Abstract
Background
Those with mild cognitive impairment (MCI) are ten times more like to develop Alzheimer’s disease (AD) than the general population. MCI diagnosis and early intervention are helpful for the diagnosis and treatment of AD in its early stages, thus delaying its development and improving the quality of life for those with MCI.
Aims
To analyze the relationship between the lifestyle of the elderly in Shanghai communities and mild cognitive impairment and to look for preventative lifestyle measures for the elderly with mild cognitive impairment.
Methods
1005 elderly persons were randomly selected from the community in Shanghai. Study participants were 265 people with an MCI diagnosis and 607 non-MCI elderly persons. The demographic and lifestyle data of these elderly people were collected for univariate and multivariate analysis to search for statistically significant indicators.
Results
The univariate analysis revealed that smoking (χ2= 10.808, p=0.001), tea drinking (χ2=11.74, p= 0.001), having hobbies (χ2= 20.815, p<0.001), reading (χ2=28.670, p= 0.001), surfing the internet (χ2=12.623, p= 0.001), and photography (χ2=4.470, p= 0.034) were protective factors for MCI. The binary logistic regression, a multivariate analysis, revealed that smoking, reading, and surfing the internet had statistical significance. Their OR values were 0.562 (0.358-0.883), 0.428 (0.253-0.726), and 0.238 (0.071-0.797) respectively. Thus, smoking, reading, and surfing the internet were protective factors for MCI.
Conclusions
Lifestyle is associated with the onset of MCI. Good life habits and behaviors are significant in the prevention of MCI developing into Alzheimer’s.
Key words: mild cognitive impairment, lifestyle, protective factors
Abstract
背景
轻度认知功能损害(Mild cognitive impairment,MCI)老人发展为阿尔茨海默病(Alzheimer’s disease,AD)的风险比普通人群高10 倍。对MCI 诊断及早期干预有助于早期诊治AD,从而延缓其发展,改善MCI老人的生活质量。
目的
分析上海社区老人生活方式与轻度认知损害的关系,从生活方式中寻找老年轻度认知损害的防治措施。
方法
随机抽取1005 名上海社区老人,最终确诊的265 名MCI 和607 名正常老人作为研究对象,搜集这些老人的人口学、生活习惯等资料,进行单因素和多因素分析,寻找有统计学意义的指标。
结果
单因素分析发现吸烟(χ2= 10.808, p=0.001)、饮茶(χ2=11.74, p= 0.001)、有业余爱好(χ2= 20.815,p<0.001)、读书(χ2=28.670, p= 0.001)、上网(χ2=12.623,p= 0.001)、摄影(χ2=4.470, p= 0.034)为MCI 的保护性因素。多因素分析二项分类logistic 回归分析发现,吸烟、读书、上网有统计学意义,其OR 值分别为0.562(0.358-0.883)、0.428 (0.253-0.726)、0.238 (0.071-0.797)。即吸烟、读书、上网为MCI 的保护性因素。
结论
生活方式和MCI 的发病相关,良好的生活习惯及行为方式对预防MCI 有积极意义。
关键词: 轻度认知功能损害, 生活方式, 保护因素
1. Background
Mild cognitive impairment (MCI) refers in particular to memory or cognitive function decline, that does not meet the full diagnostic requirements for dementia. MCI is considered as a normal phase of physiological aging and can also transition into Alzheimer’s disease (AD).[1] Those with MCI are ten times more likely to develop Alzheimer’s disease (AD) than those in the general population.[2] MCI diagnosis and early intervention are helpful for the diagnosis and treatment of AD in its early stages, making it possible to push back the onset of AD and improve the quality of life for those with MCI. We explored the risk factors and protective factors for MCI from the vantage point of lifestyle.
2. Participants and methods
2.1 Participants
This study was based on the China’s national study on the evaluation, early recognition, and treatment of psychological problems in the elderly.[3] The subjects of this study selected were elderly people that had household registration in four representative communities in Shanghai (including Pudong New Area, Huangpu district, Changning district, and Baoshan district) in 2011. There were 4530 elderly individuals with an age of 60 years or older. SPSS statistical software was used to select 2720 elderly people by a random sampling method. Among them, 1302 people agreed to participate and provided written informed consent. Of the 1302 persons selected, 1005 people completed the survey. There were 4 psychological evaluators who assessed the cognitive function of all study subjects and collected demographic and lifestyle data. A training and comprehensive exam on the training was conducted before the study began. Evaluator consistency was assessed after the training. The intraclass correlation coefficient (ICC) was above 0.9 in all the tests of consistency, indicating good consistency. All subjects were diagnosed by 3 psychiatrists that had the rank of associate chief physician or above. In the end, a confirmed diagnosis was given to 607 normal elderly people and 265 elderly people with MCI. The study was approved by the ethics committee of the Shanghai Mental Health Center affiliated to the Shanghai Jiao Tong University.
Inclusion criteria:
The MCI group: met the MCI diagnostic criteria developed by the Petersen study group
the patient is conscious of his or her loss of memory or someone with intimate knowledge of the patient thinks the patient has a memory disorder;
the overall cognitive function is normal;
objective examination of memory impairment or an impairment of other cognitive functions. The memory or cognitive function scores were lower than the mean score of those of the same age and education attainment by 1.5 to 2 standard deviations;
the score of the clinical dementia rating scale was 0.5;
patient maintains normal daily activities;
does not meet the diagnostic criteria for dementia.
Normal control group
age ≥60, both genders;
normal cognitive functions;
not having other severe somatic diseases;
being able to cooperate and complete relevant exams.
Exclusion criteria:
excluding Alzheimer’s diseases and other forms of dementia;
excluding other cognitive impairments caused by neurodegenerative diseases, brain trauma, epilepsy, tumours, or infection;
excluding cognitive impairments caused by endocrine and metabolic diseases; excluding cognitive impairments due to severe cardiovascular, hepatic, lung, renal, and hematopoietic diseases; excluding cognitive impairments due to alcohol, smoking, and psychoactive drugs; other cognitive impairments or dementia caused by physical and chemical factors;
excluding those who are not able to complete the exam due to vision or hearing impairments.
2.2 Assessment tools
We used the consolidated assessment sheets, which included general information, neuropsychological tests and scale assessments, physician assessments, laboratory examinations, and imaging examinations. General information contained lifestyle and demographic data such as gender, age, educational attainment, and occupation. Lifestyle mainly consisted of smoking, drinking history, tea drinking history, exercise, hobbies, reading, listening to music, painting, calligraphy, chess and cards, surfing the internet, fishing, and practicing Taiji. Neuropsychological test and scale evaluation comprised the Mini-mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), Neuropsychological Test Battery (NTB), Self-Rating Anxiety Scale (SAS), Geriatric Depression Scale (GDS), Life Event Scale (LES), and Social Support Rating Scale (SSRS). The sections for physicians to evaluate included the current medical history, past medical history, physical examination, and clinical scale evaluation. The clinical scale evaluation comprised The Neuropsychiatric Inventory (NPI), Activity of Daily Living Scale (ADL), Global Deterioration Scale (GDS), Clinical Dementia Rating (CDR), and Clinical Global Impression (CGI). The laboratory tests included blood routine test, blood biochemical, vitamin B12, folic acid, thyroid function, blood viscosity, and serum syphilis screening results. The imaging examination method was mainly brain magnetic resonance imaging.
2.3 Statistical methods
SPSS 20.0 statistical software was used for data processing. The chi-square test was used to compare the numeration data. T-test was used to compare measurement data. Logistic regression analysis was used for multivariate analysis, in which a difference of p<0.05 was considered statistically significant.
3. Results
3.1 Demographic data of the study subjects in 2 groups
The average age of the MCI group was older than the normal control group; the female ratio was higher than the normal control group; the years of education was lower than the normal control group. The difference of age, gender, and years of education between two groups had statistical significance, age (t= -11.352, p< 0.001), gender (χ2= 25.072, p< 0.001), years of education (t= 10.430, p< 0.001). See table 1.
Table 1.
Comparison of the general data between the non-MCI elders and patients with MCI
| Group | Control group | MCI group | χ2 or t | p |
|---|---|---|---|---|
| Age (years) | 70.10 (7.555) | 76.46 (7.734) | -11.352 | <0.001 |
| Gender (male/ female) | 294/ 313 | 80/ 185 | 25.072 | <0.001 |
| Years of education (years) | 8.95 (4.281) | 5.22 (4.775) | 10.430 | <0.001 |
3.2 The univariate analysis of the relationship between the elderly people’s lifestyle and mild cognitive impairment
Smoking (χ2= 10.808, p= 0.001), tea drinking (χ2=11.747, p=0.001), having hobbies (χ2= 20.815, p< 0.001), reading (χ2= 28.670, p< 0.001), surfing on the internet (χ2= 12.623, p< 0.001), and photography (χ2= 4.470, p= 0.034) were protective factors for MCI. See table 2.
Table 2.
Univariate analysis of lifestyle related factors
| Factors | Control group | MCI group | χ2 | p |
|---|---|---|---|---|
| Smoking | 166 (27.3%) | 45 (17.0%) | 10.808 | 0.001* |
| Alcohol drinking | 109 (18.0°%) | 38 (14.3%) | 1.722 | 0.189 |
| Tea drinking | 253 (47.1%) | 78(29.4%) | 11.747 | 0.001* |
| Exercise | 375 (61.8°%) | 147 (55.5%) | 3.054 | 0.081 |
| Hobbies | 317 (54.5°%) | 94 (37.7%) | 20.815 | 0.000* |
| Reading | 157 (25.9°%) | 26 (9.8%) | 28.670 | 0.000* |
| Listening to music | 113 (18.6%) | 39 (14.7%) | 1.949 | 0.163 |
| Calligraphy | 22 (3.8%) | 4 (1.5%) | 2.852 | 0.091 |
| Chess and cards | 86 (14.2%) | 33 (12.5%) | 0.461 | 0.497 |
| Surfing on the internet | 42 (6.9%) | 3 (1.1%) | 12.623 | 0.000* |
| Photography | 30 (4.9%) | 5 (1.9%) | 4.470 | 0.034* |
| Fishing | 10 (1.6%) | 5 (1.9%) | 0.063 | 0.083 |
| Taiji | 47 (7.7%) | 20 (7.5%) | 0.010 | 0.920 |
3.3 The multivariate analysis of the relationship between the elderly people’s lifestyle and mild cognitive impairment
Binary logistic regression was conducted for the study participants of both groups. The dependent variables were the elderly people with a diagnosis of MCI and non-MCI elders. All the study factors in table 2 were independent variables. From the results, the variables smoking, reading, and surfing the internet had statistical significance at the 0.05 level. The OR values were 0.562 (0.358-0.883), 0.428 (0.253-0.726), and 0.238 (0.071-0.797) respectively. Hence, smoking, reading, and surfing the Internet were protective factors for MCI. See table 3.
Table 3.
Multivariate analysis of lifestyle related factors
| Factors | Parameter estimation | Standard error | Wald χ2 | p | OR | 95% confidence interval |
|---|---|---|---|---|---|---|
| Smoking | -0.576 | 0.230 | 6.264 | 0.012* | 0.562 | 0.358-0.883 |
| Reading | -0.848 | 0.269 | 9.907 | 0.002* | 0.428 | 0.253-0.726 |
| Surfing the internet | -1.438 | 0.618 | 5.415 | 0.020* | 0.238 | 0.071-0.797 |
4. Discussion
4.1 Main findings
Dementia is one of the major diseases that threatens the health of the elderly. China has a large population and a large base of patients with dementia. Currently, there are over 7 million persons with Alzheimer’s in China, accounting for approximately 1/4 of all cases in the world. Annually, the number of people who develop Alzheimer’s in China is about 300,000. The prevention and treatment of dementia is directly related to our national economy and people’s livelihood.[4] The vast majority of neurodegenerative and vascular dementia are irreversible. The existing treatment methods are far from meeting the goal of delaying or stabilizing the disease. How to prevent dementia has attracted much attention among researchers. MCI is the transition phase of cognitive decline and dementia induced by normal aging. The diagnosis and intervention of MCI can facilitate early diagnosis and treatment of dementia, thus delaying its development and improving the quality of life in patients with MCI. However some of the high risk factors such as gender, age and educational attainment cannot be changed. However, we can change other factors such as lifestyle and diet.
This study showed that the average age of the MCI group was older than the control group. The number of MCI cases increased with age and the difference was statistically significant. It is consistent with the general rule that cognitive function declines with age. The education attainment of the MCI group was lower than the control group, which is also consistent with past studies. A meta-analysis of 19 studies by Caamano-Isorna and colleagues[5] found that the risk of dementia was negatively associated with education attainment. This indicates that high education attainment is a protective factor for cognitive functioning. Some studies have shown that this may be associated with less cortical synapses due to low educational attainment. There is a significant gender difference with the MCI group in this study with females more than males. Some epidemiological studies show that the prevalence of AD among women is significantly higher than that of men.[6,7,8] The incidence of AD in postmenopausal women is higher than men of the same age group. The reason is related to the decrease of estrogen levels in postmenopausal women.[5]
This study has found that smoking, tea drinking, having some hobbies such as reading, surfing the internet, and photography are protective factors for MCI. The impact of smoking on cognitive function is still controversial. Some reports suggest that smoking may reduce cognitive function or increase the risk of Alzheimer’s disease.[9] However, nicotine has been proven to be able to improve cognition and emotion under certain conditions.[10] In terms of its independent effect, smoking has a protective effect on AD and the mechanism may be related to nicotine having a proposed anti-aging effect. Nevertheless, most studies suggest that smoking increases the risk of cardiovascular disease, thereby increasing the risk of AD.[11] In addition, other studies[12] showed that the protective effect of smoking depends on the dosage and time of smoking. The protective effect is more apparent when the person has had a smoking duration of 40 to 49 years or 200 to 299 packs of cigarette per year. However, this protective effect is gone when the smoking duration is over 60 years or the amount of smoking is more than 400 packs per year. Hence, only a moderate dosage of smoking has a protective effect on the decline of cognitive function. For a large number of smokers, the risk of other diseases and mortality may increase by merging with other smoking related diseases. Moreover, some other studies[13] have reported a positive correlation between smoking and cognitive impairment in middle-aged people. Yet this correlation wanes as the age increases. The amount and duration of smoking were not further analyzed in this study. All in all, the effect of smoking on cognition remains to be further studied.
The results of this study show that reading and surfing the internet are protective factors for cognitive function, which is consistent with the previous studies.[14] In epidemiological studies,[15] having a regular lifestyle, proper intensity of mental activity, maintaining curiosity about new things, high education, wide social relationship, and a reasonable diet can help reduce the risk of AD. Strengthening brain function exercises can help maintain or increase memory function. Some scholars[6] have reported that strengthening physical exercises of the left half of the body can help improve the role of the right hemisphere (memory increase), and finger movement exercises provide positive stimulation to the brain. Frequent use of the brain and hands, persistent study, and maintaining sharp insight and analytical ability can prevent mental deterioration. The protective mechanism of intellectual activities on cognitive function may that intellectual activities strengthen the synaptic function and slow brain atrophy so as to delay the occurrence of cognitive impairment.[16]
4.2 Limitations
This study investigated only 4 communities in Shanghai, which can only represent the elderly in these Shanghai communities. As a result, extrapolation has some limitations. Furthermore, the study was a cross-sectional study and there was no further follow-up.
4.3 Implications
We found that lifestyle was associated with the onset of MCI. In addition to smoking, good lifestyle and behaviors may have positive significance to MCI prevention. Active intervention on lifestyle can reduce the risk of MCI to some extent. Lifestyle interventions that are easy to implement may have the most significance towards the prevention of neurodegenerative diseases.
Figure 1.
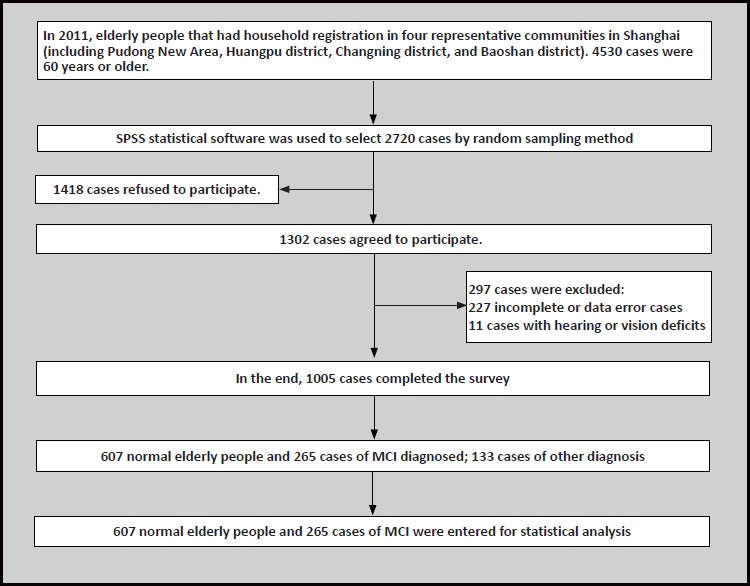
Flowchart of the study
Biography

Ning Su graduated from Shanghai Jiaotong University School of Medicine with a master’s degree in 2011. She has been working in the Shanghai Mental Health Center from August 2011 till now. Currently she works as a resident doctor in the geriatrics department. Her research of interest is geriatric psychiatry.
Footnotes
Funding statement
The National Key Technology Research and Development Program (project code: 2009BA177803).
Conflict of interest statement
The authors declare no conflict of interest related to this manuscript.
Informed consent
All the participants in this study provided written informed consent.
Ethical approval
This study was approved by the ethics committee of the Shanghai Mental Health Center affiliated to Shanghai Jiao Tong University.
Authors’ contributions
Ning Su was responsible for doing cognitive function assessment on some of the subjects, collecting data of demography and lifestyle, data statistics, and writing and modifying this article. Wei Li was responsible for doing cognitive function assessment on some of the subjects, collecting data of demography and lifestyle, and providing valuable advice on the statistics in this paper. Xia Li, Tao Wang, and Minjie Zhu were responsible for the diagnosis of the subjects. Yuanyuan Liu and Yan Shi were responsible for doing cognitive function assessment on some of the subjects and collecting data of demography and lifestyle. Shifu Xiao was the head of the project and cor-respondence author.
References
- 1.Ma YX, Yu ZW, Hong Z, Bai CX, Chen SD, Xiao SF, et al. [New Progress in Aging, Dementia, and Preventive Medicine]. Beijing: Science and Technology Literature Press; 2013. p: 581-586. Chinese [Google Scholar]
- 2.Chui DH, Tian XS, Wang HC, Wang W, Xiao WZ, Fan DS. The Relationship Between Brain Aging and Preclinical Alzheimer’s Disease. Prog Biochem Biophys. 2012; 39(8): 741-746. doi: http://dx.doi.org/10.3724/SPJ.1206.2012.00351 [Google Scholar]
- 3.Xiao S, Li J, Tang M, Chen W, Bao F, Wang H, et al. Methodology of China’s national study on the evaluation, early recognition, and treatment of psychological problems in the elderly: the China Longitudinal Aging Study. Shanghai Arch Psychiatry. 2013; 25: 91-97. doi: http://dx.doi.org/10.3969/j.issn.1002-0829.2013.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jia JP, Wang MH, Zhang CD, Ding XS, Zhang ZX, Zhang XJ, et al. [Guideline for diagnosis and treatment of dementia and cognitive impairment in China (1): diagnosis process of dementia]. Zhong Hua Yi Xue Za Zhi. 2011; 9: 577-581. Chinese. doi: http://dx.chinadoi.cn/10.3760/cma.j.issn.0376-2491.2011.09.001 [PubMed] [Google Scholar]
- 5.Ma YX, Yu ZW, Hong Z, Bai CX, Chen SD, Xiao SF, et al. [New Progress in Aging, Dementia, and Preventive Medicine]. Beijing: Science and Technology Literature Press; 2013. p: 30-40. Chinese [Google Scholar]
- 6.Jiang KD, Yu X, Li LJ, Wang GH. [Psychiatry]. Beijing: People’s Medical Publishing House; 2010. p: 69-73. Chinese [Google Scholar]
- 7.Matsui Y, Tanizaki Y, Arima H, Yonemoto K, Doi Y, Ninomiya T, et al. Incidence and survival of dementia in a general population of Japanese elderly: the Hisayama Study. J Neurol Neuro-SurgPsy. 2009; 80(4): 366-370. doi: http://dx.doi.org/10.1136/jnnp.2008.155481 [DOI] [PubMed] [Google Scholar]
- 8.Heun R, Kölsch H, Jessen F. Risk factors and early signs of Alzheimer’s disease in a family study sample. Eur Arch Psychiatry ClinNeurosci. 2006; 256(1): 28-36. doi: http://dx.doi.org/10.1007/s00406-005-0596-4 [DOI] [PubMed] [Google Scholar]
- 9.Deng J, Wang YJ, Zhang M, Yan JC, Yi X, Zhou DH. [The effect of cigarette smoking on cognitive function and pathological changes of hippocampal neurons in Alzheimer’s disease rats]. Zhong Hua Lao Nian Xin Nao Xue Guan Bing Za Zhi. 2011; 1(13): 72-74. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1009-0126.2011.01.024 [Google Scholar]
- 10.Besson M, Forget B. Cognitive Dysfunction, Affective States, and Vulnerability to Nicotine Addiction: A Multifactorial Perspective. Front Psychiatry. 2016; 21(7): 160. doi: http://dx.doi.org/10.3389/fpsyt.2016.00160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang QH, Zhang ZX, Tang MN, Hong Z, Qu QM, Jiang XZ, et al. [Smoking, alcohol and tea drinking on Alzheimer’s disease]. Zhong Hua Shen Jing Ke Za Zhi. 2004; 3: 4549. Chinese. doi: http://dx.chinadoi.cn/10.3760/j.issn:1006-7876.2004.03.013 [Google Scholar]
- 12.Liu XH, Meng C, Tang Z, Chen B. [The research of influence with smoking on cognitive function in elderly - “Multidimensional longitudinal study on aging in Beijing” baseline survey analysis]. Zhongguo Lao Nian Xue Za Zhi. 2002; 22(3): 163-165. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1005-9202.2002.03.002 [Google Scholar]
- 13.Liu J, Shang S, Li P, Deng M, Chen C, Jiang Y, et al. Association between current smoking and cognitive impairment depends on age: A cross-sectional study in Xi’an, China. Med Clin (Barc). 2017; doi: http://dx.doi.org/10.1016/j.medcli.2017.02.033 [DOI] [PubMed] [Google Scholar]
- 14.Dong L, Xiao R, Cai C, Xu Z, Wang S, Pan L, Yuan L, et al. Diet, lifestyle and cognitive function in old Chinese adults. Arch Gerontol Geriatr. 2016; 63: 36-42. doi: http://dx.doi.org/10.1016/j.archger.2015.12.003 [DOI] [PubMed] [Google Scholar]
- 15.Scarmeas N, Luchsinger JA, Schupf N, Brickman AM, Cosentino S, Tang MX, et al. Physical activity, diet, and risk of Alzheimer disease. JAMA. 2009; 302(6): 627-637. doi: http://dx.doi.org/10.1001/jama.2009.1144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karp A, Andel R, Parker MG, Wang HX, Winblad B, Fratiglioni L. Mentally stimulating activities at work during midlife and dementia risk after age 75: follow-up study from the Kungsholmen Project. Am J Geriatr Psychiatry. 2009; 17(3): 227-236. doi: http://dx.doi.org/10.1097/JGP.0b013e318190b691 [DOI] [PubMed] [Google Scholar]


