaccine is even lower among young adult women compared with adolescents,12 and the CDC estimated that only 36% of women 19–26 years of age received 1 or more doses in 2013.13
In addition, there are substantial racial and socioeconomic disparities in the uptake of the HPV vaccine. Previous research has found that women of lower socioeconomic status or of racial/ethnic minority backgrounds were less likely to complete the immunization series than either higher-income women or women identifying as white.14 These disparities in the uptake of the HPV vaccine are of particular concern, given both the higher incidence and the poorer outcomes of cervical cancer among women who are of either racial or ethnic minorities or from lower-income groups.15,16
Missed clinical opportunities to recommend and to administer the HPV vaccine are considered one of the most important reasons for its low uptake in the United States.17 A study of more than 400,000 women demonstrated that >96% of unvaccinated adolescent girls had at least 1 missed opportunity for immunization over a 6 year period.18 Studies from pediatric practices have shown that clinic-specific strategies that identify and decrease missed opportunities can substantially increase the uptake of the HPV vaccine.19 However, most of the efforts to increase vaccine uptake have been focused on adolescents and pediatric practices. There is little information about such efforts in young adult populations that are eligible for immunization or with obstetrics-gynecology practices.20 Continued efforts are needed to improve coverage and understand missed opportunities among young adults.
This study aims to assess both the rates of and the factors associated with missed opportunities for HPV immunization among young adult women (18–26 years old) who attended an urban obstetrics and gynecology clinic in New Haven, CT, that cares for a large proportion of women from racial/ethnic minority and low-income backgrounds.21,22 Understanding the frequency of, and risk factors for, missed opportunities in this high-risk population may be integral to guiding interventions aimed at increasing the uptake of the HPV vaccine.
Materials and Methods
In this cross-sectional study, electronic medical records were reviewed for all women 18–26 years of age who were underimmunized (had received 0, 1, or 2 doses of the HPV vaccine), who were vaccine eligible and who were seen at the Yale New Haven Hospital Women’s Center, a hospital-based obstetrics and gynecology clinic that serves primarily low-income patients of racial and ethnic minority backgrounds, from February 1, 2013, to January 31, 2014.
Using a standardized form, data were collected regarding the number of visits, sociodemographic variables (age, race, ethnicity, preferred language, insurance), pregnancy status, and receipt of HPV vaccine. Additional data were collected for the subset of women considered to have missed opportunities (see the following text), which included reasons for visits as documented in the clinic note as well as documentation of administration of other immunizations and injectable medications.
HPV immunization status was determined by evaluating the immunization history section of the electronic medical record in which the dates of vaccine administration are documented and reviewing all Women’s Center clinic notes and scanned records from the study period for the mention of receipt or offer of the HPV vaccine by a provider.
The Institutional Review Board at Yale University approved this project.
Measures
A vaccine-eligible visit was defined as a visit at which the patient was between 18 and 26 years of age, was not pregnant, and was underimmunized or had never been immunized. A missed opportunity was defined as a vaccine-eligible visit at which the patient was due for either the first, second, or third dose of the HPV vaccine but it was not administered.
The recommendations from the CDC’s Advisory Committee on Immunization Practices are that any available HPV vaccine product (bivalent, quadrivalent, or nonavalent) be used to continue or complete the series for protection against HPV 16 and 18.6 Accordingly, we considered the use of any HPV vaccine as a capitalized opportunity. If the patient had received a dose of the vaccine before the visit, the patient was not defined as eligible for another dose until at least 8 weeks after a first dose or 16 weeks after the second dose (and 24 weeks between the first and third dose).
Insurance was classified as public, private, uninsured, and other. Public insurance included Medicaid, Medicare, Indian Health Service, and military insurance. Self-reported race and ethnicity were classified as non-Hispanic white, non-Hispanic black (subsequently referred to as white and black, respectively), His-panic, and non-Hispanic other.
Statistical analysis
Logistic regression models were estimated to identify patient characteristics associated with at least 1 missed opportunity for HPV immunization during the 1 year study period. All patient characteristics were first evaluated individually for association with missed opportunities using simple regression models (ie, including 1 patient characteristic at a time).
For the multivariable logistic regression model, backward stepwise selection was used to select the final group of variables, in which variables with the highest p-values were removed in sequence until all variables in the final model had a value of P ≤.1. A value of P <.05 was considered to be statistically significant.
This is a descriptive and exploratory study utilizing a convenience sample consisting of the number of women who attended the clinic during a 12 month period. Data were analyzed using Stata statistical software 12.0 (StataCorp, College Station, TX).
Results
During the 1 year study period, a total of 1410 women, 18–26 years of age, had a total of 6988 visits, with a mean of 4.9 visits per person. Of these women, 169 (11.9%) had received 3 doses of the HPV vaccine prior to the study period and were excluded from the analyses (Figure 1). The final group included 1241 age-eligible women who were underimmunized (had received <3 doses of the HPV vaccine) and had at least 1 visit during the study period.
FIGURE 1. Classification of women seen for obstetrics-gynecology care, February 1, 2013 to January 31, 2014.
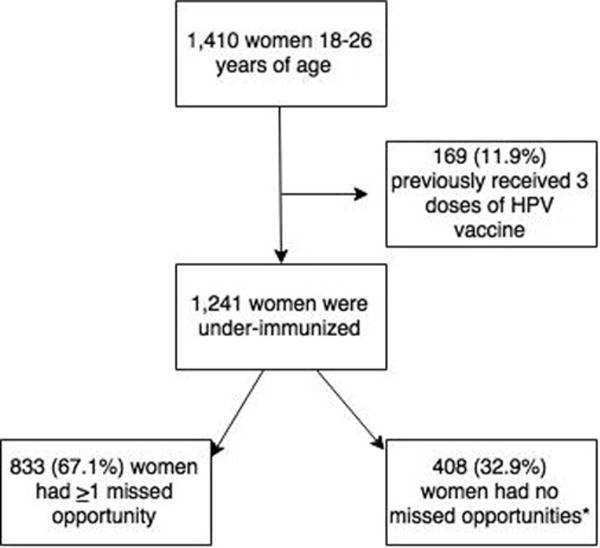
Flowchart showing classification of women seen for obstetrics-gynecology care at The Women’s Center, Feb. 1, 2013, and Jan. 31, 2014. Asterisk indicates that these women had only vaccine-ineligible encounters.
HPV, human papillomavirus.
Of the underimmunized women, 833 (67.1%) had at least 1 missed opportunity for immunization, 362 (29.2%) had noneligible pregnancy visits, 39 (3.1%) received a dose during the study period and did not have any further eligible visits, and 7 (0.6%) were offered the vaccine and declined it. Of the 833 underimmunized women, there was a mean of 1.3 (range 0–9) missed opportunities per person. Women eligible to receive their first dose were equally likely to have a missed opportunity compared with those who were eligible to receive their second or third dose (odds ratio, 0.72 [95% confidence interval (CI), 0.48–1.08]; P = .11). Characteristics of the underimmunized women and women with at least 1 missed opportunity are shown in Table 1.
TABLE 1.
Characteristics of underimmunized women
| Characteristics | ≥ 1 Missed opportunities (n = 833) | No missed opportunities (n = 408) | All women (n = 1241) |
|---|---|---|---|
| Age, y, median (range) | 23 (18–26) | 22 (18–26) | 23 (18–26) |
| Race/ethnicity, n, % | |||
| Non-Hispanic white | 80 (9.6) | 52 (12.8) | 132 (10.6) |
| Hispanic | 329 (39.5) | 164 (40.2) | 493 (39.7) |
| Non-Hispanic black | 367 (44.1) | 147 (33.0) | 514 (41.4) |
| Non-Hispanic othera | 10 (1.2) | 6 (1.5) | 16 (1.3) |
| Not identified | 47 (5.6) | 39 (9.6) | 86 (6.9) |
| Insurance type, n, % | |||
| Private/commercial | 55 (6.6) | 20 (4.9) | 75 (6.0) |
| Public | 642 (77.1) | 311 (76.2) | 953 (76.8) |
| Uninsured | 120 (14.4) | 67 (16.4) | 187 (15.1) |
| Other | 16 (1.9) | 10 (2.5) | 26 (2.1) |
| Preferred language, n, % | |||
| English | 689 (82.7) | 322 (78.9) | 1011 (81.5) |
| Spanish | 133 (16.0) | 62 (15.2) | 195 (15.7) |
| Otherb | 11 (1.3) | 24 (5.9) | 35 (2.8) |
| Previously pregnant, n, % | 648 (77.8) | 311 (76.2) | 959 (77.3) |
Other race: American Indian, Asian, and Native Hawaiian;
Other languages: Arabic, Turkish, Chinese, Farsi, French, Pashto, Serbian, Sign, Swahili, Tigrinya, Vietnamese, and Hindi.
The types of visits that were associated with missed opportunities are shown in Figure 2. The most common types were visits for contraception (33%; for medroxyprogesterone acetate [58%] and other types of contraception [42%]), visits for sexually transmitted disease (STD) screening (21%), and postpartum visits (17%). Of the patients with a missed opportunity, 221 (26.5%) had at least 1 vaccine-eligible visit at which an injectable medication (medroxyprogesterone acetate) or a different vaccine was administered.
FIGURE 2. Types of visits for women with missed opportunities.
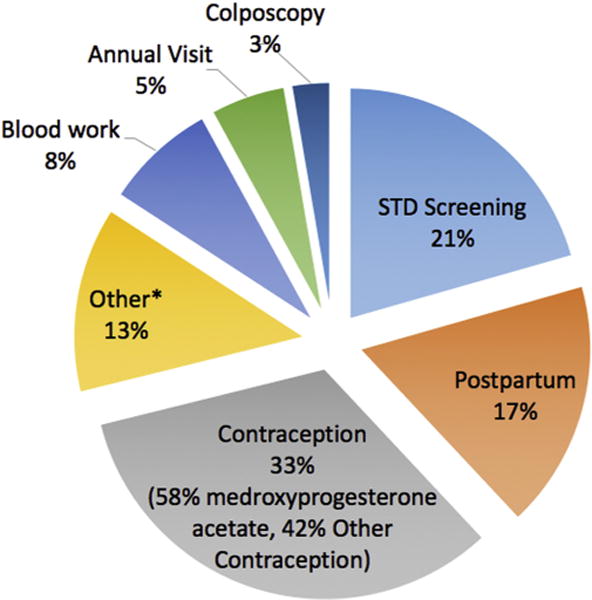
Asterisk indicates the category of other: the most common were visits for menstrual problems, preoperation screening, postoperation follow-up, nutrition counseling, hospitalization follow-up, anemia, urinary tract infections, and endometriosis.
STD, sexually transmitted disease.
Results from simple and multivariable logistic regression are detailed in Table 2. The independent variables included in the final model were race, preferred language, and insurance. Women who identified their race as black had 61% higher adjusted odds of having a missed opportunity compared with white women (adjusted odds ratio [aOR], 1.61 [95% CI, 1.08–2.41]; P =.02). Women who identified their preferred language as other than English or Spanish were less likely to have a missed opportunity compared with preferred English speakers (aOR, 0.25 [95% CI, 0.07–0.87]; P =.03). Associations between missed opportunities and age, Hispanic ethnicity, Spanish language, or parity were not statistically significant.
TABLE 2.
Association between patient characteristics and missed opportunities
| Characteristics | ORa | 95% CI | P value | aORb | 95% CI | P value |
|---|---|---|---|---|---|---|
| Age | 1.02 | 0.97–1.07 | .39 | c | c | c |
| Race/ethnicity | ||||||
| Non-Hispanic white | Reference | Reference | ||||
| Hispanic | 1.31 | 0.88–1.94 | .19 | 1.23 | 0.81–1.90 | .33 |
| Non-Hispanic black | 1.62 | 1.09–2.42 | .01 | 1.61 | 1.08–2.41 | .02 |
| Non-Hispanic otherd | 1.08 | 0.37–3.16 | .88 | 1.45 | 0.47–4.48 | .52 |
| Not identified | c | c | c | c | c | c |
| Insurance type | ||||||
| Private | Reference | Reference | ||||
| Public | 0.75 | 0.44–1.27 | .29 | 0.65 | 0.36–1.16 | .15 |
| Uninsured | 0.65 | 0.36–1.18 | .16 | 0.55 | 0.28–1.08 | .08 |
| Other | 0.58 | 0.22–1.49 | .26 | 0.51 | 0.18–1.44 | .21 |
| Preferred language | ||||||
| English | Reference | Reference | ||||
| Spanish | 1.01 | 0.72–1.39 | .98 | 1.23 | 0.81–1.88 | .33 |
| Othere | 0.21 | 0.13–0.44 | .01 | 0.25 | 0.07–0.87 | .03 |
| Previously pregnant | 1.09 | 0.83–1.45 | .54 | c | c | c |
aOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
Odd ratios were calculated with simple logistic regression;
Adjusted odd ratios were calculated with multivariable logistic regression adjusting for race, preferred language, and insurance;
Omitted from analysis;
Other races: American Indian, Asian, and Native Hawaiian;
Other languages: Arabic, Turkish, Chinese, Farsi, French, Pashto, Serbian, Sign, Swahili, Tigrinya, Vietnamese, and Hindi.
Comment
Despite the availability of a safe and cost-effective vaccine against HPV,23 the uptake of the vaccine in the United States is low. The consequences of maintaining the low HPV immunization rates are not insignificant. In 2017, immunization experts estimated that if the HPV immunization rate could be raised to 80%, an additional 53,000 cases of cervical cancer could be prevented during the lifetime of those younger than 12 years; this is equivalent to 4400 new cases of cervical cancer for every year that the immunization rate does not increase.24
Missed opportunities for administering the HPV vaccine are a major barrier to achieving high rates of immunization. Several studies in adolescents have identified factors associated with the low uptake of the HPV vaccine, such as a lack of knowledge about it, cost, or reluctance of providers to recommend the vaccine25,26; however, less is known about the frequency or characteristics of missed opportunities to administer the vaccine in the young adult population (18–26 years of age).27,28
One qualitative study reported that gaps in knowledge about cervical cancer, HPV, and the HPV vaccine as well as other barriers, such as poor access to transportation and prioritizing other responsibilities over health, were important obstacles to immunization in these women.29 Our study contributes to the literature by specifically examining patient characteristics and providing detailed descriptive analysis of clinical factors such as the reason for the visit or concomitant care received during a visit. Such information may provide a greater context for missed opportunities for immunization when a woman engages in a clinical visit in a women’s health setting and insight into strategies for addressing these missed opportunities.
Our study found that women who self-identify as black were more likely to have had a missed opportunity compared with white women. The racial disparities observed in our study are consistent with previous research reporting that racial minorities, specifically non-Hispanic blacks, are less likely to receive a recommendation to vaccinate from health care providers and are less likely to complete the HPV vaccine series.30,31 Although studies have shown there has been progress in closing the gap in uptake among minorities (particularly among Hispanics and women living below the poverty level),7 our study suggests there is still disparity among women of the black race.
Of note, the cost of the HPV vaccine is covered under most Medicaid plans for women up through 26 years of age. Likewise, most private insurance covers the cost of the vaccine for women up until their 27th birthday. Uninsured women can have the cost of the vaccine covered by the Connecticut Vaccine Program until they turn 19 years of age.32 Women who are 19 years of age or older and uninsured would need to pay out of pocket for the vaccine, which can range between $150 and $200 per dose.
Our study population consisted of women who had access to care and who were predominantly insured through Medicaid. Therefore, the disparity in missed opportunities for HPV immunization among racial and ethnic minorities after controlling for insurance status is especially concerning and warrants further investigation. The disparity may be driven by a multitude of factors including possible provider biases and assumptions, sociocultural beliefs about vaccines and cervical cancer, or perceived quality of patient-provider interactions.
Understanding the nature of this disparity can facilitate development of strategies to eliminate missed opportunities for immunization with the HPV vaccine and potentially reduce disparities in cervical dysplasia and cancer.
There was no statistically significant association between missed opportunities and preferring either the Spanish or the English language. However, women whose preferred language was one other than Spanish or English were less likely to have a missed opportunity.
While our study was not designed to explore this association in greater depth, based on our extensive experience with this diverse patient population, representing 12 different languages, we believe this association could be related to several potential factors. It is possible that many of these women come from cultures where it is improper to question recommendations from an authority figure, and hence, these women are more likely to be agreeable to the vaccine. The combination of this increased willingness to trust in the clinicians with a significant language barrier (eg, women not fully understanding what they are agreeing to) may have contributed to the lower rate of missed opportunities in this population group.
Of the missed opportunity visits, 26.5% occurred when another vaccine or injectable medication was administered. These visits are excellent opportunities for providers to encourage patients to receive the HPV immunization because studies have shown that patients are more willing to accept the HPV vaccine when it is viewed as routine or when given with other injections.33
Although some data suggest that providers are less likely to recommend the HPV vaccine to avoid giving multiple injections in 1 visit, Wallace et al34 found that providers overestimate concerns of patients about multiple immunizations, and education and reassurance from providers often address these concerns. This suggests that interventions that bundle administration of the HPV vaccine with other vaccines or injectable medications might help avoid missed opportunities in clinics that cater to young adults.
In obstetrics and gynecology clinics, many injectable medications (such as medroxyprogesterone acetate) are given during nurse-only visits. In our study, the large number of missed opportunities that occurred when other injectable medications were administered highlights the potential role of nurses in promoting uptake of HPV vaccine and the potential value in developing protocols for the nurse-initiated recommendation of the HPV vaccine.
The 2 most common missed opportunity visit types were for contraception and STD screening visits. As Dilley et al35 recently advocated, these visits could be prime opportunities for women’s health providers to improve the rates of HPV immunization because most of these patients are planning to become or already are sexually active, and a recommendation for HPV vaccine could easily be integrated into a broader discussion of reproductive health and family planning.
A common context for missed opportunities among young adult women during our study period were postpartum visits. In contrast to other vaccines such as Tdap (tetanus, diphtheria, and pertussis), influenza, and MMR (measles, mumps, and rubella), the HPV vaccine is not routinely available in the immediate inpatient postpartum period and may not be a priority for patients or providers in follow-up visits in the outpatient setting.36
One study of more than 48,000 age-eligible, unvaccinated pregnant women found that only 1.8% of the women had received a dose of HPV vaccine during the first postpartum year.37 Interventions focused on implementing routine HPV immunization during the inpatient postpartum admission and system-generated reminders to complete the immunization series in postpartum follow-up appointments are likely to improve the uptake in this age group.35,38,39
Our study has several limitations. This was a single-center study from a clinic that provides care to a predominantly low-income, minority population. Therefore, our findings may not be generalizable to other settings. Future research is needed in different clinical settings to validate our findings and inform the generalizability of our results.
Our data also relied on electronic medical records from a single health care system; immunizations administered by providers not affiliated with our system may not have been completely captured. This may result in a potential overestimation of missed opportunities. However, in our study population, this is unlikely to have been a major issue. In a different study from our institution, a sample of adult women who sought care at our clinic were interviewed to assess all prior sources of care since 2006, when the HPV vaccine was introduced. We found that an accurate HPV vaccine history could be ascertained in 82% of these women by reviewing electronic medical records because the majority of these adult women received care either exclusively at our clinic or at one of the other sites within the Yale–New Haven Hospital System (unpublished data).
In the self-report designations of race and ethnicity, the majority of women who designated themselves as being of Hispanic ethnicity did not provide a particular race, which is why we used a combined race/ethnicity variable.
Lastly, the data collection focused on detailed information about the missed opportunity visits. Similar information was not obtained about opportunities at which patients were immunized. Because only 3.1% of women appropriately received a dose of the HPV vaccine during the study period without any missed opportunity, the validity of comparisons of those visits would be impaired by poor statistical power.
Conclusions
This study, conducted in a diverse urban population, found that a majority of underimmunized vaccine-eligible young-adult women (18–26 years of age) had at least 1 missed opportunity in their interaction with an obstetrics and gynecology clinic over a 1 year study period, most of which were related to postpartum visits or to visits for either contraception or STD screening. Interventions that aim to eliminate these missed opportunities are likely to improve the uptake of the HPV vaccine in this population of young adult women.
Acknowledgments
This study was supported, in part, from grants from the American Cancer Society (Dr Oliveira), the Robert E. Leet and Clara Guthrie Patterson Trust (Dr Oliveira) and by Clinical and Translational Science Award grant numbers KL2 TR001862 (Drs Sheth and Shapiro), TL1TR001864 (Drs Oliveira and Shapiro), and UL1TR000142 (Dr Shapiro) from the National Center for Advancing Translational Science at the National Institutes of Health (NIH) and the NIH roadmap for Medical Research. The contents herein are solely the responsibility of the authors and do not necessarily represent the official views of National Institutes of Health.
Footnotes
The views expressed herein are those of the authors and do not necessarily represent the official views of the National Institutes of Health.
The authors report no conflict of interest.
Presented at the 31st International Papillomavirus Conference, Cape Town, South Africa, February 2017.
References
- 1.Weinstock H, Berman S, Cates W., Jr Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health. 2004;36:6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 2.Brotherton JM, Ogilvie GS. Current status of human papillomavirus vaccination. Curr Opin Oncol. 2015;27:399–404. doi: 10.1097/CCO.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 3.Schiffman M, Solomon D. Findings to date from the ASCUS-LSIL Triage Study (ALTS) Arch Pathol Lab Med. 2003;127:946–9. doi: 10.5858/2003-127-946-FTDFTA. [DOI] [PubMed] [Google Scholar]
- 4.Chesson HW, Ekwueme DU, Saraiya M, Watson M, Lowy DR, Markowitz LE. Estimates of the annual direct medical costs of the prevention and treatment of disease associated with human papillomavirus in the United States. Vaccine. 2012;30:6016–9. doi: 10.1016/j.vaccine.2012.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barr E, Sings HL. Prophylactic HPV vaccines: new interventions for cancer control. Vaccine. 2008;26:6244–57. doi: 10.1016/j.vaccine.2008.07.056. [DOI] [PubMed] [Google Scholar]
- 6.Petrosky E, Bocchini JA, Jr, Hariri S, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2015;64:300–4. [PMC free article] [PubMed] [Google Scholar]
- 7.Reagan-Steiner S, Yankey D, Jeyarajah J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:850–8. doi: 10.15585/mmwr.mm6533a4. [DOI] [PubMed] [Google Scholar]
- 8.Liu G, Markowitz LE, Hariri S, Panicker G, Unger ER. Seroprevalence of 9 human papillomavirus types in the United States, 2005–2006. J Infect Dis. 2016;213:191–8. doi: 10.1093/infdis/jiv403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elbasha EH, Dasbach EJ, Insinga RP. Model for assessing human papillomavirus vaccination strategies. Emerg Infect Dis. 2007;13:28–41. doi: 10.3201/eid1301.060438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Introcaso CE, Dunne EF, Hariri S, Panicker G, Unger ER, Markowitz LE. Pre-vaccine era human papillomavirus types 6, 11, 16 and 18 seropositivity in the U.S.A., National Health and Nutrition Examination Surveys, 2003–2006. Sex Transm Infect. 2014;90:505–8. doi: 10.1136/sextrans-2013-051490. [DOI] [PubMed] [Google Scholar]
- 11.Paavonen J, Naud P, Salmeron J, et al. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet. 2009;374:301–14. doi: 10.1016/S0140-6736(09)61248-4. [DOI] [PubMed] [Google Scholar]
- 12.Daniel-Ulloa J, Gilbert PA, Parker EA. Human papillomavirus vaccination in the United States: uneven uptake by gender, race/ethnicity, and sexual orientation. Am J Public Health. 2016;106:746–7. doi: 10.2105/AJPH.2015.303039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams WW, Lu PJ, O’Halloran A, et al. Vaccination coverage among adults, excluding influenza vaccination—United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64:95–102. [PMC free article] [PubMed] [Google Scholar]
- 14.Williams WW, Lu PJ, Saraiya M, et al. Factors associated with human papillomavirus vaccination among young adult women in the United States. Vaccine. 2013;31:2937–46. doi: 10.1016/j.vaccine.2013.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams WW, Lu PJ, O’Halloran A, et al. Surveillance of vaccination coverage among adult populations—United States, 2014. MMWR Surveill Summ. 2016;65:1–36. doi: 10.15585/mmwr.ss6501a1. [DOI] [PubMed] [Google Scholar]
- 16.Lim JW, Ashing-Giwa KT. Examining the effect of minority status and neighborhood characteristics on cervical cancer survival outcomes. Gynecol Oncol. 2011;121:87–93. doi: 10.1016/j.ygyno.2010.11.041. [DOI] [PubMed] [Google Scholar]
- 17.Vadaparampil ST, Kahn JA, Salmon D, et al. Missed clinical opportunities: provider recommendations for HPV vaccination for 11–12 year old girls are limited. Vaccine. 2011;29:8634–41. doi: 10.1016/j.vaccine.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunne EF, Stokley S, Chen W, Zhou F. Human papillomavirus vaccination of females in a large health claims database in the United States, 2006–2012. J Adolesc Health. 2015;56:408–13. doi: 10.1016/j.jadohealth.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mayne SL, duRivage NE, Feemster KA, Localio AR, Grundmeier RW, Fiks AG. Effect of decision support on missed opportunities for human papillomavirus vaccination. Am J Prev Med. 2014;47:734–44. doi: 10.1016/j.amepre.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walling EB, Benzoni N, Dornfeld J, et al. Interventions to improve HPV vaccine uptake: a systematic review. Pediatrics. 2016;138 doi: 10.1542/peds.2015-3863. [DOI] [PubMed] [Google Scholar]
- 21.Connecticut Department of Public Health. Epidemiological profile of HIV in Connecticut. 2016 Available at: http://www.ct.gov/dph/lib/dph/aids_and_chronic/surveillance/epiprofile.pdf. Accessed October 15, 2017.
- 22.Polednak AP, Flannery JT, Janerich DT. Cervical cancer rates by population size of towns: implications for cancer control programs. J Community Health. 1991;16:315–23. doi: 10.1007/BF01324516. [DOI] [PubMed] [Google Scholar]
- 23.Laprise JF, Markowitz LE, Chesson HW, Drolet M, Brisson M. Comparison of 2-dose and 3-dose 9-valent human papillomavirus vaccine schedules in the United States: a cost-effectiveness analysis. J Infect Dis. 2016;214:685–8. doi: 10.1093/infdis/jiw227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American College of Obstetricians and Gynecologists. ACOG Immunization Expert Work Group Committee on Adolescent Health Care. Human papillomavirus vaccination. ACOG Committee opinion no. 704. Obstet Gynecol. 2017;129:e173–8. [Google Scholar]
- 25.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168:76–82. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richards MJ, Peters M, Sheeder J. Human papillomavirus vaccine: continuation, completion, and missed opportunities. J Pediatr Adolesc Gynecol. 2016;29:117–21. doi: 10.1016/j.jpag.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 27.Chou B, Krill LS, Horton BB, Barat CE, Trimble CL. Disparities in human papillomavirus vaccine completion among vaccine initiators. Obstet Gynecol. 2011;118:14–20. doi: 10.1097/AOG.0b013e318220ebf3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel DA, Zochowski M, Peterman S, Dempsey AF, Ernst S, Dalton VK. Human papillomavirus vaccine intent and uptake among female college students. J Am Coll Health. 2012;60:151–61. doi: 10.1080/07448481.2011.580028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mills LA, Head KJ, Vanderpool RC. HPV vaccination among young adult women: a perspective from Appalachian Kentucky. Prev Chronic Dis. 2013;10:E17. doi: 10.5888/pcd10.120183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papilloma-virus vaccination, and race/ethnicity in the US National Immunization Survey. Am J Public Health. 2013;103:164–9. doi: 10.2105/AJPH.2011.300600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. National and state vaccination coverage among adolescents aged 13–17 years—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:671–7. [PubMed] [Google Scholar]
- 32.Stewart AM, Lindley MC, Cox MA. Medicaid provider reimbursement policy for adult immunizations. Vaccine. 2015;33:5801–8. doi: 10.1016/j.vaccine.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernstein HH, Bocchini JA, Jr, Committee on Infectious Diseases The need to optimize adolescent immunization. Pediatrics. 2017;139 doi: 10.1542/peds.2016-4187. [DOI] [PubMed] [Google Scholar]
- 34.Wallace AS, Mantel C, Mayers G, Mansoor O, Gindler JS, Hyde TB. Experiences with provider and parental attitudes and practices regarding the administration of multiple injections during infant vaccination visits: lessons for vaccine introduction. Vaccine. 2014;32:5301–10. doi: 10.1016/j.vaccine.2014.07.076. [DOI] [PubMed] [Google Scholar]
- 35.Dilley S, Scarinci I, Kimberlin D, Straughn JM., Jr Preventing human papilloma-virus-related cancers: we are all in this together. Am J Obstet Gynecol. 2017;216:576–9.e1. doi: 10.1016/j.ajog.2017.02.026. [DOI] [PubMed] [Google Scholar]
- 36.Beigi RH, Fortner KB, Munoz FM, et al. Maternal immunization: opportunities for scientific advancement. Clin Infect Dis. 2014;59(Suppl 7):S408–14. doi: 10.1093/cid/ciu708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kilfoyle KA, Rahangdale L, Dusetzina SB. Low uptake of human papillomavirus vaccine among postpartum women, 2006–2012. J Womens Health (Larchmt) 2016;25:1256–61. doi: 10.1089/jwh.2016.5834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wright JD, Govindappagari S, Pawar N, et al. Acceptance and compliance with postpartum human papillomavirus vaccination. Obstet Gynecol. 2012;120:771–82. doi: 10.1097/AOG.0b013e31826afb56. [DOI] [PubMed] [Google Scholar]
- 39.Berenson AB, Rahman M, Hirth JM, Rupp RE, Sarpong KO. A human papillomavirus vaccination program for low-income postpartum women. Am J Obstet Gynecol. 2016;215:318.e1–9. doi: 10.1016/j.ajog.2016.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]


