Abstract
Background & objectives:
Ischaemic heart disease (IHD) has been one of the leading causes of mortality in the world. In many European countries the mortality rates due to IHD have been rising rapidly. This study was aimed to assess the IHD mortality trend in Serbia.
Methods:
A population-based cross-sectional study analyzing IHD mortality in Serbia in the period 1991-2013 was carried out based on official data. The age-standardized rates (ASRs, per 100,000) were calculated using the direct method, according to the European standard population. Joinpoint analysis was used to estimate the average annual percentage change (AAPC) with the corresponding 95 per cent confidence interval (CI).
Results:
More than 253,000 people (143,420 men and 110,276 women) died due to IHD in Serbia during the observed period, and most of them (over 160,000 people) were patients with myocardial infarction (MI). Average annual ASR for IHD was 113.6/100,000. There was no overall significant trend for mortality due to IHD (AAPC=+0.1%, 95% CI −0.8-1.0), but there was one joinpoint: the trend significantly increased by +2.3 per cent per year from 1991 to 2006 and then significantly decreased by −6.4 per cent from 2006 to onwards. Significantly decreased mortality trends for MI in both genders were observed: according to the comparability test, mortality trends in men and women were parallel (final selected model failed to reject parallelism, P=0.0567).
Interpretation & conclusions:
No significant trend for mortality due to IHD was observed in Serbia during the study period. The substantial decline of mortality from IHD seen in most developed countries during the past decades was not observed in Serbia. Further efforts are required to reduce mortality from IHD in Serbian population.
Keywords: Ischaemic heart disease, joinpoint regression analysis, mortality, myocardial infarction, Serbia, trend
Ischaemic heart disease (IHD) was the leading killer disease during the last decades in the world1,2. According to the World Health Organization (WHO) estimates, IHD caused 7.4 million deaths in the world in 2012 (this represents about 13.2% of all deaths globally), up from 6.0 million (11.3%) deaths in 20001. IHD alone has been the most common cause of death in Europe, accounting for nearly 2 million deaths each year: approximately 22 per cent of all deaths in women and 21 per cent of all deaths in men2.
In 2013, the number of people who died from IHD worldwide was more than 8.1 million, representing an increase of 41 per cent from 1990: the global increase in deaths was a result of population ageing (52.5% increase from 1990) and population growth (23.6% increase from 1990)3. In addition, IHD was the leading cause of years of life lost due to premature mortality in 20014. Three-fourths of global deaths due to IHD occurred in the low- and middle-income countries5. Currently, IHD is a growing problem in most of the developing regions of the world4,5,6,7,8.
In the past decades, mortality rates from IHD have been generally higher in Central and Eastern Europe than in other regions1,2. Mediterranean countries (such as Spain, Greece) have been historically considered as those of ‘low risk’ for IHD9. Since 1970s, death rates from IHD have been falling rapidly in North America and many Northern and Western European countries but rising rapidly in some Central and Eastern European countries2,7. The main exception was Slovakia and several countries in Latin America, where rates varied very slightly from year to year during the last decades1,2. Around two-thirds of the decline in IHD mortality were due to a decline in exposure to cardiovascular risk factors and the remaining one-third was due to improvements in treatment10. The aetiology of IHD has not been entirely elucidated, but advancing age, tobacco use, overweight/obesity, high level of blood cholesterol, hypertension and diabetes mellitus were recognized as risk factors for IHD11. There is no direct evidence, but some contemporary risk factors (such as infectious agents, C-reactive protein, etc.) have been associated with IHD12,13.
Serbia is a small country in Southeast Europe. Former studies14,15 on IHD in Serbia were aimed to assess only patterns within country regions. The aim of this study was to assess the IHD mortality trend in the entire Serbia from 1991 to 2013 and to compare the similarities and differences in mortality with other parts of the world.
Material & Methods
Annual data on the number of deaths due to IHD - codes 410-414 in the 9th and codes I20-I25 in the 10th revision of the International Classification of Diseases (ICD)16,17 were obtained from the National Statistical Office of the Republic of Serbia for the period 1991-2013 (unpublished data). The data about the deceased from myocardial infarction (MI: code 410 in the 9th and codes I21-I22 in the 10th revision) were presented separately.
All deaths occurring in Serbia were registered with the statistical report on death18 (DEM-2 form), which contained a death certificate, form for registration of the main cause of death. Death certificates in Serbia are granted by an authorized physician in the healthcare organization, a coroner or a forensic doctor. Death certificate is coded and processed at the local public health institute where certain disease is specified as the underlying and/or immediate cause of death. The death certificate passes through several levels of control and verification (from the local registrar to the referral public health institute). The procedure is consistent throughout the entire Serbia. The quality of the data was provided by certified physicians by checking the accuracy of the death certificate data, the selection of the main cause of death and the coding of the cause of death. If necessary, death files are corrected by another trained medically qualified staff (medical doctor or a specialist). In Serbia, from 1991 to 1996 data about the cause of death were classified by the ICD 9th revision19, and since 1997, the data processing of mortality statistics was based on the ICD 10th revision20. The proportion of deaths assigned as ‘symptoms, signs and ill-defined conditions’ (ICD 9th revision codes 780-799 and ICD 10th revision codes R00-R99), as one indicator of the quality of coding in the registration system, was on average <10 per cent and indicated the quality of the mortality data in Serbia as of medium-quality in the observed period. The completeness of mortality database of Serbia was 98 per cent in 200021.
Data about the Serbian population were extracted from demographic statistics database from the Statistical Office of the Republic of Serbia. Data for the Republic of Serbia, without the Autonomous Province of Kosovo and Metohija (for which data are unavailable since 1998 and which declared itself independent in 2008), were included in the analysis. The Serbian population data were provided on the basis of official censuses in 1991, 2002 and 2011, while for inter-census years, the estimates of the resident population were obtained from the State Statistical Office database22. The analysis was conducted on the entire Serbian population (approximately 7.2 million inhabitants in 201322). The data on internally displaced persons and refugee population in Serbia were also included in the analysis.
This study was approved by the Ethics Committee of the Faculty of Medical Sciences, University of Kragujevac (protocol: 01-4801).
Statistical analysis: Age- and sex-specific and age-standardized rates (ASRs, using the European standard population and the method of direct standardization) were calculated. Rates were expressed as deaths per 100,000 persons. Age-specific mortality rates were calculated for the age interval from 0 to 80 and over by 10-yr periods. The results are not shown for the subgroups aged <30 yr because fewer than five cases of IHD deaths occurred in each of the decennium in any year.
Mortality trends from IHD were assessed using the joinpoint regression analysis (Joinpoint regression software, Version 4.0.4 - May 2013; Statistical Methodology and Applications Branch, Surveillance Research Program of the U.S. National Cancer Institute; Bethesda, MD, USA), as per the method proposed by Kim et al23. Joinpoint analysis was performed to identify the points at which a significant change of direction in the trend occurred for IHD mortality (also called ‘joinpoints’). The true number of joinpoints was verified with the Monte Carlo Permutation method23 with 4499 randomly selected data sets. The analysis starts with the minimum number of joinpoints (i.e., 0 joinpoint, representing a straight line) and tests for model fit with a maximum of five joinpoints in each analysis. The Grid Search Method24 was used to fit the segmented line regression where the joinpoint estimates occur at discrete grid points and to determine the best fit for each individual model. Results are presented as the annual percentage change (APC) between successive change points. In addition, the average APC (AAPC) over entire study period was calculated25. All estimates are presented with 95 per cent confidence intervals (CIs). Comparability test was used to assess disparities in mortality trends according to age and gender26.
Comparison with the World Health Organization (WHO) mortality data
The comparison of the mortality from IHD in Serbia with the corresponding rates from selected European countries was performed using Serbian population-based data and estimates from the WHO Regional Office for Europe27. The mortality rates from IHD, standardized to the European population, were compared for the beginning and the end of the study period (or last available).
Results
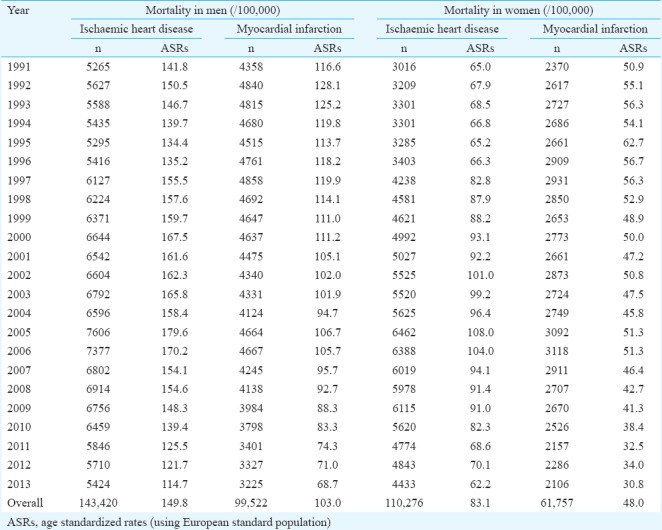
More than 253,000 persons (143,420 men and 110,276 women) died due to IHD in Serbia in 1991-2013, and most of them (over 160,000 of deceased, nearly 65% of all) were patients with MI (Table I). The average annual ASR for MI was higher in men (103.0 per 100,000) than in women (48.0), as well as the average ASR for IHD overall (149.8 in men and 83.1 in women).
Table I.
Ischaemic heart disease mortality for men and women in Serbia (excluding the Autonomous Province of Kosovo and Metohia) during 1991-2013
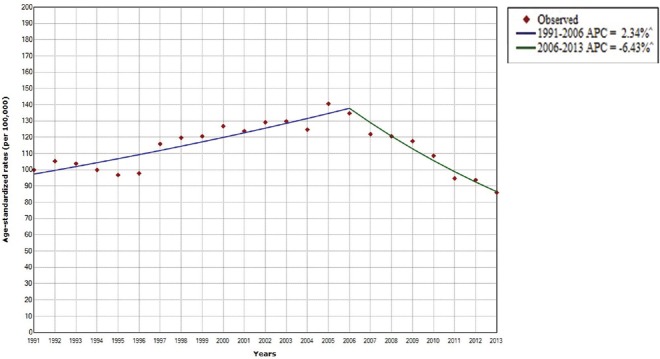
There was no overall significant trend for mortality of IHD in Serbia over the entire observation period (AAPC=+0.1%, 95% CI −0.8-1.0), but joinpoint regression analysis showed that the mortality significantly increased by +2.3 per cent per year from 1991 to 2006 and then significantly decreased by −6.4 per cent from 2006 onwards (Fig. 1).
Fig. 1.
Ischaemic heart diseases mortality trend in Serbia (excluding the Autonomous Province of Kosova and Metohia), 1991-2013; joinpoint analysis: all: 1 joinpoint.
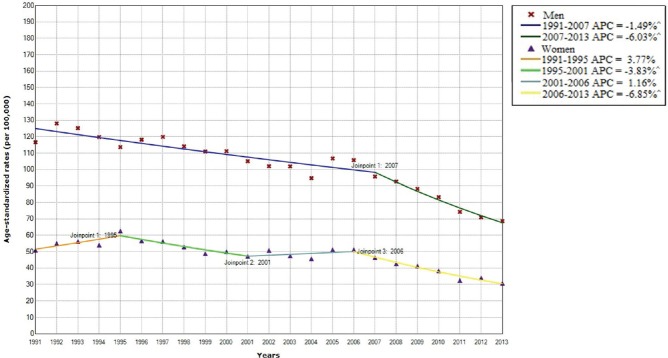
Significantly decreasing trends in MI mortality were observed in men and women (Fig. 2). Among men, a significant decrease of MI mortality from 1991 to 2007 (by −1.5% per year) was followed by a marked decrease (by –6.0% per year). In women, after a non-significant increase from 1991 to 1995 (+3.8% per year), MI death rates began to significantly decline in 1995-2001 period (by −3.8% per year), but then showed a non-significant increase from 2001 to 2006 (+1.2% per year) followed by a significant downwards trend in the last eight years of the observed period (by −6.9% per year). According to the comparability test, mortality trends from MI in men and women were parallel (final selected model failed to reject parallelism, P=0.0567).
Fig. 2.
Myocardial infarction mortality in Serbia (excluding the Autonomous Province of Kosova and Metohia), by gender, 1991-2013; joinpoint analysis: Men: 1 joinpoint versus women: 3 joinpoints.
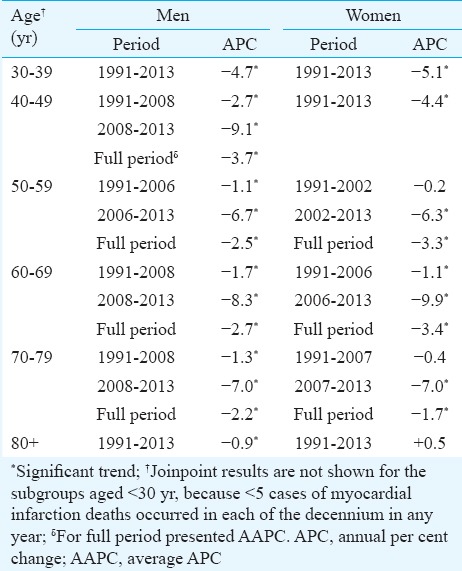
The negligible gender differences between mortality trends from MI by age were presented in Table II: in both genders, a significant declining trend was evident, only in women in the oldest age group (80+ years) an upwards trend (+0.5% per year) was present but without significance. Significant decline in MI mortality in men was observed in all age groups since 1991, with greater decrease starting from 2008. Significant declining trends in MI mortality were observed for women aged 30-49 yr for the entire period. There was also a significant decrease of MI mortality among women aged 50-79 after the mid-2000s.
Table II.
Trends in age-specific myocardial infarction rates in Serbia (excluding the Autonomous Province of Kosovo and Metohia) by gender, 1991-2013: Joinpoint analysis
The mortality ASRs in Serbia for 1991 and 2013 against European estimates are presented in Fig. 3. The ASRs of IHD in Serbia were higher than the mortality in Mediterranean countries (such as Portugal, Spain and Italy) both in beginning and end year of the study period. IHD mortality rates in Western and Northern Europe in 1991 were higher than rates in Serbia while in 2013, these rates were lower (except in Finland). In the countries of Western, Northern, Central and Southern Europe, mortality rates in 2013 were significantly lower than rates in 1991. On the contrary, in most East European countries (such as Ukraine, Russian Federation, Republic of Moldova, Belarus, Kyrgyzstan), IHD mortality rates were higher in 2013 compared to 1991. The mortality of IHD in the Serbian population (94.7/100,000) was above the average mortality rates in European Union (75.9/100,000) in 2013.
Fig. 3.
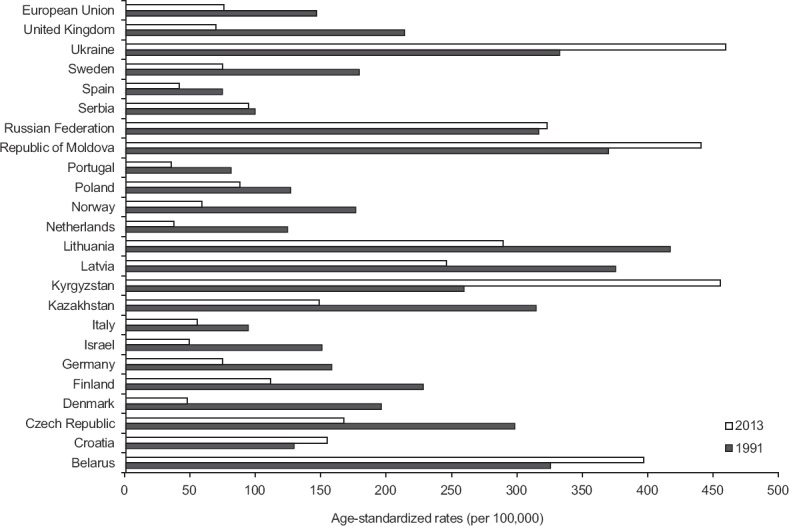
Ischaemic heart diseases mortality, World Health Organization 1991 and 2013 estimates (Source: Ref 27).
Discussion
Serbia ranks among the countries with intermediate mortality rates for IHD in the world. There was no overall significant trend for mortality of IHD over the entire observation period: a significant increase in mortality rates was observed at the beginning, with a significant decrease in mortality reported in the end of study period.
According to the recent available data for European Region (2010), the highest mortality rates for IHD in both genders were observed in Eastern and Central Europe (Republic of Moldova - 496.2 per 100,000 persons, Ukraine - 491.9), very high rates were recorded in the Russian Federation - 349.4 and Lithuania - 313.9, high rates were recorded in Slovakia - 260.7 and Croatia - 164.2, intermediate rates were observed in Germany - 80.9 and the United Kingdom - 77.2, and the lowest rates were noticed in France - 30.327. In addition, the highest rates among men were recorded in Ukraine (656.3) and Republic of Moldova (597.0), and the lowest rates were found in France (47.3) and Portugal (55.0). Similarly, the lowest rates in women were recorded in France and Spain (17.5 and 26.8, respectively) while the highest rates were noticed in Republic of Moldova and Ukraine (424.3 and 391.5, respectively). With a rate of 86.0 in 2010, Serbia was ranked among the countries with intermediate mortality rates of IHD. The highest rates across the countries of the former Eastern Bloc likely reflect the rapid social and economic changes during the transition period since 1980s27,28. The main contributor to the high mortality rates of IHD was high smoking prevalence21.
During the last decades of the 20th century, IHD has demonstrated a declining trend of deaths in both men and women throughout more developed regions: in Western and Northern European countries (in the United Kingdom, Finland) and worldwide (in the United States of America, Australia)1,2,29. At the beginning of the 21st century, the decline was also recorded in Japan2, and France30. In contrast, in some countries in Eastern Europe (such as Ukraine, Kyrgyzstan), as well as some other countries (Mexico, Republic of Korea), the increase in mortality from IHD was recorded2. More than half of the IHD mortality decrease in developed countries was attributed to favourable population risk factor trend (principally declining smoking prevalence, mean cholesterol concentrations and blood pressure levels) while the remaining minor part was due to improvements in medical and surgical treatment10,31,32. The mortality rate from IHD began to decline earlier in the countries where the tobacco control started to be implemented earlier (such as the USA, the United Kingdom, Australia). The plateaus in IHD mortality among young population may be partly linked to the increased rates of obesity and diabetes that have occurred over the same period in some of developed countries33. However, the recent increasing trends in some Eastern European countries suggest that other factors (including mainly obesity, physical inactivity, diabetes and dietary factors), besides smoking, may have influenced the IHD mortality9,29. Reasons for the substantial declines in mortality rates of IHD in Serbia since 2006 were not completely elucidated. Decreased smoking, particularly in men, has been widely recognized as the main contributor to the decreases in mortality trends from IHD in Serbia34. The antismoking campaign in Serbia might have contributed to a decrease in the number of smokers by 6.9 per cent in 2006 (by 9.8 and 3.8% in men and women, respectively)34. The WHO Convention on Tobacco Control entered into force in Serbia in June 2006, followed by other activities on tobacco control35. In addition, improvements in diagnostic and therapeutic technologies, re-establishment of a regular supply of drugs (including better treatment of hypertension, hyperlipidaemia and diabetes mellitus), and general improvements in living conditions probably contributed to the decreasing IHD mortality noted in Serbia36.
Like in the other European countries, mortality rates for MI were substantially higher in males than females in Serbia that could be due to differences in age, smoking habit, diabetes and alcohol use between men and women. In Serbia, MI mortality pattern was characterized by an initial decrease and followed by a sharp decline since 2007 (less pronounced declines observed in eldest women during the study). With exception of older women, mortality from MI in Serbia declined since 1991 in all age groups in both genders. The National health surveys (2000, 2006, 2013)34 have shown that the prevalence of cardiovascular risk factors (such as smoking, obesity, diabetes mellitus, hypertension, hyperlipidaemia) in Serbian population was higher in comparison to the majority of the neighbouring countries and other European countries10,11,33.
The strength of this study was that this was a nationwide study. Furthermore, the death registration system was uniform over entire Serbia, with comprehensive coverage by death registration system across the country. Mortality data in Serbia was evaluated as medium quality based on the WHO criteria (criterion used: completeness reporting is >90% and ill-defined causes and injury deaths with undetermined intent appear on <10% of registrations)37 and thus enabled comparison with other countries.
The lack of data on the incidence of IHD and survival rates in Serbia in the observed period was a limitation of our study. Acute coronary syndrome population register was established in 2006 in Serbia. In this study, data were collected for the period during which the definition of MI was amended in 2000. The definition of MI (and IHD) should be resistant to changes over time so that temporal trends in the mortality of MI can be evaluated38. The inability to specifically analyze the trend of IHD mortality in a population of refugees and internally displaced persons in Serbia was also a limitation of this study.
In conclusion, there was no significant trend for mortality of IHD in Serbia over the entire observation period. Additional analytical epidemiological research on risk factors for IHD among the Serbian population is needed.
Acknowledgment
This work was supported by the Ministry of Education and Science of Republic of Serbia through Contract No. 175042.
Footnotes
Conflicts of Interest: None.
References
- 1.World Health Organization. World Health Statistics 2013. Geneva: WHO; 2013. [Google Scholar]
- 2.World Health Organization. WHO Mortality Database. Geneva: WHO; 2015. [Google Scholar]
- 3.Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333–41. doi: 10.1056/NEJMoa1406656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Disease Control Priorities Project. Washington: The World Bank - Oxford University Press; 2006. Global Burden of Disease and Risk Factors. [Google Scholar]
- 5.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta R, Joshi P, Mohan V, Reddy KS, Yusuf S. Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008;94:16–26. doi: 10.1136/hrt.2007.132951. [DOI] [PubMed] [Google Scholar]
- 7.Murray CJL, Lopez AD, editors. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and Projected to 2020. Boston: The Harvard School of Public Health; 1996. [Google Scholar]
- 8.Liu MB, Wang W, Zhou MG. Trend analysis on the mortality of cardiovascular diseases from 2004 to 2010 in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2013;34:985–8. [PubMed] [Google Scholar]
- 9.Menotti A, Puddu PE. Coronary heart disease differences across Europe: A contribution from the seven countries study. J Cardiovasc Med (Hagerstown) 2013;14:767–72. doi: 10.2459/JCM.0b013e3283628dff. [DOI] [PubMed] [Google Scholar]
- 10.Unal B, Critchley JA, Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation. 2004;109:1101–7. doi: 10.1161/01.CIR.0000118498.35499.B2. [DOI] [PubMed] [Google Scholar]
- 11.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 12.Padmavati S, Gupta U, Agarwal HK. Chronic infections & coronary artery disease with special reference to Chalmydia pneumoniae. Indian J Med Res. 2012;135:228–32. [PMC free article] [PubMed] [Google Scholar]
- 13.Ray S, Talukdar A, Sonthalia N, Saha M, Kundu S, Khanra D, et al. Serum lipoprotein ratios as markers of insulin resistance: A study among non-diabetic acute coronary syndrome patients with impaired fasting glucose. Indian J Med Res. 2015;141:62–7. doi: 10.4103/0971-5916.154504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vujcic IS, Sipetic SB, Dubljanin ES, Vlajinac HD. Trends in mortality rates from coronary heart disease in Belgrade (Serbia) during the period 1990-2010: A joinpoint regression analysis. BMC Cardiovasc Disord. 2013;13:112. doi: 10.1186/1471-2261-13-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ratkov I, Sipetić S, Vlajinac H, Sekeres B. Mortality from heart attack in Belgrade population during the period 1990-2004. Srp Arh Celok Lek. 2008;136:598–602. doi: 10.2298/sarh0812598r. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organisation. International Classification of Diseases, 9 th revision (ICD-9) Geneva: WHO; 1977. [Google Scholar]
- 17.World Health Organisation. International Statistical Classification of Diseases and Related Health Problems, 10 th Revision (ICD-10) Geneva: WHO; 1992. [Google Scholar]
- 18.Statistical Office of the Republic of Serbia. Statistics of deaths. Belgrade: Statistical Office of the Republic of Serbia; [accessed on December 12, 2015]. Available from: http://www.stat.gov.rs/WebSite/userFiles/file/Stanovnistvo/SMET/SMETEng/SMET018020E.pdf . [Google Scholar]
- 19.Institute of Public Health of Serbia. Health Statistical Yearbook of Republic of Serbia, 1991-1996. Belgrade: Institute of Public Health of Serbia; 1991-1996. [Google Scholar]
- 20.Institute of Public Health of Serbia. Health Statistical Yearbook of Republic of Serbia, 1997-2013. Belgrade: Institute of Public Health of Serbia; 1997-2013. [Google Scholar]
- 21.Atanackovic-Markovic Z, Bjegovic V, Jankovic S, Kocev N, Laaser U, Marinkovic J, et al. The burden of disease and injuries in Serbia. Belgrade: Ministry of Health, Republic of Serbia; 2003. [Google Scholar]
- 22.Statistical Office of the Republic of Serbia. Statistical Yearbook of Serbia, 1991-2013. Belgrade: Statistical Office of the Republic of Serbia; 1991-2013. [Google Scholar]
- 23.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 24.Lerman PM. Fitting segmented regression models by grid search. Appl Stat. 1980;29:77–84. [Google Scholar]
- 25.Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28:3670–82. doi: 10.1002/sim.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim HJ, Fay MP, Yu B, Barrett MJ, Feuer EJ. Comparability of segmented line regression models. Biometrics. 2004;60:1005–14. doi: 10.1111/j.0006-341X.2004.00256.x. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization. European Health for All Database (HFA-DB) Copenhagen: WHO Regional Office for Europe; 2015. [Google Scholar]
- 28.Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, et al. Cardiovascular disease and risk factors in Asia: A selected review. Circulation. 2008;118:2702–9. doi: 10.1161/CIRCULATIONAHA.108.790048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nichols M, Townsend N, Scarborough P, Rayner M. Trends in age-specific coronary heart disease mortality in the european union over three decades: 1980-2009. Eur Heart J. 2013;34:3017–27. doi: 10.1093/eurheartj/eht159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finegold JA, Asaria P, Francis DP. Mortality from ischaemic heart disease by country, region, and age: Statistics from World Health Organisation and United Nations. Int J Cardiol. 2013;168:934–45. doi: 10.1016/j.ijcard.2012.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levi F, Chatenoud L, Bertuccio P, Lucchini F, Negri E, La Vecchia C, et al. Mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world: An update. Eur J Cardiovasc Prev Rehabil. 2009;16:333–50. doi: 10.1097/HJR.0b013e328325d67d. [DOI] [PubMed] [Google Scholar]
- 32.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: Concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128–32. doi: 10.1016/j.jacc.2007.05.056. [DOI] [PubMed] [Google Scholar]
- 33.Hotchkiss JW, Davies CA, Dundas R, Hawkins N, Jhund PS, Scholes S, et al. Explaining trends in Scottish coronary heart disease mortality between 2000 and 2010 using IMPACTSEC model: Retrospective analysis using routine data. BMJ. 2014;348:g1088. doi: 10.1136/bmj.g1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ministry of Health, Republic of Serbia. Results of the National Health Survey of the Republic of Serbia, 2013. Belgrade: Ministry of Health, Republic of Serbia; 2014. [Google Scholar]
- 35.Statistical Office of the Republic of Serbia. Demographic Yearbook, 2015. Belgrade: Statistical Office of the Republic of Serbia; 2016. [Google Scholar]
- 36.Vlahovic Z, Radojkovic D. Healthcare in Serbia in transition period. EPMA J. 2010;1:601–6. doi: 10.1007/s13167-010-0055-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mathers CD, Fat DM, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: An assessment of the global status of cause of death data. Bull World Health Organ. 2005;83:171–7. [PMC free article] [PubMed] [Google Scholar]
- 38.Richards AM, Lainchbury JG, Nicholls MG. Unsatisfactory redefinition of myocardial infarction. Lancet. 2001;357:1635–6. doi: 10.1016/S0140-6736(00)04858-3. [DOI] [PubMed] [Google Scholar]