Abstract
Metastatic lesions of the colon are a rare clinical entity that may present difficulties in management. The incidence of these metastases appears to be increasing, as a result of physicians’ greater awareness during follow-up investigations of a primary neoplasm. Furthermore, the presence of a greater proportion of these abnormalities at autopsy should be a triggering factor for further investigation for doctors dealing with colorectal oncology. Their clinical presentation may vary from asymptomatic to signs similar to those of colorectal cancer. However, immunohistological analysis is considered the cornerstone for differentiating metastases to the colon, originating from other primaries, from primary colorectal neoplasms. Survival reports and treatment options vary. This article concisely presents the main characteristics of the secondary lesions to the colon from neoplasms that metastasize to the large intestine (namely, lung, ovary, breast, prostate, kidney, and melanoma) focusing on their incidence, their clinical presentation and the workup investigation. Physicians aware of this uncommon entity are much better prepared to apply an efficient diagnosis and workup, as well as an appropriate treatment strategy.
Keywords: Metastatic lesions to colorectum, lung cancer, ovarian cancer, breast cancer, prostate cancer, renal cancer, melanoma
Introduction
Colorectal cancer (CRC) is the most common neoplasia in the gastrointestinal (GI) tract and the third most frequent malignancy worldwide, with an incidence approaching 1.5 million cases annually [1,2]. Furthermore, it is considered that over 600,000 deaths each year are attributable to tumors of the large intestine, making them the third cause of cancer-related deaths [3]. In contrast, metastatic neoplasms in the colon are an uncommon entity, emerging in approximately 1% of total colorectal cancers [4]. Although colonic metastases are generally a rare incidence, post-mortem investigations demonstrate a greater occurrence than expected [5,6].
Secondary involvement of colorectum is often diagnosed in patients with a known primary neoplasm, usually deriving from the lung, ovary, breast, prostate, kidney, skin, stomach, or hepatobiliary system [7,8]. In most cases there are multiple lesions; however, one third of them may still be asymptomatic or found only at autopsy. The commonest pathway of metastatic spreading to the bowel is through peritoneal seeding (typical of ovarian cancer), though hematogenous and lymphatic dissemination to the colon has also been reported, as in breast carcinoma, lung carcinoma, and melanoma (Fig. 1) [5,9-11].
Figure 1.
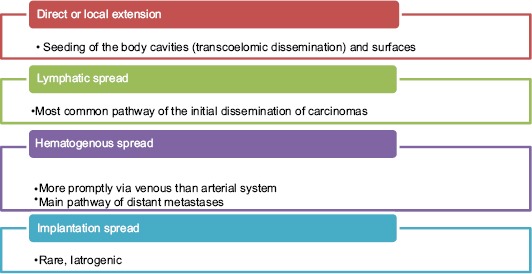
Main pathways of cancer metastasis
As regards the clinical presentation of metastatic lesion to colon, they may present with bowel obstruction, lower GI bleeding, anemia, and weight loss, though exuberant symptomatology is considered uncommon [12]. Acute abdomen is even rarer, with limited survival rates [7,8,13,14]. On the other hand, a third of such colonic metastases are asymptomatic or found only at autopsy, as mentioned above.
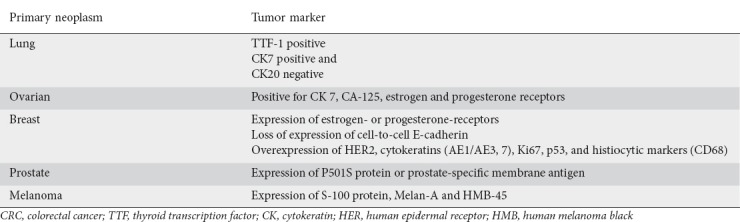
Therefore, the aim of this manuscript was to present a brief review of the most prevalent primary malignancies (namely, lung, ovary, breast, prostate, kidney, and melanoma) that metastasize to the colon, focusing on their frequency, their clinical presentation and the workup investigation. With regard to the latter, the histological and immunochemical study of specimens derived from colon biopsies seems to be the most crucial factor in the differential diagnosis of secondary tumors to the colon from other colorectal neoplasms (Table 1).
Table 1.
Evaluation of immunohistochemical markers indicative of primary tumors (other than CRC) which can metastasize to colorectum
Materials and methods
An extensive English-language literature search was conducted using PubMed to identify original studies and review articles, using as keywords “metastatic lesions to colorectum”, “lung cancer”, “ovarian cancer”, “breast cancer”, prostate cancer”, “renal cancer”, “melanoma”.
Lung cancer (LC) metastatic to colon
LC is the leading cause of cancer-related deaths in men and the second most common in women after breast cancer [15]. The most commonly involved organs of LC metastasis are the thoracic lymph nodes, liver, adrenal glands, brain, pleura, kidneys, and bones. The GI tract is an extremely rare field of LC metastasis and few cases have been reported [13,16-25]. In this context, Antler et al, in a separate autopsy series of 423 patients, found an overall 14% (58 cases) involvement of the GI tract from metastatic LC [19]. Of these, a majority (46%) were secondary to the direct infiltration of the esophageal wall, while the small and large bowel were involved in only 6% of the cases.
Colonic metastatic disease should be considered when a patient with LC presents with bowel obstruction, perforation, GI fistula, microcytic anemia, bleeding, and rarely bowel intussusception [26]. Therefore, it is deduced that there is no pathognomonic symptom that can lead us to the diagnosis of metastasis from primary LC to the large intestine. On the contrary, it seems that, based on the symptoms and the rarity of metastasis from lung to colon, it is very difficult to distinguish if the colon is the primary cancer site or a metastasis from LC.
Diagnosis of secondary disease of LC to colon can be made by radiological examination and/or endoscopy of the lower GI tract. Diagnostic tests such as computed tomography (CT) of the abdomen can reveal thickening of the bowel, whereas colonoscopy mainly shows a lesion of the intestinal wall that may cause bowel obstruction. During colonoscopy, biopsies should be taken to determine whether the cancer has metastasized from lung to colon. Immunohistochemistry is of utmost importance for the diagnosis and the differentiation of metastatic from primary colonic malignancy. Colorectal adenocarcinoma is typically CDX-2 positive, cytokeratin (CK) 20 positive, and CK7 negative. Most primary lung malignancies are TTF-1 positive, CK7 positive, and CK20 negative [27].
In conclusion, even though metastases from lung to large bowel exhibit a diminutive incidence, when patients with a history of LC diagnosis and/or treatment present with GI symptoms (pain, bleeding, acute abdomen, obstruction), the possibility of colonic secondary disease should be part of our differential diagnosis [26].
Ovarian cancer metastatic to colon
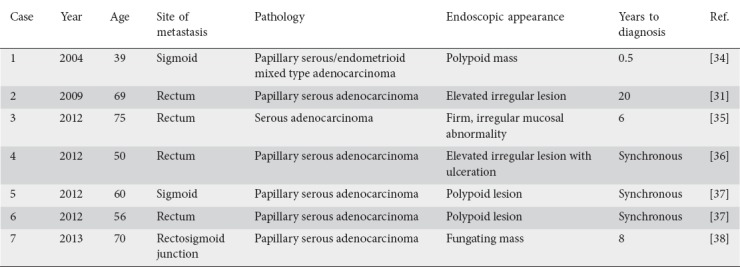
Ovarian cancer is the sixth most common malignancy worldwide, with an incidence of 11 in 100,000 people in Europe, being the most lethal gynecological cancer [28]. It mainly metastasizes to the pelvis, peritoneum and omentum, as well as the contralateral ovary and sigmoid colon. Distant extraperitoneal metastases are considered an extremely rare phenomenon [29]. Colonic metastases of ovarian origin account for 4-6% of cases [4,30]. The interval between the initial diagnosis and the development of metastases ranges from 1-22 years, with a mean of 9 years [31], whilst the age of affected patients ranges from 34-77 years, with a mean of 58.8 years [32]. Furthermore, it should be highlighted that certain cases have been described where the presence of colonic metastasis was synchronous with ovarian carcinoma (Table 2) [33-38].
Table 2.
Clinical characteristics of published colonic metastases from primary ovarian cancer
The pathway of dissemination of ovarian neoplasm to the colon and rectum may involve four different routes: lymphogenous, hematogenous, by direct infiltration of the bowel wall, or by spreading through the peritoneum [39]. The latter, known as the transcoelomic route, provides the most plausible pathophysiologic explanation for secondary disease to the colon.
Clinical manifestations of metastatic disease can be obscure; hence, patients may present abdominal discomfort, bowel obstruction or intussusception, a palpable abdominal mass, or may even be free of symptoms [31-33,39]. Diagnostic evaluation includes imaging, such as abdominal CT or ultrasonography, which can reveal unilateral or bilateral masses in the pelvis, regional lymphadenopathy, ascites or a mass on the colonic wall or intraluminally [30]. Endoscopy and subsequent assessment of biopsies are necessary for the diagnosis and identification of the tumor origin [30,33,40,41]. Finally, immunohistochemical evaluation with tumor markers, namely CEA, CA-125, CA 19-9, CK7 and CK20, estrogen and progesterone receptors, is paramount for the identification of the origin of the metastasis. Specifically, immunohistochemical staining positive for CK7, CA-125, estrogen and progesterone receptors is considered indicative of ovarian origin. On the other hand, a CK20 and CEA positive stain hints at a colorectal origin [30]. Interestingly, though a CK7 positive/CK20 negative immunophenotype is very unlikely to demonstrate a primary colon malignancy, CK7-/CK20+ phenotype is usually found in CRC biopsies [33,41].
Breast cancer metastatic to colon
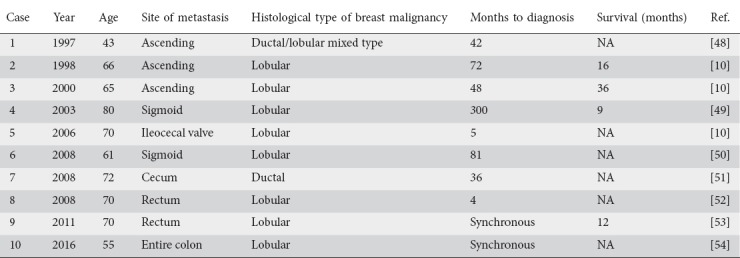
Breast cancer is considered as a common entity in oncology, accounting for approximately 32% of the total number of neoplasms, being at the same time a major mortality factor for women. Despite an increase in survival, which can be attributed to earlier diagnosis and improved therapeutic approach, it is estimated that 30% of patients will develop distant metastases, even after treatment. GI tract metastases are relatively rare, with some studies reporting colonic involvement in between 3% and 12% of cases [42-45]. They are associated with extensive disease and poor survival rates [46]. The most common histopathological subtype of GI tract metastasis seems to be invasive lobular carcinoma, which constitutes a mere 5-15% of total breast neoplasms (Table 3) [10,47-54]. The interval between the diagnosis of lobular carcinoma and colon metastasis is approximately 20-30 years [55]. Pathophysiologically, the main pathway responsible for colonic disease is hematogenous dissemination; however, peritoneal and lymphatic spreading have been documented [56].
Table 3.
Clinical characteristics of published colonic metastases from primary breast cancer
Clinical manifestations of metastatic lobular breast carcinoma to the colon are frequently non-specific and can usually pose a diagnostic challenge, as they can quite often imitate acute or chronic inflammatory processes, such as diverticulitis and inflammatory bowel diseases, or may mimic primary colonic tumors. Further diagnostic tests, such as radiology or endoscopy, are essential for the accurate diagnosis and treatment. CT imaging of the abdomen can reveal thickening of the intestinal wall, possibly with nodal infiltration [47]. Colonoscopy may reveal an abnormal lumen appearance, such as an intraluminal obstructing lesion or even multiple polypoid lesions [49,54]. Hence, female patients presenting new GI lesions, microcytic anemia and/or vague GI symptoms, especially those with a history of breast neoplasm, should be rigorously evaluated towards metachronous malignant lesions in the large intestine through pathologic evaluation and immunohistochemical analysis.
Histopathological examination of metastatic lobular breast carcinoma shows a typical pattern of invasion, with intramural infiltration throughout the submucosa, muscular propria and serosa. Tumor cells grow to form cords (Indian files) or small clusters [53,54]. They commonly present a signet-ring appearance. The absence of dysplasia or nuclear atypia in the colonic epithelium and the presence of infiltrating tumoral cells surrounding the preexistent glands is consistent with the diagnosis of metastatic tumor. Immunohistochemical study can help to rule out neoplasms with similar appearance, such as intestinal signet-ring cell carcinoma. More importantly, immunostaining can reveal the expression of estrogen or progesterone receptors and the loss of expression of cell-to-cell E-cadherin, consistent with the unique dispersion pattern of lobular carcinoma, in contrast to that of ductal carcinoma. Other immunohistochemical markers include overexpression of HER2, cytokeratins (AE1/AE3, 7), ki67, p53, and histiocytic markers (CD68), which can contribute to an accurate diagnosis by comparison to the immunophenotype of the breast neoplasm [47,55]
Prostate cancer (PCA) metastatic to colon
It is well known that two of the most prevalent tumors among adult males are PCA and CRC [57]. Although rare, the anatomical adjacency of these two organs predisposes to locoregional penetration by a locally advanced PCA with an occurrence of 1-12% [58]. This dissemination occurs through three different routes: direct invasion through Denonvilliers’ fascia and rectal infiltration; lymphatic spread through the common pelvic lymph node channels; and implantation along a needle biopsy tract in rectal or perirectal tissue [59,60]. The vast majority of metastases are localized to the sigmoid and rectum.
The clinical presentation includes any possible manifestation that a colorectal mass might present with. The absence of specific symptoms, in combination with the long interval between the initial PCA diagnosis and metastasis presentation (combined with a lack of serum prostate-specific antigen elevation in many cases), may often lead to an incorrect diagnosis of CRC. Lane et al, who studied 23 patients with a diagnosis of PCA metastasized to colon, reported that 19 of them had a PCA diagnosis 2-18 years before colorectal metastasis, whereas the remaining 4 patients had initially presented with lower GI symptoms [61]. Regarding the histological workup, signs of prostatic colonization, such as the presence of microacinar or acinar architecture and extensive lymphovascular invasion, are absent in most cases. Immunohistochemical investigation reveals a metastasis in case of the presence of at least one prostate-specific marker (P501S protein or prostate-specific membrane antigen) combined with the lack of markers of colonic differentiation [61,62].
Renal cancer metastatic to colon
Renal cell carcinoma (RCC) is the commonest renal cancer in adults and can exhibit metastatic spreading in almost 40% of cases, even after a radical excision [63]. Solitary metastasis has been reported in less than 10% of cases. Lungs, liver, bones and brain are the major target organs of metastatic renal disease, whilst less than 10 cases present secondary disease to the colon [64,65].
The range of symptoms and signs during the clinical assessment of colorectal metastases is wide and roughly identical with those of CRC, including mainly lower GI bleeding [64]. Likewise, findings of colonoscopy and biopsy specimens are nonspecific, as the current bibliography reveals. Additionally, the location of metastases in the large intestine does not provide useful information; lesions have been found along the entire colon, from cecum to rectum. In contrast, pathologic findings of late recurrences tend to be unique and are often associated with primary renal tumors of T2 stage or greater, being poorly differentiated [63].
A high level of clinical suspicion is required to track colorectal metastasis of RCC, because there are no definite guidelines for surveillance beyond 5 years postoperatively. However, a long-term longitudinal study of 3651 patients after surgery for M0 RCC showed that up to a third of RCC recurrences would have been missed if the guidelines of the National Comprehensive Cancer Network and American Urological Association were strictly followed [66]. Consequently, the increased likelihood of a late RCC recurrence requires the extension of postoperative monitoring.
Melanoma metastatic to colon
Melanoma is a type of skin cancer originating from the pigment-producing melanocytes in the basal layer of the epidermis [67]. The main cause of melanomas is ultraviolet radiation and the primary site of appearance is the skin (especially for those with “Type I” skin) [68,69]. Several rare genetic defects can also increase the risk [70]. Other common sites of primary lesions are the mouth, the eyes, and the GI tract (mainly the esophagus and the stomach) [68,69]. The tumor spreads through the lymph and the distant organs mostly affected are the liver, the lungs, the bones, and the brain [71]. Although melanoma metastasizes frequently to the GI tract (esophagus and stomach are the commonest sites), secondary colonic disease is rare. A study by Giuliano et al showed that, in 980 patients with metastasis from melanoma of unknown primary site, less than 7% had metastasis to the colon [72]. The absence of melanocytes in the colon, apart from the anorectal region, is probably the main reason that colonic metastases of melanoma rarely occur [73].
The most common sign of colonic metastasis in patients with melanoma is intestinal bleeding and obstruction or perforation [74]. Most colonic metastases are discovered after a CT or positron emission tomography-CT during regular surveillance. These patients undergo a colonoscopy because of its high sensitivity and specificity. Endoscopy with biopsies has an essential role in the diagnosis and identification of the tumor’s origin, which helps define the treatment that the patient will receive. Most melanomas have immunohistochemical staining positive for S-100 protein, Melan-A and HMB-45 [75].
Concluding remarks
Colorectal malignancies are considered amongst the deadliest to date, even though various techniques are available to prevent and detect their occurrence. Nevertheless, their detection, especially metastatic lesions to the colon, may be a difficult issue for physicians to resolve because of their rarity. Therefore, great awareness is needed during workup investigations and subsequent follow-up examinations for primary neoplasms, so as to prevent secondary pathologies to the colorectum. Thus, with this review we tried to highlight the main epidemiological, clinical, and histopathological features of metastatic disease from the most prevalent primary neoplasms presenting in the colorectum.
Biography
Evangelismos, Ophthalmiatreion Athinon and Polyclinic Hospitals; 401 General Military Hospital; Veterans Hospital 417 NIMTS, Athens, Greece
Footnotes
Conflict of Interest: None
References
- 1.Siegel R, Desantis C, Jemal A. Colorectal cancer statistics 2014. CA Cancer J Clin. 2014;64:104–117. doi: 10.3322/caac.21220. [DOI] [PubMed] [Google Scholar]
- 2.Galanopoulos M, Tsoukalas N, Papanikolaou IS, Tolia M, Gazouli M, Mantzaris GJ. Abnormal DNA methylation as a cell-free circulating DNA biomarker for colorectal cancer detection:A review of literature. World J Gastrointest Oncol. 2017;9:142–152. doi: 10.4251/wjgo.v9.i4.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galanopoulos M, Papanikolaou IS, Zografos E, et al. Comparative study of mutations in single nucleotide polymorphism loci of KRAS and BRAF genes in patients who underwent screening colonoscopy, with and without premalignant intestinal polyps. Anticancer Res. 2017;37:651–657. doi: 10.21873/anticanres.11360. [DOI] [PubMed] [Google Scholar]
- 4.Caramella E, Bruneton JN, Roux P, Aubanel D, Lecomte P. Metastases of the digestive tract. Report of 77 cases and review of the literature. Eur J Radiol. 1983;3:331–338. [PubMed] [Google Scholar]
- 5.Eyres KS, Sainsbury JR. Large bowel obstruction due to metastatic breast cancer:an unusual presentation of recurrent disease. Br J Clin Pract. 1990;44:333–334. [PubMed] [Google Scholar]
- 6.Jang HJ, Lim HK, Kim HS, et al. Intestinal metastases from gastric adenocarcinoma:helical CT findings. J Comput Assist Tomogr. 2001;25:61–67. doi: 10.1097/00004728-200101000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Remo A, Zanella C, Pancione M, et al. Lung metastasis from TTF-1 positive sigmoid adenocarcinoma. Pitfalls and management. Pathologica. 2013;105:69–72. [PubMed] [Google Scholar]
- 8.Habeşoğlu MA, Oğuzülgen KI, Oztürk C, Akyürek N, Memiş L. A case of bronchogenic carcinoma presenting with acute abdomen. Tuberk Toraks. 2005;53:280–283. [PubMed] [Google Scholar]
- 9.Feczko PJ, Collins DD, Mezwa DG. Metastatic disease involving the gastrointestinal tract. Radiol Clin North Am. 1993;31:1359–1373. [PubMed] [Google Scholar]
- 10.Taal BG, den Hartog Jager FC, Steinmetz R, Peterse H. The spectrum of gastrointestinal metastases of breast carcinoma:II. The colon and rectum. Gastrointest Endosc. 1992;38:136–141. doi: 10.1016/s0016-5107(92)70378-2. [DOI] [PubMed] [Google Scholar]
- 11.Reintgen DS, Thompson W, Garbutt J, Seigler HF. Radiologic, endoscopic, and surgical considerations of melanoma metastatic to the gastrointestinal tract. Surgery. 1984;95:635–639. [PubMed] [Google Scholar]
- 12.Gateley CA, Lewis WG, Sturdy DE. Massive lower gastrointestinal haemorrhage secondary to metastatic squamous cell carcinoma of the lung. Br J Clin Pract. 1993;47:276–277. [PubMed] [Google Scholar]
- 13.Hirasaki S, Suzuki S, Umemura S, Kamei H, Okuda M, Kudo K. Asymptomatic colonic metastases from primary squamous cell carcinoma of the lung with a positive fecal occult blood test. World J Gastroenterol. 2008;14:5481–5483. doi: 10.3748/wjg.14.5481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woods JM, 4th, Koretz MJ. Emergency abdominal surgery for complications of metastatic lung carcinoma. Arch Surg. 1990;125:583–585. doi: 10.1001/archsurg.1990.01410170029005. [DOI] [PubMed] [Google Scholar]
- 15.World Cancer Report 2014.World Health Organization 2014. Chapter 1.1. ISBN 9283204298 [Google Scholar]
- 16.Centeno Cortés C, Borau Clavero MJ, Sanz Rubiales A, López-Lara Martín F. Intestinal bleeding in disseminated non-small cell lung cancer. Lung Cancer. 1997;18:101–105. doi: 10.1016/s0169-5002(97)00050-0. [DOI] [PubMed] [Google Scholar]
- 17.Carr CS, Boulos PB. Two cases of solitary metastases from carcinoma of the lung presenting as primary colonic tumours. Br J Surg. 1996;83:647. doi: 10.1002/bjs.1800830519. [DOI] [PubMed] [Google Scholar]
- 18.Otera H, Ikeda F, Nakagawa S, et al. Intussusception of small intestine due to metastasis of large cell carcinoma of the lung with a rhabdoid phenotype. Eur Respir Rev. 2010;19:248–252. doi: 10.1183/09059180.00001610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Antler AS, Ough Y, Pitchumoni CS, Davidian M, Thelmo W. Gastrointestinal metastases from malignant tumors of the lung. Cancer. 1982;49:170–172. doi: 10.1002/1097-0142(19820101)49:1<170::aid-cncr2820490134>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 20.Fujiwara A, Okami J, Tokunaga T, Maeda J, Higashiyama M, Kodama K. Surgical treatment for gastrointestinal metastasis of non-small-cell lung cancer after pulmonary resection. Gen Thorac Cardiovasc Surg. 2011;59:748–752. doi: 10.1007/s11748-011-0811-3. [DOI] [PubMed] [Google Scholar]
- 21.Stinchcombe TE, Socinski MA, Gangarosa LM, Khandani AH. Lung cancer presenting with a solitary colon metastasis detected on positron emission tomography scan. J Clin Oncol. 2006;24:4939–4940. doi: 10.1200/JCO.2006.06.3354. [DOI] [PubMed] [Google Scholar]
- 22.John AK, Kotru A, Pearson HJ. Colonic metastasis from bronchogenic carcinoma presenting as pancolitis. J Postgrad Med. 2002;48:199–200. [PubMed] [Google Scholar]
- 23.Carroll D, Rajesh PB. Colonic metastases from primary squamous cell carcinoma of the lung. Eur J Cardiothorac Surg. 2001;19:719–720. doi: 10.1016/s1010-7940(01)00646-7. [DOI] [PubMed] [Google Scholar]
- 24.Brown KL, Beg RA, Demany MA, Lacerna MA. Rare metastasis of primary bronchogenic carcinoma to sigmoid colon:report of a case. Dis Colon Rectum. 1980;23:343–345. doi: 10.1007/BF02586842. [DOI] [PubMed] [Google Scholar]
- 25.Pezzuto A, Mariotta S, Fioretti F, Uccini S. Metastasis to the colon from lung cancer presenting with severe hyponatremia and dyspnea in a young male:A case report and review of the literature. Oncol Lett. 2013;5:1477–1480. doi: 10.3892/ol.2013.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goh BK, Yeo AW, Kong HN, Ooi LL, Wong W. Laparotomy for acute complications of gastrointestinal metastases from lung cancer:is it worthwhile or futile effort? Surg Today. 2007;37:370–374. doi: 10.1007/s00595-006-3419-y. [DOI] [PubMed] [Google Scholar]
- 27.Su YC, Hsu YC, Chai CY. Role of TTF-1, CK20, and CK7 immunohistochemistry for diagnosis of primary and secondary lung adenocarcinoma. Kaohsiung J Med Sci. 2006;2B(2):14–19. doi: 10.1016/S1607-551X(09)70214-1. [DOI] [PubMed] [Google Scholar]
- 28.Chornokur G, Amankwah EK, Schildkraut JM, Phelan CM. Global ovarian cancer health disparities. Gynecol Oncol. 2013;129:258–264. doi: 10.1016/j.ygyno.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lengyel E. Ovarian cancer development and metastasis. Am J Pathol. 2010;177:1053–1064. doi: 10.2353/ajpath.2010.100105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dvoretsky PM, Richards KA, Bonfiglio TA. The pathology and biologic behavior of ovarian cancer. An autopsy review. Pathol Annu. 1989;24:1–24. [PubMed] [Google Scholar]
- 31.Shibahara K, Endo K, Ikeda T, et al. Colon metastasis 20 years after the removal of ovarian cancer:Report of a case. Surg Today. 2009;39:153–156. doi: 10.1007/s00595-008-3809-4. [DOI] [PubMed] [Google Scholar]
- 32.Reed E, Zerbe CS, Brawley OW, et al. Analysis of autopsy evaluations of ovarian cancer patients treated at the National Cancer Institute 1972-1988. Am J Clin Oncol. 2000;23:107–116. doi: 10.1097/00000421-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Loy TS, Calaluce RD, Keeney GL. Cytokeratin immunostaining in differentiating primary ovarian carcinoma from metastatic colonic adenocarcinoma. Mod Pathol. 1996;9:1040–1044. [PubMed] [Google Scholar]
- 34.Zighelboim I, Broaddus R, Ramirez PT. Atypical sigmoid metastasis from a high-grade mixed adenocarcinoma of the ovary. Gynecol Oncol. 2004;94:850–853. doi: 10.1016/j.ygyno.2004.05.058. [DOI] [PubMed] [Google Scholar]
- 35.Yarze J. Ovarian carcinoma metastatic to the colon. Am J Gastroenterol. 2009;104(Suppl 3):S318–S351. [Google Scholar]
- 36.Akhtar K, Sherwani R, Anees A. Synchronous ovarian carcinoma with colorectal metastases:an unusual presentation. Clin Pract. 2012;2:e53. doi: 10.4081/cp.2012.e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shimazaki J, Tabuchi T, Nishida K, et al. Synchronous ovarian metastasis from colorectal cancer:A report of two cases. Oncol Lett. 2016;12:257–261. doi: 10.3892/ol.2016.4553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim JR, Kim BM, Kim YM, Lee WA, Namgung H. Colonic metastasis presenting as an intraluminal fungating mass 8 years after surgery for ovarian cancer. Ann Coloproctol. 2015;31:198–201. doi: 10.3393/ac.2015.31.5.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O'Hanlan KA, Kargas S, Schreiber M, et al. Ovarian carcinoma metastases to gastrointestinal tract appear to spread like colon carcinoma:implications for surgical resection. Gynecol Oncol. 1995;59:200–206. doi: 10.1006/gyno.1995.0008. [DOI] [PubMed] [Google Scholar]
- 40.Lindner V, Gasser B, Debbiche A, Tomb L, Vetter JM, Walter P. Ovarian metastasis of colorectal adenocarcinomas. A clinico-pathological study of 41 cases. Ann Pathol. 1999;19:492–498. [PubMed] [Google Scholar]
- 41.Rekhi B, George S, Madur B, Chinoy RF, Dikshit R, Maheshwari A. Clinicopathological features and the value of differential Cytokeratin 7 and 20 expression in resolving diagnostic dilemmas of ovarian involvement by colorectal adenocarcinoma and vice-versa. Diagn Pathol. 2008;3:39. doi: 10.1186/1746-1596-3-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Graham WP, 3rd, Goldman L. Gastrointestinal metastases from carcinoma of the breast. Ann Surg. 1964;159:477–480. [PMC free article] [PubMed] [Google Scholar]
- 43.Klein MS, Sherlock P. Gastric and colonic metastases from breast cancer. Am J Dig Dis. 1972;17:881–886. doi: 10.1007/BF02239526. [DOI] [PubMed] [Google Scholar]
- 44.Cifuentes N, Pickren JW. Metastases from carcinoma of mammary gland:an autopsy study. J Surg Oncol. 1979;11:193–205. doi: 10.1002/jso.2930110303. [DOI] [PubMed] [Google Scholar]
- 45.Hartmann WH, Sherlock P. Gastroduodenal metastases from carcinoma of the breast. An adrenal steroid-induced phenomenon. Cancer. 1961;14:426–431. doi: 10.1002/1097-0142(196103/04)14:2<426::aid-cncr2820140223>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 46.Washington K, McDonagh D. Secondary tumors of the gastrointestinal tract:surgical pathologic findings and comparison with autopsy survey. Mod Pathol. 1995;8:427–433. [PubMed] [Google Scholar]
- 47.Winston CB, Hadar O, Teicher JB, et al. Metastatic lobular carcinoma of the breast:patterns of spread in the chest, abdomen and pelvis on CT. AJR Am J Roentgenol. 2000;175:795–800. doi: 10.2214/ajr.175.3.1750795. [DOI] [PubMed] [Google Scholar]
- 48.Uygun K, Kocak Z, Altaner S, Cicin I, Tokatli F, Uzal C. Colonic metastasis from carcinoma of the breast that mimics a primary intestinal cancer. Yonsei Med J. 2006;47:578–582. doi: 10.3349/ymj.2006.47.4.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mistrangelo M, Cassoni P, Mistrangelo M, et al. Obstructive colon metastases from lobular breast cancer:report of a case and review of the literature. Tumori. 2011;97:800–804. doi: 10.1177/030089161109700619. [DOI] [PubMed] [Google Scholar]
- 50.Wadah A, Zakir KM, Thekkinkattil D. Colonic metastasis from a breast carcinoma, an unusual colonoscopic finding. BJMP. 2016;9:a901. [Google Scholar]
- 51.Birla R, Mahawar KK, Orizu M, Siddiqui MS, Batra A. Caecal metastasis from breast cancer presenting as intestinal obstruction. World J Surg Oncol. 2008;6:47. doi: 10.1186/1477-7819-6-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eljabu W, Finch G, Nottingham J, Vaingankar N. Metastatic deposits of breast lobular carcinoma to small bowel and rectum. Int J Breast Cancer. 2011;2011:413949. doi: 10.4061/2011/413949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Arrangoiz R, Papavasiliou P, Dushkin H, Farma JM. Case report and literature review:Metastatic lobular carcinoma of the breast an unusual presentation. Int J Surg Case Rep. 2011;2:301–305. doi: 10.1016/j.ijscr.2011.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Albero-González R, Gimeno-Beltrán J, Vázquez de las Heras I, et al. Lobular breast carcinoma with colonic metastases:A synchronous diagnosis in a 4-day period. Human Pathology:Case Reports. 2017;7:27–30. [Google Scholar]
- 55.Grewal J, Zhou H, Factor R, Kesari S. Isolated loss of hormonal receptors in leptomeningeal metastasis from estrogen receptor- and progesterone receptorpositive lobular breast cancer. J Clin Oncol. (e200-) 2010;28:e202. doi: 10.1200/JCO.2009.25.3518. [DOI] [PubMed] [Google Scholar]
- 56.Gifaldi AS, Petros JG, Wolfe GR. Metastatic breast carcinoma presenting as persistent diarrhea. J Surg Oncol. 1992;51:211–215. doi: 10.1002/jso.2930510317. [DOI] [PubMed] [Google Scholar]
- 57.Jemal A, Murray T, Ward E, et al. Cancer statistics 2005. CA Cancer J Clin. 2005;55:10–30. doi: 10.3322/canjclin.55.1.10. [DOI] [PubMed] [Google Scholar]
- 58.Bowrey DJ, Otter MI, Billings PJ. Rectal infiltration by prostatic adenocarcinoma:report on six patients and review of the literature. Ann R Coll Surg Engl. 2003;85:382–385. doi: 10.1308/003588403322520726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Murray SK, Breau RH, Guha AK, Gupta R. Spread of prostate carcinoma to the perirectal lymph node basin:analysis of 112 rectal resections over a 10-year span for primary rectal adenocarcinoma. Am J Surg Pathol. 2004;28:1154–1162. doi: 10.1097/01.pas.0000131543.80147.3d. [DOI] [PubMed] [Google Scholar]
- 60.Vaghefi H, Magi-Galluzzi C, Klein EA. Local recurrence of prostate cancer in rectal submucosa after transrectal needle biopsy and radical prostatectomy. Urology. 2005;66:881. doi: 10.1016/j.urology.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 61.Lane Z, Epstein JI, Ayub S, Netto GJ. Prostatic adenocarcinoma in colorectal biopsy:clinical and pathologic features. Hum Pathol. 2008;39:543–549. doi: 10.1016/j.humpath.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 62.Abbas TO, Al-Naimi AR, Yakoob RA, Al-Bozom IA, Alobaidly AM. Prostate cancer metastases to the rectum:A case report. World J Surg Onc. 2011;9:56. doi: 10.1186/1477-7819-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fujii Y, Ikeda M, Kurosawa K, et al. Different clinicopathological features between patients who developed early and late recurrence following surgery for renal cell carcinoma. Int J Clin Oncol. 2015;20:802–807. doi: 10.1007/s10147-014-0775-2. [DOI] [PubMed] [Google Scholar]
- 64.Saitoh H. Distant metastasis of renal adenocarcinoma. Cancer. 1981;48:1487–1491. doi: 10.1002/1097-0142(19810915)48:6<1487::aid-cncr2820480635>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 65.Vo E, Palacio C, Omino R, Link RE, Sada Y, Avo A. Solitary colon metastasis from renal cell carcinoma nine years after nephrectomy:A case report. Int J Surg Case Rep. 2016;27:55–58. doi: 10.1016/j.ijscr.2016.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stewart SB, Thompson RH, Psutka SP, et al. Evaluation of the National Comprehensive Cancer Network and American Urological Association renal cell carcinoma surveillance guidelines. J Clin Oncol. 2014;32:4059–4065. doi: 10.1200/JCO.2014.56.5416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.National Cancer Institute. Melanoma. Treatment for health professionals (PDQR) 2015 [Google Scholar]
- 68.Guo Lian C, Mihm MC., Jr Stewart BW, Wild CP, editors. Skin cancer. World Cancer Report 2014. World Health Organization. 2014:495–502. [Google Scholar]
- 69.Kanavy HE, Gerstenblith MR. Ultraviolet radiation and melanoma. Semin Cutan Med Surg. 2011;30:222–228. doi: 10.1016/j.sder.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 70.Azoury SC, Lange JR. Epidemiology, risk factors, prevention, and early detection of melanoma. Surg Clin North Am. 2014;94:945–962, vii. doi: 10.1016/j.suc.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 71.Fiddler IJ. Melanoma metastasis. Cancer Control. 1995;2:398–404. doi: 10.1177/107327489500200503. [DOI] [PubMed] [Google Scholar]
- 72.Giuliano AE, Moseley HS, Morton DL. Clinical aspects of unknown primary melanoma. Ann Surg. 1980;191:98–104. doi: 10.1097/00000658-198001000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schuchter LM, Green R, Fraker D. Primary and metastatic diseases in malignant melanoma of the gastrointestinal tract. Curr Opin Oncol. 2000;12:181–185. doi: 10.1097/00001622-200003000-00014. [DOI] [PubMed] [Google Scholar]
- 74.Tessier DJ, McConnell EJ, Young-Fadok T, Wolff BG. Melanoma metastatic to the colon:case series and review of the literature with outcome analysis. Dis Colon Rectum. 2003;46:441–447. doi: 10.1097/01.DCR.0000059657.64526.B6. [DOI] [PubMed] [Google Scholar]
- 75.Elder DE, Lever WF. Lever's histopathology of the skin. 10th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2009. [Google Scholar]


