Abstract
Depressive symptoms are the most frequently treated psychiatric condition in the United States. Brief behavioral activation treatment for depression (BATD) is a popular, evidence-based psychotherapy with strong research support for the treatment of depression. In this paper, we describe the development and initial pilot feasibility testing of a BATD mobile application (Behavioral Apptivation) to be used by patients and therapists in conjunction with BATD therapy. We present information regarding the app development process as well as results from a small open-label feasibility trial of the app utilized in conjunction with individual BATD. We include a case series from the open-label trial highlighting how Behavioral Apptivation can be utilized in clinical practice.
Keywords: behavioral activation, depression, mHealth
Depressive symptoms are the most frequently treated psychiatric condition in the United States (Kessler, 2012). Regarding treatment for depressive symptomatology, brief behavioral activation treatment for depression (BATD; Lejuez, Hopko, Acierno, Daughters, & Pagoto, 2011; Lejuez, Hopko, LePage, Hopko, & McNeil, 2001) is a widely used, evidence-based treatment (Sturmey, 2009). BATD is based in behavioral principles of depression suggesting that depression is caused by a lack of reinforcement in the environment for positive, nondepressed behaviors. As such, the goal of BATD is to help the patient reengage in positive, nondepressed activities.
A considerable amount of literature speaks to both the efficacy and effectiveness of BATD for the treatment of depressive symptomatology and comorbid disorders. Across studies, BATD is associated with reductions in depressive symptoms among individuals with elevated depressive symptoms (Gawrysiak, Nicholas, & Hopko, 2009; Reynolds, MacPherson, Tull, Baruch, & Lejuez, 2011) as well as with major depressive disorder (Hopko, Lejuez, Lepage, Hopko, & McNeil, 2003). Moreover, BATD has been used efficaciously with depressed individuals with a range of other comorbidities including substance use (Daughters et al., 2008; MacPherson et al., 2010; Magidson et al., 2011), anxiety/trauma (Gros et al., 2012; Strachan, Gros, Ruggiero, Lejuez, & Acierno, 2012), and physical health conditions such as cancer (Hopko et al., 2011). BATD has been tested in a variety of patient populations including college students (Gawrysiak et al., 2009; Reynolds et al., 2011), veterans (Egede et al., 2015), Spanish-speaking Latinos (Collado, Calderon, MacPherson, & Lejuez, 2016; Collado, Castillo, Maero, Lejuez, & MacPherson, 2014; Collado, Long, MacPherson, & Lejuez, 2014), and survivors of systematic violence in Kurdistan, Iraq (Bolton et al., 2014). A key strength of BATD, which contributes to its popularity, is that it is simple, straightforward, and as such is easy for clinicians to be trained in and to use with their patients (e.g., Bolton et al., 2014). Contributing to the widespread utilization of BATD, behavioral activation has strong research support as an empirically supported treatment (Sturmey, 2009; www.div12.org) and has been selected as an evidence-based therapy by the UK National Institute for Health and Care Excellence (www.nice.org.uk).
In a traditional delivery of BATD, a therapist would guide the patient through the basic BATD components that include (a) treatment overview and rationale: introduction to the BATD model; (b) identification of life areas, values, and associated activities: identification of values and goals within a variety of life areas important to the patient, including relationships, education, career, recreation, and health; (c) daily monitoring and activity planning: selection of activities that allow the patient to live according to his or her values and incorporation of the activities into the patient’s daily schedule—at the end of each week, scheduling additional activities for the following week; and (d) contracts: identification of a supportive individual to facilitate completion of difficult activities (see Lejuez et al., 2011, for the full BATD treatment manual). Between sessions, patients complete daily monitoring forms on which they record their already occurring activities and their new, value-driven activities. The BATD manual is written for delivery across 8–10 sessions, although it can be delivered in as few as 5 sessions and can extend beyond 10 sessions depending on patient needs and the need to combine it with other therapeutic approaches (Cassar et al., 2016).
Although BATD is a simple, straightforward psychotherapy for depression, the traditional delivery of BATD is hampered by some practical issues for some patients, primarily associated with utilization of paper forms. In BATD, at every therapy session, the patient is provided with a week’s worth of daily monitoring forms to complete between sessions and is instructed to complete one monitoring form per day. As the treatment progresses, monitoring forms are used both to schedule in new value-driven activities as well as to monitor already occurring activities. This reliance on paper forms may make it difficult for some patients to complete between-session exercises and may similarly make it difficult for some therapists to draw associations between completed activities and mood. Addressing limitations associated with utilization of paper forms has the potential to improve treatment efficiency and efficacy.
A growing literature base suggests that mobile applications (apps) may be useful adjuncts for increasing the dissemination of evidence-based psychotherapies and therapist fidelity to evidence-based treatments (e.g., Donker et al., 2013; Reger et al., 2013; Rizvi, Dimeff, Skutch, Carroll, & Linehan, 2011). Moreover, a recent meta-analysis examining the effects of mobile technology utilization on psychotherapy outcomes found that patients who utilized mobile technology (including apps) as either a supplement to treatment or as a substitute for direct therapist contact experienced superior outcomes as compared with patients who did not receive mobile technology (Lindhiem, Bennett, Rosen, & Silk, 2015). Supporting the utilization of mobile technologies in psychotherapy, over recent years mobile technologies broadly and mobile phones more specifically have dramatically increased in both affordability and ubiquity, with estimates suggesting that there are over 3.2 billion unique mobile users worldwide (Steinhubl, Muse, & Topol, 2013). A mobile app adjunct to traditional BATD psychotherapy would offer a fitting solution for addressing the above limitations associated with utilization of paper forms in BATD. Specifically, a mobile app adjunct to BATD has the potential to (a) provide the therapist with real-time data on patient treatment adherence and functioning; (b) make sessions more efficient as the therapist can review patient progress via a website prior to sessions, a feature which may be particularly useful for settings in which therapy sessions are delivered briefly (i.e., < 30 minutes); and (c) decrease motivational and organizational burden on the patient by eliminating the need for paper monitoring forms and delivering treatment materials via a smartphone, which may be preferable for some patients.
In order to potentially improve the feasibility of BATD, our team developed a mobile app version of BATD (Behavioral Apptivation) to be used in conjunction with ongoing therapy. In the remainder of this paper, we (a) describe the development of Behavioral Apptivation, (b) present preliminary data from a small open-label trial suggesting the feasibility of Behavioral Apptivation for the treatment of depressive symptomatology, and (c) highlight case examples illustrating utilization of Behavioral Apptivation.
Development and Description of Behavioral Apptivation
We assembled a diverse team with unique insights and skill sets to develop Behavioral Apptivation. Our team consisted of an original developer of BATD, a doctoral trainee who used the treatment frequently in research and clinical settings, and a small business focused on mobile app development. Our primary goals for app development were to (a) faithfully translate all treatment materials from BATD into a mobile application format and (b) utilize technology to potentially improve the feasibility of BATD.
Behavioral Apptivation consists of a patient mobile application, available via the iTunes app store, and a therapist Web site, accessible at www.behavioralapptivation.com. Consistent with BATD, we incorporated the following components into the Behavioral Apptivation patient mobile app:
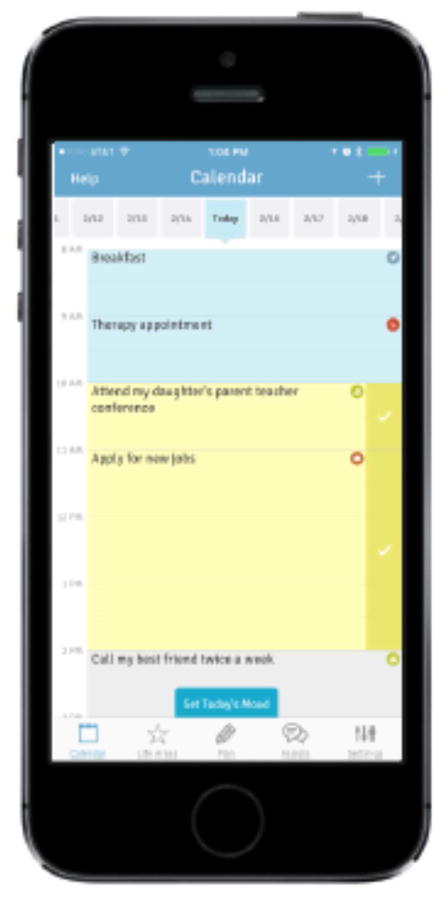
Daily monitoring. Patients complete daily monitoring via a Calendar screen (Figure 1). This screen was developed to serve the same purpose as the daily monitoring form (Form 1) in the original BATD manual, which is to facilitate monitoring of already occurring activities and rating of enjoyment and importance for each completed activity.
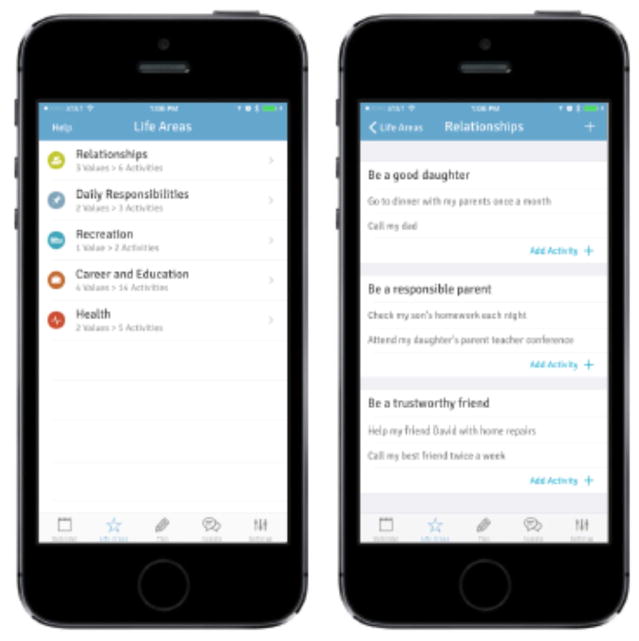
Life areas, values, and activities. We translated the Life Areas, Values, and Activities (LAVA) Inventory (Form 2 in the BATD manual) into an app version, which patients can access via the Life Areas icon at the bottom of each screen within the app. Similar to the paper LAVA Inventory, the purpose of this component is to facilitate development of values and activities across five different life areas (relationships, daily responsibilities, recreation, career and education, and health; Figure 2).
Scheduling value-driven activities. The cornerstone of BATD is incorporation of enjoyable and important value-driven activities. This is accomplished in BATD by utilizing the daily monitoring form to plan new activities. During BATD sessions 4 and beyond, planning new activities is the major focus of each therapy session. We translated this functionality to an app by incorporating a Plan tab (Figure 3), which patients can use to schedule value-driven activities and to view upcoming, scheduled activities. These scheduled activities can then be monitored via the Calendar screen, on which patients can rate enjoyment and importance of each activity.
Daily mood rating. BATD instructs patients to rate their mood daily at the bottom of the daily monitoring form. This information is then used during therapy sessions as therapists and patients work together to identify the relationship between activity level and mood. We translated this to an app format by having a tab that pops up on the bottom of the Calendar screen once per day (Figure 1), prompting patients to rate their mood for the day on a scale of 1 (terrible) to 5 (great).
Assists. For activities that are difficult for a patient to complete on his or her own, BATD suggests that the patient develop a contract in order to receive assistance to complete the activity. We translated this to an app component, which we refer to as “Assists.” We decided to change the term from “Contracts” to “Assists” as therapists have previously reported that the term “Contract” can be intimidating to patients. Via the Assists screen (Figure 4), a patient can select a difficult activity and then identify a person to help him or her complete that activity. The patient will then describe how the other person can help him or her to complete the activity and can schedule in a time to ask the other person for help. This function is similar to Form 4 (Contract) from the BATD manual.
Figure 1.
Calendar Screen
Figure 2.
Life Areas, Values, and Activities
Figure 3.
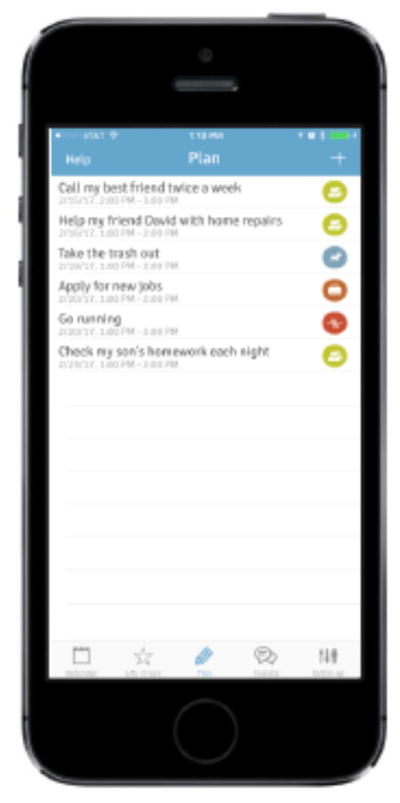
Viewing Planned Activities and Planning New Activities
Figure 4.
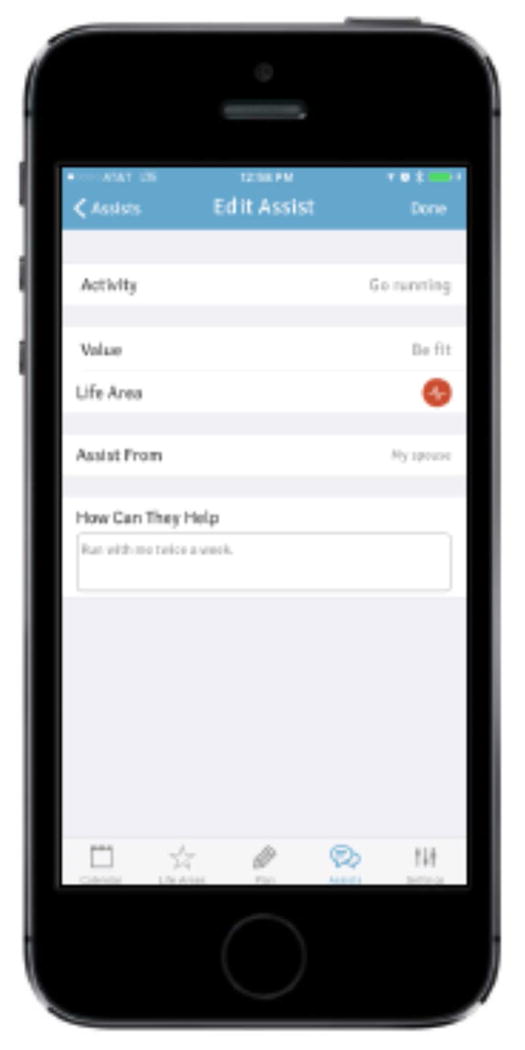
Assists
As noted above, in developing Behavioral Apptivation, we also sought to utilize technology to potentially improve treatment feasibility. The Behavioral Apptivation therapist Web site is a feature that is not available when utilizing BATD without the mobile app, which may improve treatment feasibility. Features that we incorporated into the therapist Web site that are not available in BATD without the mobile app include:
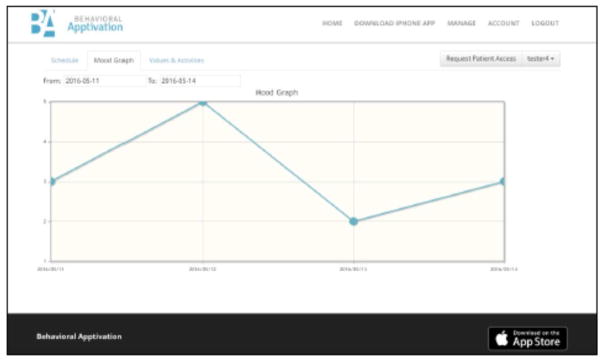
Mood graph. In our previous utilization of BATD in diverse clinical settings, we noted that therapists often liked to create a graph of their patients’ daily mood ratings. These graphs were then used in session as a catalyst for discussing fluctuations in daily mood. We decided to automate this graph and incorporate it into the therapist Web site, so that therapists could more easily track fluctuations in daily mood with their patients (Figure 5). By toggling back and forth between the Schedule screen and the Mood Graph screen on the therapist Web site, therapists have the option to work with their patients to identify the activities patients engaged in on days when mood was optimal as compared with days when mood was suboptimal.
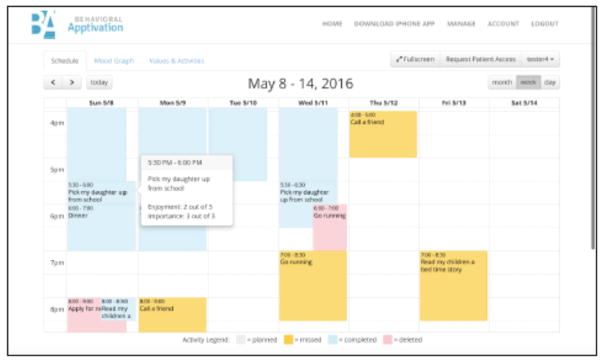
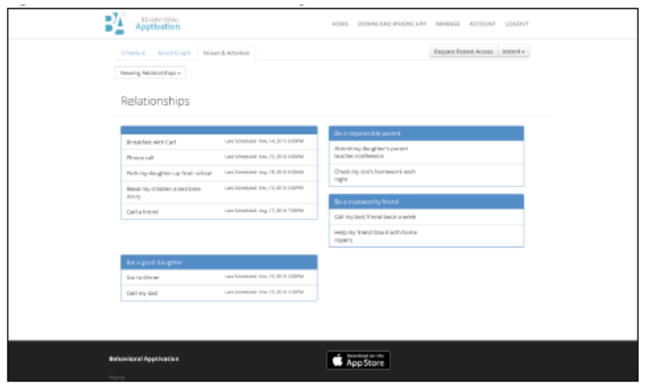
Ability to access patient treatment materials between sessions. Also in our utilization of BATD, we noted that some (but not all) therapists wished to have access to their patients’ treatment materials throughout the week, so that they could intervene early if they noticed that their patients were not adherent to the treatment. This could also potentially provide therapists with the ability to reinforce treatment compliance during the week. Thus, via the therapist Web site, therapists have access to their patients’ activity monitoring and scheduling, which updates in real time as a patient uses the app (Figure 6). It is important to note that this feature may not be appealing to all therapists as it could require that a therapist spend additional time each week reviewing each patient’s activity monitoring and scheduling.
Figure 5.
Mood Graph
Figure 6.
Viewing Patient Activity Monitoring and Scheduling
There were additional clinical features that we considered incorporating into Behavioral Apptivation, but ultimately opted against. These include:
Psychoeducation about depression and treatment rationale. A key component of BATD is psychoeducation, including an overview of treatment and treatment rationale. As patients utilizing Behavioral Apptivation should be utilizing the app in conjunction with a therapist and with ongoing therapy, we opted not to include this component in the app so as to allow therapists flexibility to approach psychoeducation and treatment rationale in whatever way is typical for their clinical practice. As an example, BATD is often integrated into other treatment modalities (e.g., substance use treatment, anxiety treatment). Thus, if we solely focused the treatment rationale within the app on depression, we would likely limit the reach of the app.
In-app reinforcement for completing activities. We considered adding “gamification” components, such as earning badges for utilizing the app, to Behavioral Apptivation with the goal of promoting treatment adherence. We ultimately opted against adding these features in order to allow therapists flexibility to reinforce patients in whatever way(s) align with their treatment plans. However, we did incorporate a simple, reinforcing message of “Nice going, you did it!” after a patient records an activity as completed.
Push notifications as reminders to complete activities. One way that Behavioral Apptivation could potentially improve BATD adherence is by reminding patients in the moment to complete their scheduled activities and daily monitoring via push notifications. We considered adding this feature in this version of the app, but opted against this due to concerns that patients might get frustrated with receiving too many notifications (e.g., if a patient scheduled five activities in 1 day, he or she would receive at least five notifications). Ultimately, the question of how frequently notifications should be sent to patients to reinforce treatment adherence is an empirical one, which we intend to explore in future research.
Syncing app calendar data to a patient’s personal calendar. We considered syncing calendar data from the Behavioral Apptivation Calendar screen to a patient’s personal calendar (e.g., Google Calendar, Outlook). We opted against adding that functionality at this point for two reasons: (a) it is unlikely that all patients would like this function, as many may prefer to keep information regarding their depression treatment separate from their personal or work calendars, and (b) the vast number of different electronic calendar systems (e.g., iCal, Google Calendar, Outlook) would have required considerable time and resources from our programming team. Thus, we decided to prioritize other app functions outlined above for the first version of Behavioral Apptivation.
Behavioral Apptivation Open-Label Trial
Following app development, we conducted a small, open-label feasibility trial of BATD utilizing Behavioral Apptivation with the goals of examining patient and therapist feasibility, acceptability, and change in depressive symptoms associated with receiving BATD with Behavioral Apptivation. The open-label trial utilized the 10-year revision of the BATD treatment manual (BATD-R; Lejuez et al., 2011). The intervention consisted of eight sessions of BATD. All treatment forms (e.g., LAVA Inventory, daily monitoring, contracts) were completed within the Behavioral Apptivation mobile application.
Study participants included both therapist participants (N = 10) who provided BATD and patient participants (N = 11, referred to as “participants” throughout the remainder of this section as these participants were recruited from the community). Each therapist was randomly assigned one participant. As discussed below, one participant discontinued treatment after Session 5, which resulted in one therapist treating a second participant. Therapists were recruited from the University of Maryland, College Park, clinical psychology doctoral program, which is a CBT-oriented program, and were advanced doctoral-level trainees in the program. All study therapists had prior experience administering BATD either via clinical research trials, in the university’s psychology clinic, or in local community clinics. In addition to prior experience administering BATD, therapists also completed a 2-hour “refresher” training in BATD prior to beginning in the trial. All study therapists attended weekly group supervision, during which all clinical cases were reviewed. Inclusion criteria for participants were as follows: (a) between the ages of 18 and 65, (b) reporting current elevated depressive symptoms (Beck Depression Inventory–II; BDI-II [Beck, Steer, & Brown, 1996] ≥ 14), and (c) owner of an iOS-compatible mobile phone (i.e., iPhone). No additional exclusion criteria were applied. Participants who did not meet study inclusion criteria were provided with community referrals.
Procedures
All study procedures were approved by the University of Maryland, College Park, Institutional Review Board. Participants were recruited using flyers and postings on Internet message boards and represent a convenience sample from the neighboring community around the University of Maryland, College Park, campus. Interested participants were directed to contact the study via e-mail, at which time they were e-mailed an online screening survey used to determine their eligibility. Once eligible for the study, participants were invited to our research center for weekly individual therapy sessions. Each therapist was randomly assigned one participant with the exception of one therapist who saw two participants (which resulted from an 11th patient being enrolled into the study after one patient discontinued treatment). Prior to Session 1, participants were sent an invitation to download the Behavioral Apptivation mobile app via Apple’s TestFlight app and successful installation was confirmed by research staff during their first scheduled appointment. Study therapists were similarly sent a unique username and password to www.behavioralapptivation.com with which they were able to log into the Web site and access their assigned participant’s data. At the beginning of the first scheduled appointment, the participant completed an informed consent. Immediately prior to each 1-hour therapy session, patients and participants completed study assessments. Participants were compensated $40 at the trial outset for completion of subsequent study assessments. Thus, participant compensation was not contingent upon therapy session attendance. Therapists were each similarly compensated $50 for completion of study assessments.
Measures
Participant Measures
Demographics
A standard demographics questionnaire was administered at baseline assessing participant age, gender, race/ethnicity, education, occupation, and income.
Depression
Depressive symptomatology was assessed using the BDI-II. The BDI-II was used both as a screening measure and as the primary outcome measure. Participants completed the BDI-II during the online screening and at the beginning of each of the eight therapy sessions and, thus, completed the BDI-II a total of nine times during the course of the study. Scores on the BDI-II are interpreted as follows: 0–13 = minimal depression, 14–19 = mild depression, 20–28 = moderate depression, 29–63 = severe depression.
Feedback on behavioral apptivation
At the end of treatment, participants completed a self-report measure regarding their experiences using Behavioral Apptivation. Participants responded to the following statements using a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree): (a) “I find Behavioral Apptivation easy to use,” (b) “I want to continue to use Behavioral Apptivation on my own after therapy has ended,” and (c) “I have experienced benefits from using Behavioral Apptivation.”
Therapist Measures
Feedback on Behavioral Apptivation
At the end of treatment, therapists completed a self-report measure assessing their experiences using Behavioral Apptivation and the Behavioral Apptivation Web site with their patients. Therapists responded to the following statements using a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree): (a) “I found Behavioral Apptivation easy to use with my patient,” (b) “I want to continue to use Behavioral Apptivation with patients in the future,” (c) “I have experienced benefits from using Behavioral Apptivation in therapy,” and (d) “The Behavioral Apptivation Web site was helpful.”
Data Analytic Plan
Data were analyzed using SPSS version 22 and SAS version 9.3. Descriptive statistics on the BDI-II across participants over time were used for examining changes in depressive symptoms during the course of treatment. Individual linear regression models were then fit for each participant, with the slope estimates averaged across participants to determine the general trend in depressive symptoms over time. Finally, a linear mixed-effects model with repeated participant measures was used in order to assess change in depression over time across participants, accounting for baseline levels of depressive symptoms. In this model, time was treated as a continuous variable. Descriptive statistics were used to understand participant and therapist feedback regarding Behavioral Apptivation utilization.
Open-Label Trial Results
Demographic and Clinical Characteristics
Participant demographic characteristics are summarized in Table 1. Ten out of the 11 participants attended all eight treatment sessions. One participant dropped out of the study following Session 5 and, thus, did not attend Sessions 6–8. Participants were primarily young adults, age M (SD) = 21.10 (3.25), and the majority of participants were female (n = 10). On average, at Session 1, participants scored in the moderate depression range on the BDI-II, M (SD) = 22.71 (6.14), range = 13.00–29.40).
Table 1.
Patient Demographics
| N | 11 |
| Age (M(SD)) | 19.41(1.06) |
| Gender (% Female) | 90.90% |
| Race | |
| White | 45.50% |
| Black | 18.20% |
| Asian | 27.30% |
| Other | 9.10% |
| BDI-II (M(SD)) Baseline | 25.64(4.72) |
| BDI-II (M(SD)) Session 1 | 22.71(6.14) |
| BDI-II (M(SD)) Session 2 | 18.64(7.23) |
| BDI-II (M(SD)) Session 3 | 18.55(9.72) |
| BDI-II (M(SD)) Session 4 | 19.64(9.51) |
| BDI-II (M(SD)) Session 5 | 19.73(9.21) |
| BDI-II (M(SD)) Session 6 | 18.02(10.78) |
| BDI-II (M(SD)) Session 7 | 19.32(7.52) |
| BDI-II (M(SD)) Session 8 | 14.62(10.65) |
Descriptive Analyses of Depressive Symptoms Over Time
Mean scores on the BDI-II across participants over time are presented in Table 1. Individual linear regression models were fit for each participant with time (treatment session) as a continuous predictor of depressive symptoms. The average of the individual regression slopes was M (SD) = –0.68 (1.12), 95% CI [–1.49, 0.12], suggesting a pattern of decreasing depressive symptoms over time across patients.
Mixed Effects Model of Depressive Symptoms Over Time
A linear mixed-effects model of depressive symptoms over time accounting for baseline depression and repeated measures within a participant revealed significant main effects of both time (B = –0.66, SE = 0.25, p = .01) and baseline depression (B = 0.97, SE = 0.42, p = .02) on depressive symptoms. These results suggest that depressive symptoms decreased over time and higher depressive symptoms at baseline were associated with higher depressive symptoms across assessments.
Participant Feedback on Behavioral Apptivation
Participant feedback regarding use of Behavioral Apptivation was, overall, positive. Average scores for each item on the feedback self-report were as follows: (a) ease of use, M (SD) = 4.00 (0.00); (b) continued desire to use Behavioral Apptivation on my own after therapy has ended, M (SD) = 2.80 (0.92); and (c) experienced benefits from using Behavioral Apptivation, M (SD) = 3.80 (0.92).
Therapist Feedback on Behavioral Apptivation
Feedback gathered from therapists regarding use of Behavioral Apptivation and the Behavioral Apptivation therapist Web site was similarly positive. Average scores for each item on the feedback self-report were as follows: (a) ease of use, M (SD) = 4.11 (0.33); (b) continued desire to use Behavioral Apptivation with patients in the future, M (SD) = 4.33 (0.71); (c) experienced benefits from using Behavioral Apptivation M (SD) = 4.56 (0.53); and (d) helpfulness of the Behavioral Apptivation Web site, M (SD) = 4.22 (0.83).
Limitations
In interpreting the results of this open-label trial, it is important to acknowledge study limitations. This was a small feasibility study with no control treatment, thus it is unclear whether treatment effects of BATD were bolstered by the addition of Behavioral Apptivation. Moreover, study participants were a nonclinical sample (i.e., they were not recruited on the basis of a depression diagnosis, nor did we assess for diagnostic-level depression) of female young adults, thus generalizability of these results is likely limited. Study therapists were doctoral-level trainees who were trained in BATD and had ongoing clinical supervision throughout the duration of the study. It is unclear whether similar outcomes would be found if this treatment were administered by other clinicians with different training backgrounds.
Case Examples
Below we provide several case examples of participants who participated in the open-label trial with the goal of illustrating how Behavioral Apptivation can be utilized with BATD. All participants treated during the open-label trial were discussed during weekly clinical supervision.
Case 1: Utilization of Behavioral Apptivation to Efficiently Use Session Time
Behavioral Apptivation may enhance BATD for some patients and therapists by making patient monitoring data easily accessible to the therapist, in real time, and easily interpretable. A therapist can check his or her patient’s monitoring data via the therapist Web site prior to session and color coding of activities on the Web site makes it easy to see which activities were completed and which were missed.
“Jessica” was a 20-year-old Asian American female who presented to treatment with elevated depressive symptoms that were exacerbated by academic stress. Jessica reported that she felt as if her life was completely wrapped up in academics and that she needed to “do more things for herself.” She reported feeling as if she was so focused on school and school-related activities that it was hard for her to plan things unrelated to school. She endorsed constant feelings of guilt when not completing school-related activities. Jessica was adherent to completing daily monitoring via the patient app and did not miss any days of monitoring.
Prior to each therapy session, Jessica’s therapist would spend approximately 5 minutes reviewing Jessica’s activity monitoring data from the previous week. All activities in Behavioral Apptivation are color coded, which made it easy for Jessica’s therapist to identify which activities were completed and which were missed. (See Figure 6 for an example of how activities appear and are color coded on the Behavioral Apptivation therapist Web site; note: To protect participant privacy, the data depicted in Figure 6 is mock data and is not specific to Jessica.) Jessica’s therapist then brought a laptop with her to each of Jessica’s therapy sessions and they together discussed patterns in Jessica’s activities and mood (see Figure 5 for an example of how mood is graphed on the Behavioral Apptivation therapist Web site). Because Jessica and her therapist were using Behavioral Apptivation, and Jessica’s therapist reviewed the therapist Web site ahead of the session, they were able to save time in session. This allowed Jessica’s therapist to focus the majority of each therapy session on Jessica, addressing (including praising) treatment adherence and generating and scheduling new value-driven activities.
Case 2: Utilization of Behavioral Apptivation to Make Therapy Materials More Accessible
Difficulties with concentration and, by extension, organization, are hallmark features of depression. Behavioral Apptivation seeks to limit the impact of these depressive symptoms on treatment by making all therapy materials available to the patient via the patient mobile app. If a patient has a smartphone, he or she is likely to have it nearby throughout the day, increasing the likelihood of real-time monitoring and decreasing the likelihood of forgetting treatment materials and not bringing them to a therapy session.
“Rebecca” was a 19-year-old African American female who presented with elevated symptoms of depression including depressed mood, isolation, and feelings of hopelessness. She reported prominent difficulties with concentration and that her difficulties concentrating were currently impairing her academic performance. Rebecca was a premedical major, but currently was getting grades of “C” and “D” in the majority of her classes due to losing and forgetting to complete assignments. Rebecca began using Behavioral Apptivation and, in the first session, her therapist reviewed with her the importance of regularly completing monitoring. Between Rebecca’s first and second therapy sessions, her therapist logged on to the Behavioral Apptivation therapist Web site to view Rebecca’s monitoring data. Rebecca’s therapist noticed that Rebecca completed activity monitoring for the first day after her therapy session, but then stopped monitoring. During Rebecca’s second therapy session, she problem solved with her therapist in order to improve her adherence to monitoring and efficiency with monitoring. Rebecca and her therapist scheduled in times to monitor when Rebecca was on the bus to and from campus. This was an ideal time to complete monitoring because Rebecca was typically on her phone at these times already. Rebecca’s monitoring subsequently improved between her second and third sessions and she completed monitoring for six out of the seven days between sessions.
Case 3: Utilization of Behavioral Apptivation for Tracking Patient Progress and for Providing Reinforcement Based on Progress
Typically, a therapist meets with a patient once per week, the patient is assigned between-sessions exercises (i.e., homework) to complete between sessions, and the therapist does not have contact with the patient until the next therapy session. However, if a therapist could be provided with additional information related to treatment progress and treatment response throughout the week, he or she could have the opportunity to intervene either when symptoms acutely worsen or to reinforce treatment adherence. Behavioral Apptivation provides therapists with this additional information via the therapist Web site so that therapists then have the option to provide support/encouragement and/or praise throughout the week.
“Jacob” was a 20-year-old White male who presented with elevated symptoms of depression that tended to peak when experiencing consequences related to binge drinking. Jacob was a member of a fraternity and would drink with friends at his fraternity house on most nights. When intoxicated, he did things he later regretted such as getting into fights with friends and destroying property. After these binge episodes, he would feel depressed, guilty, and self-critical.
Jacob developed the following values in session: (a) be consistent with exercise, (b) have good communication in my relationship, (c) be a diligent musician, and (d) spend more time engaging in positive alcohol-free activities (see Figure 2 for an example of how a patient would record values and activities within the patient mobile app). Consistent with these values, Jacob identified the following activities: (a) run three times a week for 45 minutes at a time, (b) text or call my girlfriend at least once per day, (c) play bass twice a week, and (d) go to two events per month organized by the Jewish Student Union. After Session 3 of therapy, Jacob scheduled playing the bass twice for the following week.
Jacob’s therapist reviewed Jacob’s treatment data on the therapist Web site between sessions and noticed that Jacob did not complete playing the bass on the first day it was scheduled. Jacob’s therapist decided to reach out to Jacob to provide support to increase the likelihood that Jacob would complete the activity of playing the bass the second time it was scheduled (as the therapist indicated he might do in the previous session). Jacob’s therapist called Jacob prior to the second time he was scheduled to play the bass to remind him to play the bass and they together problem solved around playing the bass. Subsequently, during Jacob’s next therapy session, he and his therapist worked together to develop an Assist (see Figure 4 for an example) to ask his roommate to form a band with him so that he would be more likely to play bass twice a week. Jacob scheduled in a time to ask his roommate to form a band with him. During the next week, Jacob’s therapist checked the therapist Web site on the day that Jacob was scheduled to ask his roommate to form a band with him. Jacob’s therapist noted that Jacob marked that he had completed the assist of asking his roommate to form a band with him and sent him an email saying, “Good job asking your roommate to form a band with you!” The level of “reaching out” between sessions is completely up to the therapist and should be discussed with the patient at the first session. It may not be the right strategy for some patients/therapists, but the option is available when using Behavioral Apptivation.
Summary, Current Status, and Future Directions
The current paper presents the development of Behavioral Apptivation, a BATD mobile app and accompanying therapist Web site. We also present results from a pilot open-label feasibility trial, including a case series from the trial. Results from the open-label trial suggest that utilization of Behavioral Apptivation as an adjunct to traditional BATD psychotherapy is feasible. Moreover, regarding changes in depression among patients enrolled in the treatment, results were encouraging as, across participants, there were significant decreases in depressive symptoms over time. On average across patients, BDI-II scores decreased 43% with patients in general moving from the moderate to mild depression range. These results are consistent with other BATD trials that have demonstrated significant effects of behavioral activation for the reduction of depression and associated impairment (Cuijpers, Van Straten, & Warmerdam, 2007; Mazzucchelli, Kane, & Rees, 2009). These similar effects on depression may suggest similar efficacy for the two delivery formats and that both may be viable options depending on variables such as patient and therapist preference, setting, and resources available. However, firm conclusions cannot be drawn without a larger randomized clinical trial.
Following the open-label trial, we subsequently made minor modifications to the Behavioral Apptivation therapist Web site and patient mobile app consistent with user feedback. These modifications included:
Incorporation of patient values into the therapist Web site. During clinical supervision, therapists in the clinical trial noted that it would be useful to have access to the values and activities their patients developed via the therapist Web site. We subsequently incorporated this feature into the therapist Web site (see Figure 7).
Graphic design changes to improve usability. Both patients and therapists provided feedback on graphic design changes that would improve functionality, which we incorporated into both the app and the Web site. These changes included things such as allowing the calendar on the therapist Web site to scroll vertically, so that there was more room to read each activity, as well as having importance and enjoyment ratings display when the therapist’s mouse hovers over an activity rather than having to click an activity. In the patient mobile app, we added a “Forgot Password” feature, as well as a link for the patient to learn more about BATD.
Figure 7.
Values and Activities Via the Therapist Website
It is important to note that Behavioral Apptivation likely is not universally preferable to traditional BATD without utilization of an app. For example, some patients may prefer paper forms or may not have a smartphone. Similarly, Behavioral Apptivation may not be useful in therapy practices in which therapists do not have quick access to a computer and to the Internet. Thus, both patient and therapist preference should be taken into account when deciding whether to utilize Behavioral Apptivation and should be discussed during treatment planning. Moreover, therapist contact time may not be equal with traditional BATD as compared with BATD + Behavioral Apptivation. For example, if a therapist decides to utilize Behavioral Apptivation to reach out to a patient between sessions, this would increase contact time and potentially burden on the therapist. To maximize the app’s ability to reinforce treatment adherence, it is likely that therapists would need to plan in additional time to monitor the therapist Web site and to contact patients between sessions.
Future Directions
The development of Behavioral Apptivation was informed by a wealth of clinical data supporting the original version of BATD. Moving forward, Behavioral Apptivation may be a clinical tool that can improve convenience of activity planning and tracking for patients in BATD, which thereby may improve treatment adherence and outcomes. Furthermore, therapists may find the available data in Behavioral Apptivation a useful clinical tool as compared with retrospective reported paper forms. These hypotheses are yet untested and are important avenues for future research. Additionally, it will be important to continue to evaluate Behavioral Apptivation in the context of both clinical trials and real-world clinical practice. Regarding real-world clinical practice, it will be important to empirically examine the cost/benefit of utilizing Behavioral Apptivation and potentially dedicating additional, nonbillable time between therapy sessions to activities such as reviewing the therapist Web site between sessions. Our preliminary pilot feasibility data set the stage for future larger-scale investigation of this intervention as well as dissemination. As Behavioral Apptivation continues to be evaluated, we intend to continue to update both the therapist Web site and patient mobile app based on user feedback.
Importantly, an evidence-based mobile app such as Behavioral Apptivation may be particularly useful for certain individuals who may be either unwilling or unable to engage in in-person therapy. Future adaptations of Behavioral Apptivation targeting these groups specifically has the potential to be clinically useful. For example, developing a self-help adaptation of Behavioral Apptivation for those individuals who may not be able to participate in traditional psychotherapy could reach a large number of individuals experiencing impairment from depressive symptomatology. Adaptations of Behvavioral Apptivation for incorporation in telehealth or phone/Skype therapy or for use during the maintenance phase of therapy to bolster retention of therapeutic gains could be impactful. Finally, as Behavioral Apptivation incorporates all treatment components of BATD, the app and therapist Web site could be useful in the future for therapist training.
Highlights.
Behavioral Apptivation is a mobile app adjunct to BATD.
Behavioral Apptivation consists of a patient mobile app and a therapist Web site.
We conducted a small feasibility trial of Behavioral Apptivation used with BATD.
Patients on average had a 43% reduction in depression from pre- to posttreatment.
Behavioral Apptivation is now available for use by clinicians and patients.
Acknowledgments
The authors thank the creative team at MountainPass Technology, LLC, including Zachary Gavin, Brian Cordyack, and Jim Nichols for their help with programming and graphic design of Behavioral Apptivation, as well as user support throughout the present trial.
Funding for this work was provided by the Maryland Technology Development Corporation (TEDCO) via the Maryland Innovation Initiative (MII; grant 2015-MII-1127, CWL), by the University of Maryland, College Park, and by NIDA (T32 DA007288, JD). The funding sources had no role in study design, data collection, data analysis, or data interpretation in writing this report, or in the decision to submit this article for publication. The authors declare no other conflicts of interest.
Footnotes
The authors are co-owners of Behavioral Activation Tech, LLC, which owns the rights to Behavioral Apptivation. The authors report no other actual or potential conflicts of interest that may bias the present work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jennifer Dahne, Medical University of South Carolina.
Jacob Kustanowitz, MountainPass Technology.
C. W. Lejuez, The University of Kansas
References
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Bolton P, Bass JK, Zangana GA, Kamal T, Murray SM, Kaysen D, … Murray LK. A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan, Northern Iraq. BMC Psychiatry. 2014;14(1):360. doi: 10.1186/s12888-014-0360-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassar J, Ross J, Dahne J, Ewer P, Teesson M, Hopko D, Lejuez CW. Therapist tips for the brief behavioural activation therapy for depression–revised (BATD-R) treatment manual practical wisdom and clinical nuance. Clinical Psychologist. 2016;20(1):46–53. doi: 10.1111/cp.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collado A, Calderon M, MacPherson L, Lejuez C. The efficacy of behavioral activation treatment among depressed Spanish-speaking Latinos. Journal of Consulting and Clinical Psychology. 2016;84(7):651–657. doi: 10.1037/ccp0000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collado A, Castillo SD, Maero F, Lejuez C, MacPherson L. Pilot of the brief behavioral activation treatment for depression in Latinos with limited English proficiency: Preliminary evaluation of efficacy and acceptability. Behavior Therapy. 2014;45(1):102–115. doi: 10.1016/j.beth.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collado A, Long KE, MacPherson L, Lejuez CW. The efficacy of a behavioral activation intervention among depressed US Latinos with limited English language proficiency: Study protocol for a randomized controlled trial. Trials. 2014;15(1):231. doi: 10.1186/1745-6215-15-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Van Straten A, Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review. 2007;27(3):318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Braun AR, Sargeant MN, Reynolds EK, Hopko DR, Blanco C, Lejuez C. Effectiveness of a brief behavioral treatment for inner-city illicit drug users with elevated depressive symptoms: The life enhancement treatment for substance use (LETS Act!) Journal of Clinical Psychiatry. 2008;69(1):122–129. doi: 10.4088/JCP.v69n0116. [DOI] [PubMed] [Google Scholar]
- Donker T, Petrie K, Proudfoot J, Clarke J, Birch MR, Christensen H. Smartphones for smarter delivery of mental health programs: A systematic review. Journal of Medical Internet Research. 2013;15(11):e247. doi: 10.2196/jmir.2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede LE, Acierno R, Knapp RG, Lejuez C, Hernandez-Tejada M, Payne EH, Frueh BC. Psychotherapy for depression in older veterans via telemedicine: A randomised, open-label, non-inferiority trial. Lancet Psychiatry. 2015;2(8):693–701. doi: 10.1016/S2215-0366(15)00122-4. [DOI] [PubMed] [Google Scholar]
- Gawrysiak M, Nicholas C, Hopko DR. Behavioral activation for moderately depressed university students: Randomized controlled trial. Journal of Counseling Psychology. 2009;56(3):468–475. doi: 10.1037/a0016383. [DOI] [Google Scholar]
- Gros DF, Price M, Strachan M, Yuen EK, Milanak ME, Acierno R. Behavioral activation and therapeutic exposure: An investigation of relative symptom changes in PTSD and depression during the course of integrated behavioral activation, situational exposure, and imaginal exposure techniques. Behavior Modification. 2012;36:580–599. doi: 10.1177/0145445512448097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopko DR, Armento ME, Robertson S, Ryba MM, Carvalho JP, Colman LK, … McNulty JK. Brief behavioral activation and problem-solving therapy for depressed breast cancer patients: Randomized trial. Journal of Consulting and Clinical Psychology. 2011;79(6):834–849. doi: 10.1037/a0025450. [DOI] [PubMed] [Google Scholar]
- Hopko DR, Lejuez C, Lepage JP, Hopko SD, McNeil DW. A brief behavioral activation treatment for depression: A randomized pilot trial within an inpatient psychiatric hospital. Behavior Modification. 2003;27(4):458–469. doi: 10.1177/0145445503255489. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The costs of depression. Psychiatric Clinics of North America. 2012;35(1):1–14. doi: 10.1016/j.psc.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, Acierno R, Daughters SB, Pagoto SL. Ten year revision of the brief behavioral activation treatment for depression: Revised treatment manual. Behavior Modification. 2011;35(2):111–161. doi: 10.1177/0145445510390929. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, LePage JP, Hopko SD, McNeil DW. A brief behavioral activation treatment for depression. Cognitive and Behavioral Practice. 2001;8(2):164–175. doi: 10.1016/S1077-7229(01)80022-5. [DOI] [Google Scholar]
- Lindhiem O, Bennett CB, Rosen D, Silk J. Mobile technology boosts the effectiveness of psychotherapy and behavioral interventions: A meta-analysis. Behavior Modification. 2015;39(6):785–804. doi: 10.1177/0145445515595198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson L, Tull MT, Matusiewicz AK, Rodman S, Strong DR, Kahler CW, … Lejuez C. Randomized controlled trial of behavioral activation smoking cessation treatment for smokers with elevated depressive symptoms. Journal of Consulting and Clinical Psychology. 2010;78(1):55–61. doi: 10.1037/a0017939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Gorka SM, MacPherson L, Hopko DR, Blanco C, Lejuez C, Daughters SB. Examining the effect of the life enhancement treatment for substance use (LETS ACT) on residential substance abuse treatment retention. Addictive Behaviors. 2011;36(6):615–623. doi: 10.1016/j.addbeh.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin RC. Agile software development: Principles, patterns, and practices. Upper Saddle River, NJ: Prentice Hall; 2003. [Google Scholar]
- Mazzucchelli T, Kane R, Rees C. Behavioral activation treatments for depression in adults: A meta-analysis and review. Clinical Psychology: Science and Practice. 2009;16(4):383–411. doi: 10.1111/j.1468-2850.2009.01178.x. [DOI] [Google Scholar]
- Reger GM, Hoffman J, Riggs D, Rothbaum BO, Ruzek J, Holloway KM, Kuhn E. The “PE coach” smartphone application: An innovative approach to improving implementation, fidelity, and homework adherence during prolonged exposure. Psychological Services. 2013;10(3):342–349. doi: 10.1037/a0032774. [DOI] [PubMed] [Google Scholar]
- Reynolds EK, MacPherson L, Tull MT, Baruch DE, Lejuez C. Integration of the brief behavioral activation treatment for depression (BATD) into a college orientation program: Depression and alcohol outcomes. Journal of Counseling Psychology. 2011;58(4):555–564. doi: 10.1037/a0024634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Dimeff LA, Skutch J, Carroll D, Linehan MM. A pilot study of the DBT coach: An interactive mobile phone application for individuals with borderline personality disorder and substance use disorder. Behavior Therapy. 2011;42(4):589–600. doi: 10.1016/j.beth.2011.01.003. [DOI] [PubMed] [Google Scholar]
- Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? JAMA. 2013;310(22):2395–2396. doi: 10.1016/j.beth.2011.01.003. [DOI] [PubMed] [Google Scholar]
- Strachan M, Gros DF, Ruggiero KJ, Lejuez CW, Acierno R. An integrated approach to delivering exposure-based treatment for symptoms of PTSD and depression in OIF/OEF veterans: Preliminary findings. Behavior Therapy. 2012;43(3):560–569. doi: 10.1016/j.beth.2011.03.003. [DOI] [PubMed] [Google Scholar]
- Sturmey P. Behavioral activation is an evidence-based treatment for depression. Behavior Modification. 2009;33(6):818–829. doi: 10.1177/0145445509350094. [DOI] [PubMed] [Google Scholar]
- Vanderplasschen W, Rapp RC, Wolf JR, Broekaert E. The development and implementation of case management for substance use disorders in North America and Europe. Psychiatric Services. 2014;55(8):913–922. doi: 10.1176/appi.ps.55.8.913. [DOI] [PMC free article] [PubMed] [Google Scholar]