Abstract
Introduction
The radial and posterior interosseous nerves (PIN) are prone to injury at multiple sites. Electrodiagnostic (EDX) studies may only identify the most proximal lesion. Nerve ultrasound could augment electrodiagnosis by visualizing additional pathology.
Methods
Retrospective examination of ultrasound and electrodiagnosis from 26 patients evaluated for posterior cord/radial/PIN lesions.
Results
Eighteen of 26 patients had abnormalities on electrodiagnosis (15 radial; 2 PIN; 1 posterior cord). Ultrasound identified 15 of 18 (83%) of the EDX abnormalities and provided additional diagnostic information. In 6 of 15 (40%) patients with EDX evidence of radial neuropathy, ultrasound identified both radial nerve enlargement and additional, unsuspected PIN enlargement (53% to 339% enlarged vs. unaffected side). Ultrasound also identified: nerve (dis)continuity at the trauma site (n=8); and nerve tumor (n=2; 1 with normal EDX).
Conclusion
In radial neuropathy, ultrasound often augments EDX studies and identifies a second lesion in the PIN. Further studies are required to determine the etiology and significance of this additional distal pathology.
Keywords: Ultrasound, radial nerve, posterior interosseous nerve, double crush syndrome, neuropathy
Introduction
Injuries to the radial nerve and its distal motor branch, the posterior interosseous nerve (PIN), are relatively common and can occur at multiple sites along the course in the arm1,2. Lesion localization is typically based on the pattern of clinical and electrodiagnostic findings. PIN neuropathy is distinguished from the more proximal radial neuropathy by sparing of sensation and sparing of strength in the triceps brachii and brachioradialis muscles. In patients with wrist and finger drop, lesion localization is clinically relevant and affects outcomes3. Definitive lesion localization may not always be possible with clinical and electrodiagnostic (EDX) examinations. As the radial and PIN encounter multiple potential entrapment sites along their course, it is possible that patients with radial neuropathy have a superimposed PIN lesion that is undetected, especially following trauma4. Dual lesions have been reported rarely, often following trauma but to our knowledge have not been systematically evaluated in the radial and PINs 5-8. This may be because neither clinical nor EDX findings can clearly identify a superimposed PIN lesion in patients with a more proximal radial neuropathy.
Nerve ultrasound is a non-invasive and painless diagnostic modality that can readily identify abnormalities in both the radial and PIN 9-13 and can identify multiple pathologies in a single nerve distribution14,15. Nerve pathology identified using ultrasound includes nerve enlargement, change in nerve caliber, and alterations in nerve echogenicity and vascularity. Ultrasound is complementary to electrodiagnosis for evaluating poly- and mononeuropathy and provides additional information that influences clinical management16-20. Imaging nerves with ultrasound or magnetic resonance imaging (MRI) can provide data on the etiology of a neuropathy, such as laceration, tumor, or compression, and they can also reveal pathology disparate from the location suspected based on clinical exam and EDX studies. For instance, in patients with anterior interosseous nerve syndrome, MRI showed nerve pathology in select motor fascicles of the proximal median nerve rather than the anterior interosseous nerve 21. In this study, we describe how ultrasound augments electrodiagnosis in the evaluation of patients with radial and/or PIN neuropathy and highlight examples of patients with abnormalities in both the radial and PIN.
Methods
This study was approved by our institutional review board. We identified and reviewed medical records of 53 patients referred for nerve ultrasound with concern for unilateral radial and/or posterior interosseous neuropathy from 1/2009 to 9/2014. We excluded 27 patients who did not undergo EDX studies and/or sonographic evaluation of both the radial and PIN (n=15), or who had prior surgery (i.e. nerve decompression/transfer) directly involving the radial or PIN (n=7), inflammatory polyneuropathies (n=3), or radiculoplexopathy (n=1), and 1 who had EDX evaluation 85 days prior to the ultrasound. Of the 26 patients included, EDX was performed on the same day as the ultrasound in 22 and within 35 days in 4. All patients were evaluated in our neuromuscular electrodiagnostic laboratory. In 1 patient, we also reviewed the nerve conduction studies performed at the University of North Carolina 2 months prior to the studies performed at our institution. We also reviewed the clinical examinations performed by the referring/consulting physicians, and noted the presence and pattern of weakness.
Nerve ultrasound was performed by CMZ using a Philips iu22 machine with an L12-5 or L15-7 probe. The radial nerve was visualized in the arm and forearm through its division into the posterior interosseous nerve. The posterior interosseous nerve was visualized from its division from the superficial radial sensory nerve to the crossing of the distal margin of the supinator muscle. Results of the ultrasound examination were characterized based on the reported final conclusion of the sonographer (CMZ) in the medical record. We identified abnormalities such as enlargement, tumor, displacement, impingement, or laceration in these nerves qualitatively. We often also performed measurements of nerve cross sectional area, but due to the oblique course of the normal radial nerve and the very small and often separated fascicles of the normal appearing PIN we did not rely on quantitative values to define abnormalities. In the symptomatic arm, we measured the cross sectional area (CSA) of the radial nerve in all and the PIN in 13 of 26 patients. For comparison, in the contralateral, unaffected arm we measured the CSA of the radial nerve in11 of 26 (median 4.4 mm2, range 3.4 mm2 - 6.1 mm2) and the PIN in 9 of 26 (median 1.8 mm2, range 1.2 mm2 - 2.3 mm2) patients. Ultrasound abnormalities included nerve enlargement with caliber change at the lesion site, evidence of nerve trauma (laceration, displacement, or impingement from fracture, gunshot wound), or nerve tumor. Abnormalities were classified as involving the common radial nerve, posterior interosseous nerve, or both. For clarity, the deep motor branch of the radial nerve, identified from its division from the common radial nerve and proximal to the supinator muscle, was classified as the posterior interosseous nerve.
Electrodiagnostic testing was performed in our laboratory by neuromuscular specialists (all certified by the American Board of Electrodiagnostic Medicine) using standard techniques. All patients had radial motor and superficial radial nerve sensory nerve conduction studies recorded from the extensor indicis and anatomic snuffbox, respectively, as well as needle EMG of muscles innervated by the radial nerve and PIN. Conduction block was defined as >50% decrease in the proximal relative to the distal compound motor action potential (CMAP) amplitude. Electrodiagnostic abnormalities were localized based on neuroanatomic criteria22 as follows: 1) Posterior interosseous neuropathy (includes lesions within and distal to the deep motor branch of the radial nerve), defined as active and/or chronic denervation of the muscles innervated by the PIN (i.e.: extensor indicis, extensor digitorum, or extensor carpi ulnaris) with sparing of muscles innervated by the more proximal branches of the radial nerve (i.e. brachioradialis, supinator, and triceps brachii), sparing of the radial sensory nerve action potential (SNAP), and/or conduction block localized to the forearm segment; 2) Radial neuropathy, defined as active and/or chronic denervation of muscles innervated by the radial nerve proximal to the deep motor branch/PIN (i.e. brachioradialis), an abnormal radial SNAP, or conduction block in the arm; 3) Posterior cord plexopathy, defined as denervation of the most proximal muscles innervated by the radial nerve (i.e. triceps brachii) and additional denervation of the deltoid and/or latissimus dorsi.
We classified a patient as normal if both ultrasound and electrodiagnosis were normal and as abnormal (neuropathy) if either was abnormal. Examiners were not blinded to clinical features or the results of the ultrasound or electrodiagnosis. We categorized the etiology of neuropathy based on the clinical history.
Results
The 26 patients (15 men) were age 17-79 years. Seven had both normal ultrasound and electrodiagnosis, and 19 had a neuropathy. Neuropathies (Table 1) were due to trauma (n=8), idiopathic (n=5), compression related to position during sleep or surgery (n=4), or tumor (n=2).
Table 1. Etiology and Findings of Electrodiagnosis and Nerve Ultrasound in Patients with Radial or Posterior Interosseous Neuropathy.
| Patient # | Etiology | EDX Result | NUS Result |
|---|---|---|---|
| 1 | Idiopathic | RN | RN + PIN |
| 2 | Humerus Fracture | RN | RN + PIN |
| 3 | Humerus Fracture | RN | RN + PIN |
| 4 | Gunshot Wound | RN | RN + PIN |
| 5 | Sleep Compression | RN | RN + PIN |
| 6 | Idiopathic | RN | RN + PIN |
| 7 | Humerus Fracture | RN | RN |
| 8 | Gunshot Wound | RN | RN |
| 9 | Gunshot Wound | RN | RN |
| 10 | Post- Surgery | RN | RN |
| 11 | Tumor | RN | RN |
| 12 | Idiopathic | RN | RN |
| 13 | Idiopathic | RN | RN |
| 14 | Idiopathic | RN | Normal |
| 15 | Sleep Compression | RN | Normal |
| 16 | Elbow Fracture | PIN | PIN |
| 17 | Idiopathic | PIN | PIN |
| 18 | Humerus Fracture | Posterior cord | RN |
| 19 | Tumor | Normal | RN |
Legend: EDx: electrodiagnosis; NUS: nerve ultrasound; RN: radial neuropathy; PIN: posterior interosseous neuropathy. Patients #1-6, in bold, had both radial and posterior interosseous neuropathy identified with nerve ultrasound.
Eighteen had abnormal electrodiagnosis: 15, radial neuropathy; 2, posterior interosseous neuropathy; and 1 posterior cord brachial plexopathy (Table 1, electrodiagnostic details in Supplementary Table S1, available online). All (n=18) had fibrillation potentials or positive sharp waves and reduced recruitment in 1 or more muscles innervated by the radial and/or posterior interosseous nerves. Other electrodiagnostic abnormalities included: conduction block above the elbow (n=3) or in the forearm (n=1), a small or absent radial CMAP from the extensor indicis (n=15), and a small or absent radial SNAP (n=12).
Seventeen had abnormal ultrasound: 9 had radial neuropathy, 2 had posterior interosseous neuropathy, and 6 had both radial and posterior interosseous neuropathy (Table 1). Ultrasound abnormalities in the radial nerve were nerve enlargement with caliber change (n=10), transection (n=2), tumor (n=2), and displacement by surgical hardware with caliber change (n=1). Ultrasound abnormalities in the PIN were nerve enlargement with caliber change in all (n=8). Enlarged radial nerves had a median (range) CSA of 11.8 mm2 (6.1 mm2 – 35.1 mm2). All enlarged radial nerves were either 44% - 176% larger than the unaffected side (n=7) or had CSA > 12 mm2 (n=3). Enlarged PINs had a median (range) CSA of 5.1 mm2 (2.9 mm2 -7.9 mm2) and, in 7, were 53-392% larger than the unaffected side. One very enlarged PIN (CSA 7.5 mm2) was not compared to the unaffected arm. Ultrasound confirmed the electrodiagnostic abnormality in 15 of 18 (83%) patients (Table 2): 13 with radial neuropathy and 2 with posterior interosseous neuropathy.
Table 2. Location of Neuropathy Based on Nerve Ultrasound vs. Electrodiagnosis.
| Electrodiagnosis | Total (based on NUS) | |||||
|---|---|---|---|---|---|---|
| Nerve Ultrasound | Lesion Location | Posterior Cord | Radial | PIN | None | |
| Radial only | 1 | 7 | 0 | 1 | 9 | |
| Radial + PIN | 0 | 6 | 0 | 0 | 6 | |
| PIN only | 0 | 0 | 2 | 0 | 2 | |
| None | 0 | 2 | 0 | 7 | 9 | |
| Total (based on EDX) | 1 | 15 | 2 | 8 | N=26 | |
NUS: nerve ultrasound, EDX: electrodiagnosis, PIN: posterior interosseous nerve
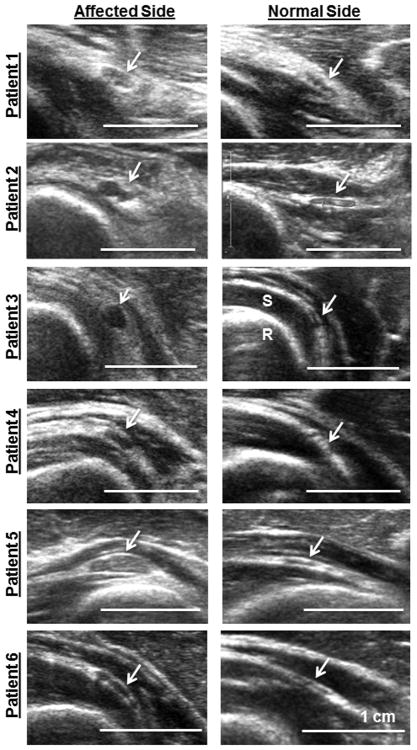
Ultrasound often added additional information to the electrodiagnosis. In 6 of 15 (40%) patients with electrodiagnostic evidence of a radial neuropathy in the arm (patients #1-6, Table 1 and Figure 1), ultrasound identified enlargement of both the radial nerve in the arm (CSA 8.6 mm2 -12.0 mm2, all >44% larger than the contralateral side) and additional, distinct enlargement of the PIN within the body of the supinator muscle (CSA 2.9 -7.9mm2, all >53% larger than the contralateral side, Figure 1). Ultrasound clarified or augmented electrodiagnosis in an additional 10 patients. Two had nerve tumors identified with ultrasound (1 with normal electrodiagnosis). Eight had traumatic neuropathies with no (n=7) or single (n=1) motor unit potentials in the finger extensor muscles; ultrasound identified nerve continuity in 6 and transection in 2.
Figure 1.
Ultrasound images of the enlarged posterior interosseous nerve (arrows, left panels) compared to the normal, contralateral side (arrows, right panels) in 6 patients with electrodiagnostic evidence of a radial neuropathy. The radius (R) appears as bright and rounded deep to the supinator (S). White bar = 1 cm.
The 6 patients (#1-6) with radial neuropathy and PIN enlargement had clinical findings consistent with radial neuropathy and similar electrodiagnosis to those without PIN enlargement (Table 1). None had nerve transection or direct trauma to the PIN. Of these 6 patients, 3 had trauma to the arm proximal to the elbow [2 humerus fractures (patients #2 and #3) and 1 gunshot wound (patient #4)], 2 had idiopathic onset (patients #1 and #6), and 1 had compression during sleep (patient #5). None of these patients had diabetes mellitus. Patients #1-5 had weakness in the brachioradialis. Patients #2-6 had abnormal sensation in the superficial radial nerve distribution. Following ultrasound and electrodiagnosis, 3 (patients #1, #3, and #6) had surgical release of the PIN and 1 (#1) of the radial nerve; all had nerve constriction identified intraoperatively.
Ten patients with electrodiagnosis of radial neuropathy had clinical follow up of brachioradialis and wrist/finger extensor strength 1 month – 6 years after the ultrasound examination. Five had PIN enlargement, and 5 did not. At last follow up, all 5 patients (#1, #3, #4, #5, and #6) with radial neuropathy and PIN enlargement, but only 2 of 5 patients (#9 and #10) with radial neuropathy without PIN enlargement had weakness preferentially affecting muscles innervated by the PIN compared to the proximal radial nerve braches. One (#9) suffered a gunshot wound to the elbow just proximal to the takeoff of the PIN. Patients #2, 12, 13, 14, and 15 were lost to follow up or had insufficient examinations recorded.
Electrodiagnosis and ultrasound differed in 4 patients. One (patient #18) had electrodiagnosis of a posterior cord lesion and also had conduction block in the forearm/PIN following a displaced humerus fracture with internal fixation; ultrasound showed a normal PIN and an abnormal appearing radial nerve displaced by surgical screws in the distal arm. Two patients (#14 and #15) had electrodiagnosis of radial neuropathy at the spiral groove with conduction block (1 idiopathic, 1 Saturday night palsy) but had normal ultrasound. One patient (#19) had a radial nerve tumor identified on ultrasound but had normal electrodiagnosis.
Discussion
Nerve ultrasound identified dual, distinct pathologies in the radial and posterior interosseous nerves that were not suspected based on the primary mechanism of injury or electrodiagnostic results. This is similar to a previous case report of dual injuries in the radial and PIN following trauma4. In our patients with radial neuropathy, the etiology of the additional nerve enlargement in the PIN is unknown. Possible etiologies of PIN injury in patients with radial neuropathy could be: 1) mechanical (i.e.: strain or stretch) injury secondary to trauma to the proximal radial nerve; 2) the denervated PIN may be predisposed to a second, compressive injury, as hypothesized in “double crush syndrome” 23,24; or 3) mechanical alterations in the denervated supinator muscle could lead to compression. Axon loss could also cause mild enlargement in the PIN, but it is unlikely to cause the marked enlargement noted in most of our patients25.
Routinely imaging nerves as part of the diagnostic evaluation could improve identification of nerve pathologies not suspected based on the clinical exam or electrodiagnosis. The significance of these unsuspected alterations in nerve morphology is unknown. All patients in this study with ultrasound identified pathologies in both the PIN and radial nerve, and some patients without enlargement of the PIN, had weakness preferentially affecting the PIN innervated muscles at last follow up. Additional studies comparing clinical examination to electrodiagnostic and ultrasound results are required to determine how nerve imaging informs prognosis and impacts management.
Ultrasound often augmented electrodiagnosis in patients with radial or PIN lesions. Ultrasound confirmed the abnormal electrodiagnosis in most (83%) patients and added additional diagnostic information, such as visualizing unsuspected PIN enlargement, nerve continuity or laceration in trauma, or nerve tumors. In all, ultrasound augmented electrodiagnosis in 16 of 19 (84%) patients. The additional value of ultrasound to electrodiagnosis found in this study is similar to a previous study which found that ultrasound modified the diagnostic and therapeutic path in 42% of patients and played a confirmatory role in another 40%16. Similar to this prior study, our findings emphasize how ultrasound is especially valuable in nerve trauma, as it can evaluate nerve continuity and describe the precise location of nerve injury 17,18,26,27.
This study has several limitations. We performed a retrospective evaluation, which limited our ability to systematically define the patients' signs and symptoms. Neither the ultrasonographer nor the electrophysiologists were blinded to clinical or diagnostic information, which could inflate the rate of concordance between ultrasound and electrodiagnosis. We also therefore could not determine the sensitivity or specificity of ultrasound or electrodiagnosis in radial or posterior interosseous neuropathy. Ultrasound in our study was performed by a single, experienced examiner, and results could differ at other institutions. Finally, all patients in our study had neuropathies with axon loss. Patients with less severe neuropathies may show different results.
In conclusion, ultrasound, as an addition to electrodiagnosis, improved the identification of superimposed PIN lesions in patients with proximal radial neuropathies. Forty percent of patients with radial neuropathy had abnormal PIN morphology identified with ultrasound. Further study is required to determine how the additional pathology identified with ultrasound in the PIN affects prognosis and management of the radial neuropathy.
Supplementary Material
Acknowledgments
The study was supported by the Washington University Neuromuscular Research Fund and National Institute of Health Neurological Sciences Academic Development Award Grant Number K12 NS00169009.
Abbreviations
- PIN
posterior interosseous nerve
- MRI
magnetic resonance imaging
- CSA
cross sectional area
- CMAP
compound motor action potential
- EDX
electrodiagnostic
- SNAP
sensory nerve action potential
References
- 1.Latinovic R, Gulliford MC, Hughes RA. Incidence of common compressive neuropathies in primary care. J Neurol Neurosurg Psychiatry. 2006;77:263–265. doi: 10.1136/jnnp.2005.066696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirici Y, Irmak MK. Investigation of two possible compression sites of the deep branch of the radial nerve and nerve supply of the extensor carpi radialis brevis muscle. Neurol Med Chir (Tokyo) 2004;44:14–18. doi: 10.2176/nmc.44.14. discussion 19. [DOI] [PubMed] [Google Scholar]
- 3.Pan CH, Chuang DC, Rodriguez-Lorenzo A. Outcomes of nerve reconstruction for radial nerve injuries based on the level of injury in 244 operative cases. J Hand Surg Eur Vol. 2010;35:385–391. doi: 10.1177/1753193409360283. [DOI] [PubMed] [Google Scholar]
- 4.Liotta G, Granata G, Librante A, di Pasquale A, Caliandro P, Martinoli C, Padua L. Atypical double nerve lesion after humeral fracture: diagnosis by ultrasound. Muscle Nerve. 2010;41:287–288. doi: 10.1002/mus.21580. [DOI] [PubMed] [Google Scholar]
- 5.Giannoudis PV, Da Costa AA, Raman R, Mohamed AK, Smith RM. Double-crush syndrome after acetabular fractures. A sign of poor prognosis. J Bone Joint Surg Br. 2005;87:401–407. doi: 10.1302/0301-620x.87b3.15253. [DOI] [PubMed] [Google Scholar]
- 6.Akyuz M, Yalcin E, Selcuk B, Onder B, Ozcakar L. Electromyography and ultrasonography in the diagnosis of a rare double-crush ulnar nerve injury. Arch Phys Med Rehabil. 2011;92:1914–1916. doi: 10.1016/j.apmr.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 7.Huang YG, Chang SM. Double crush syndrome due to plating of humeral shaft fracture. Indian J Orthop. 2014;48:223–225. doi: 10.4103/0019-5413.128774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bianchi ML, Padua L, Granata G, Erra C. Double site nerve lesion: ultrasound diagnosed musculocutaneous involvement in traumatic brachial plexus injury. Clin Neurophysiol. 2013;124:629–630. doi: 10.1016/j.clinph.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Nakashima Y, Sunagawa T, Shinomiya R, Ochi M. High-resolution ultrasonographic evaluation of “hourglass-like fascicular constriction” in peripheral nerves: a preliminary report. Ultrasound Med Biol. 2014;40:1718–1721. doi: 10.1016/j.ultrasmedbio.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Bodner G, Buchberger W, Schocke M, Bale R, Huber B, Harpf C, Gassner E, Jaschke W. Radial nerve palsy associated with humeral shaft fracture: evaluation with US--initial experience. Radiology. 2001;219:811–816. doi: 10.1148/radiology.219.3.r01jn09811. [DOI] [PubMed] [Google Scholar]
- 11.Choi SJ, Ahn JH, Ryu DS, Kang CH, Jung SM, Park MS, Shin DR. Ultrasonography for nerve compression syndromes of the upper extremity. Ultrasonography. 2015 doi: 10.14366/usg.14060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cartwright MS, Yoon JS, Lee KH, Deal N, Walker FO. Diagnostic ultrasound for traumatic radial neuropathy. Am J Phys Med Rehabil. 2011;90:342–343. doi: 10.1097/PHM.0b013e3181e29daa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martinoli C, Bianchi S, Pugliese F, Bacigalupo L, Gauglio C, Valle M, Derchi LE. Sonography of entrapment neuropathies in the upper limb (wrist excluded) J Clin Ultrasound. 2004;32:438–450. doi: 10.1002/jcu.20067. [DOI] [PubMed] [Google Scholar]
- 14.Liotta G, Librante A, Di Pasquale A, Granata G, Pazzaglia C, Caliandro P, Padua L. Multiple bilateral sciatic compressions due to cast in a patient with leg lengthening diagnosed through ultrasound. Clin Neurophysiol. 2011;122:2539–2540. doi: 10.1016/j.clinph.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 15.Zaidman CM, Seelig MJ, Baker JC, Mackinnon SE, Pestronk A. Detection of peripheral nerve pathology: comparison of ultrasound and MRI. Neurology. 2013;80:1634–1640. doi: 10.1212/WNL.0b013e3182904f3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Padua L, Liotta G, Di Pasquale A, Granata G, Pazzaglia C, Caliandro P, Martinoli C. Contribution of ultrasound in the assessment of nerve diseases. Eur J Neurol. 2012;19:47–54. doi: 10.1111/j.1468-1331.2011.03421.x. [DOI] [PubMed] [Google Scholar]
- 17.Cokluk C, Aydin K, Senel A. Presurgical ultrasound-assisted neuro-examination in the surgical repair of peripheral nerve injury. Minim Invasive Neurosurg. 2004;47:169–172. doi: 10.1055/s-2004-818486. [DOI] [PubMed] [Google Scholar]
- 18.Zhu J, Liu F, Li D, Shao J, Hu B. Preliminary study of the types of traumatic peripheral nerve injuries by ultrasound. Eur Radiol. 2011;21:1097–1101. doi: 10.1007/s00330-010-1992-3. [DOI] [PubMed] [Google Scholar]
- 19.Zaidman CM, Harms MB, Pestronk A. Ultrasound of inherited vs. acquired demyelinating polyneuropathies. J Neurol. 2013;260:3115–3121. doi: 10.1007/s00415-013-7123-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zaidman CM, Pestronk A. Nerve size in chronic inflammatory demyelinating neuropathy varies with disease activity and therapy response over time: a retrospective ultrasound study. Muscle Nerve. 2014;50:733–738. doi: 10.1002/mus.24227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pham M, Baumer P, Meinck HM, Schiefer J, Weiler M, Bendszus M, Kele H. Anterior interosseous nerve syndrome: fascicular motor lesions of median nerve trunk. Neurology. 2014;82:598–606. doi: 10.1212/WNL.0000000000000128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Preston DC, Shapiro BE. Electromyography and neuromuscular disorders : clinical-electrophysiologic correlations. xvii. London; New York: Elsevier Saunders; 2013. p. 643. [Google Scholar]
- 23.Upton AR, McComas AJ. The double crush in nerve entrapment syndromes. Lancet. 1973;2:359–362. doi: 10.1016/s0140-6736(73)93196-6. [DOI] [PubMed] [Google Scholar]
- 24.Molinari WJ, 3rd, Elfar JC. The double crush syndrome. J Hand Surg Am. 2013;38:799–801. doi: 10.1016/j.jhsa.2012.12.038. quiz 801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zaidman CM, Al-Lozi M, Pestronk A. Peripheral nerve size in normals and patients with polyneuropathy: an ultrasound study. Muscle Nerve. 2009;40:960–966. doi: 10.1002/mus.21431. [DOI] [PubMed] [Google Scholar]
- 26.Padua L, Di Pasquale A, Liotta G, Granata G, Pazzaglia C, Erra C, Briani C, Coraci D, De Franco P, Antonini G, Martinoli C. Ultrasound as a useful tool in the diagnosis and management of traumatic nerve lesions. Clin Neurophysiol. 2013;124:1237–1243. doi: 10.1016/j.clinph.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 27.Cartwright MS, Chloros GD, Walker FO, Wiesler ER, Campbell WW. Diagnostic ultrasound for nerve transection. Muscle Nerve. 2007;35:796–799. doi: 10.1002/mus.20761. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.