Abstract
Adults with ASD fall short of social outcomes of non-ASD peers in mid-life, as documented by currently published research. The aim of the current study was to extend what is known about social functioning, employment, independent living, and use of social services by examining details of the current life status for a population-based sample of adults with ASD (mean age = 35.5 years, range = 22.2 – 51.4). We collected outcome data via direct assessment and informant report for 169 individuals. Three-fourths of the sample had cognitive abilities in the intellectually-disabled range. Social functioning outcomes, as a single measure, mirror those reported previously for other samples, including samples with a high proportion of individuals with normal range intellectual abilities, with 20% achieving the most independent outcomes and 46% requiring high levels of support across most life areas. Participant subgroups who achieved maximal outcomes represented a range of social and intellectual abilities for several outcome metrics. Participants used high levels of public and private supports, yet specific areas of clear, unmet need were also identified.
Keywords: Adult, Autism spectrum disorder, Outcome, Longitudinal, Relationships, Employment, Housing, Legal, Transportation, Leisure
The number of studies on adult outcome of autism spectrum disorders (ASD) is small, but growing rapidly (Cottle et al., 2016). These studies often include social functioning outcomes for adults with ASD, reporting limited achievements among participants in employment, social relationships, independent living, and social service access. Limited outcomes are found even among individuals with ASD without intellectual disability (Howlin & Moss, 2012; Magiati et al., 2014; Tobin et al., 2014; Roy et al., 2015; Helles et al., 2016). Approximately 25 to 30% of adult participants with ASD are employed across the range of employment support types from sheltered to independent (Farley et al., 2009; Billstedt et al., 2011; Howlin et al., 2013; Roux et al., 2013; Howlin et al., 2014). The majority of adults with ASD remain in their parents’ home during adulthood (Howlin et al., 2000; Engstrom et al., 2003; Eaves & Ho, 2008; Farley et al., 2009; Esbensen et al., 2010; Chamak & Bonniau, 2016). Unfortunately, many adults with ASD experience significant frustration as they try to improve their social opportunities or find work commensurate with their training and abilities. Families provide substantial emotional and financial supports to the family member with ASD; this support often increases when children age out of public education (Seltzer et al., 2011; Van Bourgondien et al., 2014). Up to 12% are institutionalized (Howlin et al., 2000; Engstrom et al., 2003; Howlin et al., 2004; Eaves & Ho, 2008; Mazefsky et al., 2008). When indicators of independent functioning and general life attainments are collapsed into a single variable to describe adult life situations in an incremental manner, virtually all adults with ASD identified in childhood require ongoing assistance to maintain their community placement.
ASD symptoms usually decline in quantity and intensity over time (Piven et al., 1996; Seltzer et al., 2003; McGovern & Sigman, 2005; Shattuck et al., 2007). This may be due in part to individuals learning new and more adaptive skills in childhood, which is the focus of many early intensive and other intervention programs. Taylor, Smith, Mailick, Shattuck and others examined the trajectories of youth and adults with ASD (Shattuck, et al., 2007; Taylor et al., 2007; Taylor and Seltzer, 2010; Taylor and Seltzer, 2011; Smith et al., 2012; Taylor et al., 2014). Their analyses suggest that over time many adolescents and young adults with ASD demonstrated lower levels of autism symptoms and maladaptive behaviors, as well as improved daily living skills. However, the rate of amelioration of ASD symptoms and disruptive behavior slowed upon high school exit for many cognitively able young adults with ASD, which may have coincided with lower engagement in further education and/or employment (Taylor and Seltzer, 2010; Taylor et al., 2011). Functional skill development plateaued by the late 20’s for many (Smith et al., 2012). Successful engagement in educational programs or jobs was associated with continued gains in daily living skills and reductions in problematic ASD symptoms and maladaptive behaviors (Taylor et al., 2014). These results suggest some plausible explanations for the limited outcomes experienced by most adults with ASD across all levels of cognitive and functional abilities, many of whom have been unable to reach their career goals.
In a prior pilot study, we examined outcomes for members of a population-based cohort of adults with ASD and normal or near normal cognitive ability who were ascertained during childhood in the mid-1980’s (Ritvo et al., 1989; Farley et al., 2009). These 41 adults were diagnosed with DSM-III autism (American Psychiatric Association, 1980) and participated in a 20-year follow-up study. As a whole, cognitive functioning remained stable, with substantial individual variation. Daily living skills were closely associated with independent functioning in adulthood, and this sample achieved as good or slightly greater levels of independence in adulthood as had been reported for similar samples.
The current study evolved from this pilot study and included those participants as well as others from the original autism prevalence study who span the range of intellectual functioning. In addition, participants were included who did not meet DSM-III autism criteria in the 1980’s but were subsequently reclassified as having DSM-IV-TR autism spectrum disorder (American Psychiatric Association, 2000) through a systematic chart review process (Miller et al., 2013). Earlier reports on this extended cohort have described psychiatric comorbidities (Buck et al., 2014), mortality (Bilder et al., 2013), and co-occurring medical conditions (Jones et al., 2016). The aim of the current study is to extend the existing knowledge on adult outcomes related to social functioning, employment, independent living, and use of social services.
Methods
Participants
Between 1984 and 1988, researchers at the University of Utah and UCLA (Ritvo et al., 1989) conducted an epidemiological survey aimed at identifying all children with autism living in Utah and born between 1960 and 1984. Parent interviews, direct observations, and records reviews were used to achieve a consensus diagnosis for each case (cf. Ritvo et al., 1989 for details). In that study, 241 of the 489 participants were diagnosed with DSM-III autistic disorder, while 138 did not meet full diagnostic criteria. Another 110 were excluded because they declined participation, exceeded the age range, or were lost to follow-up.
Records for the 138 participants in the 1980’s epidemiological survey who did not meet full DSM-III autism criteria were re-evaluated using DSM-IV criteria and the Centers for Disease Control and Prevention’s Autism and Developmental Disabilities Monitoring (ADDM) Network records review methodology (Miller et al., 2013). Of these 138 individuals, 108 had sufficient behavioral information on file to conduct a record review. Sixty-four met case criteria and were included in the current study as prospective participants. The average childhood IQ estimate for these 64 individuals was significantly lower than the average estimate for the 241 participants who met the DSM-III criteria for autism in the 1980’s epidemiological survey. With the addition of these 64, prospective participants for the current study included 305 individuals with DSM-III or DSM-IV ASD diagnoses.
Attempts were made to contact those eligible for the current study using information from published telephone directories, public records databases, and contact information from the 1980’s epidemiological survey. Invitations to participate were mailed to potential participants and their parents. Phone calls were placed to those who did not respond within two weeks; a second letter was mailed one month later, followed by additional efforts to contact participants by phone. In a final attempt at recruitment, we went in person to the home addresses of individuals residing within one hour of Salt Lake City. Recruitment and data collection occurred from 2007 through 2012.
We use the term “participants” to refer to the adults with ASD about we whom we collected data for this study. We collected data directly from participants and from informants who knew participants well. Most often these were participants’ parents, but some adult siblings and support staff also provided information about the participants.
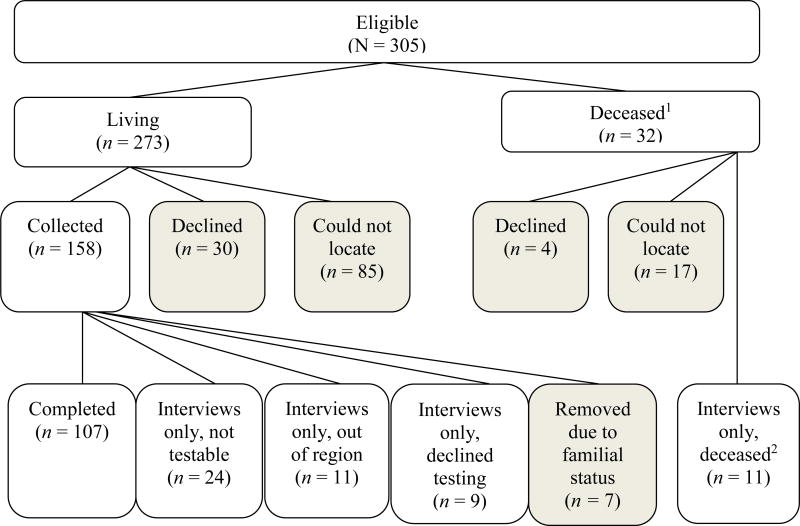
Data were collected for 169 (55%) of the total 305 potential participants (see Figure 1). Among the participants were 26 people who met DSM-IV criteria for ASD through the records-based re-evaluation process (Miller et al., 2013). The mean age of the participants was 35.5 (SD = 6.1, Range = 22.2–51.4) and included 128 males (76%). Two individuals who completed participation during the course of the study died before the study closed. Thus, 34 of the total 305 were known to have died by the study’s closure. There were also 7 sibling pairs among the 169 participants; in order to control for interdependence in results for those participants, one sibling from each pair was randomly removed. Table 1 shows basic characteristics of the final 162 participants, and the 143 whom we were not able to contact or who declined to participate.
Figure 1. Participation Status.
162 total participants (unshaded boxes); 143 non-participants (shaded boxes).
1 Two more individuals passed away in the course of the study, following their participation. They are included in the n collected. The final n deceased was 34.
2 Parents or other next of kin were interviewed for information concerning their family member with ASD
Table 1.
Sample Characteristics of 305 adults with DSM-III or DSM-IV diagnoses of ASD eligible for participation in the current study.
| Sample | Participants1 | Nonparticipants2 | Total Eligible |
|---|---|---|---|
| N | 162 | 143 | 305 |
| Mean age at Time 1 (years) | 7.5 | 7.6 | 7.5 |
| Mean age at Time 2 (years) | 35.4 | 33.9 | 34.6 |
| Male:Female ratio | 3.0:1 | 2.5:1 | 2.8:1 |
| Reclassified ASD (N) | 22 | 42 | 64 |
Excludes a random set of 7 first- or second-degree blood relatives for whom data were collected to ensure independence of data.
Unable to contact or declined to participate.
Ethics Approval
Approval was granted by the Institutional Review Boards of the University of Utah, Utah’s State Department of Human Services, and the Utah State Developmental Center.
Measures
Independent living
The Adult Outcome Interview (AOI), an informant-based interview developed for our study, was used to assess participants’ work histories and residential situations. Other areas of interest included use of social services, experiences with law enforcement, transportation, and chronic medical or co-occurring psychiatric conditions. Ratings defined by Engstrom et al. (2003) were used to describe levels of assistance provided by caregivers and social services. The AOI was completed for 150 participants who were living at the time of data collection.
Social functioning
In addition to questions about employment and independent living, the AOI included questions regarding social relationships and involvement in social organizations. Questions addressed historical and current friendships and romantic relationships. Informants were also asked to provide their impression of the participants’ level of interest in developing additional relationships.
Social Functioning Composite
Several investigators have used a set of broadly-defined categories to summarize the objective living, social, and employment situations in which adults with ASD live, often called the “Social Functioning Composite” (SFC). We used a set of categorical definitions devised by Howlin and colleagues (2004; see Table 2 for an abbreviated description and Howlin et al. (2004) for full details). Members of our team independently assigned a composite rating to each participant. Raters were trained to 85% agreement; individual case discrepancies were reviewed and consensus was reached through case conferences.
Table 2.
Social Functioning Composite Definitions (Howlin et al., 2004)
| Rating | Definition |
|---|---|
| Very Independent | Achieving a high level of independence, having some friends and a job |
| Independent | Generally in work but requiring some degree of support in daily living; some friends/acquaintances |
| Fair | Has some degree of independence, and although requires support and supervision does not need specialist residential provision; no close friends but some acquaintance |
| Limited | Requiring special residential provision/high level of support; no friends outside of residence |
| Very Limited | Needing high-level hospital care, no friends; no autonomy |
Autism Symptoms
Current presentation of autistic symptoms was assessed using the Autism Diagnostic Observation Schedule-Generic (ADOS; Lord et al., 2000), an observational measure used to directly assess behaviors characteristic of ASD. Three of the 4 modules (1, 2, and 4) were relevant for our population. Materials for Modules 1 and 2 were modified to maintain the purpose of tasks but to improve the age appropriateness of the materials for adult participants. These changes were made in consultation between a member of our group in the study’s planning stages (i.e., Judith Miller, PhD) and members of Catherine Lord’s laboratory at the University of Michigan. ADOS scores were obtained for 104 individuals. One-third of the study participants (n = 58) did not have ADOS scores. In some cases, the ADOS was not administered because parental report or our observations indicated the person was functioning at a mental age below 12 months. There were also instances in which we administered the ADOS, but the individual showed such limited responsiveness to the examiner that there were questions about the validity of the administration for assessing ASD characteristics. In other cases, participants were out of the region or declined to participate, themselves, in direct assessment.
Adult cognitive abilities
Participants’ current cognitive abilities were assessed using one of the following: Wechsler Adult Intelligence Scale, Third Edition (WAIS-III; Wechsler, 1997); Wechsler Adult Intelligence Scale, Fourth Edition (WAIS-IV; Wechsler, 2008); Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999); or Stanford-Binet, Fifth Edition (SB5; Roid, 2003). We obtained valid scores for 72 participants out of the 162 for whom data were collected (44%). Twenty-eight of the 72 participants were administered the SB5 (39%), and 44 were administered a Wechsler scale: WAIS-III (n = 32, 44%), WAIS-IV (n = 11, 15%), WASI (n = 1, 1%).
Statistical Analyses
Two tailed t-tests were used to compare interval-level variables. Spearman’s rho tests were used in nonparametric analyses.
Results
Representativeness of the Sample
Participants (n = 162) and non-participants (n = 143) were compared on 14 current and historical variables to estimate participation bias. Historical comparison data were drawn from epidemiologic survey datasets, and current data were extracted from the Utah Population Database (UPDB), a repository for genealogical, demographic, and medical information for families in Utah. Comparisons were made for gender; age at testing in childhood and current age; historical full scale, verbal, and nonverbal IQ; age at which parents were first concerned about their child’s development; age of single word use and use of phrase speech; acquisition of a driver’s license or state-issued identification card; histories of marriage and divorce; and birth of offspring. A statistically significant difference was identified between participants and non-participants only on the childhood IQ score, where participants had significantly higher scores (n = 150, M = 56.3, SD = 28.2) than did nonparticipants (n = 126, M = 47.9, SD = 25.4.; t(274) = 2.6, P = 0.01).
Diagnostic Stability
ADOS scores were obtained for 104 individuals. Module 1 was administered to 36 participants, among whom 34 met criteria for autism and 2 reached the threshold for ASD. Module 2 was administered to 16 participants, and all met criteria for autism. Fifty-two participants completed a Module 4. Of these, 34 met criteria for autism, and 7 obtained scores at the ASD level. Eleven participants did not meet criteria for an ASD on the ADOS. There were no significant gender differences in any category (i.e., autism, ASD, not ASD, refused, untestable).
Cognitive Abilities
Full scale IQ scores were obtained for 71 participants in adulthood (mean = 71.2, SD = 27.4, range = 40 – 140). IQ levels for another 56 were estimated at below 40 based on adaptive behavior scores, attempted psychometric assessment, and clinical judgment. Taken together, the scores and estimates combine to reflect cognitive functioning at the IQ level of 70 or below for 77% of this sample. Parents of one participant living across the country reported on his current full scale IQ based on recent testing. Only nonverbal IQ scores were obtainable for 2 others. In one case, administration of verbal subtests was disrupted by factors in the home testing environment. In another case, the participant obtained a valid nonverbal IQ score but could not perform on verbal subtests being nonverbal, himself. A detailed discussion of results of psychometric testing is beyond the scope of the current analysis.
Employment
We had current employment data for 153 individuals who were living at the time of data collection (Table 3). Examples of full-time and part-time work included: janitorial, restaurant, retail, trucking, library help, or work in a family business. There were participants working in various capacities within the IT field. Of the 11 participants who did not meet ASD diagnostic criteria on the ADOS Module 4 (an estimate of current functioning), only 6 were in competitive employment.
Table 3.
Daily Occupation
| n (%) | |
|---|---|
| Full-time, unsupported1 | 19 (12%) |
| Part-time, unsupported | 19 (12%) |
| Volunteer | 3 (2%) |
| Supported employment2 | 10 (7%) |
| Sheltered workshop3 | 21 (14%) |
| Day program | 51 (33%) |
| Unemployed | 30 (20%) |
This includes participants in full-time work or postsecondary education
“Supported employment” refers to working in a regular job with support from a job coach
“Sheltered workshops” are highly structured and supported work environments where individuals with significant functional impairments work in exchange for minimal pay.
Thirty (20%) individuals were completely unemployed at the time of data collection. Sixteen had never been employed or involved with any kind of structured adult program. The remaining 14 individuals had as many as 9 previous jobs, with difficulty sustaining employment or no desire to continue in day programming. Informants indicated that these participants had difficulty maintaining employment due to inflexibility with work schedules, social challenges, or the slow pace at which they worked. Some of these participants took significantly longer than expected to complete tasks. Other participants reportedly had difficulty getting along with co-workers or customers (e.g., could not tolerate the messes customers would make). Punctuality or missing work due to health problems were also reasons participants had difficulty keeping a job.
We collected employment and IQ data for 128 individuals. Although mean cognitive abilities were within the low average range for participants who were competitively employed on a part-time basis and within the average range for those in full-time employment, the full range of cognitive and functional ability levels was represented at the individual participant level. In fact, 10 of 38 participants with full- or part-time jobs had measured cognitive abilities below 70. The same was true for those who were completely unemployed; 12 of these 24 participants (with employment and IQ data) had IQ scores below 40 or were not testable, while 5 unemployed participants had scores of 80 or higher.
Informants were asked to comment on possible factors limiting outcomes. The following themes were most common: trouble with abstract concepts or novel experiences, difficulty staying on task and judging social situations, poor interviewing skills, requiring more supervision than other employees, and chronic health problems.
Friendships and Social Life
Eight participants (5%) had experience with marriage; 5 were men. Seven participants were married, and one of these was in his second marriage. Another participant had been married in the past but was divorced at the time of data collection.
Almost 75% of the participants had no experience with dating (n = 111). Twenty (13%) had dated only in a group setting, 8 (5%) had dated in only a single couple arrangement, and 10 (6%) had dated in both group and single couple interactions. Most of the individuals who had previous or current relationships (n = 24) reported having 1 or 2 relationships over their lifetime. Four participants had 3 to 6 relationships, which each lasted less than 3 years. One individual was reported as having up to 20 different relationships, most of which lasted less than a year.
Informants reported on the duration of relationships and reasons why they ended. There was wide variation in relationship duration, with most lasting less than 6 months (n =14). Five relationships lasted 6 months to 2 years. Another 5 lasted 2 to 3 years. Six relationships lasted 10 years or more. Informants reported many reasons for relationships ending, most often saying that the relationship was immature or there was an insurmountable level of dysfunction from either the participant or partner. Many parents reported that their son or daughter did not understand the nature of or the need for a relationship; others indicated that the adult with ASD had unrealistic ideas of what the relationship should entail or how they would want to meet their partner.
When asked whether they felt their adult child wished to have a romantic partner, informants for 29 participants (19%) said they believed the adult with ASD would like to be in a relationship. Informants for 103 (67%) participants felt that the adult with ASD did not want a romantic partner, and 13 (8%) said they were uncertain.
Informants were also asked about involvement in organized social and interest groups by the adult with ASD (Table 4). Over half of the participants were involved in at least one club or organization in which they regularly attended group meetings. Parents also estimated the average amount of time their adult child spent with peers per week. Just below half of the participants were reported as spending little or no time with their peers.
Table 4.
Social Participation
| n (%) | |
|---|---|
| Involved in organized groups | 86 (59%) |
| One club or organization | 6 (4%) |
| 2 clubs or organizations | 21 (15%) |
| 3 or more clubs or organizations | 5 (3%) |
| Time spent with peers per week | |
| Little or no time | 65 (47%) |
| 1 to 10 hours | 28 (20%) |
| 11 to 40 hours | 18 (13%) |
| 41 hours or more1 | 27 (20%)a |
In most cases those spending 40 hours or more with peers were living in sheltered living situations or participating in day programs.
Of those participating in groups, 67 (45%) indicated that they attended church. In 63 cases, participants belonged to the Church of Jesus Christ of Latter-Day Saints, the predominant religion in Utah. Examples of other organized activities included martial arts classes, Special Olympics, and self-advocacy organizations.
Transportation
About a third of the participants were able to travel independently, either by driving or public transit. Numbers of public transit users may be limited by availability of these services in different communities. Eleven participants (7%) had a driver’s license and drove regularly. Twenty-two participants independently took public transit on a regular basis (15%). Nine participants (6%) drove and took public transit regularly. Fourteen participants (9%) used a special public transit service for people with disabilities or rode regular public transit with support. Ninety-seven participants (62%) relied on family or social services staff to transport them.
Independent Living
Current residential data were available for 154 living individuals (see Table 5). On average, participants were reported to have lived in 2.7 residences across the course of their lives (SD = 2.2, range = 1 – 18). This includes long-term placements in pediatric residential treatment centers and therapeutic boarding schools. Six of the 11 people who did not meet diagnostic criteria on the ADOS were living with parents or siblings. The average current IQ of the 9 participants who lived independently and who were available for direct assessment was 107 (SD = 28.3, range = 65 - 134). Requisite levels of caregiver support were rated based on the strategy described by Engstrom et al. (2003, see Table 6).
Table 5.
Residential Situation
| n (%) | |
|---|---|
| Own home, purchased | 7 (5%) |
| Own apartment | 6 (4%) |
| Living with family of origin | 69 (47%) |
| Supported apartment, family | 5 (3%) |
| Supported apartment, public | 4 (3%) |
| Group home | 39 (27%) |
| Professional parent | 3 (2%) |
| Institution/ICF-MR | 13 (9%) |
Table 6.
Required Levels of Caregiver Support (based on Engstrom et al., 2003)
| Rating | Definition | n (%) |
|---|---|---|
| None | No contact with family | 2 (1%) |
| Low | Normal or near normal contact with parents, siblings and other relative; support and practical assistance from time to time | 18 (12%) |
| Moderate | Regular practical assistance at home; daily contact by phone or physically; help with local authorities | 20 (14%) |
| High | Extensive help with social contacts and employment sites; total control of economic affairs; lives with relatives from time to time | 103 (72%) |
Social Functioning Composite (SFC)
SFC ratings for our sample were: "Very Independent," 15 (10%); "Independent," 15 (10%); "Fair," 52 (34%); "Limited," 62 (41%); and "Very Limited," 7 (5%). The 30 participants with measured cognitive abilities of 70 or higher were described with: “Very Independent,” 9 (30%); “Independent” 8 (27%); “Fair,” 12 (40%); and “Limited” 1 (3%). SFC ratings for participants (n = 22, M = 7.7, SD = 2.9) who met DSM-IV criteria for ASD upon records-based re-evaluation (Miller et al., 2013) were not statistically different [t(148) = −2.1, P = n.s.) from the other participants (n = 128, M = 6.3, SD = 2.8).
Challenging Behaviors
We asked informants about participants’ aggressive or destructive behavior. Seventy-two (47%) were described as damaging property in the preceding year. Eighteen (12%) of these individuals also directed aggression toward themselves or others. An additional 14 (9%) participants had histories of damaging property or aggression toward themselves or others in the past but no current behavior of this type. In rare instances, participants were said to perform this behavior with no identifiable provocation, but most participants were only aggressive in response to frustrating situations or when experiencing problems with medical conditions.
Social Services
Individuals with an ASD in the U.S. may be eligible for various types of social services, including Vocational Rehabilitation, long term supports and services (LTSS) which include Medicaid Home and Community Based Waivers, Supplemental Security Income (SSI), and Medicaid. Informants provided information to estimate levels of public support required by participants. Ratings of these levels were made based on the strategy described by Engstrom et al. (2003, see Table 7).
Table 7.
Required Levels of Public Support (based on Engstrom et al., 2003)
| Rating | Definition | n (%) |
|---|---|---|
| None | No public support | 15 (10%) |
| Low | Advice and support from habilitation; regular home help service | 15 (10%) |
| Moderate | Continuous home support; sheltered job; job assistant; regular support from psychiatry and/or habilitation | 18 (12%) |
| High | Supported living; group home or institution; day center, personal assistant | 108 (69%) |
LTSS includes funding for adults with significant functional impairments to help pay for supports in their daily lives, including employment and residential supports and day programming. Over half of the participants (n = 106, 65%) received LTSS.
Vocational Rehabilitation provides funding to individuals with disabilities for services that will lead to employment in the open marketplace. These services are available to clients until they are employed successfully for several months. At the time of data collection, 12 participants (8%) were accessing Vocational Rehabilitation services, and 9 participants (6%) had previously accessed services.
Social Supplemental Income (SSI), a federal program that provides income assistance to individuals with disabilities, served 129 participants (83%). Individuals receiving SSI typically qualify for public health benefits through Medicaid. One hundred twenty-three participants (79%) were Medicaid beneficiaries. Fifty-six of these participants received their primary and mental health care in a Medicaid-funded medical home for individuals with neurodevelopmental disabilities and co-occurring psychiatric conditions, a unique resource in Utah (Weedon et al., 2012; Ruiz et al., 2016).
Encounters with Law Enforcement
Informants were asked about involvement with law enforcement. There were 35 interactions reported for 31 participants (20%). Eight events occurred in childhood, 3 during adolescence, and 24 in adulthood. Eleven cases involved clear social or behavioral misunderstandings, including participants appearing as though they were “on drugs”, stalking peers, and/or acting on compulsions on others’ property. One instance involved a participant disrobing in public as an adult under “untrained staff” supervision. One participant was coaxed into providing transportation for neurotypical peers committing a crime. Nine assault cases were reported resulting in charges for 3 participants; the remaining 6 were released. Three participants damaged property. Two participants threatened other people. Four people received moving vehicle violations for which one person lost his license. Two of these cases involved driving under the influence of alcohol. There were 2 cases of shoplifting, and 2 participants engaged with police because of episodes of rage. No sexual assault, homicide, or illegal drug use was cited for any participant.
Legal Guardianship
Seventy-five participants (44%) had a legal guardian. Legal guardians were almost all parents (n = 70). One participant had a sibling as her guardian, and the other 4 had professional guardians. Those with guardians and current full scale IQ scores had a mean full scale IQ of 55.7 (SD = 17.6). Thirty-five individuals with estimated IQ levels in the impaired range (i.e., below 70) did not have a legal guardian. Reasons offered anecdotally by caregivers for not obtaining guardianship were nearly always related to the expense of obtaining guardianship or confusion surrounding the guardianship process.
DISCUSSION
This study provides detailed information about the experiences and circumstances of a large, population-based cohort of children and youth with ASD after 25 years who are now in mid-life. The median estimated cognitive ability was below 50, with just over 75% functioning at a level of 70 or below. Social functioning composite scores were similar to those previously reported (Gillespie-Lynch et al., 2012; Steinhausen et al., 2016), even when compared to ASD outcome studies of adults with higher mean IQ (Howlin et al., 2004; Cederlund et al., 2008). Importantly, participants had somewhat higher childhood IQ scores than did nonparticipants, suggesting that our results may reflect more independent functioning than would be seen for the full sample. However, because all study participants were identified with significant social impairment during childhood in the mid-1980’s, albeit with some meeting DSM-IV ASD criteria, these results are most applicable to adults with ASD whose impairment raised concern for autism at that time. The outcomes experienced by our 33 participants with normal or near normal adult IQ inform our understanding of more intellectually-able adults. These results may reflect the challenges and successes experienced by the majority of adults who have been more recently identified with ASD or who are as-yet undiagnosed.
As would be expected given the high proportion of participants with co-occurring intellectual disability, participants require high levels of support from caregivers and public assistance programs. Most of those with intellectual disability received support from LTSS, and all received assistance through SSI and Medicaid. A larger proportion of this sample was employed than has been reported in most other studies (48% in work ranging from sheltered employment to full-time, competitive employment, compared to an estimated 25% in previous studies). Still, a sizeable proportion (20%) was without any structured daytime activities outside the home. Almost half of the participants (n = 69) continued to live with their families of origin, and of this group, 12 had measured cognitive abilities of 80 or higher. As has been described elsewhere (Seltzer et al., 2011), in some cases this was not perceived as burdensome or undesirable by family members of the adult child; rather, there was mutual benefit in terms of social relating and practical household support for families.
A smaller number of participants were married than has been reported in other studies (5% versus approximately 14%; Howlin & Moss, 2012), but around 25% had experience with dating. Importantly, parents of many of the participants reported that they felt their adult son or daughter did not desire a romantic relationship. This finding is an example of an aspect of life satisfaction for which some adults with ASD may desire a different outcome (i.e., no close romantic relationship) from most adults in the general population. This type of difference is why validated methods to assess subjective outcome for adults with ASD are needed.
As seen in other samples (Szatmari et al., 1989; Piven et al., 1996; Cederlund et al., 2008), some participants (n = 11) did not meet diagnostic criteria on the ADOS. However, 4 of these were not competitively employed, and 6 were still living with parents or siblings. All of these participants still struggled with important aspects of independent functioning in adulthood. The data were collected prior to the ADOS-2 release; future studies will inform the extent to which the ADOS-2 captures ASD behavioral symptoms in this subgroup. While the ADOS-2 may prove to be a better diagnostic test of ASD in adults, our data suggest that direct assessment without the use of collateral history may result in false negatives.
Our results demonstrate the unmet need for effective strategies aimed at securing and maintaining meaningful work opportunities for adults with ASD. This will require innovative methods for assessing employable skills, including sensory or social accommodations and matching individuals to specific employer needs. It will also require education and cultivation of employers to recognize openings within niches of opportunity where focus and ASD-enhanced skills add value to each specific business. Continued efforts to support adults with ASD in achieving their own career goals are critically important, including ways to comply with social expectations in the workplace as well as how to advocate for themselves around supports or accommodations.
Caregivers currently face barriers to establishing legal guardianship over their adult children or using other supported decision making procedures when needed. While 75% of this sample had intellectual disability, only 44% had a legal guardian. Many caregivers were aware of legal guardianship but faced financial and logistical obstacles to completing the process. The lack of guardianship or other formal supported decision making procedures among adults with autism and intellectual disability may inhibit both future care decisions and the availability of adults with autism and intellectual disability to participate in clinical trials or research associated with moderate risk.
The current availability of social opportunities was also inadequate to meet the needs of our adult participants. Although 58% of the adults with ASD participated in regularly-occurring social groups, caregivers emphasized the need for social opportunities that would substantially enhance the adult’s quality of life (e.g. an invitation to play basketball with peers or go out for ice cream once a week). It was important that these outings be something initiated by a peer rather than managed by the caregiver and that the peer also experience some enjoyment in the activity rather than doing so out of a sense of service for a few weeks before exiting from the relationship.
This sample included members who screened into the 1980’s study due to having some behaviors characterizing autism that did not meet DSM-III criteria in use at the time. The richness of the behavioral records allowed us to revisit those historical cases using DSM-IV criteria and ADDM Network methods (Miller et al., 2013). A higher proportion of the newly identified cases had intellectual disability than was recorded for the DSM-III participants (84% versus 66%). While the impact of changing criteria on identifying more individuals with milder symptom presentations of ASD is widely appreciated, results from the 2013 reclassification study demonstrated that the broadening definitions of Autistic Disorder over time also captured more individuals with intellectual disability.
While this study adds substantially to the understanding of details surrounding the outcomes of adults with ASD in mid-life, there are many limitations. In spite of our efforts to connect with all members of this cohort, we were unable to locate one-third of the original sample. This is not surprising in light of the fact that over two decades had passed since the original study. We suspect that many may have been lost to follow-up because they did not have information in public records databases that are generally derived from utility company registries and other sources used by adults living independently. Given the low levels of childhood cognitive abilities for the majority of those we could not locate, we suspect that many of these adults reside in long-term care facilities or other supported living agencies, where contact and access are limited by government regulations and the policies and procedures of individual facilities or agencies that aim to protect clients’ privacy.
Lastly, this study does not account for the subjective experiences of individuals with ASD, which are influenced by elements like the “fit” between a person and his or her environment (Henninger & Taylor, 2013). It is likely that if we were to account for important features of a person’s life like the person-environment fit, the distribution of outcome types would reflect better subjective outcomes. However, in using our outcome rating strategy for our large, population-based sample in mid-life, there is an opportunity to assimilate these findings into the existing body of research on this topic.
This study provides a close examination of several variables related to adult life in a sample that is similar in terms of overall outcome to other adult cohorts with ASD previously described. Nevertheless, much remains to be understood about the qualitative experience of the men and women living with ASD. Future research on adult cohorts should investigate the extent to which current social landscapes are satisfying. It is also essential that groups developing these methods include voices of adults with ASD and proxies for those who are unable to articulate their own values.
Lay Summary.
This paper describes the social functioning outcomes for 169 adults with ASD in mid-life. Adult participants spanned the full range of functional and cognitive ability levels, with over 75% functioning in the cognitively impaired range. While summary descriptions of outcomes for this sample were similar to those reported for other groups of adults, this report provides detailed information regarding employment outcomes, social relationships, leisure activities, participation in the community, residential situations, public service use, and involvement with law enforcement.
Acknowledgments
We thank the individuals and caregivers who have participated in the ongoing research projects at the Utah Autism Research Program. We would like to acknowledge the contributions of Judith Miller, PhD, Jubel Morgan, RN, Sarah Harward, PhD, Emily Haygeman, PhD, and Pauline Cordray, MA, EdS ed. adm. We would also like to acknowledge Drs. Riva-Ariella Ritvo and Edward Ritvo for their contribution to the original autism prevalence study and preservation of this important resource. Drs. Bilder and McMahon have served as consultants to BioMarin. Dr. McMahon has a patent with Lineagen. Megan Farley, PhD had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Contributor Information
Megan Farley, Waisman Center, University of Wisconsin – Madison, 1500 Highland Ave., Madison, WI 53705.
Kristina J. Cottle, University of Utah Department of Psychiatry, 501 Chipeta Way, Salt Lake City, Utah 84108
Deborah Bilder, University of Utah Department of Psychiatry, 501 Chipeta Way, Salt Lake City, Utah 84108.
Joseph Viskochil, University of Utah Department of Psychiatry, 501 Chipeta Way, Salt Lake City, Utah 84108.
Hilary Coon, University of Utah Department of Psychiatry, 501 Chipeta Way, Salt Lake City, Utah 84108.
William McMahon, University of Utah Department of Psychiatry, 501 Chipeta Way, Salt Lake City, Utah 84108.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. third. Washington DC: Author; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. fourth. Washington DC: Author; 2000. text revision. [Google Scholar]
- Bilder D, Botts EL, Smith KR, Pimentel R, Farley M, Viskochil J, McMahon WM, Block H, Ritvo E, Ritvo RA, Coon H. Excess mortality and causes of death in autism spectrum disorders: a follow up of the 1980s Utah/UCLA autism epidemiologic study. Journal of Autism and Developmental Disorders. 2013;43(5):1196–204. doi: 10.1007/s10803-012-1664-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billstedt E, Gillberg IC, Gillberg C. Aspects of quality of life in adults diagnosed with autism in childhood: a population-based study. Autism. 2011;15(1):7–20. doi: 10.1177/1362361309346066. [DOI] [PubMed] [Google Scholar]
- Buck TR, Viskochil J, Farley M, Coon H, McMahon WM, Morgan J, Bilder DA. Psychiatric comorbidity and medication use in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2014;44(12):3063–71. doi: 10.1007/s10803-014-2170-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cederlund M, Hagberg B, Billstedt E, Gillberg IC, Gillberg C. Asperger syndrome and autism: A comparative longitudinal follow-up study more than 5 years after original diagnosis. Journal of Autism and Developmental Disorders. 2008;38(1):72–85. doi: 10.1007/s10803-007-0364-6. [DOI] [PubMed] [Google Scholar]
- Chamak B, Bonniau B. Trajectories, long-term outcomes and family experiences of 76 adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2016;46(3):1084–1095. doi: 10.1007/s10803-015-2656-6. [DOI] [PubMed] [Google Scholar]
- Cottle KJ, McMahon WM, Farley M. Adults with autism spectrum disorders: Past, present, and future. In: Wright SD, editor. Autism spectrum disorder in mid and later life. Philadelphia, PA: Jessica Kingsley Publishers; pp. 30–51. [Google Scholar]
- Eaves LC, Ho H. Young adult outcome of autism spectrum disorders. Journal of Autism and Developmental Disorders. 2008;38(4):739–747. doi: 10.1007/s10803-007-0441-x. [DOI] [PubMed] [Google Scholar]
- Engstrom I, Ekstrom L, Emilsson B. Psychosocial functioning in a group of Swedish adults with Asperger syndrome or high-functioning autism. Autism. 2003;7(1):99–110. doi: 10.1177/1362361303007001008. [DOI] [PubMed] [Google Scholar]
- Esbensen AJ, Bishop S, Seltzer MM, Greenberg JS, Taylor JL. Comparisons between individuals with autism spectrum disorders and individuals with Down syndrome in adulthood. American Journal on Intellectual and Developmental Disabilities. 2010;115(4):277–90. doi: 10.1352/1944-7558-115.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley MA, McMahon WM, Fombonne E, Jenson WR, Miller J, Gardner M, Block H, Pingree CB, Ritvo ER, Ritvo RA, Coon H. Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Research. 2009;2(2):109–118. doi: 10.1002/aur.69. [DOI] [PubMed] [Google Scholar]
- Gillespie-Lynch K, Sepeta L, Wang Y, Marshall S, Gomez L, Sigman M, Hutman T. Early childhood predictors of the social competence of adults with autism. Journal of Autism and Developmental Disorders. 2012;42(2):161–74. doi: 10.1007/s10803-011-1222-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helles A, Gillberg IC, Gillberg C, Billstedt E. Asperger syndrome in males over two decades: Quality of life in relation to diagnostic stability and psychiatric comorbidity. Autism. 2017;21(4):458–469. doi: 10.1177/1362361316650090. [DOI] [PubMed] [Google Scholar]
- Henninger NA, Taylor JL. Outcomes of adults with autism spectrum disorders: A historical perspective. Autism. 2013;17(1):103–116. doi: 10.1177/1362361312441266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45(2):212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Howlin P, Mawhood L, Rutter M. Autism and developmental receptive language disorder – a follow-up comparison in early adult life. II: Social, behavioural, and psychiatric outcomes. Journal of Child Psychology and Psychiatry. 2000;41(5):561–578. doi: 10.1111/1469-7610.00643. [DOI] [PubMed] [Google Scholar]
- Howlin P, Moss P. Adults with autism spectrum disorders. The Canadian Journal of Psychiatry. 2012;57(5):275–283. doi: 10.1177/070674371205700502. [DOI] [PubMed] [Google Scholar]
- Howlin P, Moss P, Savage S, Rutter M. Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(6):572–81. doi: 10.1016/j.jaac.2013.02.017. [DOI] [PubMed] [Google Scholar]
- Howlin P, Savage S, Moss P, Tempier A, Rutter M. Cognitive and language skills in adults with autism: a 40-year follow-up. Journal of Child Psychology & Psychiatry. 2014;55(1):49–58. doi: 10.1111/jcpp.12115. [DOI] [PubMed] [Google Scholar]
- Jones KB, Cottle K, Bakian A, Farley M, Bilder D, Coon H, McMahon W. A description of medical conditions in adults with autism spectrum disorder: A follow up of the 1980s Utah/UCLA Autism Epidemiologic Study. Autism. 2016;20(5):551–561. doi: 10.1177/1362361315594798. [DOI] [PubMed] [Google Scholar]
- Kamio Y, Inada N, Koyama T. A nationwide survey on quality of life and associated factors of adults with high-functioning autism spectrum disorders. Autism. 2013;17(1):15–26. doi: 10.1177/1362361312436848. [DOI] [PubMed] [Google Scholar]
- Lounds J, Seltzer MM, Greenberg JS, Shattuck PT. Transition and change in adolescents and young adults with autism: longitudinal effects on maternal well-being. American Journal of Mental Retardation. 2007;112(6):401–17. doi: 10.1352/0895-8017(2007)112[401:TACIAA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Magiati I, Tay XW, Howlin P. Cognitive, language, social and behavioural outcomes in adults with autism spectrum disorders: A systematic review of longitudinal follow-up studies in adulthood. Clinical Psychology Review. 2014;34:73–86. doi: 10.1016/j.cpr.2013.11.002. [DOI] [PubMed] [Google Scholar]
- Mazefsky CA, Folstein SE, Lainhart JE. Overrepresentation of mood and anxiety disorders in adults with autism and their first-degree relatives: what does it mean? Autism Research. 2008;2:109–118. doi: 10.1002/aur.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern CW, Sigman M. Continuity and change from early childhood to adolescence in autism. Journal of Child Psychology and Psychiatry. 2005;46(4):401–408. doi: 10.1111/j.1469-7610.2004.00361.x. [DOI] [PubMed] [Google Scholar]
- Miller JS, Bilder D, Farley M, Coon H, Pinborough-Zimmerman J, Jenson W, Rice CE, Fombonne E, Pingree CB, Ritvo E, Ritvo RA, McMahon WM. Autism spectrum disorder reclassified: a second look at the 1980s Utah/UCLA Autism Epidemiologic Study. Journal of Autism and Developmental Disorders. 2013;43(1):200–10. doi: 10.1007/s10803-012-1566-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piven J, Harper J, Palmer P, Arndt S. Course of behavioral change in autism: A retrospective study of high-IQ adolescents and adults. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(4):523–529. doi: 10.1097/00004583-199604000-00019. [DOI] [PubMed] [Google Scholar]
- Renty J, Roeyers H. Quality of life in high-functioning adults with autism spectrum disorder: The predictive value of disability and support characteristics. Autism. 2007;10(5):511–524. doi: 10.1177/1362361306066604. [DOI] [PubMed] [Google Scholar]
- Ritvo ER, Freeman BJ, Pingree C, Mason-Brothers A, Jorde L, Jenson WR, McMahon WM, Petersen PB, Mo A, Ritvo A. The UCLA-University of Utah epidemiologic survey of autism: prevalence. American Journal of Psychiatry. 1989;146(2):194–199. doi: 10.1176/ajp.146.2.194. [DOI] [PubMed] [Google Scholar]
- Roid GH. Stanford-Binet Intelligence Scales: Fifth Edition. Itasca, IL: Riverside; 2003. [DOI] [PubMed] [Google Scholar]
- Roux AM, Shattuck PT, Cooper BP, Anderson KA, Wagner M, Narendorf SC. Postsecondary employment experiences among young adults with an autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(9):931–9. doi: 10.1016/j.jaac.2013.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy M, Prox-Vagedes V, Ohlmeier MD, Dillo W. Beyond childhood: psychiatric comorbidities and social background of adults with Asperger syndrome. Psychiatrica Danubina. 2015;27(1):50–59. [PubMed] [Google Scholar]
- Ruiz LM, Damron M, Jones KB, Weedon D, Carbone PS, Bakian AV, Bilder DA. Antipsychotic medication use and metabolic monitoring in an integrated outpatient clinic for individuals with autism and other neurodevelopmental disabilities. Journal of Autism and Developmental Disorders. 2016;46(6):1887–94. doi: 10.1007/s10803-016-2712-x. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Greenberg JS, Taylor JL, Smith L, Orsmond GI, Esbensen A, Hong J. Adolescents and adults with autism spectrum disorders. In: Amaral D, Geschwind D, Dawson G, editors. Autism Spectrum Disorders. New York: Oxford University Press; 2011. pp. 241–252. [Google Scholar]
- Seltzer MM, Krauss MW, Shattuck PT, Orsmond G, Swe A, Lord C. The symptoms of autism spectrum disorders in adolescence and adulthood. Journal of Autism and Developmental Disorders. 2003;33(6):565–581. doi: 10.1023/b:jadd.0000005995.02453.0b. [DOI] [PubMed] [Google Scholar]
- Shattuck PT, Seltzer MM, Greenberg JS, Orsmond GI, Bolt D, Kring S, Lounds J, Lord C. Change in autism symptoms and maladaptive behaviors in adolescents and adults with an autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;37(9):1735–1747. doi: 10.1007/s10803-006-0307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Maenner MJ, Seltzer MM. Developmental trajectories in adolescents and adults with autism: the case of daily living skills. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(6):622–31. doi: 10.1016/j.jaac.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhausen HC, Mohr Jensen C, Lauritsen MB. A systematic review and meta-analysis of the long-term overall outcome of autism spectrum disorders in adolescence and adulthood. Acta Psychiatrica Scandinavica. 2016;133(6):445–52. doi: 10.1111/acps.12559. [DOI] [PubMed] [Google Scholar]
- Szatmari P, Bartolucci G, Brenner R, Bond S, Rich S. A follow-up study of high-functioning autistic children. Journal of Autism and Developmental Disorders. 1989;19(2):213–225. doi: 10.1007/BF02211842. [DOI] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Changes in the autism behavioral phenotype during the transition to adulthood. Journal of Autism and Developmental Disorders. 2010;40(12):1431–46. doi: 10.1007/s10803-010-1005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Employment and post-secondary educational activities for young adults with autism spectrum disorders during the transition to adulthood. Journal of Autism and Developmental Disorders. 2011;41(5):566–74. doi: 10.1007/s10803-010-1070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Smith LE, Seltzer MR. Engagement in vocational activities promotes behavioral developmental for adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2014;44:1447–1460. doi: 10.1007/s10803-013-2010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin MC, Drager KD, Richardson LF. A systematic review of social participation for adults with autism spectrum disorders: support, social functioning, and quality of life. Research in Autism Spectrum Disorders. 2014;8:214–229. [Google Scholar]
- Van Bourgondien ME, Dawkins T, Marcus L. In: Adolescents and Adults with Autism Spectrum Disorders. Volkmar FR, et al., editors. Springer Science+Business Media; New York: 2014. pp. 15–36. 2014. [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence (WASI) San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale – Third Edition. San Antonio, TX: Psychological Corporation; 1997. [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale–Fourth Edition. Pearson; San Antonio, TX: Pearson; 2008. [Google Scholar]
- Weedon D, Carbone P, Bilder D, O’Brien S, Dorius J. Building a person-centered medical home: lessons from a program for people with developmental disabilities. Journal of Health Care for the Poor and Underserved. 2012;23:1600–1608. doi: 10.1353/hpu.2012.0175. [DOI] [PubMed] [Google Scholar]